Abstract
The purpose of this study was to evaluate the relation between ocular discomfort and ocular Demodex infestation, and therapeutic effects of tea tree oil (TTO) in Demodex blepharitis patients. Three hundred and thirty-five patients with ocular discomfort were evaluated for ocular Demodex infestation and subjective symptoms with ocular surface discomfort index (OSDI) score. Among them, Demodex-infested patients were randomized to receive either eyelid scrubbing with TTO (TTO group,106 patients) or without TTO (Control group, 54 patients) for 1 month. Demodex were found in 84% of patients with ocular discomfort. The number of Demodex was significantly correlated with age (P = 0.04) and OSDI score (P = 0.024). After eyelid scrub treatment, Demodex count was reduced from 4.0 ± 2.5 to 3.2 ± 2.3 in the TTO group (P = 0.004) and from 4.3 ± 2.7 to 4.2 ± 2.5 in the control group (P = 0.27). Also, OSDI score was reduced from 34.5 ± 10.7 to 24.1 ± 11.9 in the TTO group (P = 0.001) and from 35.3 ± 11.6 to 27.5 ± 12.8 in the control group (P = 0.04). In conclusion, Demodex number showed a significant positive correlation with age and subjective ocular discomfort. The tea tree oil eyelid scrub treatment is effective for eliminating ocular Demodex and improving subjective ocular symptoms.
Keywords: Blepharitis, Demodex, Ocular Surface, Tea Tree Oil
INTRODUCTION
Demodex (class Arachnida, superorder Acariformes) is one of the most commonly found ectoparasites in humans (1). Among the many Demodex species, only D. folliculorum and D. brevis are found on the human body, including the face, cheeks, forehead, nose, and eyelids (2). On the skin, Demodex colonizes the entire body, approximately ≤ 5 per square centimeter, and is associated with follicular pityriasis, pustular folliculitis, and rosacea.
On the eyelids, D. folliculorum lives in the eyelash follicles and D. brevis lives deep in the meibomian glands and the sebaceous glands of the lashes. They eat skin cells, hormones, and oils in the hair follicle. The pathogenic role of Demodex in ophthalmology has long been debated. Some studies indicate that Demodex is a nonpathogenic parasite. However, other reports that Demodex is an etiologic factor in chronic blepharitis, conjunctival inflammation, and meibomian gland dysfunction. In patients with ocular rosacea, Demodex causes unusual manifestations, such as superficial corneal neovascularization, marginal corneal infiltration, phlyctenule-like lesions, superficial corneal opacity, and nodular corneal scars (3-7). Gao et al. (8) reported a high prevalence of Demodex in eyelashes with cylindrical dandruff and introduced a method of evaluating ocular demodecosis by sampling and counting Demodex. Recently, Lee et al. (9) showed that the number of Demodex is significantly related to age, ocular discomfort, tear film instability, and poor ocular hygiene. In another study, IL-17, which causes inflammation of the lid margin and ocular surface, was significantly higher in the tears of Demodex infested blepharitis patients than Demodex free blepharitis patients (10, 11).
Tea tree oil (TTO) is natural oil distilled from the leaf of Melaleuca alternifolia. Gao et al. (12) showed its effect for killing Demodex in vitro and in vivo and introduced a lid scrubbing treatment with TTO, which has proven effective for decreasing Demodex in eyelash.
In this study, we tried to evaluate the relation between ocular surface discomfort and ocular demodecosis and analyzed the therapeutic effects of eyelash scrubbing with TTO and in a large group of ocular demodecosis patients.
MATERIALS AND METHODS
This study was a prospective, randomized study performed at the Department of Ophthalmology of the Chung-Ang University Hospital.
Study participants
Three hundred and thirty five patients with ocular surface discomfort, such as dryness, pruritus, ocular pain, or visual disturbance were enrolled between October 1, 2009 and December 31, 2011. Exclusion criteria were as follows: 1) Patient underwent any kind of eye surgery in last 6 months, 2) patients currently using eyedrops other than artificial tears, 3) patients who had eyelid scrubbing treatment previously or currently.
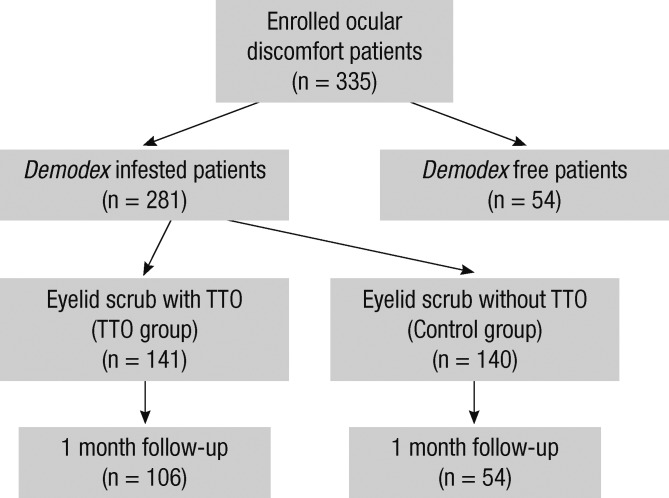
Among those patients, ocular demodecosis (Demodex positive) patients were randomly divided into two groups. The TTO group (n = 141) received eyelid scrub with TTO, and control group (n = 140) received eyelid scrub without TTO. One hundred and six ocular demodecosis patients were followed after eyelid scrub with TTO and 54 patients were followed after eyelid scrub without TTO (Fig. 1).
Fig. 1.
Flow chart shows the total numbers of eyes enrolled, treated, and observed during the follow-up of the study.
Ocular examination
All patients underwent complete ophthalmologic examinations, including slit-lamp biomicroscope examination, microscopic Demodex examination, and tear sampling. After the potential consequences of the study were explained, informed consent was obtained from all participants for examinations.
Patients filled questionnaires about ocular discomfort (Ocular Surface Disease Index, OSDI) by themselves. The OSDI is a 12-item questionnaire designed to provide a rapid assessment of the ocular discomfort symptoms (light sensitiveness, soreness, blurred vision and etc.) and their impact on vision-related functioning (reading, driving, watching TV and etc.). The questionnaires were assessed on a scale of 0 to 100, with higher scores representing greater ocular discomfort (13).
Microscopic Demodex examination
Ocular demodecosis and treatment response were confirmed in a blind manner by single examiner with microscopic examination of epilated lashes. A total of eight eyelashes were examined per patient. Two eyelashes with cylindrical dandruff were sampled from each lid and placed on a glass slide. Under a optical microscope in 400 magnification, a 20 µL drop of saline was applied by pipette to the edge of the glass slide for lashes without retained dandruff. For lashes with retained heavy dandruff, 20 µL of 100% alcohol was added. For the former, the number of Demodex was counted immediately, and for the latter the counting time was delayed up to 20 min to allow the cylindrical dandruff to dissolve and to stimulate the migration of embedded Demodex. The Demodex count was recorded as the total number of mites found in a total of eight lashes per patient.
Eyelid scrub treatment
Ocular demodecosis patients were divided into two groups. The TTO group received eyelid scrub with TTO, and control group received eyelid scrub without TTO.
TTO (Tea tree certified organic®, Sydney Oil Co, Sydney, Australia) was diluted with mineral oil into different concentrations. Weekly lid scrubs with 50% TTO were performed in the clinic, and daily lid scrubs with 10% TTO were advised for four weeks, according to the method reported by Gao et al. (12). In brief, the clinic procedure was as follows: after applying a drop of 0.5% proparacaine, a cotton tip wetted in 50% TTO was used to scrub the lid margin and lash roots three times with a 10-min interval between each scrub. The patients were instructed to continue scrubbing daily at home and advised to close their eyes and massage their lids with medium pressure for three to five minutes using a cotton tip wetted in 10% TTO. After the treatment, the skin was rinsed with clean water and dried with a towel. We advised patients to perform home lid scrubs twice daily.
Control group patients were treated with eyelid scrubs without TTO. The control group patients were asked to scrub their eyelid and lashes with only saline as same as TTO group. We compared the Demodex count and OSDI score change of the two groups.
Statistical analysis
All data are expressed as means ± standard deviation (SD). Pre-treatment and post-treatment parameters were evaluated by Student's t-test, and the between-group data were assessed by 1-way analysis of variance (ANOVA) with Scheffe's post hoc tests. P value of < 0.05 was considered to be statistically significant. SPSS software version 16.0 (SPSS, Inc, Chicago, IL, USA) was used for data analysis.
Ethics statement
The institutional review board of Chung-Ang University approved this study (2001-022-10), and all of the methods adhered to the principles of the Declaration of Helsinki.
RESULTS
Demographic and clinical features
The 335 patients enrolled in this study included 104 men and 231 women, with an average age of 55.7 ± 12.4 yr (range, 23-85 yr). Demodex was found in 281(84%) of 335 patients. The mean total Demodex count per patient was 3.4 ± 3.3 per 8 cilia. The mean total Demodex count per 8 cilia was 3.2 ± 3.6 in men and 3.5 ± 3.2 in women. There was no statistically significant difference in the prevalence of Demodex between the sex (P = 0.56) (Table 1). Demodex was found in 80 of 104 men (77%) and 201 of 231 women (87%).
Table 1.
Ocular Demodex counts and the OSDI scores of patients with ocular discomfort
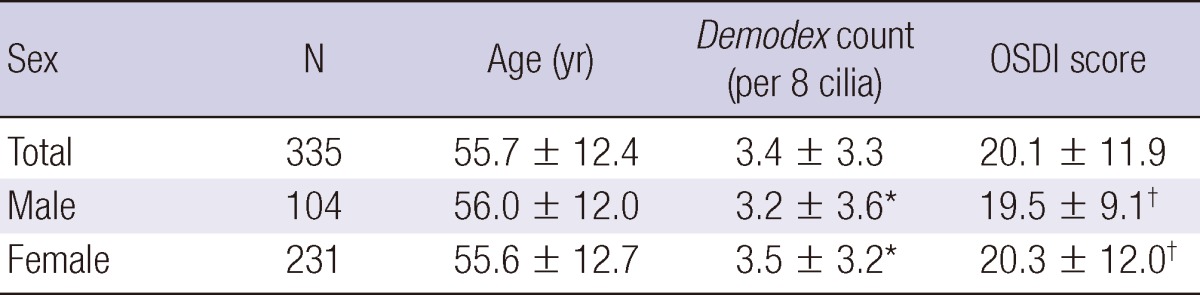
Student's t-test. *P = 0.56; †P = 0.43.
Among Demodex infested patient, most common symptom was ocular dryness (74.7%), and followed by itching sensation (42.7%), ocular irritation (39.1%), visual disturbance (32.0%), conjunctival injection (9.9%), and glare (3.6%).
The prevalence of Demodex according to age is shown in Table 2. The average number of Demodex per patient increased with age. The total number of Demodex per patient was positively correlated with increased age in all patients (Fig. 2A; P = 0.04, correlation coefficient R = 0.563). The mean OSDI score was 20.1 ± 11.9, and the Demodex count showed a significant positive correlation with the OSDI score (Fig. 2B; P = 0.024, correlation coefficient R = 0.512).
Table 2.
The relationship between ocular Demodex count and patient age
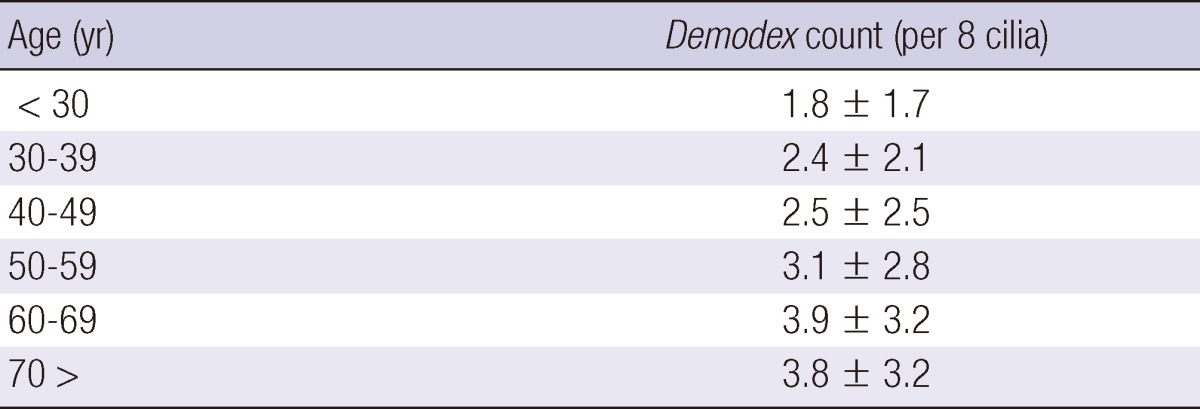
Fig. 2.
Correlation of Demodex with age and ocular surface discomfort index. The number of Demodex showed significant positive correlations with increasing age (A; P = 0.04, correlation coefficient R = 0.563) and ocular surface discomfort index (OSDI) score (B; P = 0.024, correlation coefficient R = 0.512) in ocular discomfort patients.
Tea tree oil treatment group
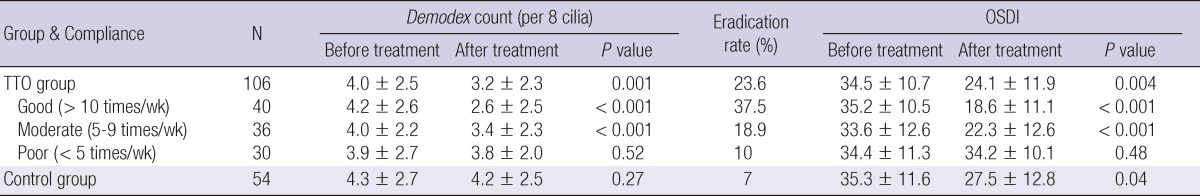
One hundred and six patients with ocular Demodex were followed after completing 1 month of TTO scrubs. Patients included 36 men and 70 women, with an average age of 53.7 ± 10.3 yr (range, 23-85 yr). In these patients, the average number of Demodex and the OSDI score were significantly decreased. The Demodex count was decreased from 4.0 ± 2.5 to 3.2 ± 2.3 (P = 0.001), and the OSDI score also decreased from 34.5 ± 10.7 to 24.1 ± 11.9 (P = 0.004) (Table 3).
Table 3.
Demodex counts and OSDI scores before and after tea tree oil treatment in ocular Demodex patients
TTO, tea tree oil.
Since the TTO scrub was a daily treatment, the effects were expected to differ according to patient compliance. We divided the patients into three groups according to compliance and compared the effect. In the poor compliance group of patients who scrubbed their eyelids less than 5 times per week, the Demodex count and the OSDI score were slightly decreased from 3.9 ± 2.7 to 3.8 ± 2.0 and from 34.4 ± 11.3 to 34.2 ± 10.1, respectively. However, this result was not statistically significant. In the moderate (5 to 9 times per week) and the good (more than 10 times per week) compliance groups, both the Demodex count and the OSDI score decreased significantly, and the changes were statistically significant (Table 3).
Among the tea tree oil treatment group, 23.6% of patients showed eradication of Demodex (zero Demodex). Patients of good compliance group showed 37.5% eradication rate and moderate group showed 18.9% eradication rate. In poor compliance group, only 10% of patients were Demodex free after tea tree oil treatment.
Control group (eyelid scrub without TTO)
Fifty four patients with Demodex were followed after receiving eyelid scrub without tea tree oil. Patients were 20 men and 34 women, with an average age of 55.6 ± 11.3 yr (range, 25-85 yr). The Demodex count was decreased from 4.3 ± 2.7 to 4.2 ± 2.5 but not statistically significant (P = 0.27). And only 7% of patients were Demodex-free after eyelid scrubs without TTO. The OSDI score also decreased statistically significantly from 35.3 ± 11.6 to 27.5 ± 12.8 (P = 0.04) (Table 3).
Both TTO treatment group and control group showed Demodex decrease after treatment, but TTO group showed higher decrease of mean Demodex number (TTO group, -0.85 ± 1.84; Control group, -0.17 ± 1.14) which is statistically significant (P = 0.004).
Changes in Demodex count and OSDI score of TTO sub-group and control group were compared with ANOVA and Scheffe's post hoc test. Both Demodex counts and OSDI scores were significantly decreased in good compliance group compared with poor compliance group or control group. However, Demodex decrease in moderate and poor compliance group showed no statistical significance compared with control group (Fig. 3).
Fig. 3.
Changes in Demodex count (A) and OSDI score (B) after eyelid scrub in TTO group and control group. Group comparisons were performed using ANOVA and Scheffe's post hoc tests. Only significant P values are shown.
DISCUSSION
The number of Demodex increased with patient age in this study. Lee et al. (9) also reported such correlation between age and the number of Demodex, for which there are several explanations. Because Demodex is a symbiotic mite, old people tend to be more heavily infested with Demodex. Also, poor ocular hygiene with increasing age may be associated with an increase of Demodex. From our experience, old people with good eyelid hygiene had fewer Demodex, while young people with poor eyelid hygiene had more Demodex.
Demodex feed on skin cells, hormones, and oils that accumulate within the hair follicle (4-6). Therefore, the sex of the host is thought to be related to the prevalence of ocular Demodex. However in our study, there was no relationship between the number of Demodex and the sex of the patients. There are several reports describing the relationship between rates of Demodex infestation and sex, but this topic remains controversial. Türk et al. (14) reported that males have a higher rate of Demodex infestation, whereas Forton et al. (15) reported that females have a higher rate. Kemal et al. (16) and Lee et al. (9) reported no relationship between rates of Demodex infestation and sex.
In our study, an increase in Demodex was correlated with an increase in subjective symptoms. The index demonstrates sensitivity and specificity in distinguishing between normal subjects and patients with ocular discomfort. Higher OSDI scores represent greater ocular subjective disability. The mean OSDI score of patients with ocular Demodex was 20.1, which indicates moderate to severe ocular discomfort. Patients with Demodex visited our clinic with various ocular surface symptoms, such as dryness, pruritus, ocular pain, visual disturbance, conjunctival injection, and glare. These symptoms are typical of blepharitis. Many reports suggest that ocular Demodex is prevalent in blepharitis patients. Several studies reported that the Demodex infestation is related to corneal and conjunctival pathologic features, and the severity of disease decreases after Demodex is treated (2-5). Since 84% of patients who complained of ocular discomfort were infested with ocular Demodex in our sample, clinicians should be aware of the possibility of ocular Demodex and perform appropriate examinations in these patients.
The role of Demodex in the pathogenesis of blepharitis and other ocular diseases has long been debated. Although many reports and studies have presented Demodex as a non-pathogenic organism, recent studies show evidence of tissue damage in association with Demodex. Dry eye syndrome and blepharitis are thought to be related to Demodex-induced ocular surface disease. A recent study from Kim et al. (11) proposed a possible mechanism of Demodex-induced blepharitis. The study revealed significant differences in the concentrations of a number of cytokines and chemokines in the blepharitis group with ocular Demodex compared with the blepharitis group without ocular Demodex. Specifically, levels of IL-7, IL-12, and IL-17 in the tears of patients with Demodex blepharitis were elevated but then normalized after TTO treatment. The authors concluded that the infestation of Demodex mites induces secretion of IL-17, which can stimulate inflammatory or allergic reactions, as well as cause mechanical blockage of follicles, which ultimately results in ocular surface damage.
There have been many attempts to eliminate ocular Demodex in blepharitis patients. Gao et al. (12) reported that Demodex can be effectively eliminated, in vitro and in vivo, by TTO eyelid scrubs. TTO has traditionally been used in Australia for skin wounds and infections. It is also known for its antibacterial, antifungal, anti-inflammatory, and acaricidal effects (17-20). Gao reported that an eyelid scrub using 50% TTO mixed with shampoo was effective for eliminating Demodex. The two main ingredients of TTO, 1,8-cineole and terpinen-4-ol, have acetylcholinesterase-inhibiting effects that produce an acaricidal effect, and also lead the mite to exit the hair follicle and sweep out before mating.
The effects of TTO on ocular demodecosis have been reported previously in our study (10, 11); however, there were no large-scale clinical trials of TTO treatment for ocular Demodex. Our results demonstrated that scrubbing eyelashes with TTO decreased Demodex counts and improved ocular discomfort. Eyelid scrubbing is one of the most commonly recommended treatments for blepharitis. From our study, simple eyelid scrubbing with saline without TTO might help reducing Demodex numbers and improve ocular symptoms. However, it is not enough to eradicate ocular Demodex. Only 7% of the patients were Demodex-free after eyelid scrubbing without TTO, on the other hand, 24% were Demodex-free after eyelid scrubbing with TTO. Also TTO group showed significantly higher decrease of mean Demodex number and OSDI score elevation than control group.
Patient compliance is a key for successful Demodex eradication. TTO group showed variable eradication results according to patient compliance. Eradication rates were varied from 37.5% to 10%. Only eyelid scrubbing more than 10 times per week with TTO showed significant decrease of both Demodex and OSDI score. From this result, authors recommend patients to scrub frequently, at least 5 times per week. Eyelid scrub without TTO showed decreased OSDI score but no Demodex change. This shows eyelid scrub without TTO has only limited effect on improving subjective discomfort and cannot eliminate the Demodex.
Contact dermatitis, allergic reactions, and ocular irritation are well-known complications of TTO treatment. In this study, five of 106 followed patients reported ocular irritation. Most of these symptoms were caused by improper scrubbing. After reeducation of eyelid scrubbing method, ocular irritation has been disappeared in these patients. There were no severe complications of TTO treatment. TTO treatment is safe and acceptable for clinical use in patients with ocular Demodex. Since patient compliance is a crucial factor for the successful eradication of ocular Demodex with tea tree oil, proper patient education is important.
This study focused on the effect of TTO eyelid scrub treatment in patients with ocular Demodex infestation. The results show that the severity of ocular surface discomfort has a strong positive correlation with the number of Demodex and TTO eyelid scrub treatment is an effective method for eliminating Demodex when frequently applied. Although pathologic role of ocular Demodex may still in debate, these findings suggest that the treatment of ocular demodecosis may improve ocular discomfort.
Footnotes
The authors indicate no financial support or financial conflict of interest. The study protocol was approved by the Institutional Review Board of the Chung Ang University Hospital, Seoul, Korea and was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants.
References
- 1.Basta-Juzbasić A, Subić JS, Ljubojević S. Demodex folliculorum in development of dermatitis rosaceiformis steroidica and rosacea-related diseases. Clin Dermatol. 2002;20:135–140. doi: 10.1016/s0738-081x(01)00244-9. [DOI] [PubMed] [Google Scholar]
- 2.English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91:362–372. doi: 10.1016/0002-9394(81)90291-9. [DOI] [PubMed] [Google Scholar]
- 3.Kamoun B, Fourati M, Feki J, Mlik M, Karray F, Trigui A, Ellouze S, Hammami B, Chaabouni M, Ayadi A. Blepharitis due to Demodex: myth or reality? J Fr Ophtalmol. 1999;22:525–527. [PubMed] [Google Scholar]
- 4.Humiczewska M. Demodex folliculorum and Demodex brevis (Acarida) as the factors of chronic marginal blepharitis. Wiad Parazytol. 1991;37:127–130. [PubMed] [Google Scholar]
- 5.Coston TO. Demodex folliculorum blepharitis. Trans Am Ophthalmol Soc. 1967;65:361–392. [PMC free article] [PubMed] [Google Scholar]
- 6.Heacock CE. Clinical manifestations of demodicosis. J Am Optom Assoc. 1986;57:914–919. [PubMed] [Google Scholar]
- 7.Morfin Maciel BM. Demodicidosis in a female patient treated as allergic blepharoconjunctivitis: a case report. Rev Alerg Mex. 2003;50:232–236. [PubMed] [Google Scholar]
- 8.Gao YY, Di Pascuale MA, Li W, Liu DT, Baradaran-Rafii A, Elizondo A, Kawakita T, Raju VK, Tseng SC. High prevalence of ocular Demodex in lashes with cylindrical dandruffs. Invest Ophthalmol Vis Sci. 2005;46:3089–3094. doi: 10.1167/iovs.05-0275. [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between Demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51:2906–2911. doi: 10.1167/iovs.09-4850. [DOI] [PubMed] [Google Scholar]
- 10.Kim JH, Chun YS, Kim JC. Clinical and immunological responses in ocular demodecosis. J Korean Med Sci. 2011;26:1231–1237. doi: 10.3346/jkms.2011.26.9.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JT, Lee SH, Chun YS, Kim JC. Tear cytokines and chemokines in patients with Demodex blepharitis. Cytokine. 2011;53:94–99. doi: 10.1016/j.cyto.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Gao YY, Di Pascuale MA, Li W, Baradaran-Rafii A, Elizondo A, Kuo CL, Raju VK, Tseng SC. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89:1468–1473. doi: 10.1136/bjo.2005.072363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000;118:615–621. doi: 10.1001/archopht.118.5.615. [DOI] [PubMed] [Google Scholar]
- 14.Türk M, Oztürk I, Sener AG, Küçükbay S, Afşar I, Maden A. Comparison of incidence of Demodex folliculorum on the eyelash follicule in normal people and blepharitis patients. Turkiye Parazitol Derg. 2007;31:296–297. [PubMed] [Google Scholar]
- 15.Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, Sass U, Stene JJ, Thibaut S, Tytgat M, Seys B. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52:74–87. doi: 10.1016/j.jaad.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 16.Kemal M, Sümer Z, Toker MI, Erdoğan H, Topalkara A, Akbulut M. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005;12:287–290. doi: 10.1080/092865805910057. [DOI] [PubMed] [Google Scholar]
- 17.Messager S, Hammer KA, Carson CF, Riley TV. Assessment of the antibacterial activity of tea tree oil using the European EN 1276 and EN 12054 standard suspension tests. J Hosp Infect. 2005;59:113–125. doi: 10.1016/j.jhin.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Halcón L, Milkus K. Staphylococcus aureus and wounds: a review of tea tree oil as a promising antimicrobial. Am J Infect Control. 2004;32:402–408. doi: 10.1016/S0196655304003657. [DOI] [PubMed] [Google Scholar]
- 19.Oliva B, Piccirilli E, Ceddia T, Pontieri E, Aureli P, Ferrini AM. Antimycotic activity of Melaleuca alternifolia essential oil and its major components. Lett Appl Microbiol. 2003;37:185–187. doi: 10.1046/j.1472-765x.2003.01375.x. [DOI] [PubMed] [Google Scholar]
- 20.Hammer KA, Carson CF, Riley TV. Antifungal effects of Melaleuca alternifolia (tea tree) oil and its components on Candida albicans, Candida glabrata and Saccharomyces cerevisiae. J Antimicrob Chemother. 2004;53:1081–1085. doi: 10.1093/jac/dkh243. [DOI] [PubMed] [Google Scholar]