Summary
Background
Characteristically, osteonecrosis affects younger patients who typically refer to the orthopedic surgeon for the first time in the third to fifth decades of life, in the late stages of the disease. Femoral metal-on-metal hip resurfacing is as an alternative to conventional total hip arthroplasty in treating osteoarthritis of the hip. Since there are already many reports regarding the successful outcome of resurfacing in advanced osteoarthritis, the purpose of this study was to analyze the clinical outcomes of this procedure in patients with osteonecrosis of the femoral head and to compare them with a matched group of patients with osteoarthritis.
Material/Methods
This retrospective cohort study evaluated a consecutive series of 52 patients with end-stage osteonecrosis (28 patients) and osteoarthritis (24 patients) of the femoral head, managed by metal-on-metal hip resurfacing in a referral orthopedic center from Feb 2002 to May 2007. Pain, function and deformity were evaluated with the use of the Harris hip score after the operation. Patients were clinically followed for a mean of 41 months.
Results
The patients in the osteoarthritis group had a significantly higher mean age than those in the osteonecrosis group (47.88±12.6 vs 30.86±7.5, p=0.003).
The clinical outcomes were similar for both groups. There was no significant difference in mean Harris hip score (p=0.347) and hip joint range of motion (p=0.346) between osteonecrosis and osteoarthritis groups after surgery.
Conclusions
On the basis of these initial findings, we recommend MOM resurfacing as a viable treatment option for patients with advanced stages of osteonecrosis.
Keywords: total hip arthroplasty, osteonecrosis, metal-on-metal, resurfacing
Background
According to reports on large series of total hip arthroplasties (THA) and the percentage performed for osteonecrosis (ON), there are almost 20 000 new cases of ON of the femoral head in the United States annually, which accounts for 5% to 10% of all primary THA in that country [1–5]. Characteristically, ON affects younger patients who typically refer to the orthopedic surgeon for the first time in their thirties to fifties, in the late stage of the disease [6,7]. THA is a standard treatment option, but for most of the past 40 years it has had less success, specifically in patients with ON and in those who are younger and more active [8–11].
Femoral bone-conserving metal-on-metal (MOM) hip resurfacing was introduced in the early 1990’s [12,13]. It is a procedure that can be particularly useful in patients who may have outlived conventional total hip replacements. It is an attractive method of joint reconstruction, particularly in younger patients, as it preserves proximal femoral bone stock for further revisions, optimizes stress transfer to the proximal femur, and, due to the large diameter of the articulation, offers inherent stability and optimal range of motion [14–16]. MOM-associated problems, including migration of the femoral component, necrosis of the femoral head and fracture of the femoral neck or head, continue to be reported [7,17–20].
MOM hip resurfacing arthroplasty has recently emerged as an alternative to conventional THA in treating advanced stages of osteoarthritis of the hip [14–17] and late Ficat stage III or IV of avascular necrosis. Hip resurfacing has been attempted since the 1950’s. Throughout the 1960’s and 1970’s clinical results were inferior to those of stemmed hip replacement, and the procedure was largely abandoned by the mid 1980’s. The rebirth of MOM hip resurfacing can be attributed to advances in orthopedic implants manufacturing, as well as to the evolution of the surgical technique [21]. A number of recent short- and mid-term reports described early successes of this procedure [1,14,22–31].
Since many reports have already been published regarding the successful outcome of resurfacing in advanced osteoarthritis, the purpose of this study was to analyze the clinical outcomes of MOM total hip resurfacing arthroplasty in patients with osteonecrosis of the femoral head, and to compare them with the results from a matched group of patients with osteoarthritis.
Material and Methods
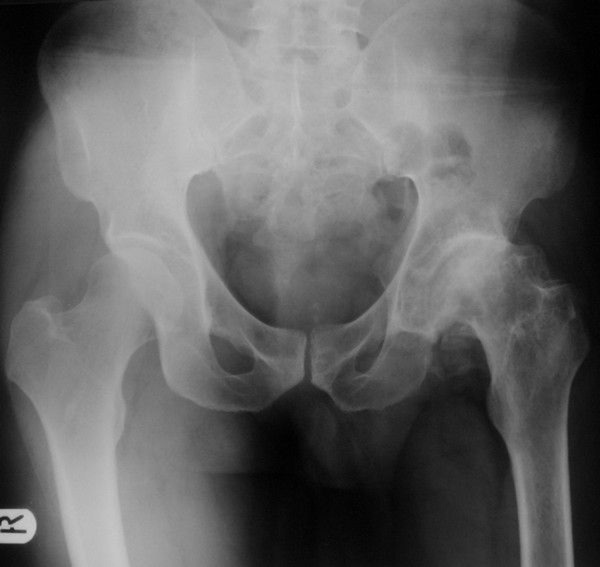
This historical cohort study consisted of a consecutive series of 52 patients managed by MOM hip resurfacing for the treatment of end-stage osteonecrosis and osteoarthritis of the femoral head in a major orthopedic referral center from Feb 2002 to May 2007. All operations were performed by a single orthopedic surgeon (F.M). The patients were divided into 2 groups: the first group included 28 patients with diagnosis of hip osteonecrosis of late Ficat stage 3 and 4 (Figure 1) [32], and the second group consisted of 24 patients with Grade 4 and 5 (Croft’s Grade) of hip joint osteoarthritis (Figure 2) [33]. The 2 groups were matched by sex. All patients were candidates for THA and underwent MOM hip resurfacing.
Figure 1.

Bilateral osteonecrosis of the hip in a 42 year old patient.
Figure 2.
Unilateral osteoarthritis of the hip in a 55 year old patient.
There was no significant sex distribution difference between the 2 groups. In the AVN group, 15 (53.6%) patients were male and 13 (46.4%) patients were female. In the OA group, 13 (54.2%) were male and 11(45.8%) were female (p=0.251). The mean age of patients was significantly different in the AVN and OA groups (30.86±7.5 vs 47.88±12.6 years; p=0.003). In the AVN group, 8 (28.6%) patients were in stage 3 and 20 (71.4%) patients were in stage 4 of the disease. In the OA group, 10 (41.6%) patients were in grade 4 and 14 (58.4%) patients were in grade 5 of the disease.
Patients with stage ≤2 of AVN, grade ≤3 of hip joint OA, infective osteoarthritis and trombophelebitis were excluded from the study.
The operations were performed with an anterolateral approach [34]. Standard instruments for the MOM surface replacement prosthesis (CORMET™, Corin Medical Ltd.) were used for all patients in this study. The acetabular component was nearly hemispherical, with a titanium-plasma spray process creating a porous surface for cementless press-fit fixation. The femoral component had a short metaphyseal stem to facilitate accurate component alignment. The smallest cap was never less than 44 in size and the cup size was always 8 numbers larger than its cap. Figures 3 and 4 show X-rays of the patients with osteonecrosis and osteoarthritis operated on by the MOM resurfacing procedure, respectively.
Figure 3.
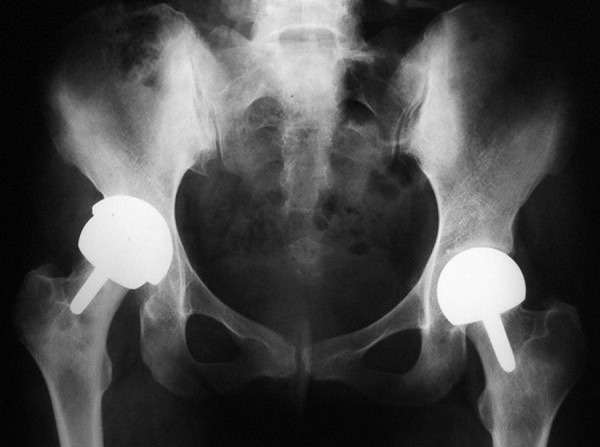
Bilateral Metal on Metal hip resurfacing in a 42 year old patient with osteonecrosis.
Figure 4.
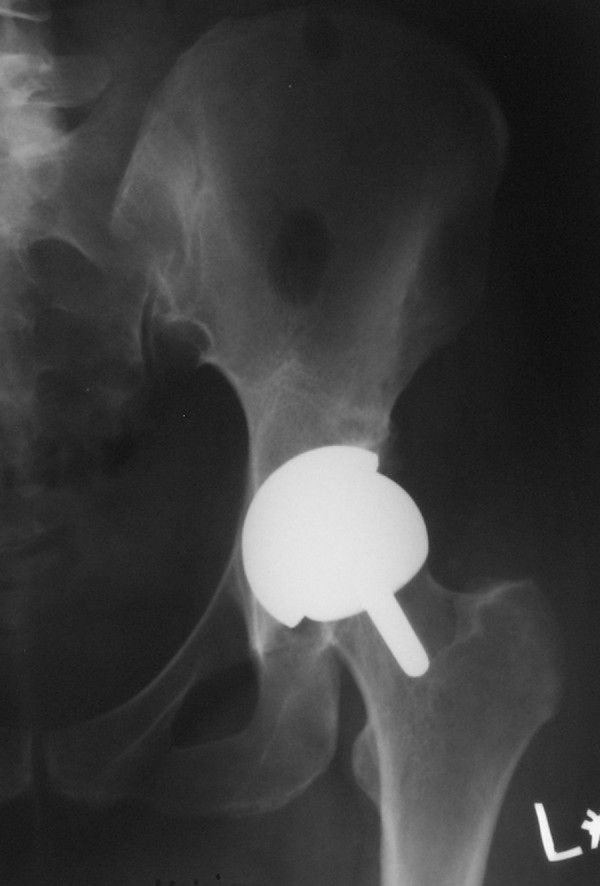
Unilateral Metal on Metal hip resurfacing in a 55 year old patient with osteoarthritis.
Thromboembolic prophylaxis with subcutaneous heparin or enoxaparin was started on the day of the operation, and was continued for 14 consecutive days. On the first postoperative day, all patients were allowed to stand and take a few steps, and physical therapy, including strengthening exercises, was initiated. Patients were restricted to 20% weight-bearing (with the aid of 2 crutches or a walker) until the sixth postoperative week, and then were allowed to advance to 50% (cane or crutch in the opposite hand). From the 12th week onwards, all patients were encouraged to bear full-weight as long as they could tolerate, and to continue hip-strengthening exercises 3 times per week.
The patients were evaluated at 6 weeks, 6 months and 1 year postoperatively, and annually thereafter, and the data were only gathered at the final follow-up. Pain, function, and deformity were evaluated with the use of the Harris hip score (HHS) after the operation. A Harris hip score of ≥90 points was defined as excellent; 80 to 89 as good; 70 to 79 as fair; and <70 as poor outcome. Excellent and good results were classified as successful outcomes, whereas fair or poor results were classified as unsuccessful.
The indications for revision to THA were notching, accidental neck fractures or acetabular cup failure, discovering large cysts in the neck and shortening of the neck where less than 2 cm of the neck remains during the operation.
Statistical analysis
Statistical analysis was performed with SPSS statistical software (version 15.0; SPSS, Chicago, Illinois). Paired t-tests were utilized to compare variables between the 2 study groups. The end point of survival was defined as revision (removal or exchange of 1 or more components) for any reason (eg, aseptic loosening). P-value <0.05 was considered significant.
Results
There was no significant difference between the mean HHS (P=0.347) and hip joint range of motion (P=0.346) between the 2 groups after surgery at the final follow-up (Table 1.) Three (10.7%) patients in the AVN group and 3 (12.5%) patients in the OA group encountered femoral neck fracture or acetabular cup failure (P=0.251) that resulted in revision to standard THA. There was also no significant difference regarding mortality rate after surgery between AVN and OA groups [1 (3.6%) vs 2 (8.3%); P=0.243].
Table 1.
The means of evaluation indices of the clinical outcome in the study patients.
| Evaluation Index | Groups | Patients’ frequency | Mean scores (±SD) | P-values |
|---|---|---|---|---|
| HHS | AVN | 28 | 94±(7.2) | 0.347 |
| OA | 24 | 91.2±(9.4) | ||
| Hip-Joint ROM | AVN | 28 | 216±(6.2) | 0.346 |
| OA | 24 | 196±(5.6) | ||
| Complications (FNF or ACF) | AVN | 3 | 10.7% | 0.251 |
AVN – Avascular Necrosis; OA – Osteoarthritis; ROM – Range Of Motion; HHS – Harris Hip Score; FNF – Femoral Neck Fracture; ACF – Acetabular Cup Failure.
Discussion
The results of our study demonstrated that at a short-term follow-up (a mean of 41 months) there were high levels of function and activity. In 90% of our patients the results were satisfactory; moreover, in this study the MOM total hip resurfacing lead to similar results in patients with osteonecrosis of the femoral head and a matched group of patients with osteoarthritis. Although the mean age of patients was significantly higher in the OA group, there was no difference regarding complications in the 2 groups.
Our result was are in agreement with Mont et al. [1], who demonstrated that the MOM procedure was satisfactory in 95% of patients; moreover, 93% of osteonecrosis and 98% of OA patients were treated successfully with this procedure. Revell et al found there was an overall survival rate of 93.2% at a mean of 6.1 years follow-up. They concluded that MOM hip resurfacing for osteonecrosis can be considered a safe and effective method of surgery [7].
Amstutz et al. studied 85 hips with ON and 915 hips with other etiologies (696 hips with osteoarthritis) [28], demonstrating no difference in survivorship between the ON group and the control group after MOM resurfacing, even after adjusting for head size, body mass index, and defect size. They concluded that the etiology of ON itself does not constitute a contraindication for resurfacing, and the risk factors for the procedure are similar to those of other etiologies.
In an investigation by Stalberg et al., a modern hip resurfacing system was implanted in 1148 hips as part of a U. S. multicenter investigational device exemption study. Of these, 116 hips had a preoperative diagnosis of osteonecrosis, compared to 1023 hips with osteoarthritis. Survival rates were not significantly different (95.9% and 95.8% at 24 months for osteoarthritis and osteonecrosis, respectively). They concluded that resurfacing arthroplasty for patients with osteonecrosis appears to be a reasonable alternative, taking into consideration implant size, patient sex, and size of femoral deficiency [29].
In another study, Beckman et al. analyzed the bone quality and 3-dimensional microarchitecture of the femoral head and neck in patients with ON of the femoral head, and compared them to a group of patients with primary osteoarthritis [30]. They found no statistically significant differences in bone volume and bone volume fraction, connectivity density and the structure model index in patients with ON of femoral head and those with OA. They concluded that hip resurfacing arthroplasty is a possible therapeutic option in the treatment of ON of femoral head in young and active patients, and that an insufficient bone stock in ON of the femoral head seems not to be the deciding factor for failure.
Lei et al. [31] evaluated the short-term clinical outcomes of MOM total hip resurfacing arthroplasty in treating osteonecrosis of the femoral head (ONFH) in young and middle-aged patients, and compared them with hip osteoarthritis patients at the same period. They studied 33 patients (45 hips) with ONFH and 39 patients (45 hips) with osteoarthritis. The patients were observed for 26 months in the ONFH group and 28 months in the osteoarthritis group. Femoral neck fracture occurred after 4 months in 1 patient in the osteoarthritis group, who received total hip arthroplasty; no complication of prosthesis loosening, dislocation, incision infection, osteonecrosis, and bone absorption occurred in other patients. At last follow-up, the Harris scores were 93.0±5.5 in the ONFH group and 94.0±2.4 in the osteoarthritis group, showing no significant difference between the 2 groups (P>0.05); but there were significant differences between pre- and post-operation (P<0.01). They concluded that the clinical short-term outcomes of metal-on-metal total hip resurfacing arthroplasty to treat ONFH are satisfactory and can achieve similar outcomes to that of the osteoarthritis group.
Some previous studies reported that femoral resurfacing hemiarthroplasty can be a viable option for certain patients with late-stage osteonecrosis and minimal acetabular involvement [18,35–37]. However, it is not a permanent solution, since failure eventually occurs as a result of acetabular cartilage erosion. Resurfacing of both sides of the joint, as in MOM resurfacing, may offer a more permanent solution than limited resurfacing of only the femoral side [3,18,24,34,36–42].
In this study we used the HHS, which is a known classification for evaluation of the hip joint function. Some studies have reported different results by using different methods of scoring. For example, Pollar et al. [43] reported that by using the Oxford hip score the result from the patients who underwent hybrid total hip arthroplasty and those who underwent MOM resurfacing method were not different, but by using Activity score and Euro Qol score the patients who underwent MOM resurfacing arthroplasty achieved higher scores after 7 years of follow-up.
This study was limited by the relatively small patient population and the limited duration of follow-up. We are waiting for long-term results to see if these early excellent results are maintained.
Conclusions
On the basis of these initial findings, we recommend MOM resurfacing as a viable treatment option for patients with advanced stages of osteonecrosis.
Acknowledgement
The authors wish to thank Dr. Abbas Daneshmand, Anaesthetist; Mrs. Masoomeh Sadeghian, RN; Mrs. Mobashereh Bagheri, Clinical Manager; Mrs. Khadijeh Poor Seyyed. RN and Mrs. Eshrat Alambeigi, Librarian for their help in preparing the patients, providing their data, inviting the patients for follow up and providing some necessary references.
Footnotes
Conflict of interest
The authors declare that they have no relevant financial interests in this manuscript.
Source of support: Departmental sources
References
- 1.Mont MA, Seyler TM, Marker DR, et al. Use of metal-on-metal total hip resurfacing for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg [Am] 2006:889–97. doi: 10.2106/JBJS.F.00543. [DOI] [PubMed] [Google Scholar]
- 2.Parsons IM, IV, Weldon EJ, III, Titelman RM, Smith KL. Glenohumeral arthritis and its management. Phys Med Rehabil Clin N Am. 2004;15(2):447–74. doi: 10.1016/j.pmr.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Lieberman JR, Berry DJ, Mont MA, et al. Osteonecrosis of the hip: management in the 21st century. J Bone Joint Surg [Am] 2002;84:834–53. [PubMed] [Google Scholar]
- 4.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Parker Vail T, Covington DB. The incidence of osteonecrosis. In: Urbaniak JR, Jones JP Jr, editors. Osteonecrosis-etiology, diagnosis, and treatment. Rosemont, Ill: AAOS; 1997. p. 43. [Google Scholar]
- 6.Callaghan JJ, Forest EE, Sporer SM, et al. Total hip arthroplasty in the young adult. Clin Orthop Relat Res. 1997;344:257–62. [PubMed] [Google Scholar]
- 7.Revell MP, McBryde CW, Bhatnagar S, et al. Metal-on-metal hip resurfacing in osteonecrosis of the femoral head. J Bone Joint Surg [Am] 2006;88(3):98–103. doi: 10.2106/JBJS.F.01070. [DOI] [PubMed] [Google Scholar]
- 8.Chandler HP, Reineck FT, Wixson RL, et al. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426. [PubMed] [Google Scholar]
- 9.Fyda TM, Callaghan JJ, Olejniczak J, et al. Minimum ten-year follow-up of cemented total hip replacement in patients with osteonecrosis of the femoral head. Iowa Orthop J. 2002;22:8. [PMC free article] [PubMed] [Google Scholar]
- 10.Jinnah RH, Amstutz HC, Tooke SM, et al. The UCLA Charnley experience: a long-term follow-up study using survival analysis. Clin Orthop Relat Res. 1986;(211):164–72. [PubMed] [Google Scholar]
- 11.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg Am. 1996;78:995. doi: 10.2106/00004623-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Amstutz HC, Grigoris P, Dorey FJ. Evolution and future of surface replacement of the hip. J Orthop Sci. 1998;3:169–86. doi: 10.1007/s007760050038. [DOI] [PubMed] [Google Scholar]
- 13.McMinn D, Treacy R, Lin K, Pynsent P. Metal-on-metal surface replacement of the hip: experience of the McMinn prosthesis. Clin Orthop Relat Res. 1996;329:89–98. doi: 10.1097/00003086-199608001-00009. [DOI] [PubMed] [Google Scholar]
- 14.Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 year: results of 2- to 9-year follow-up. Clin Orthop Relat Res. 2007;460:159–64. doi: 10.1097/BLO.0b013e318041f0e7. [DOI] [PubMed] [Google Scholar]
- 15.Forrest N, Welch A, Murray AD, et al. Femoral head viability after Birmingham resurfacing hip arthroplasty: assessment with use of [18F] Xuoride positron emission tomography. J Bone Joint Surg Am. 2006;88(Suppl 3):84–89. doi: 10.2106/JBJS.F.00877. [DOI] [PubMed] [Google Scholar]
- 16.Grigoris P, Roberts P, Panousis K, Jin Z. Hip resurfacing arthroplasty: the evolution of contemporary designs. Proc Inst Mech Eng [H] 2006;220:95–105. doi: 10.1243/095441105X69042. [DOI] [PubMed] [Google Scholar]
- 17.Adili A, Trousdale RT. Femoral head resurfacing for the treatment of osteonecrosis in the young patient. Clin Orthop Relat Res. 2003;417:93–101. doi: 10.1097/01.blo.0000096815.78689.3e. [DOI] [PubMed] [Google Scholar]
- 18.Cuckler JM, Moore KD, Estrada L. Outcome of hemi resurfacing in osteonecrosis of the femoral head. Clin Orthop Relat Res. 2004;429:146–50. doi: 10.1097/01.blo.0000150121.88033.50. [DOI] [PubMed] [Google Scholar]
- 19.Schmalzried TP. Total resurfacing for osteonecrosis of the hip. Clin Orthop Relat Res. 2004;429:151–56. doi: 10.1097/01.blo.0000150319.35347.2d. [DOI] [PubMed] [Google Scholar]
- 20.Shimmin AJ, Bare J, Back DL. Complications associated with hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:187–93. doi: 10.1016/j.ocl.2005.01.002. (ix) [DOI] [PubMed] [Google Scholar]
- 21.Trebse R, Berce A, Kovac S. Metal-On-Metal hip resurfacing arthroplasty using the direct lateral approach. First results and literature review. Zdravniski Vestnik-Slovenian medical journal. 2008;77:751–55. [Google Scholar]
- 22.Mont MA, Ragland PS, Etienne G, et al. Hip resurfacing arthroplasty. J AmAcad Orthop Surg. 2006;14:454–63. doi: 10.5435/00124635-200608000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years follow up. Clin Orthop Relat Res. 2006;453:123–31. doi: 10.1097/01.blo.0000238852.08497.92. [DOI] [PubMed] [Google Scholar]
- 24.Amstutz HC, Beaule’ PE, Dorey FJ, et al. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 25.Beaule’ PE, Le Duff M, Campbell P, et al. Metal-on-metal surface arthroplasty with a cemented femoral component: a 7–10 year follow-up study. J Arthroplasty. 2004;19:17–22. doi: 10.1016/j.arth.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Mac Donald SJ. Metal-on-metal total hip arthroplasty: the concerns. Clin Orthop Relat Res. 2004;429:86–93. doi: 10.1097/01.blo.0000150309.48474.8b. [DOI] [PubMed] [Google Scholar]
- 27.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 28.Amstutz HC, Le Duff MJ. Hip resurfacing results for osteonecrosis are as good as for other etiologies at 2 to 12 years. Clin Orthop Relat Res. 2010;468(2):375–81. doi: 10.1007/s11999-009-1077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stulberg BN, Fitts SM, Zadzilka JD, Trier K. Resurfacing arthroplasty for patients with osteonecrosis. Bull NYU Hosp Jt Dis. 2009;67(2):138–41. [PubMed] [Google Scholar]
- 30.Beckmann J, Matsuura M, Grässel S, et al. A muCT analysis of the femoral bone stock in osteonecrosis of the femoral head compared to osteoarthrosis. Arch Orthop Trauma Surg. 2009;129(4):501–5. doi: 10.1007/s00402-008-0666-y. [DOI] [PubMed] [Google Scholar]
- 31.Lei M, Yang S, Xu W, et al. [Metal-on-metal total hip resurfacing arthroplasty for treatment of advanced osteonecrosis of femoral head in young and middle-aged patients] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24(3):262–65. [PubMed] [Google Scholar]
- 32.Canale T. Operative orthopedics. Vol.1.11th. edition. Mosby; 2008. p. 1033. [Google Scholar]
- 33.Reijuan M. Validity and reliability of three definitions of hip osteoarthritis: cross sectional and longitudinal approach. Annals of the rheumatic disease. 2004;63:1427–33. doi: 10.1136/ard.2003.016477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rue JP, Inoue N, Mont MA. Current overview of neurovascular structures in hip arthroplasty: anatomy, preoperative evaluation, approaches, and operative techniques to avoid complications. Orthopedics. 2004;27:73–83. doi: 10.3928/0147-7447-20040101-25. [DOI] [PubMed] [Google Scholar]
- 35.DisBrinker MR, Rosenberg AG, Kull L, Galante JO. Primary total hip arthroplasty using non cemented porous-coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty. 1994;9:457–68. doi: 10.1016/0883-5403(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 36.Mont MA, Rajadhyaksha AD, Hungerford DS. Outcomes of limited femoral resurfacing arthroplasty compared with total hip arthroplasty for osteonecrosis of the femoral head. J Arthroplasty. 2001;16(8):134–39. doi: 10.1054/arth.2001.28722. [DOI] [PubMed] [Google Scholar]
- 37.Beaule PE, Schmalzried TP, Campbell P, et al. Duration of symptoms and outcome of hemi resurfacing for hip osteonecrosis. Clin Orthop Relat Res. 2001;385:104–17. doi: 10.1097/00003086-200104000-00018. [DOI] [PubMed] [Google Scholar]
- 38.Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg [Br] 2005;87-B:324–29. doi: 10.1302/0301-620x.87b3.15556. [DOI] [PubMed] [Google Scholar]
- 39.Beaule PE, Dorey FJ. Survivorship analysis of cement less total hip arthroplasty in younger patients. J Bone Joint Surg [Am] 2001;83:1590–91. doi: 10.2106/00004623-200110000-00028. [DOI] [PubMed] [Google Scholar]
- 40.Seyler TM, Etienne G, Plate JF, et al. Use of large femoral heads without liners in total hip arthroplasty. Surg Technol Int. 2006;15:217–20. [PubMed] [Google Scholar]
- 41.Grigoris P, Roberts P, Panousis K, Bosch H. The evolution of hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36(2):125–34. doi: 10.1016/j.ocl.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 42.Campbell P, Mirra J, Amstutz HC. Viability of femoral heads treated with resurfacing arthroplasty. J Arthroplasty. 2000;15:120–22. doi: 10.1016/s0883-5403(00)91415-3. [DOI] [PubMed] [Google Scholar]
- 43.Pollar TCB, Baker RP, Eastaugh WSJ, et al. A five to seven years comparison of hybrid total hip arthroplasty and metal on metal resurfacing. Journal Bone and joint surgery. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]


