Abstract
Study Objectives:
To assess the amount and quality of sleep that flight crew are able to obtain during flight, and identify factors that influence the sleep obtained.
Design:
Flight crew operating flights between Everett, WA, USA and Asia had their sleep recorded polysomnographically for 1 night in a layover hotel and during a 7-h in-flight rest opportunity on flights averaging 15.7 h.
Setting:
Layover hotel and in-flight crew rest facilities onboard the Boeing 777-200ER aircraft.
Participants:
Twenty-one male flight crew (11 Captains, mean age 48 yr and 10 First Officers, mean age 35 yr).
Interventions:
N/A.
Measurements and Results:
Sleep was recorded using actigraphy during the entire tour of duty, and polysomnographically in a layover hotel and during the flight. Mixed model analysis of covariance was used to determine the factors affecting in-flight sleep.
In-flight sleep was less efficient (70% vs. 88%), with more nonrapid eye movement Stage 1/Stage 2 and more frequent awakenings per h (7.7/h vs. 4.6/h) than sleep in the layover hotel. In-flight sleep included very little slow wave sleep (median 0.5%). Less time was spent trying to sleep and less sleep was obtained when sleep opportunities occurred during the first half of the flight. Multivariate analyses suggest age is the most consistent factor affecting in-flight sleep duration and quality.
Conclusions:
This study confirms that even during long sleep opportunities, in-flight sleep is of poorer quality than sleep on the ground. With longer flight times, the quality and recuperative value of in-flight sleep is increasingly important for flight safety. Because the age limit for flight crew is being challenged, the consequences of age adversely affecting sleep quantity and quality need to be evaluated.
Citation:
Signal TL; Gander PH; van den Berg MJ; Graeber RC. In-flight sleep of flight crew during a 7-hour rest break: implications for research and flight safety. SLEEP 2013;36(1):109–115.
Keywords: In-flight sleep, total sleep time, sleep quality, sleep timing, aircrew, aviation, crew rest facility, polysomnography, age, ultra-long-range
INTRODUCTION
The number of flight operations in which a single sector exceeds a scheduled flight time of 16 h is increasing with the greater range of new-generation aircraft and the commercial demand for nonstop services. These are defined as “ultra-long-range” (ULR) operations1 and require flight crew to be on duty for up to 22 h. These long duty periods have the potential to increase fatigue-related operational risk, particularly during safety critical phases of flight such as the approach and landing phase.
In previous studies of long-haul operations of less than 16 h duration, high levels of sleepiness have been frequently demonstrated through flight crew or observer notes2 and objective measures such as the occurrence of microsleeps.3 Excessive sleepiness can also be inferred from the level of sleep loss experienced, duration of periods of wakefulness required, and the necessity for flight crew to function through the nadir of their circadian rhythm.4
The primary method in place to address the fatigue-related risk in ULR operations is the use of augmented crew, which enables flight crew to rotate through crew rest facilities during scheduled rest breaks and use the opportunity to sleep. The effectiveness of in-flight rest breaks as a mitigation for extended wakefulness on ULR flights depends on the amount and quality of sleep that crew members are able to obtain during the flight.
Subjective reports indicate that sleeping on board the aircraft is more difficult than sleeping at home, and that sleep during flight is disturbed by a range of factors with the most frequently cited being noise, turbulence, and having “thoughts on the mind.”5,6 In previous studies of long-haul flights of between 6.2-15 h duration, retrospective surveys and in-flight questionnaires indicate that the average amount of sleep obtained is relatively short, averaging between 2.2 and 2.4 h.5–7
There is currently very little objective information on how long or how well crew members may be able to sleep during in-flight rest breaks and the factors that might influence this sleep. A limited number of previous studies have used polysomnography to record sleep during flight.7–9 Findings from these studies indicate that rest opportunities earlier in a flight result in less sleep than later rest opportunities and that, not surprisingly, sleep is influenced by the timing of the rest period in relation to circadian phase and duration of prior wakefulness. In these studies, the flight duration was much shorter than the ULR flights now possible, and the duration of in-flight rest opportunities was often very short. Furthermore, no previous studies have compared sleep during flight with that taken in a more ideal sleep location on the ground.
In previous polysomnographic studies of in-flight sleep, the short sleep opportunity and lack of comparison with sleep in a location outside the aircraft are limiting factors in understanding the architecture of in-flight sleep. The aim of the current study was to add to the small body of knowledge on the amount and quality of sleep that flight crew are able to obtain in on-board crew rest facilities during 7-h rest opportunities. Such information is crucial for developing safe operating procedures for ULR flights, and to meet the need for data-driven approaches for managing fatigue in this safety-critical setting.
METHODS
The study received approval from the Wellington Regional Ethics Committee, and written informed consent was obtained from participants. From June to November 2002 data were gathered in association with six delivery flights of Boeing 777-200ER aircraft between Paine Field, Everett, WA (located 40 km north of Seattle) and either Kuala Lumpur International Airport, Malaysia (one flight) or Singapore Changi Airport, Singapore (five flights). These flights were on average 15.7 h (range = 14.8-17 h). A delivery flight involves operating a new aircraft from the location of manufacture to its destination with only operating crew onboard (flight and cabin crew).
Participation
Each flight was operated with four flight crew, with three flight crew on the roster for two separate delivery flights. All 21 flight crew on the roster for the six delivery flights agreed to participate. Once their flight was scheduled, they received an Actiwatch (Philips-Respironics, Bend, Oregon) and sleep diary to record their sleep/wake patterns prior to departing from home in either Kuala Lumpur (Coordinated Universal Time (UTC)+8) or Singapore (UTC+8), while in Seattle (UTC-8), and after returning to their home base (approximately 9 days). Participants also had their sleep polysomnographically recorded in a layover hotel in Seattle and during their 7-h in-flight rest opportunity. Crew rest facilities were located on the same level as the main cabin and contained a bunk bed that allowed horizontal rest.
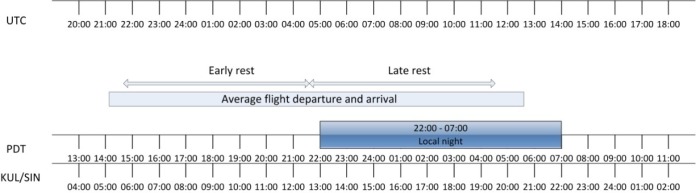
Prior to departure from Seattle, the pattern of work and rest during the flight was agreed upon among the crew, with a designated “early sleep crew” and “late sleep crew.” The early sleep crew had their electrodes applied and were connected to a polysomnographic recorder when they boarded the aircraft. They commenced their 7-h rest opportunity at the top of climb approximately 30 min after takeoff and were awakened if they were still asleep after 7 h. The late sleep crew had electrodes applied at a suitable time in the flight and began their 7-h rest opportunity once the early sleep crew had taken over the operation of the aircraft. After a 7-h rest, or at least 1 h 10 min prior to landing, the late crew were awakened if they were still asleep (Figure 1). Electrodes were removed once the flight crew was no longer operating the aircraft. Participants also completed a questionnaire addressing demographic data and information about normal sleep habits at home and in flight.
Figure 1.
Schematic of average flight departure and arrival time and timing of in-flight rest opportunities relative to Coordinated Universal Time, local time in Seattle, and time in the home base of the flight crew. UTC, Coordinated Universal Time; PDT, Pacific Daylight Time (Seattle local time); KUL, Kuala Lumpur; SIN, Singapore.
Polysomnography
A researcher applied electrodes for all polysomnographic recordings in the layover hotel and during the flight. The researcher was also present for 3 days/nights in Seattle prior to the flight and during the entire flight. Gold electrodes (Grass Technologies, West Warwick, RI, USA) were placed according to the 10-20 system at electroencephalogram (EEG) sites C4, O2, A1, and A2 (recordings on the aircraft also included Fz, Cz, and Oz but data from these sites are not reported here). Left and right electrooculogram (EOG) were recorded from the left and right outer canthus (referenced to A1/A2). Bipolar electromyogram (EMG) was recorded from two electrodes positioned on the mentalis/submentalis muscles. The Embla A10 ambulatory recorder was used (Embla, Denver, Colorado, USA) with inputs sampled simultaneously at 2,000 Hz, digitized to 16-bit resolution, and downsampled to 200 Hz. The signal was digitally filtered (0.5-90 Hz) and stored on a PCMCIA card (SanDisk, Milpitas, CA, USA). To minimize artifacts, impedances were below 5 kΩ when electrodes were connected, electrodes and conducting paste were held securely in place with medical tape, electrode wires were bundled behind the head, and connections were stored in a waist bag to enable crew to move around on the aircraft.
Data Management and Analysis
Actiwatch data were recorded at 1-min intervals and analyzed using the Sleepwatch (Philips-Respironics) software (medium sensitivity setting) in conjunction with sleep diary entries. The difference between sleep onset and sleep offset was used as an estimate of sleep duration. All sleep, including naps, obtained in a 24-h period was summed across the 4 days leading up to departure from Seattle, the day of the flight, and the 3 days after the flight. Midday Seattle time was used as the cutoff point for each 24-h period because all flights were scheduled to depart close to this time.
Sleep scoring was based on five channels: C4-A1/A2, O2-A1/A2, EOG-L, EOG-R, and EMG. EEG and EOG data were low-pass filtered at 30 Hz, whereas EMG data were high-pass filtered at 10 Hz, and low-pass filtered at 70 Hz with a notch filter set at 50 Hz. An event marker indicated when participants began trying to sleep and when they had finished trying to sleep. Sleep scoring started at the first event mark. If the marker had not been pressed, the data were visually inspected to determine where the crew member started trying to sleep (reduction in movement artifact and large blinking eye movements, and increased alpha indicating eye closure).
All sleep recordings were viewed in 30-sec epochs and scored according to the criteria of Rechtschaffen and Kales.10 EEG arousals were scored according to the criteria of the American Sleep Disorders Association (ASDA).11 Sleep recorded in the layover hotel was scored by a single experienced sleep scorer, and every second recording was scored by a second independent individual (mean interrater reliability = 96.0%, standard deviation [SD] = 2.0%, range = 92.5-98.5%). In-flight sleep was scored independently by two experienced sleep scorers (mean interrater reliability = 96.0%, SD = 1.9%, range = 90.4-98.1%).
Descriptive statistics for all variables were generated in SPSS (version 11.0, Armonk, NY, USA)) and mixed linear modeling was undertaken using the SAS system for Windows (version 8.0, Cary, NC, USA). Sleep in the layover hotel was compared with sleep during the flight using paired t-tests, or Wilcoxon signed-rank tests where variables were not normally distributed. Comparisons between sleep taken in the first and second half of the flight were undertaken using independent t-tests, or Mann-Whitney U tests where variables were not normally distributed. Mixed-model analysis of covariance was used to examine effects of the following factors on polysomnographic in-flight sleep: the timing of the sleep opportunity (early or late in flight, as a fixed effect), the total amount of sleep obtained in the 24 h preceding the flight, and the age of the crew member (as continuous variables/covariates). Participant study identification number was entered as a random effect in all models.
RESULTS
Participants
One flight crew member participated in the study protocol twice, resulting in 22 sets of data from 21 flight crew. All flight crew were male, 11 were Captains (mean age = 48 yr, mean h flight experience = 12,400, mean yr flying long-haul = 14.3), and 10 were First Officers (mean age = 35 yr, mean h flight experience = 5,770, mean yr flying long-haul = 7). All flight crew participating in the study regularly operated augmented ULR flights. For some, this was in addition to management responsibilities.
Flights Studied
The average departure time of all flights was 21:11 UTC (Seattle local time 13:11, UTC+8; range 19:02-00:25 UTC) (Figure 1). Due to weather conditions, one flight with three participants made a stopover in Inchon, Korea. Data were only recorded on the Paine Field - Inchon leg (11.3 h) during which two participants were scheduled for 7 h in the crew rest facility (i.e., early rest crew). The other participant was allocated the remaining available time and his data were excluded from analyses. The average duration of the remaining flights was 15.7 h (range = 14.8-17.0 h).
Actigraphic Sleep
Actigraphic and sleep diary data were available for all 22 flight crew. A median of 1.5 nights were recorded at home base pretrip (range = 0-3); however, 10 participants had no pretrip nights recorded. Flight crew were in Seattle for a median of 4.5 nights (range = 2-11) prior to the delivery flight. On 15 occasions participants spent 4 or more nights in Seattle prior to the departure of the delivery flight, five flight crew spent 3 nights, and two flight crew spent 2 nights in Seattle before departing. Data were collected from all flight crew after the flight for a median of 4.6 nights (range = 2-11).
The mean amount of actigraphically estimated sleep obtained in each 24-h period across the 4 days leading up to departure from Seattle and 3 days following the flight are plotted in Figure 2.
Figure 2.
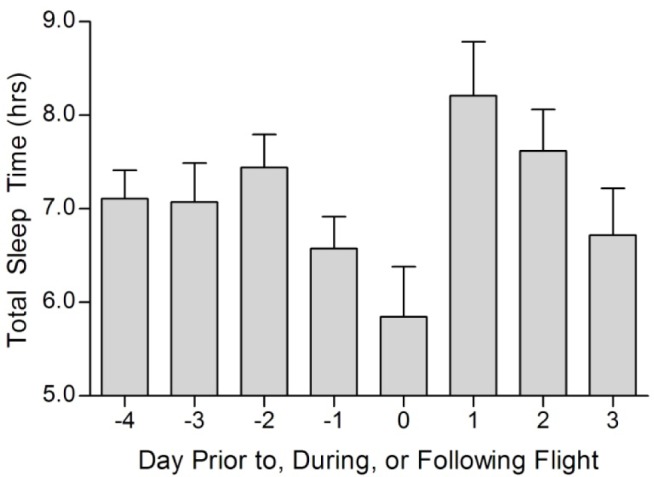
Mean (± SEM) amount of actigraphically estimated sleep obtained in 24-h periods 4 days before (labelled ∔4 to ∔1), during (labelled 0), and 3 days after the flight (labelled 1-3) (data is missing from one person in the 24-h period that includes the flight, and for two flight crew there are only data for the first two of the three 24-h periods after the flight).
Individuals reported requiring 5.6-11.0 h of sleep to feel fully rested (mean = 8.1 h, SD = 1.2), and using actigraphic data they were found to average 7.1 h per 24 h in the four 24-h periods prior to the flight (range = 4.1-11.1), 5.9 h in the 24 h that included the flight (range = 1.7-10.2), and 7.5 h per 24 h in the three 24-h periods after the flight (range = 2.6-14).
On the morning of the delivery flight, nighttime sleep periods ended on average at 07:43 local time (range 05:33-09:15), with no flight crew napping between waking and the departure of the flight. Comparisons between flight crew taking the first and second rest indicate no difference in wake times on the morning of the flight (t = 0.091, P = 0.928) or in sleep obtained in the 24 h prior to the flight (t = ∔1.27, P = 0.221). In the 24 h preceding midday on the day of the flight, flight crew had a median of 1.7 h less sleep (range = ∔4.5 to +4.9) than they reported needing to feel fully rested.
Polysomnographic Sleep
In one layover sleep recording, EEG data were lost so sleep could not be scored. The crew member who participated twice in the study completed only one recording in the layover hotel, so both his in-flight sleep periods were compared with this single night of sleep. For the remaining recordings, 11 flight crew spent 4 or more nights in Seattle before sleep was recorded in the layover hotel, whereas five had layover sleep recorded on the third night after arriving in Seattle, and four on their second night after arrival. All in-flight sleep was taken in the bunk in the crew rest facility.
Table 1 compares the sleep obtained in the layover hotel and in flight. The latency to sleep onset and the frequency of ASDA arousals did not vary according to sleep location, but sleep in flight was less efficient, with more nonrapid eye movement (NREM) Stage 1 (S1) and NREM Stage 2 (S2), less NREM Stage 3 (S3), and more awakenings per h than sleep in the layover hotel.
Table 1.
Comparison of sleep in the layover hotel and sleep in flight
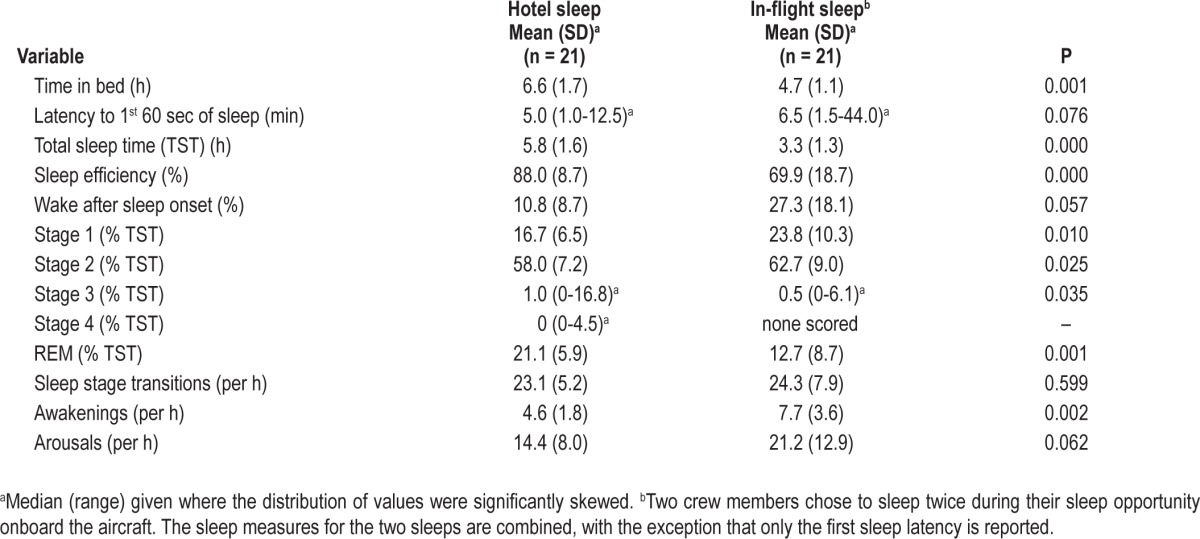
Table 2 compares the sleep of flight crew during the first half of the flight (early sleep crews) versus the second half of the flight (late sleep crews). More time was spent attempting to sleep and more sleep was obtained in the second half of the flight, but the architecture of sleep did not differ in relation to the timing of the sleep episode.
Table 2.
Comparison of sleep taken in the first versus the second half of the flight
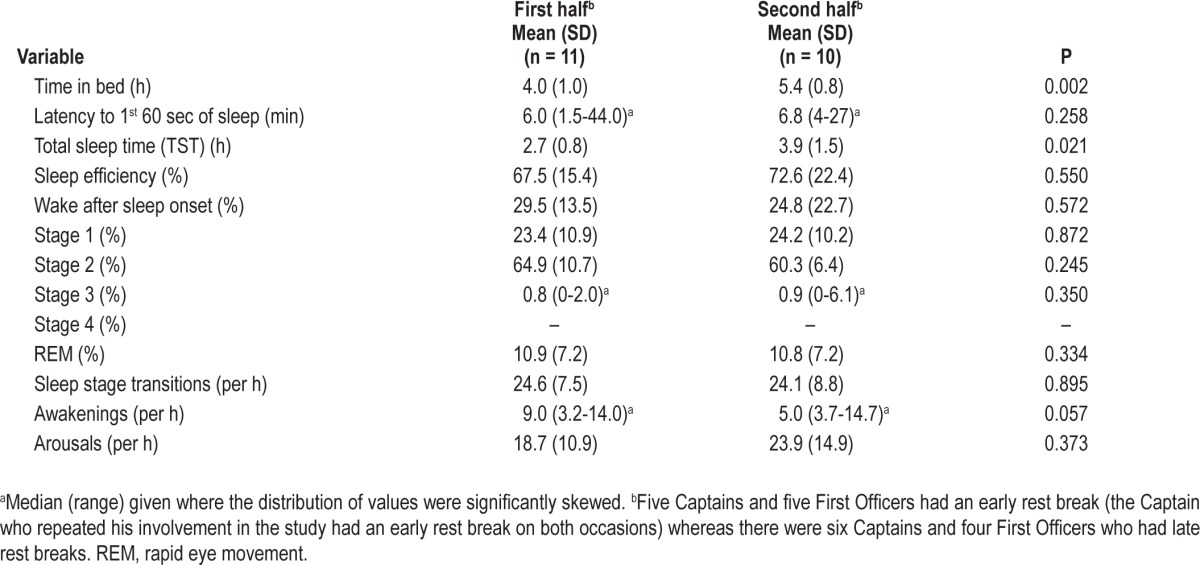
Table 3 summarizes the results of the mixed model analysis of covariance examining factors affecting sleep in flight. When controlling for additional factors, sleep in the second half of the flight was still longer and it also contained fewer awakenings > 60 sec. Crew members who obtained less sleep in the 24 h prior to the flight took longer to enter rapid eye movement (REM) sleep, and spent a smaller proportion of their in-flight sleep in REM sleep. Spearman rho correlations showed no relationship between actigraphic sleep in the 24 h prior to the flight and the percentage of NREM S3 obtained during in-flight sleep opportunities (ρ = ∔0.236, P = 0.303, n = 21).
Table 3.
Factors affecting sleep in flight
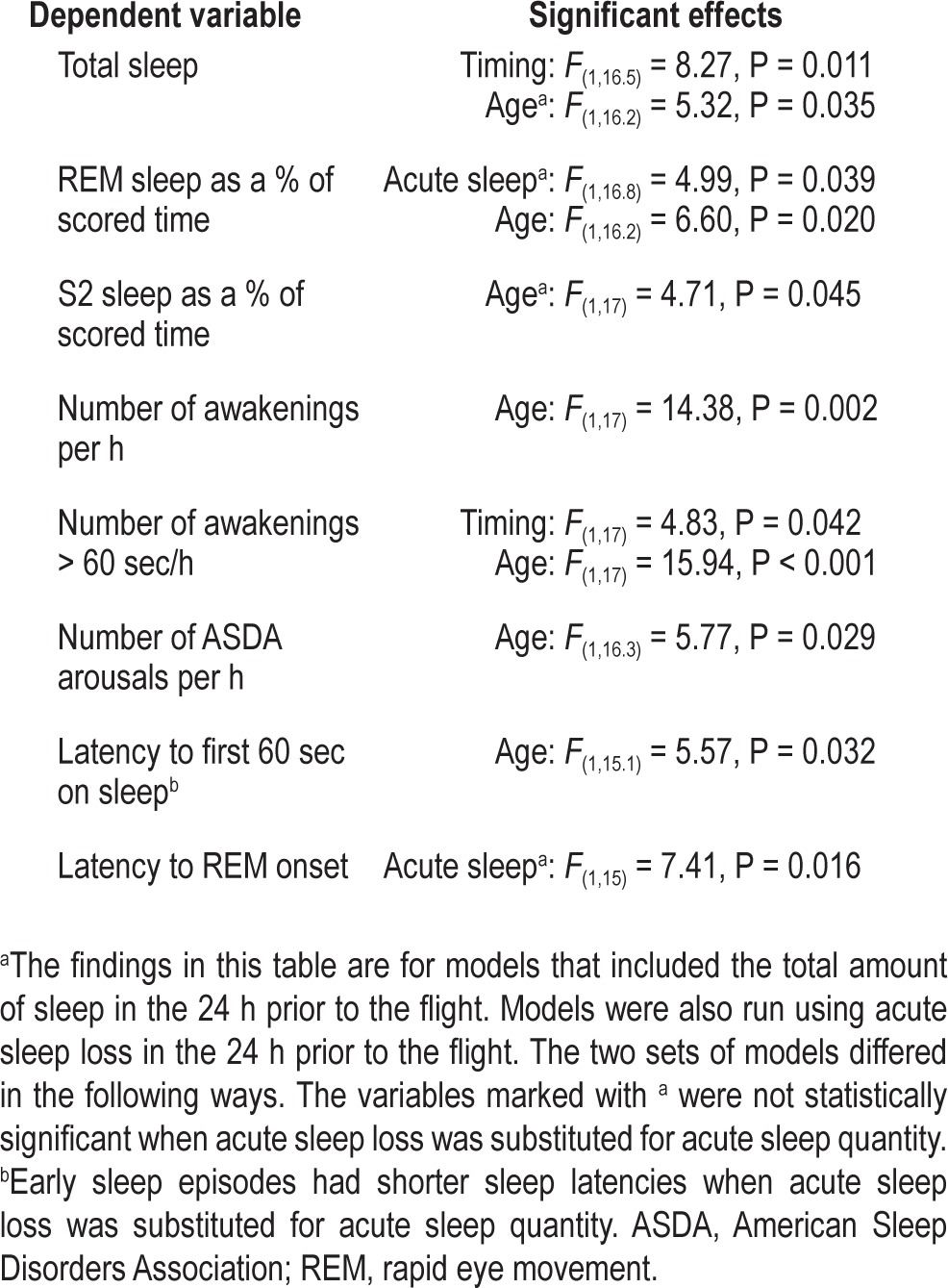
Across all models, the factor most consistently affecting in-flight sleep was age. Older crew members had longer sleep latencies and obtained less total sleep, with a smaller proportion of sleep time spent in NREM S2 sleep and in REM sleep, and with a greater number of awakenings and ASDA arousals.
DISCUSSION
This study with 7-h in-flight rest breaks provides strong objective evidence that sleep in flight is of poorer quality, with lower efficiency, more NREM S1/S2 and less NREM S3, and more awakenings per h, than sleep in the layover hotel. This difference was evident despite the fact that the quality of sleep in the layover hotel was likely to have been reduced by a ′first night effect' (crew members wore the recording equipment for the first time), and for at least four flight crew it is unlikely that they were fully adapted to local time. It is possible that the amount of sleep obtained during the flight was reduced by the presence of recording equipment. Although previous research has shown sleep is generally only affected on the first occasion when recording equipment is worn,12 this has not been confirmed in the unique recording environment studied here. On the other hand, sleep on the aircraft was obtained under ideal conditions with minimal extraneous noise due to the absence of passengers on these delivery flights.
Time Spent Trying to Sleep
Flight crew were asked to spend as much as possible of their in-flight rest opportunity trying to sleep. However, on average they used only 67% of the available time trying to sleep (4.7/7 h), and slept for an average of only 47% (3.3/7 h) of this time. Since 2004, airlines have been officially operating commercial ULR flights and most advise flight crew to split their available rest time into two in-flight rest breaks. A study that recorded in-flight sleep polysomnographically on some of the first ULR flights operated by Singapore Airlines found utilization of the rest opportunities similar to those seen in the current study, despite sleep being split into two periods.13 On the other hand, a more recent study with a Delta Air Lines ULR flight crew found much higher in-flight rest utilization, which was attributed to rest breaks occurring at more favorable times in the circadian cycle (PG, personal communication, January 2012, Wellington, NZ). Variable utilization of available rest time should be considered when biomathematical models are used to predict in-flight sleep and alertness. It also suggests that crew members might benefit from education that increases their awareness of the importance of sleep and knowledge about strategies to improve their sleep in flight.
Sleep Architecture
Very little slow wave sleep (SWS) was recorded in flight (average 0.5% of total sleep time), making it impossible to undertake multivariate analyses of the factors affecting the amount of SWS obtained. Interestingly, flight crew who had less sleep in the prior 24 h took longer to enter REM sleep and spent proportionally less time in REM sleep, after controlling for age and early versus late rest break. When sleep at night is increasingly restricted, SWS is conserved, at the expense of NREM sleep stages 1 and 2, and REM sleep.14,15 However, in the current study, Spearman rho correlations showed no relationship between actigraphic sleep in the 24 h prior to the flight and the percentage of NREM S3 obtained during in-flight sleep opportunities. The near absence of SWS in flight raises a number of questions. A recent hypobaric chamber study that compared sleep during 8-h opportunities at sea level and at typical aircraft cabin pressures occurring in cruise (equivalent to 8,000 feet above sea level) suggests that this is not an effect of altitude per se.16 The limited amount of SWS obtained has also been noted in air traffic controllers who took planned naps during the night shift.17 It is possible that minimal SWS may be a characteristic of sleep taken in the workplace, possibly due to a residual elevation of arousal related to a sense of continuing responsibility and/or the potential for being called in an emergency. A less conducive sleep environment may also play a role. This does not mean that sleep in flight does not have recuperative value. Rather, it implies that care should be taken when extrapolating the findings of studies where sleep is taken in a more ideal setting, such as the laboratory, to an occupational context.
The small amount of SWS recorded during sleep in flight may reduce concerns about severe sleep inertia after waking. Some previous research has shown an association between time in, or waking from, SWS with more severe sleep inertia,18–20 although more recent studies do not support this finding.21–23 Regardless of the relationship between SWS and sleep inertia and the relatively poor quality of sleep obtained during flight, for safety reasons sufficient time should always be provided for sleep inertia to dissipate after sleep taken either in the crew rest facility or in the flight deck before operational tasks are performed.
Factors Affecting In-Flight Sleep
Flight crew assigned the early rest break spent less time trying to sleep and obtained less sleep than those assigned the late rest break. In part, this is probably due to a lower homeostatic sleep drive at the commencement of the early rest break, although it would have encompassed the afternoon nap window for those who were fully adapted to Seattle time before departure (91% of flight crew had 3 nights or more in Seattle prior to the delivery flight and are therefore more likely to have been adapted to local time).
Due to the additional 7 h of wake, homeostatic sleep pressure would be expected to be higher for those assigned to the late rest break, and although the commencement of the rest break encompassed the evening wake maintenance zone, it also extended into the nocturnal sleep period for those who were fully adapted to Seattle time before departure. However, sleep latency and almost all sleep architecture variables did not differ significantly between sleep episodes taken in the early and late rest breaks. Multivariate analyses did indicate that awakenings of longer than 60 sec were more prevalent in the early rest breaks. This suggests that sleep quality is largely unaffected by the timing of the rest break in flight. Nevertheless, for flight crew operating during the descent and landing, sleeping later in flight was advantageous in terms of the amount of sleep obtained as well as reducing the duration of prior wakefulness.
Another factor that was expected to influence the amount of sleep obtained in the rest break was the amount of sleep obtained in the 24 h preceding the flight. However, after controlling for age and early versus late rest breaks, actigraphically determined sleep in the 24 h preceding the flight was not related to sleep duration on the aircraft. This is perhaps surprising, given that total actigraphic sleep in the 24 h to noon on the day of departure ranged from 4.9 h less to 4.5 h more sleep than flight crew thought they needed to feel fully rested (median = 1.7 h less sleep ).
In the multivariate analyses, the factor that most consistently affected the amount and quality of in-flight sleep was age. Older crew members took longer to fall asleep, and obtained less total sleep, with lower proportions of NREM S2 and REM sleep, and more awakenings and arousals. These differences remained significant after controlling for sleep in the 24 h prior to departure and for early versus late rest opportunities. It is not clear whether the lack of SWS in flight, and the greater fragmentation of sleep with aging, affect the recovery value of sleep and the functional capacity of flight crew who regularly experience sleep restriction during commercial flight operations. Newer aircraft types, such as those capable of ULR flight, are often staffed based on seniority, which is the length of time an individual has been employed by an airline. As a consequence the senior flight crew members operating these flights are likely to be older. This practice, coupled with the age limit for flight crew being challenged in general,24 suggests that the relationship between age-related changes in sleep quality and the operational performance of older flight crew deserves additional research scrutiny.
In conclusion, the current study confirms that, even during long in-flight rest periods (average 7 h) with access to lie-flat crew rest facilities, sleep in flight was less efficient and contained less SWS than sleep in a layover hotel. Sleep propensity and sleep architecture are expected to be influenced by a number of factors, including the part of the circadian cycle included in each rest break, the duration of prior wakefulness, and cumulative sleep debt. Thus, caution needs to be exercised when extrapolating these findings to different flights. On the other hand, the finding that age was the most consistent factor affecting in-flight sleep duration and quality may well be generalizable to other aviation operations.
DISCLOSURE STATEMENT
This study was funded by Boeing Commercial Airplanes. Work was performed at Massey University, Wellington, New Zealand. Dr. Graeber was employed by Boeing Commercial Airplanes during the period the study was conducted. Dr. Gander has received research support from the International Air Transport Association and Delta Air Lines. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors would like to acknowledge the participating flight crew, Boeing staff who facilitated this study, and Dr. Mike Muhm for his comments on a draft of the manuscript.
REFERENCES
- 1.Flight Safety Foundation Editorial Staff. Fatigue risk management system helps ensure crew alertness, performance. Flight Safety Digest. 2005;24:16–9. [Google Scholar]
- 2.Graeber RC. Aircrew fatigue and circadian rhythmicity. In: Weiner EL, Nagel DC, editors. Human Factors in Aviation. San Diego: Academic Press, ; 1988. pp. 305–44. [Google Scholar]
- 3.Rosekind MR, Dinges DF, Connell LJ, Rountree MS, Spinweber CL, Gillen KA. Crew factors in flight operations IX: effects of planned cockpit rest on crew performance and alertness in long-haul operations. Moffett Field, California: NASA; 1994. [Google Scholar]
- 4.Gander PH, Gregory KB, Miller DL, Graeber RC, Connell LJ, Rosekind MR. Flight crew fatigue V: long-haul air transport operations. Aviat Space Environ Med. 1998;69:B37–B48. [PubMed] [Google Scholar]
- 5.Pascoe PA, Johnson MK, Montgomery JM, Robertson KA, Spencer MB. Sleep in rest facilities on-board aircraft: questionnaire studies. Farnborough, UK: Centre for Human Sciences, DERA; 1994. [Google Scholar]
- 6.Rosekind MR, Gregory KB, Co EL, Miller DL, Dinges DF. Crew factors in flight operations XII: a survey of sleep quantity and quality in on-board crew rest facilities. Moffett Field, California: NASA; 2000. [Google Scholar]
- 7.Pascoe PA, Johnson MK, Robertson KA, Spencer MB. Sleep in rest facilities on-board aircraft: field studies. Farnborough, UK: Centre for Human Sciences, DERA; 1995. [Google Scholar]
- 8.Simons RM, Valk PJL, de Ree HJD, Veldhuijzen van Zanten BOA, d'Huyvetter K. Onboard crew rest study: quantity and quality of on-board and layover sleep: effects on crew performance and alertness. Results of EEG measurements. Netherlands: Netherlands Aerospace Medical Centre and KLM Royal Dutch Airlines, ; 1994. [Google Scholar]
- 9.Robertson KA, Spencer MB, Stone BM, Johnson MK. Scheduling the on-board rest of aircrew. Farnborough, UK: Centre for Human Sciences, DERA; 1997. [Google Scholar]
- 10.Rechtschaffen A, Kales A. A manual of standardised terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: Brain Information Service/Brain Research Institute, UCLA; 1968. [Google Scholar]
- 11.American Sleep Disorders Association. EEG arousals: scoring rules and examples. Sleep. 1992;15:174–84. [PubMed] [Google Scholar]
- 12.Agnew HW, Webb WB, Williams RL. The first night effect: an EEG study of sleep. Psychophysiology. 1966;2:263–6. doi: 10.1111/j.1469-8986.1966.tb02650.x. [DOI] [PubMed] [Google Scholar]
- 13.Signal TL, van den Berg MJ, Travier N, Gander PH. Phase 3 ultra-long-range validation: polysomnographic sleep and psychomotor performance. Report for the Civil Aviation Authority of Singapore. Wellington, New Zealand: 2004. [Google Scholar]
- 14.Van Dongen H, Maislin G, Mullington J, Dinges DF. The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 15.Belenky G, Wesenten NJ, Thorne D, et al. Patterns of performance degredation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 16.Muhm M, Signal TL, Rock P, et al. Sleep at simulated 2438m: effects on oxygenation, sleep quality and postsleep performance. Aviat Space Environ Med. 2009;80:691–7. doi: 10.3357/asem.2327.2009. [DOI] [PubMed] [Google Scholar]
- 17.Signal TL, Gander P, Anderson H, Brash S. Scheduled napping as a countermeasure to sleepiness in air traffic controllers. J Sleep Res. 2009;18:11–9. doi: 10.1111/j.1365-2869.2008.00702.x. [DOI] [PubMed] [Google Scholar]
- 18.Bruck D, Pisani DL. The effects of sleep inertia on decision-making performance. J Sleep Res. 1999;8:95–103. doi: 10.1046/j.1365-2869.1999.00150.x. [DOI] [PubMed] [Google Scholar]
- 19.Dinges DF, Orne EC, Evans FJ, Orne MT. Performance after naps in sleep-conducive and alerting environments. In: Johnson L, Tepas D, Colquhoun W, Colligan MJ, editors. Biological rhythms, sleep and shiftwork: advances in sleep research. New York: Spectrum; 1981. pp. 37–46. [Google Scholar]
- 20.Dinges DF, Orne MT, Orne EC. Assessing performance upon abrupt awakening from naps during quasi-continuous performance. Behav Res Methods. 1985;17:37–45. [Google Scholar]
- 21.Jewett M, Wyatt J, Ritz-De Cecco A, Khalsa S, Dijk D, Czeisler C. Time course of sleep inertia dissipation in human performance and alertness. J Sleep Res. 1999;8:1–8. doi: 10.1111/j.1365-2869.1999.00128.x. [DOI] [PubMed] [Google Scholar]
- 22.Scheer F, Shea T, Hilton M, Shea S. An endogenous circadian rhythm in sleep inertia results in greatest cognitive impairment upon awakening during the biological night. J Biol Rhythms. 2008;23:353–61. doi: 10.1177/0748730408318081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Signal TL, van den Berg MJ, Mulrine HM, Gander PH. Duration of sleep inertia after napping during simulated night-work and in extended operations. Chronobiol Int. 2012;29:769–79. doi: 10.3109/07420528.2012.686547. [DOI] [PubMed] [Google Scholar]
- 24.Gander P, Signal TL. Who is too old for shift work? Developing better criteria. Chronobiol Int. 2008;25:199–213. doi: 10.1080/07420520802077556. [DOI] [PubMed] [Google Scholar]