Summary
Background
Comparison of the quality of life (QoL) trends after TVT, TVT O and Burch colposuspension (BCS) procedures and comparison of long-term subjective and objective outcomes.
Material/Methods
The study included 215 women who underwent a TVT, TVT O or BCS procedure. We monitored QoL after each procedure and the effect of complications on the QoL as assessed by the IQOL questionnaire over a 3-year period.
Results
The study was completed by 74.5% of women after TVT, 74.5% after TVT O, and 65.2% after BCS procedure.
In the long-term, the QoL improved from 46.9 to 88.7 and remained stable after BCS; after TVT and TVT O, it declined, but only after TVT O was the decline statistically significant compared to BCS.
The IQOL for women with post-operative complications has a clear descending tendency. The effect of the complications is highly significant (p<0.001). Only the OAB complication had a statistically significant effect on QoL p<0.001. Preexistent OAB does not negatively affect postoperative results of anti-incontinence surgery.
Conclusions
There was a statistically significant decline with the longitudinal values of IQOL with TVT O, but not with TVT or BCS. Anti-incontinence operations significantly improve quality of life for women with MI, but compared to the SI group, the quality of life is worse when measured at a longer time interval after the operation. Anti-incontinence operations significantly improve quality of life, and the difference in preoperative status in the long-term follow-up is demonstrable.
Keywords: anti-incontinence surgery, Burch colposuspension, Incontinence Quality of Life, long-term results, Mixed Incontinence, Stress Urinary Incontinence, TVT, TVT O
Background
Stress urinary incontinence [1,2] is a common problem which affects a high percentage of women [3]. In addition to pelvic floor muscles exercise, surgery has played an important role in the treatment of stress urinary incontinence (SUI). It should be possible to offer a surgical procedure which is highly effective, safe and has good long-term outcome.
Burch colposuspension (BCS) was considered a gold standard in anti-incontinence surgery, with good long-term results [4]. Many studies have confirmed its cure rate at 69–88% [3–5]. However, over the past decade this procedure has been largely replaced by the application of various types of TVTs (tension-free vaginal tapes) [6–11]. TVT and colposuspension achieve similar success rates in treating stress incontinence [12,13]. There have not been many long-term studies dealing with the occurrence of complications and quality of life after anti-incontinence operations. The majority of studies assess the final condition of the patients, while the comparison of objective and subjective information is always an issue. Our study focused on comparing developments in the quality of life and the occurrence of complications in a long-term follow-up after TVT, TVT O and BCS. For subjective assessment of urinary incontinence, we have chosen a validated specialized Incontinence Quality of Life questionnaire (IQOL) [14], which is brief and comprehensive, for diagnosing urinary incontinence and OAB in women.
The aim of our study was to monitor the trends in quality of life after TVT, TVT O and BCS procedures, and to establish whether the occurrence of complications affects the quality of life (QoL).
Material and Methods
This prospective observational study included 215 women who underwent surgical treatment for stress urinary incontinence between January 2002 and December 2005. The study was approved by the local ethics committee. Before enrollment, all subjects gave written consent to their inclusion in the study. Final data have been processed for 154 (71.6%) women who underwent all controls according to the prepared protocol. Before surgery, the women filled in the IQOL questionnaire, their case history was taken, and they underwent a complete urogynecological examination: clinical examination, transperineal ultrasound (using an Acuson 128 XP10, Voluson 730 Expert, GE HealthCare, convex probe 3.5/5MHz), complete urodynamic examination (filling cystometry, profilometry, uroflowmetry – using Dantec duet Meditronics and later Uromics 7 B-K Medical A/S equipment) and 3-day voiding diary [2,15]. All women who underwent the operation had urodynamic stress urinary incontinence. Mixed type of incontinence with predominant stress type was not an exclusion criterion from the study. Exclusion criteria were pelvic organ prolapse >1st stadium using pelvic organ prolapse quantification system POP-Q [16], predominant urgency incontinence, and postvoid residual volume (PVR) greater than 100 mL. Surgery was only offered if conservative therapy was unsuccessful. Women with concomitant operations were also excluded from the study.
TVT procedure (Gynecare TVT, Ethicon, Inc. Piscataway, NJ, USA) was carried out as recommended by Ulmsten [7]. TVT O (Gynecare, TVT Obturator System Ethicon, Inc. Sommerville, NJ, USA) was applied as per de Leval, inside-out approach [17]. For colposuspension, the cavum Retzii was entered by means of a Pfannenstiel incision, and 2 non-absorbable stitches were applied through the pubocervical fascia and vagina paraurethraly, at the point of urethro-vaginal junction (Gynecare, Nurolon Ethicon Inc. Sommerville, NJ, USA) approximately 2 cm from the middle line. Surgical procedures were indicated consecutively.
Post-operative follow-up was carried out 3 months, 1 year and 3 years after surgery. Apart from the urodynamic examination, the procedure was the same as before surgery. Objective cure rate was determined based on a negative stress test performed in supine and in standing positions during the gynecologic examination.
The women were divided into groups by the type of surgical procedure. Patients were not randomized, and surgical procedure was mainly based on surgeon decision and in some cases on patient preference.
Occurrence of different complications and their effects on QoL was monitored. For statistical processing, the symptoms monitored were divided into 4 groups as follows: 1) the first group was the OAB group; the second group included patients with recurrent stress incontinence; 2) the pain group included patients complaining of pain and dyspareunia; 3) the descent group included cystocele, rectocele; 4) the other symptoms group included leakage at sexual intercourse, protrusion, voiding difficulty or urinary tract infections. Re-operations due to failed primary operation or serious complications, or other re-operations as a result of descent, have been recorded.
Statistical analysis
Data were analyzed and processed using R freeware [18]; tests were carried out either non-parametrically (where a single period was monitored), or using mixed linear models (the effect of the factor being monitored on IQOL), at a 5% significance level. 95% confidence intervals were based on Wald’s test. Other processes used included Pearson’s chi-square test, Kruskall-Wallis chi-square test, regression curve, Bonferroni method to ascertain the effect of complications on IQOL, Wilcoxon test and Fisher’s exact test.
The major methodological limitation of the study is non-randomization of the surgical procedures.
Results
Complete data were obtained for 154 women (71.6% of the original group); 74.5% of women after TVT, 74.5% after TVT O procedure and 65.2% after BCS completed the study; 47 women were excluded from the study due to incomplete data, 12 women refused further cooperation, 1 woman died and 1 woman experienced recurrence of cervical cancer. Median follow-up was 3.1 years, SD ±0.56 years. The mean age of the group monitored was 54.7, SD ±9.9 years (range from 32 to 81) (Table 1). The women who underwent BCS were significantly younger than the women who underwent other procedures (p<0.001). No difference between individual operation groups as regards BMI and parity could be proven at a 5% significance level. The preoperative IQOL questionnaire did not differ for individual surgical procedures.
Table 1.
Basic characteristics of the study group.
| N (%)* | Mean age (SD) | Mean BMI (SD) | MUI Patient N(%) | |
|---|---|---|---|---|
| TVT | 76 (74.5%) | 57.2 (10.8) | 26.9 (4.7) | 20 (26.3%) |
| TVT O | 35 (74.5%) | 56.2 (9.3) | 28.3 (4.4) | 11 (31.4%) |
| BU | 43 (65.2%) | 49.1 (6.0)** | 26.7 (4.2) | 15 (34.9%) |
| Total | 154/215 (71.6%) | 54.7 (9.9) | 27.2 (4.5) | 46 (29.9%) |
Number of women who completed the study;
p<0.005 women from BU group are significantly younger.
TVT, TVT O – tension free vaginal tape, TVT obturator; BU – Burch colposuspension; BMI – body mass index; MUI – mixed urinary incontinence.
Objective cure rate (negative stress test) at the end of the follow-up period for the TVT group was 89.5%, 85.7% for TVT O, and 90.7% for BCS: differences were not statistically significant. The quality of life improved with surgery (46.9 to 89.1 with BCS, 45.2 to 88.2 with TVT and 47.0 to 88.3 with TVT O) and then remained statistically significantly improved against the pre-operative condition for the whole monitored period for all 3 procedures: p<0.001 (Table 2). Three years after surgery, differences between the procedures for IQOL were not statistically significant (p=0.051). Subjective satisfaction as per the total value ascertained in the IQOL questionnaire was 82.1 for TVT, 79.6 for TVT O and 88.7 for BCS.
Table 2.
Mean values of IQOL questionnaire during the study period.
| Before | 3M | 1Y | 3Y | |
|---|---|---|---|---|
| IQOL (SD) | IQOL (SD) | IQOL (SD) | IQOL (SD) | |
| TVT (76) | 45.2 (19.2) | 88.2 (16.1) | 87.9 (15.1) | 82.1 (19.5)** |
| TVT O (35) | 47.0 (16.8) | 88.3 (11.6) | 88.1 (11.5) | 79.6 (22.1)*,** |
| BU (43) | 46.9 (20.8) | 89. 1 (10.6) | 88.3 (14.6) | 88.7 (14.9)*,** |
| SUI (108) | 46.9 (19.1) | 89.0 (13.5) | 89.4 (13.2)# | 85.5 (17.9)## |
| MUI (46) | 44.1 (18.9) | 87.4 (14.3) | 84.8 (15.8)# | 78.4 (21.4)## |
Before – before surgery; 3M – three months after surgery; 1 Y – one year after surgery; 3Y –three years after surgery.
p<0.001 the impact of anti-incontinent surgery is statistically significant in every examination after surgery during whole monitored period.
TVT, TVT O – tension free vaginal tapes; BU – Burch colposuspension; SUI – stress urinary incontinence; MUI – mixed urinary incontinence.
p=0.006 effect of TVT O and BU on IQOL;
Kruskal Wallis p=0.051 the difference only just fails to be statistically significant;
Wilcoxon test p=0.03 the difference of IQOL between MUI and SUI is significant;
Wilcoxon test p=0.032 the difference of IQOL between MUI and SUI is significant.
the difference between controls is demonstrable.
In the long-term, the QoL remain stable after BCS procedure, but after TVT and TVT O it declined (Figure 1). Only after TVT O was the decline statistically significant compared to BCS (p=0.006). The initial difference grew by 3.4 points each year after the operation (95% confidence interval is 1.0 to 5.9).
Figure 1.
Post- operative trend of QoL after TVT, TVT O and Burch colposuspension. Error bars of IQOL in monitored period (average values and standard errors).
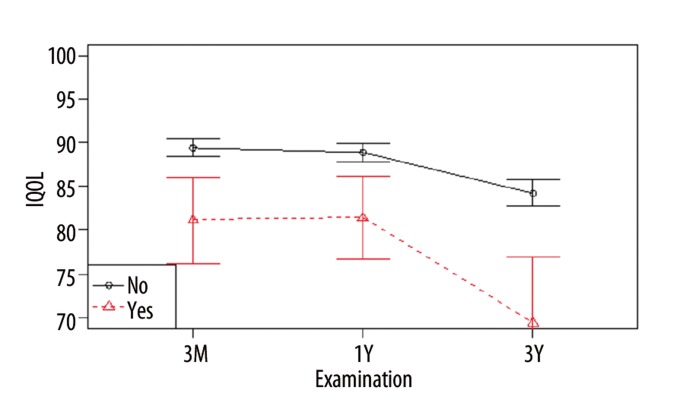
The IQOL for women with post-operative complications has a clear descending tendency (Figure 2). This interaction is proved by the test in the mixed effects model (p=0.013). The effect of the complications is highly significant (p<0.001). The complications do not occur equally over the monitored period (Table 3). If we monitor individual complications and IQOL, the graph analysis displayed in Figures 3–5 indicates a significant effect for OAB, recurring stress incontinence and other complications. However, OAB is the only complication with statistical significance (p<0.001). Occurrence of complications does not depend on the type of operation (chi square 2.04, p=0.36). All symptoms and complications that were monitored are depicted in Table 4.
Figure 2.
Comparison of QoL trend after surgery in women with or without any complications. Error bars of IQOL in monitored period (average values and standard errors).
Table 3.
Average values of IQOL questionnaire after surgery in patient with complications.
| Complications | 3M | 1Y | 3Y | |||
|---|---|---|---|---|---|---|
| N (%) | IQOL (SD) | N (%) | IQOL (SD) | N (%) | IQOL (SD) | |
| Without any complication | 69 (44.8%) | 92.3 (12.0) | 70 (45.5%) | 92.5 (10.0) | 69 (44.8%) | 92.3 (10.1) |
| With any complication | 85 (55.2%) | 85.4 (14.3) | 84 (54.5%) | 84.3 (16.0) | 85 (55.2%) | 76.1 (21.7) |
| OAB* | 55 (35.7%) | 83.4 (14.6) | 50 (32.5%) | 81.6 (18.2) | 65 (42.2%) | 73.2 (22.2) |
| Recurrence of SUI | 15 (9.7%) | 86.7 (14.4) | 16 (10.4%) | 83.6 (14.7) | 17 (11.0%) | 75.5 (18.1) |
| Pain | 8 (5.2%) | 87.8 (8.3) | 8 (5.2%) | 91.1 (8.9) | 6 (3.9%) | 91.3 (9.7) |
| Prolapse | 21 (13.6%) | 83.2 (12.7) | 24 (15.6%) | 86.6 (10.9) | 14 (9.1%) | 83.6 (19.4) |
| Other complications | 18 (11.7%) | 81.1 (20.8) | 17 (11.0%) | 81.4 (19.3) | 9 (5.8%) | 69.3 (23.7) |
SUI – stress urinary incontinence; 3M – three months after surgery; 1 Y – one year after surgery; 3Y –three years after surgery.
Other complication: leakage at sexual intercourse, protrusion, voiding difficulty or urinary tract infections.
Including of symptoms urgency, urgency de novo, frequency, nocturia, and UUI.
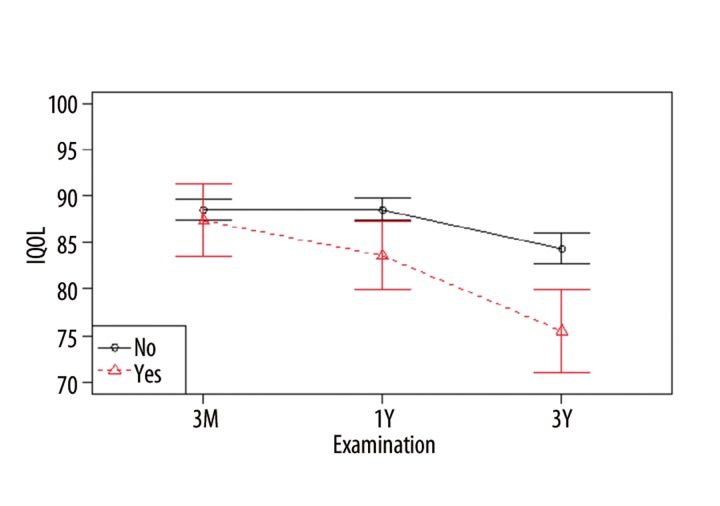
Figure 3.
Comparison of QoL trend after surgery in women with or without complication OAB. Error bars of IQOL in monitored period (average values and standard errors).
Figure 5.
Comparison of QoL trend after surgery in women with or without complications in group others symptoms included leakage at sexual intercourse, protrusion, voiding difficulty or urinary tract infections. Error bars of IQOL in monitored period (average values and standard errors).
Table 4.
Summary of late postoperative complications after TVT, TVT O and Burch colposuspension in the study period.
| 3M | 1Y | 3Y | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All N (%) | TVT N (%) | TVT 0 N (%) | BU N (%) | All N (%) | TVT N (%) | TVT O N (%) | BU N (%) | All N (%) | TVT N (%) | TVT O (%) | BU N (%) | |
| OAB | 55 (35.7%) | 18 (23.7%) | 19 (54.3%) | 18 (41.9%) | 50 (32.5%) | 23 (30.3%) | 13 (37.1%) | 14 (32.6%) | 65 (42.2%) | 31 (40.8%) | 16 (45.7%) | 18 (41.9%) |
| Recurrent SUI | 15 (9.7%) | 8 (10.5%) | 5 (14.3%) | 2 (4.7%) | 16 (10.4%) | 9 (11.8%) | 4 (11.4%) | 3 (7.0%) | 17 (11%) | 8 (10.5%) | 5 (14.3%) | 4 (9.3%) |
| Tape protrusion | 5 (3.2%) | 4 (5.3%) | 1 (2.9%) | 0 | 6 (3.9%) | 5 (6.6%) | 0 | 1 (2.3%) | 5 (3.2%) | 2 (2.6%) | 3 (8.6%) | 0 |
| Dyspareunia | 7 (4.5%) | 4 (5.3%) | 1 (2.9%) | 2 (4.7%) | 5 (3.2%) | 4 (5.3%) | 0 | 1 (2.3%) | 5 (3.2%) | 4 (5.3%) | 1 (2.9%) | 0 |
| Rectocele | 14 (9.1%) | 4 (5.3%) | 3 (8.6%) | 7 (16.3%) | 17 (11%) | 9 (11.8%) | 2 (5.7%) | 6 (14.0%) | 12 (7.8%) | 5 (6.6%) | 3 (8.6%) | 4 (9.3%) |
| Cystocele | 11 (7.1%) | 1 (1.3%) | 1 (2.9%) | 9 (20.9%) | 12 (7.8%) | 5 (6.6%) | 0 | 7 (16.3%) | 9 (5.8%) | 3 (3.9%) | 1 (2.9%) | 5 (11.6%) |
| UUI | 3 (1.9%) | 1 (1.3%) | 1 (2.9%) | 1 (2.3%) | 9 (5.8%) | 5 (6.6%) | 0 | 4 (9.3%) | 11 (7.1%) | 5 (6.6%) | 5 (14.3%) | 1 (2.3%) |
| Urinary tract infection | 8 (5.2%) | 4 (5.3%) | 3 (8.6%) | 1 (2.3%) | 9 (5.8%) | 5 (6.6%) | 1 (2.9%) | 3 (7.0%) | 4 (2.6%) | 2 (2.6%) | 1 (2.9%) | 1 (2.3%) |
Preoperatively, 29.9% of women suffered from mixed incontinence. OAB symptoms for these patients dropped to 56.5%, 45.7% and 56.5% at 3 months, 1 year and 3 years, respectively, after the procedure. Overall prevalence of OAB symptoms after procedure at 3 months was 35.7%, at 1 year 32.5%, and at the end of the survey 42.2% (Table 4). De novo anticholinergic use was postoperatively noted in 5 patients (4.6%) 3 months after surgery, 10 patients 1 year afterwards (9.3%), and 16 patients (14.8%) at the end of survey. The relatively high prevalence of OAB, which is uncommon, is due to registration of every complaint of OAB in the urinary diary. Most of these OAB did not influence the QoL and were not obligatory. The low rate of pharmacological therapy suggests an underestimation of OAB symptoms after surgery. Most OAB, such as post-operative inflammation of the urinary bladder, are solved by the physicians.
Discussion
Anti-incontinence operations significantly improve quality of life. The quality of life remained significantly improved against the pre-operative condition for the whole monitored period for all 3 procedures. Objective cure rate and subjective satisfaction are comparable with other published studies [13,19–24]. In the long-term after the operation, colposuspension was rated best, both subjectively and objectively. The IQOL deterioration in the TVT O group was more demonstrable than in the BCS group. If we had used a more simplified evaluation, with terms such as “cured”, “improvement” and “failure”, it would have been impossible to find any differences between the procedures. However, while the values of IQOL among groups TVT, TVT O and BCS were not statistically significant at the end of the survey, there were differences in deterioration development trends of QoL.
Some of the women who underwent Burch colposuspension also had concomitant surgery for abdominal hysterectomy, which may explain the difference in age compared to women after the TVT procedure. This fact alone, however, cannot explain the differences in the QoL after surgery. The monitoring of QoL after surgery in the long-term is important because de novo symptoms and complications vary over time.
We noted the effect of complications on the quality of life in our study. However, OAB is the only complication that statistically significantly influences the QoL. Occurrence of other complications is too low to obtain statistically significant differences. Compared to previously published studies, the prevalence of OAB was similar [20–24].
We agree that preexistent OAB does not negatively affect postoperative results of anti-incontinence operations [24,25]. Unlike other studies [26–28], before surgery we did not confirm statistically significantly worse quality of life for women with mixed incontinence compared to those with stress urinary incontinence. This may be due to the fact then we indicated women for the operation with predominant stress urinary incontinence; patients with predominant urgency incontinence were excluded. For patients with mixed type of incontinence, the operation has a positive effect on the urgency component [10].
Due to the low prevalence of groin or vaginal pain, tape protrusion, dyspareunia, voiding and postmicturition symptoms, it was impossible to prove a statistically significant effect on the IQOL. We were also unable to assess the change in the quality of life for re-operations, due to the small number of cases. The occurrence of complications did not depend on the type of surgical procedure.
Further long-term monitoring of the development trends in the success rate of anti-incontinence operations is needed to take into account the occurrence of complications and quality of life, as well as an overall assessment of the success rate of the new surgical procedures [29]. It is important to focus not only on the frequency of individual symptoms, but also on their development over time. The occurrence of complications shows a dynamic development over time, and its effect on the IQOL after the operation is significant.
The main limitation of this study is the non-randomization of the type of surgical procedure. Another issue is the lack of studies dealing with long-term follow-up of the quality of life after anti-incontinence operations as their main objective. The situation is further complicated by the number of different questionnaires, where use of a specific type of HRQoL (Health Related Quality of Life) questionnaire is not directed. This means that studies are often not comparable because they use different HRQoL questionnaires and methodology.
Conclusions
Anti-incontinence operations significantly improve quality of life in the long-term follow-up.
The resulting effect of the 3 monitored operations is comparable. We observed constantly high subjective satisfaction for Burch colposuspension, though less with TVT and TVTO.
Figure 4.
Comparison of QoL trend after surgery in women with or without complication recurrent SUI. Error bars of IQOL in monitored period (average values and standard errors).
Footnotes
Source of support: This work was supported by the Grant Agency of the Ministry of Health of the Czech Republic, grant NS 105 86-3/2009
References
- 1.Abrams P, Cardozo L, Magnus Fall, et al. The standardization of terminology of lower urinary tract function: Report from the standardization sub-committee of the ICS. Neurol Urodyn. 2002;21:167–78. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2010;21:5–26. doi: 10.1007/s00192-009-0976-9. [DOI] [PubMed] [Google Scholar]
- 3.Swithinban L, Abrams P. Lower urinary tracts symptoms in community dwelling women. BJU Int. 2002;88:18–22. doi: 10.1111/j.1464-410x.2001.00114.x. [DOI] [PubMed] [Google Scholar]
- 4.Alcalay M, Monga A, Stanton SL. Burch colposuspension: a 10–20 year follow up. Br J Obstet Gynaecol. 1995;102:740–45. doi: 10.1111/j.1471-0528.1995.tb11434.x. [DOI] [PubMed] [Google Scholar]
- 5.Lapitan MCM, Cody JD, Grant A. Open Retropubic Colposuspension for Urinary Incontinence in Women: A short version Cochrane Rewiew. Neurol Urodyn. 2009;28:472–80. doi: 10.1002/nau.20780. [DOI] [PubMed] [Google Scholar]
- 6.Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999;106:345–50. doi: 10.1111/j.1471-0528.1999.tb08272.x. [DOI] [PubMed] [Google Scholar]
- 7.Nilsson CG, Kuuva N, Falconer C, et al. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S5–8. doi: 10.1007/s001920170003. [DOI] [PubMed] [Google Scholar]
- 8.Nilsson C, Falconer C, Rezapour M. Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004;104:1259–62. doi: 10.1097/01.AOG.0000146639.62563.e5. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1043–47. doi: 10.1007/s00192-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 10.Novara G, Ficarra V, Boscolo-Berto R, et al. Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007;52:663–78. doi: 10.1016/j.eururo.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1043–47. doi: 10.1007/s00192-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 12.Dietz HP, Wilson PD. Colposuspension success and failure: A long-term objective follow up study. Int Urogyn J. 2000;11:346–51. doi: 10.1007/s001920070004. [DOI] [PubMed] [Google Scholar]
- 13.Ward KL, Hilton P UK a Ireland TVT group. A prospective multicentre randomized trial of TVT and colposuspension for primary urodynamic stress inkontinence: two years follow up. Am J Obst Gynecol. 2004;190:324–31. doi: 10.1016/j.ajog.2003.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Patrick DL, Martin M, Bushnell DM, et al. Quality of life of women with urinary incontinence: Further development of the incontinence quality of life instrument (I-QOL) Urology. 1999;53:71–76. doi: 10.1016/s0090-4295(98)00454-3. [DOI] [PubMed] [Google Scholar]
- 15.Schafer W, Abrams P, Liao L, et al. Good Urodynamic Practis: Uroflowmetry, Filling Cystometry, and Pressure-Flow Studies. Neurolurol Urodyn. 2002;21:75–82. doi: 10.1002/nau.10066. [DOI] [PubMed] [Google Scholar]
- 16.Bø K, Brubaker LP, DeLancey JO, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 17.de Leval J. Novel surgical technice for treatment of female stress urinary inkontinence: transobturator vaginal tape incide out. Eur Urol. 2003;44:724–30. doi: 10.1016/j.eururo.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 18.R-foundation T. R, a language and enviroment for statistical computing. Retrieved 12 December 2009, from http://www.r-project.org.
- 19.Holmgren C, Nilsson S, Lanner L, Hellberg D. Frequency of de novo urgency in 463 women who had undergone the tension-free vaginal tape (TVT) procedure for genuine stress urinary incontinencw - a long-term follow-up. Eur J Obstet Gynecol Reprod Biol. 2007;132:121–25. doi: 10.1016/j.ejogrb.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Latthe PM. Review of transobturatoe and retropubic tape procedures for stress urinary incontinence. Curr Opinion in Obst and Gyn. 2008;20:331–36. doi: 10.1097/GCO.0b013e3283073a7f. [DOI] [PubMed] [Google Scholar]
- 21.Laurikainen E, Valpas A, Kivela A, et al. Retropubic Compared With Transobturator Tape Replacement in Treatment of Urinary Incontinence. Obst and Gynecol. 2007;109:4–11. doi: 10.1097/01.AOG.0000249607.82768.a1. [DOI] [PubMed] [Google Scholar]
- 22.Novara G, Galfano A, Boscolo-Berto R, et al. Complication rate s of tension free midurethral slings in the treatment of female stress incontinence: a systematic rewiew and metaanalysis of randomized controlled trials comparing tension free midurethral tapes to other surgigal procedures and different device. Eur Urol. 2008;53:288–308. doi: 10.1016/j.eururo.2007.10.073. [DOI] [PubMed] [Google Scholar]
- 23.Porena M, Constantini E, Frea B, et al. Tension-Free Vaginal Tape versus Transobturator tape as surgery for stress urinary incontinence: Results of a multicentre randomised trial. Eur Urol. 2007;52:1481–91. doi: 10.1016/j.eururo.2007.04.059. [DOI] [PubMed] [Google Scholar]
- 24.Rinne K, Laurikainen E, Kivela A, et al. A randomized trial comparing TVT with TVT O: 12-month results. Int Urogynecol J Pelv Floor Dysf. 2008;19:1049–54. doi: 10.1007/s00192-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 25.Segal JL, Vassallo B, Kleeman S, et al. Prevalence of persistent and de novo overactive bladder symptoms after the tension-free vaginal tape. Obstet Gynecol. 2004;104:1263–69. doi: 10.1097/01.AOG.0000147596.44421.72. [DOI] [PubMed] [Google Scholar]
- 26.Swati J, Jones G, Radley S, Farkas A. Factor influencing outcome followin the tension-free vaginal tape (TVT) Eur JObst Gyn Reprod Biol. 2009;144:85–87. doi: 10.1016/j.ejogrb.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Haessler AL, Nguyen JN, Bhatia NN. Impact of urodynamic based incontinence diagnosis on quality of life in women. Neurol Urodyn. 2009;28:183–87. doi: 10.1002/nau.20637. [DOI] [PubMed] [Google Scholar]
- 28.Frick AC, Huang AJ, Van den Eeden SK, et al. Mixed urinary incontinence: greater impact on quality of life. J Urol. 2009;182:596–600. doi: 10.1016/j.juro.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jenicek M. Clinical case reports and case series research in evaluating surgery. Part I. The context: General aspects of evaluation applied to surgery. Med Sci Monit. 2008;14(9):RA133–43. [PubMed] [Google Scholar]