Abstract
Study Objectives:
Military members screening positive for blast-related traumatic brain injury (TBI) may subsequently screen positive for posttraumatic stress disorder (PTSD) or depression. The role of sleep as a mediating factor in the development of mental health symptoms was explored.
Design:
Prospective study with symptoms evaluated at two time points.
Setting:
Postdeployment service in Iraq, Afghanistan, or Kuwait during 2008 and 2009.
Participants:
There were 29,640 US Navy and Marine Corps men (29,019 who did not screen positive for PTSD at baseline, 27,702 who did not screen positive for depression at baseline, and 27,320 who did not screen positive at baseline for either condition).
Measurements and Results:
After controlling for sleep problems, the adjusted odds of receiving a positive PTSD screening at follow-up decreased from 1.61 (95% confidence interval [CI] 1.21–2.14) to 1.32 (95% CI 0.99–1.77) for a subject screening positive for TBI relative to a subject screening negative, suggesting that sleep problems mediated 26% of TBI's effect on development of PTSD. Likewise, after controlling for sleep problems, the adjusted odds of receiving a positive depression screening decreased from 1.41 (95% CI 1.11–1.80) to 1.15 (95% CI 0.90–1.47), suggesting that sleep problems mediated 41% of TBI's effect on development of depression. Results were similar for those with either PTSD or depression (37% mediated).
Conclusions:
These results suggest that sleep problems mediate the effect of a positive TBI screening on the development of mental health disorders, and sleep problems may be an early indicator of risk for PTSD or depression.
Citation:
Macera CA; Aralis HJ; Rauh MJ; MacGregor AJ. Do sleep problems mediate the relationship between traumatic brain injury and development of mental health symptoms after deployment? SLEEP 2013;36(1):83–90.
Keywords: Posttraumatic stress disorder, sleep problems, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), and depression are common occurrences for military personnel returning from deployment to Kuwait, Iraq, or Afghanistan in support of Operation Iraqi Freedom and Operation Enduring Freedom (OIF/OEF). These injuries are often the result of the type of combat to which these individuals are exposed, including explosive devices. Although physical trauma associated with combat is easy to document, diagnose, and treat, neurologic sequelae and psychologic trauma are difficult to assess, partly because the diagnosis relies on symptom reporting. However, symptoms may appear insignificant in contrast to the other injuries incurred by that person, or the diagnosis may not yet be identified because some symptoms are not immediately present and may appear gradually over subsequent weeks or months. Because TBI, PTSD, and depression have some overlapping symptoms, it is not clear if the presence of one condition is a precursor to another or how the symptoms may interact with each other.
Sleep problems are common during and after deployment. A review of an Internet-based study of more than 30,000 military men and women found that sleep problems were more common among those with current or recent deployments than among those who were not deployed.1 Another study, which used a 21-item Military Deployment Survey of Sleep, found that almost 75% of active-duty Air Force members (n = 156) rated their quality of sleep as worse while deployed than in their home environment.2 Furthermore, there is evidence that the presence of even mild TBI, which may occur during deployment, can affect sleep patterns and quality.3–5
The health of military service members who have been deployed is routinely monitored by screening tools assessing TBI, PTSD, and depression as well as by instruments measuring related symptoms. These screening tools are administered immediately after deployment and again several months later to monitor long-term health effects. Studies of these screening tools and symptoms allow tracking of sleep problems and other symptoms over time. However, the course of these symptoms that may lead to diagnosis of TBI, PTSD, or depression is complicated. One of the most prevalent complaints has concerned sleep, especially in the case of mild TBI.5 Trouble falling or staying asleep is a common symptom that occurs with TBI, PTSD, and depression, but its role in causation is unclear. There is evidence that long-standing sleep problems (e.g., insomnia) prior to trauma may lead to psychiatric disorders including depression and anxiety.6 It has also been suggested that symptoms related to sleep problems may co-occur with other cognitive and mental disorders.7–9
Although numerous studies have concluded that sleep problems are a frequent consequence of TBI, few have related these sleep problems to mental health outcomes among military service members, and no known studies have attempted to quantify potential indirect effects.5,10–13 By evaluating sleep problems and potential TBI immediately after deployment and PTSD and depression several months later, the ability to describe potential causal mechanisms will be further enhanced. This study tested whether sleep problems significantly mediated the relationship between TBI and the development of PTSD and/or depression using standardized questionnaires administered to all service members after return from deployment.
METHODS
Study Population and Data Sources
Male Navy and Marine Corps personnel who returned from an OIF/OEF deployment in 2008 or 2009 and completed a Post-Deployment Health Assessment (PDHA) and associated Post-Deployment Health Reassessment (PDHRA) were selected for inclusion in the study sample. The PDHA is a brief self-report questionnaire administered to all military personnel at deployment end. The PDHRA is similar in format and content but is administered approximately 3 to 6 mo after the end of deployment. Developed by the Department of Defense, both assessments aim to characterize service members' current health, identify possible deployment-related occupational and environmental exposures, and provide service members with an opportunity to discuss health concerns with a trained healthcare provider. Completed PDHA and PDHRA records were obtained from the US Navy's Electronic Pre- and Post-Deployment Health Assessment Database. A PDHRA was considered to be associated with a PDHA if the date of administration was at least 30 but no more than 365 days after the date of the PDHA. Because some service members had completed several assessments, in the event that more than one PDHRA met the criteria, the first PDHRA was selected. Female service members were excluded because they are believed to be at decreased risk of incurring a TBI due to combat duty restrictions. Were female service members to be included, only 32 female service members in the potential sample screened positive for TBI on the PDHA (1.7%), severely limiting our ability to conduct meditation analyses among women in this population. For the purpose of this study, OIF/OEF deployment was defined as having received hazardous duty pay while deployed for more than 30 days in Afghanistan, Iraq, or Kuwait. To exclude prolonged duty station changes to regions deemed hazardous, deployments lasting longer than 18 mo were not considered for inclusion. Hazardous duty pay and deployment start and end dates were verified using information obtained from the Defense Manpower Data Center (Monterey, CA).
TBI on the PDHA
Beginning in January 2008, a revised version of the PDHA containing additional questions on TBI was introduced. On the electronic assessment, service members were asked to respond yes or no to having experienced a blast or explosion, vehicular accident/crash, fragment wound or bullet wound above the shoulders, fall, or other event such as a sports injury to the head during deployment. After endorsement of at least one injury item, service members were asked whether or not they immediately “lost consciousness or got `knocked out',” “felt dazed, confused, or `saw stars',” or “didn't remember the event.” In accordance with guidance distributed to military healthcare providers14 and established criteria,15 service members who reported having sustained a head injury and chose at least one of the three alteration/loss of consciousness items were considered to have screened positive for a potential TBI. The TBI screening included on the PDHA and PDHRA is a modified version of the three-item Brief Traumatic Brain Injury Screen (BTBIS). One study found that among those screening positive for probable TBI on the BTBIS, 83% provided information consistent with mild TBI at a follow-up interview conducted by a trained specialist and that this percentage did not increase significantly when including the results of longer screening instruments in conjunction with the BTBIS.16
Sleep on the PDHA
The PDHA asks service members to respond yes or no to experiencing each of 24 symptoms at the time of the questionnaire. These symptoms include musculoskeletal, systemic, gastrointestinal, and mental health complaints. For the purpose of this study, a service member response of yes to experiencing the symptom described as “problems sleeping or still feeling tired after sleeping” was assumed to indicate postdeployment sleep problems. This single item aims to capture problems related to both quantity and quality of sleep, although distinction between the two issues is not possible given the nature of the measure. Researchers have noted that future inclusion of a more detailed instrument for identifying sleep problems post-deployment would have merit.17
PTSD on the PDHRA
An abbreviated screening instrument known as the four-item Primary Care PTSD screen (PC-PTSD) is included on the PDHA and PDHRA. To increase the relevance of the four-item PC-PTSD among a military population, the original stem was adapted to read “Have you ever had any experience that was so frightening, horrible, or upsetting that, in the past month, you…” By referring to a specific traumatic experience and stipulating a 1-mo time frame, the adapted stem is expected to have increased likelihood of identifying current PTSD cases. For the purpose of this study, service members received a positive PTSD screening if they answered yes to at least three of the four questions about having experienced symptoms related to the four dimensions of PTSD (re-experiencing, numbing, avoidance, and hyperarousal).18,19 The four-item PC-PTSD has been validated among combat-exposed military service members, and the three-item cutoff is known to have reasonable screening properties with a sensitivity of 0.78 and a specificity of 0.87.20,21 To focus on the development of PTSD, rather than the persistence, service members screening positive for PTSD on the PDHA were excluded from all analyses for which PTSD screening results on the PDHRA were the outcome of interest.
Depression on the PDHRA
Both the PDHA and the PDHRA assessments contain a two-item depression screen derived from the validated Patient Health Questionnaire.22 Based on identified constructs of depression, the screening instrument assesses the amount of time in the past mo a service member was bothered by “little interest or pleasure in doing things” (anhedonia) and “feeling down, depressed, or hopeless” (depressed mood). A response of “more than half the days” or “nearly every day” to either item resulted in a positive screen for potential depression. Similar to the PTSD exclusion criterion, service members who screened positive for depression on the PDHA were not included in analyses for which the outcome of interest was potential depression on the PDHRA.
Demographic and Deployment-Related Variables
A categoric variable for military pay grade was created with one category for all warrant and commissioned officers and three categories representing junior, intermediate, and senior enlisted personnel. Variables indicating service branch (Marine Corps or Navy), service component (active duty or reserve), and deployment location (Afghanistan, Kuwait, or Iraq) were also obtained. From the PDHA, information was collected regarding age in years (younger than 25, 25–29, 30–34, 35–39, or 40 and older) and combat exposure (three items specific to the previous deployment asked service members to respond yes or no to having (1) encountered dead bodies or seen people killed or wounded, (2) engaged in direct combat where they discharged a weapon, or (3) felt in great danger of being killed). Length of deployment was analyzed as a categorical variable with the effect of exceptionally long deployments examined by comparing the fourth quartile of deployment length for the entire sample (214 days or longer) to the three lesser quartiles. Although it is recommended that the PDHRA be completed 3–6 mo after the completion of the PDHA, there was wide variation in the actual time between assessments. For this reason, a variable representing the categorical number of days between questionnaires was created and used in the analyses (≤ 90, 91–120, 121–150, 151–180, > 180 days).
Statistical Analysis
Sleep problems, TBI screening results, and demographic and deployment-related variables were tested for association with mental health outcomes using chi-square tests. In testing the mental health outcome of PTSD, all subjects who screened positive for PTSD on the PDHA were excluded. Similarly, all subjects who screened positive for depression on the PDHA were excluded from depression analyses. When a positive PTSD or depression screen was the outcome of interest, all subjects who screened positive for either PTSD or depression on the PDHA were excluded from the analyses. Additionally, the hypothesis that sleep problems at baseline are associated with persistent mental health complaints was examined using a chi-square test to determine whether service members who screened positive for mental health problems on the PDHA were more likely to screen positive for the same problems on the PDHRA if they also indicated sleep problems at the time of the PDHA.
A mediator is defined as a variable that accounts for all or part of the relation between a predictor and an outcome.23 Unlike a confounder, a mediator can be thought to represent an intermediate state through which the effects of an independent variable are conferred to a dependent variable.24 Although a confounder is frequently introduced into a model to provide an undistorted estimate of the relationship between the independent and dependent variables, a mediator is introduced when interest lies in both the direct and indirect effects of the independent variable on the dependent variable. A statistically significant mediation effect does not confirm causation, but it is frequently observed when a predictor variable causes a mediator, which causes an outcome. In examining mediation, we are making the assumption that sleep problems, although measured at the same time as TBI, commonly develop after TBI. Because we are making this assumption, throughout this article sleep problems will subsequently be considered to be an intermediary symptom hypothesized to represent a causal mechanism through which TBI could potentially affect development of PTSD and/or depression. The limitations of this assumption will be further addressed in the discussion section.
To test our hypotheses that sleep problems mediate the development of PTSD, depression, and PTSD or depression following TBI, the steps for mediation outlined by Baron and Kenny23 were followed. In steps one and two, the associations of the predictor with both the outcome of interest and the potential mediator are independently tested. If both associations are significant, step three entails modeling the association between the predictor and the outcome of interest while controlling for the potential mediator. Mediation is said to occur when the coefficient for the predictor in the controlled model is significantly reduced, relative to the coefficient obtained from the univariate model excluding the mediator. The mediated or indirect effect of a predictor on an outcome can traditionally be calculated as the product of the regression coefficient relating the predictor to the mediator in the univariate model and the coefficient relating the mediator to the outcome in the multivariate model.
All mental health outcomes in this study were dichotomous screening results; therefore, logistic regression models were constructed and the appropriate procedures for mediation with dichotomous dependent variables were followed.25 For each of the three mental health outcomes, Models 1, 2, and 3 were constructed. Model 1 regressed mental health outcomes onto the TBI screening result variable. The resulting coefficient (c) represents the total effect of TBI on the outcome of interest, and a significant c suggests the existence of an effect to be mediated. Model 2 regressed sleep problems onto the TBI screening result variable. The resulting Model 2 coefficient (a), if significant, confirms the existence of a relationship between the mediator and the dependent variable. Model 3 regressed mental health outcomes onto both the TBI screening result variable and sleep problems to obtain two coefficients (c′ and b, respectively). If sleep problems are a significant mediator, a decrease should be seen from c to c′, and the indirect effect of TBI screening results on mental health outcomes (ab) should be different from zero. The Sobel test evaluates the null hypothesis that ab = 0, denoting an insignificant indirect effect of TBI on the mental health outcome of interest.26 In logistic regression, however, comparing coefficients across equations is problematic because independent and dependent variables are measured on a different scale. Prior to testing for the significance of mediation using the Sobel test, coefficients were therefore standardized by multiplying each coefficient by the standard deviation of the independent variable and dividing by the standard deviation of the dependent variable.27 Pay grade, service branch, service component, age, deployment location, combat experiences, deployment length, and time between assessments were controlled in all logistic regression models.
When the direct effect is not zero, the percentage of the total effect that is mediated (ab/[ab + c′]) and the ratio of the indirect to the direct effect (ab/c′) are two measures of the extent of mediation. Although MacKinnon et al.28 conducted simulation studies showing the limited stability of the percentage mediated and the ratio of effects, both measures stabilized when replications were increased and should therefore be acceptable for use in this large sample study.
RESULTS
A total of 55,047 Navy and Marine Corps service members completed a PDHA and an associated PDHRA in 2008–2009. Of these 55,047 sailors and Marines, assessments completed by 29,640 male service members met the inclusion criteria and 825 (2.8%) screened positive for TBI on the PDHA. Relative to service members who screened negative for TBI, those who screened positive were more likely to report sleep problems on the PDHA (36.7% versus 10.3%).
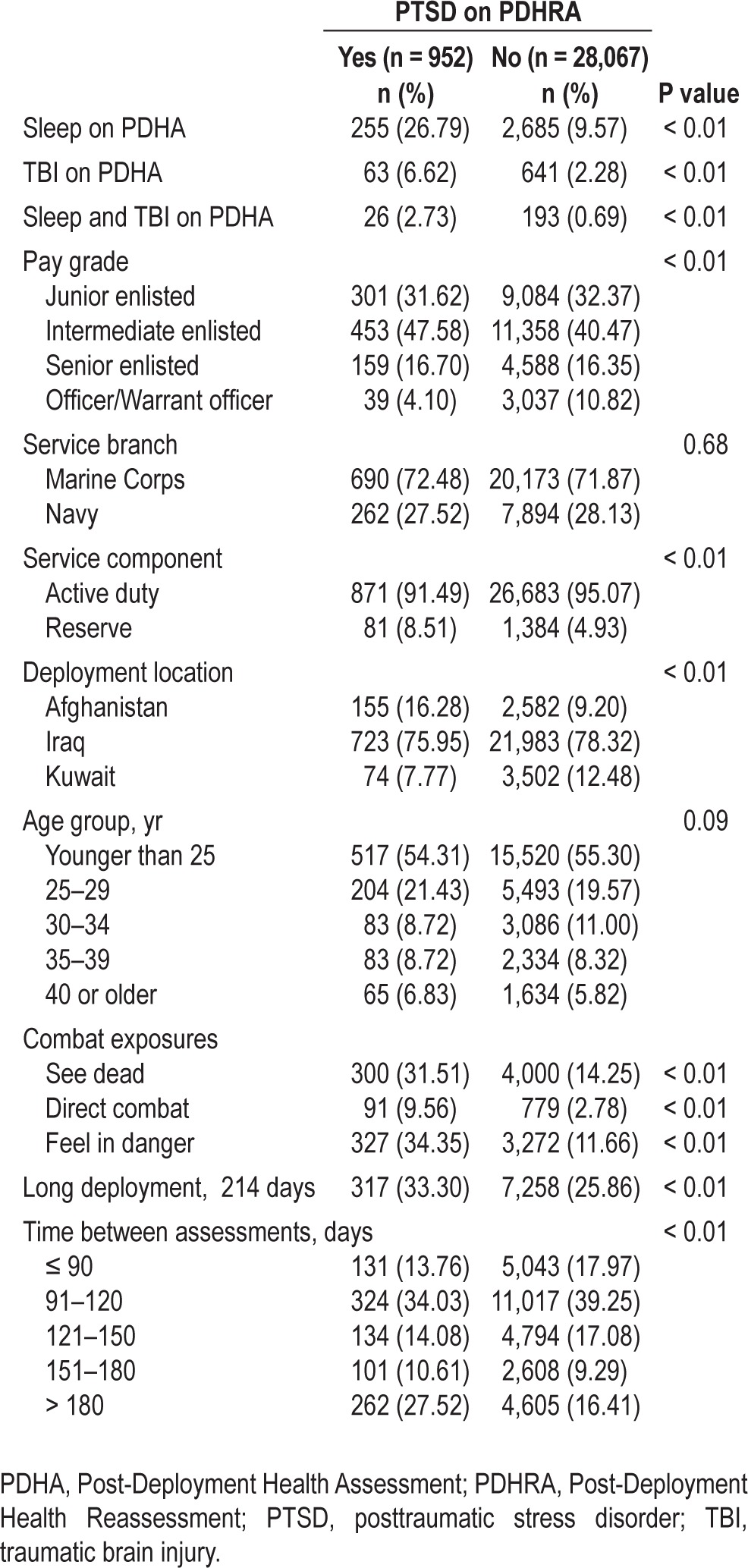
Among the 29,019 service members who did not screen positive for PTSD on the PDHA, 27% of those who screened positive for PTSD on the PDHRA had reported sleep problems on the PDHA compared with fewer than 10% of those who did not screen positive. Similarly, service members who screened positive for TBI on the PDHA had an increased likelihood of screening positive for PTSD on the PDHRA relative to those who did not screen positive for TBI (6.6% and 2.3%, respectively) (Table 1). Only 4.1% of service members screening positive for PTSD on the PDHRA were officers relative to 10.8% of those who screened negative. Additionally, reserve personnel and service members deployed to Afghanistan were significantly more likely to screen positive for PTSD on the PDHRA, relative to active-duty personnel and those deployed to Iraq or Kuwait. All three combat exposures were endorsed at a significantly higher rate among service members screening positive for PTSD on the PDHRA (Table 1). Service members returning from long deployments (≥ 214 days) and those completing the PDHRA more than 180 days after the PDHA had an increased likelihood of screening positive for PTSD (Table 1).
Table 1.
Frequencies associated with new positive PTSD screening (n = 29,019 men)
Sleep problems at baseline were determined to be associated with the persistence of mental health problems within this sample. Among service members who screened positive for PTSD on the PDHA, 47% of those who also reported sleep problems on the PDHA went on to screen positive for PTSD again on the PDHRA, relative to only 33% of those who did not report sleep problems on the PDHA (P = 0.0002). Similarly, in the sample of service members screening positive for depression on the PDHA, depression symptoms were shown to persist, based on PDHRA screening results, among 41% of those reporting sleep problems relative to only 30% of those reporting no sleep problems (P < 0.0001) (results not shown).
Excluding Navy and Marine Corps personnel who screened positive for depression on the PDHA, a sample of 27,702 men was used to evaluate factors associated with a subsequent positive depression screen. Subjects screening positive for depression on the PDHRA were more likely to have reported sleep problems on the PDHA (20.8%) and to have screened positive for TBI on the PDHA (4.5%) compared with those who did not screen positive for depression on the PDHRA (8.2% and 2.3%, respectively). Among those screening positive for depression, a significantly higher percentage were junior and intermediate enlisted personnel, Marines, service members deployed to Iraq or Afghanistan, and subjects younger than 25 years compared with senior enlisted personnel, officers, sailors, service members deployed to Kuwait, and older individuals (Table 2). All three combat exposures were reported at a significantly higher rate among service members screening positive for depression.
Table 2.
Frequencies associated with new positive depression screening (n = 27,702 men)

Navy and Marine Corps personnel who screened positive for either PTSD or depression on the PDHA were excluded, leaving a sample of 27,320 male subjects to evaluate the association of TBI and sleep problems with a subsequent positive PTSD or depression screen on the PDHRA.
Following the Baron and Kenny23 approach, sleep problems reported on the PDHA significantly mediated the relationship between TBI and receipt of a new positive PTSD screen on the PDHRA (Sobel P < 0.01). After controlling for sleep problems, the adjusted odds of receiving a positive PTSD screen for a subject screening positive for TBI compared with a subject who did not screen positive decreased from 1.61 (95% confidence interval [CI] 1.21-2.14) to 1.32 (95% CI 1.32: 0.99-1.77) (Figure 1). Twenty-six percent of the effect of TBI on development of PTSD was mediated by sleep problems. The mediated effect was 35% as large as the direct effect (Table 3).
Figure 1.
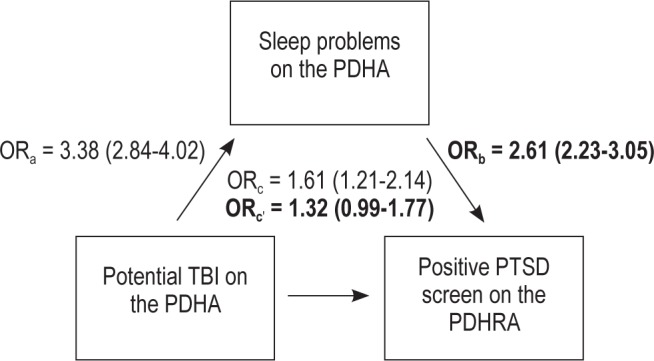
Diagram depicting the role of self-reported sleep problems in mediating the association between a positive TBI screening on the PDHA and a new positive PTSD screening on the PDHRA (n = 29,019 men). Bolding denotes estimates obtained from the final adjusted model (Model 3). CI, confidence interval; OR, odds ratio; PDHA, Post-Deployment Health Assessment; PDHRA, Post-Deployment Health Reassessment; PTSD, posttraumatic stress disorder; TBI, traumatic brain injury. Model is adjusted for pay grade, service branch, service component, age, deployment location, combat experiences, deployment length, and time between assessments.
Table 3.
Tests of significant mediated effects and additional measures of mediation

Sleep problems reported on the PDHA significantly mediated the relationship between TBI and receipt of a new positive depression screen on the PDHRA (Sobel P < 0.01). The adjusted odds of a service member screening positive for depression were estimated to be 1.41 (95% CI 1.11-1.80) times higher for a sailor or Marine who screened positive for TBI relative to a service member who screened negative. However, after controlling for sleep problems, the estimated adjusted odds ratio decreased to 1.15 (95% CI 0.90-1.47) and was no longer significant (Figure 2). Furthermore, sleep problems mediated 41% of the effect of TBI on the development of depression. The mediated effect was 70% as large as the direct effect (Table 3).
Figure 2.

Diagram depicting the role of self-reported sleep problems in mediating the association between a positive TBI screening on the PDHA and a new positive depression screening on the PDHRA (n = 27,702 men). Bolding denotes estimates obtained from the final adjusted model (Model 3). CI, confidence interval; OR, odds ratio; PDHA, Post-Deployment Health Assessment; PDHRA, Post-Deployment Health Reassessment; TBI, traumatic brain injury. Model is adjusted for pay grade, service branch, service component, age, deployment location, combat experiences, deployment length, and time between assessments.
Finally, sleep problems reported on the PDHA also significantly mediated the relationship between TBI and receipt of a new positive PTSD or depression screen on the PDHRA (Sobel P < 0.01). Thirty-seven percent of the effect of TBI on development of PTSD or depression was mediated by sleep problems. The mediated effect was 60% as large as the direct effect (Figure 3 and Table 3).
Figure 3.

Diagram depicting the role of self-reported sleep problems in mediating the association between a positive TBI screening on the PDHA and a new positive PTSD or depression screening on the PDHRA (n = 27,320 men). Bolding denotes estimates obtained from the final adjusted model (Model 3). CI, confidence interval; OR, odds ratio; PDHA, Post-Deployment Health Assessment; PDHRA, Post-Deployment Health Reassessment; PTSD, posttraumatic stress disorder; TBI, traumatic brain injury. Model is adjusted for pay grade, service branch, service component, age, deployment location, combat experiences, deployment length, and time between assessments.
DISCUSSION
This large study found that the effect of a positive TBI screenon the development of PTSD or depression (or both) is mediated by sleep problems. The results of this study emphasize the importance of early identification and treatment of sleep problems. Service members with a potential TBI reported sleep problems immediately after return from deployment but did not endorse PTSD and depression symptoms until several months later. Sleep problems may therefore be an early indicator of risk for PTSD or depression. Immediate treatment of self-reported sleep problems could mitigate the risk for development of mental health disorders, although future (intervention) studies are needed for verification. Attention to and evaluation of sleep problems (regardless of mental health diagnosis) may be an effective strategy to reduce postdeployment morbidity. When considering mental health outcomes, it may be advantageous to implement rehabilitation efforts aimed at preventing and treating sleep problems during the acute postinjury phase. Because most combat-related TBIs are mild and do not require medical evacuation to the United States, in-theater strategies for evaluating sleep should be adopted.
The low prevalence of TBI found in this study (2.8%) compared with previous studies is likely due to the broad inclusion of both combat- and noncombat-exposed personnel in our study sample. Although sleep problems have been shown to mediate the relationship between combat stressors and development of PTSD and depression,29 this study controlled for combat exposures and still identified a strong, independent relationship between TBI and sleep problems. Even after controlling for combat exposure, a known predictor of PTSD and depression, a positive TBI screen remained associated with the development of PTSD and depression both directly and indirectly through sleep problems.
TBI may be a significant predictor of sleep problems, even after controlling for combat exposures, because biological mechanisms independent of psychological distress are frequently responsible for sleep disturbances among service members with TBI. This study demonstrated that independent of reported combat exposure, sleep problems that co-occur with a positive TBI screening are associated with PTSD development.
There are several limitations in this analysis. All presumed diagnoses of TBI, PTSD, and depression were made on the basis of screening tools but without verification of clinical diagnoses. Medical records prior to deployment were not evaluated, making it impossible to determine if subjects had a history of depression, PTSD, or one or more previous TBIs. Furthermore, we did not know the specifics of the sleep problem (e.g., insomnia) or use of medications or stimulants, and we did not know if the sleep problem was preexisting. We had access to one question that indicated sleep was a problem. We had no way to quantify sleep duration and information regarding potential underlying causes for troubled sleep, such as chronic pain or recurring nightmares, was not available. Finally, the severity of TBI, sleep problems, and mental health symptoms was not evaluated. Future studies on this topic would benefit by using several measures of sleep (including objective measures) and examining the dose-response properties of the interrelationships between these three conditions along a spectrum of severity.
Another limitation of this study is that we did not know how long the sleep problems had existed. Bryant et al.6 determined that sleep disturbances during the weeks prior to traumatic injury directly increased a subject's risk of developing a psychiatric disorder in the 3 months postinjury. A study of young adults found that sleep problems (insomnia) were comorbid rather than secondary to depression,7 whereas another study of veterans returning from conflicts in Iraq and Afghanistan found that pain was comorbid with insomnia.30 Although the chronology of TBI, sleep problems, PTSD, and depression was taken into account by analyzing data from two time points, this procedure does not rule out the existence of a single causative event that results in the development of sleep problems, TBI, and delayed-onset PTSD/depression. Our conclusion that sleep problems act as an intermediary between TBI and the development of mental health symptoms also relies on the assumption that TBI precedes development of sleep problems. Such an assumption could not be verified in the current study but is supported throughout the literature.5,10–13
Other issues that should be considered in the interpretation of this report include the psychological motivations that may exist for military personnel completing the postdeployment questionnaires. Warner et al. found in a validation study that Army soldiers were less likely to report depression, PTSD symptoms, and suicidal ideation on the PDHA than with an anonymous survey with many of the same questions.31 If service members in our sample were in fact underreporting depression or PTSD symptoms on the PDHA, the findings presented here regarding sleep problems as a mediator for the development of PTSD/depression may need to be reinterpreted as sleep problems mediating the persistence or worsening of PTSD/depression to the extent where the service member thought it necessary to endorse symptoms on the PDHRA that were not endorsed on the PDHA. Further, if the nonanonymous nature of the assessments resulted in underreporting on both the PDHA and the PDHRA our findings could potentially be underestimates of the role of mediation by sleep problems.32
Several methodological features strengthened our study. Records were obtained from a large sample of more than 25,000 men who responded to a standardized set of questions immediately after deployment and again several months later. Unlike other reports, we collected information from the same men at both time points.33 This large sample used documented deployment activity and included combat- and noncombat-exposed service men. Well-validated screening tools were used to assess likelihood of TBI, PTSD, and depression. Taking a new approach, our analyses modeled sleep problems as a mediator for the association of TBI with PTSD, depression, and both conditions.
CONCLUSION
This work extends what is known about the interrelationships of TBI and mental health symptoms as mediated by sleep problems, and it points to further research directions that may improve the health of service members facing similar stresses associated with deployment. Evaluating sleep problems immediately after TBI while still in theater should be explored as a way to reduce poor mental health outcomes.
DISCLOSURE STATEMENT
This was not an industry-supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was supported by the U.S. Navy Bureau of Medicine and Surgery under Work Unit No. 60818. The views expressed are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government. Approved for public release; distribution is unlimited. This research was conducted in compliance with all applicable federal regulations governing the protection of human subjects (protocol NHRC.2009.0020).
Footnotes
A commentary on this article appears in this issue on page 7.
REFERENCES
- 1.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–35. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 3.Rao V, Bergey A, Hill H, Efron D, McCann U. Sleep disturbance after mild traumatic brain injury: indicator of injury? J Neuropsychiatry Clin Neurosci. 2011;23:201–5. doi: 10.1176/jnp.23.2.jnp201. [DOI] [PubMed] [Google Scholar]
- 4.Schreiber S, Barkai G, Gur-Hartman T, et al. Long-lasting sleep patterns of adult patients with minor traumatic brain injury (mTBI) and non-mTBI subjects. Sleep Med. 2008;9:481–7. doi: 10.1016/j.sleep.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Orff HJ, Ayalon L, Drummon SP. Traumatic brain injury and sleep disturbance: a review of current research. J Head Trauma Rehabil. 2009;24:155–65. doi: 10.1097/HTR.0b013e3181a0b281. [DOI] [PubMed] [Google Scholar]
- 6.Bryant RA, Creamer M, O'Connell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeiter JM, Friedman L, O'Hara R. Insomnia in the context of traumatic brain injury. J Rehabil Res Dev. 2009;46:827–36. doi: 10.1682/jrrd.2008.08.0099. [DOI] [PubMed] [Google Scholar]
- 9.Lewis V, Creamer M, Failla S. Is poor sleep in veterans a function of post-traumatic stress disorder? Mil Med. 2009;174:948–51. doi: 10.7205/milmed-d-04-0208. [DOI] [PubMed] [Google Scholar]
- 10.Castriotta RJ, Wilde MC, Lai JM, Atanasov S, Masel BE, Kuna ST. Prevalence and consequences of sleep disorders in traumatic brain injury. J Clin Sleep Med. 2007;3:349–56. [PMC free article] [PubMed] [Google Scholar]
- 11.Clinchot DM, Bogner J, Mysiw WJ, Fugate L, Corrigan J. Defining sleep disturbance after brain injury. Am J Phys Med Rehabil. 1998;77:291–5. doi: 10.1097/00002060-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Ouellet M, Beaulieu-Bonneau S, Morin CM. Insomnia in patients with traumatic brain injury: frequency, characteristics, and risk factors. J Head Trauma Rehabil. 2006;21:199–212. doi: 10.1097/00001199-200605000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Parcell DL, Ponsford JL, Rajaratnam SM, Redman JR. Self-reported changes to nighttime sleep after traumatic brain injury. Arch Phys Med Rehabil. 2006;87:278–85. doi: 10.1016/j.apmr.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 14.Deployment Health Clinical Center. ASD (HA) Memorandum, Implementation of Revised DD Forms 2796 and 2900, 24 Mar 08. [Accessed March 30]. Retrieved from http://www.pdhealth.mil/dcs/DD_form_2796.asp.
- 15.American Congress of Rehabilitative Medicine. Definition of mild traumatic brain injury. J Head Trauma Rehabil. 1993;8:86–7. http://dx.doi.org/10.1097/00001199-199309000-00010. [Google Scholar]
- 16.Schwab KA, Ivins B, Cramer G, et al. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: initial investigation of the usefulness of a short screening tool for traumatic brain injury. J Head Trauma Rehabil. 2007;22:377–89. doi: 10.1097/01.HTR.0000300233.98242.87. [DOI] [PubMed] [Google Scholar]
- 17.Wright KM, Adler AB, Bliese PD, Eckford RD. Structured clinical interview guide for postdeployment psychological screening programs. Mil Med. 2008;173:411–21. doi: 10.7205/milmed.173.5.411. [DOI] [PubMed] [Google Scholar]
- 18.Asmundson G, Frombach I, McQuaid J, Pedrelli P, Lenox R, Stein M. Dimensionality of posttraumatic stress symptoms: a confirmatory factor analysis of DSM-IV symptom clusters and other symptom models. Behav Res Ther. 2000;38:203–14. doi: 10.1016/s0005-7967(99)00061-3. [DOI] [PubMed] [Google Scholar]
- 19.King WW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: evidence for the dimensionality of posttraumatic stress disorder. Psychol Assessment. 1998;10:90–6. [Google Scholar]
- 20.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the Primary Care Posttraumatic Stress Disorder screen and the Posttraumatic Stress Disorder Checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76:272–81. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 21.Prins A, Ouimette P, Kimerling R, et al. The Primary Care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 23.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 24.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–58. [Google Scholar]
- 26.Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: an interactive calculation tool for mediation tests. [Accessed April 2011]. Available at: http://www.people.ku.edu/∼preacher/sobel/sobel.htm.
- 27.Herr NR. Mediation with dichotomous outcomes, spreadsheet. [Accessed April 2011]. Available at: http://nrherr.bol.ucla.edu/Mediation/logmed.html.
- 28.MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behav Res. 1995;30:41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Picchioni D, Cabrera OA, McGurk D, et al. Sleep symptoms as a partial mediator between combat stressors and other mental health symptoms in Iraq war veterans. Mil Psychol. 2010;22:340–55. [Google Scholar]
- 30.Gellis LA, Gehrman PR, Mavandadi S, Oslin DW. Predictors of sleep disturbances in Operation Iraqi Freedom/Operation Enduring Freedom veterans reporting a trauma. Mil Med. 2010;1755:67–73. doi: 10.7205/milmed-d-09-00123. [DOI] [PubMed] [Google Scholar]
- 31.Warner CH, Appenzeller GN, Grieger T, et al. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch Gen Psychiatry. 2011;68:1065–71. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- 32.Milliken C, Auchterlonie J, Hoge C. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–8. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 33.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175:759–62. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]


