History and clinical signs
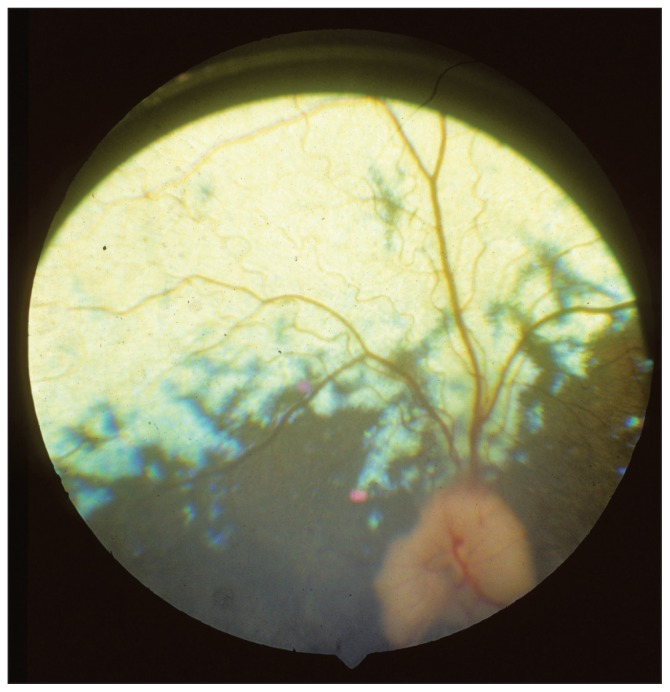
A 7-year-old female boxer dog was examined by the ophthalmology service at the Western College of Veterinary Medicine with a history of acute onset blindness of approximately 1 month. Vaccinations for distemper, parvo, and rabies viruses were current. Our neuro-ophthalmic examination revealed that bilateral mydriasis and the pupillary reflexes and menace responses were absent; palpebral and oculocephalic reflexes were present bilaterally. Photopic and scotopic maze testing was completed and the dog was unable to navigate the obstacle course. Schirmer tear tests (Schirmer Tear Test Strips; Alcon Canada, Mississauga, Ontario) values were approximately 20 mm/min bilaterally. The intraocular pressures, estimated with a rebound tonometer (Tonovet; Tiolat Oy, Helsinki, Finland), were 16 and 17 mmHg in the right and left eye, respectively. Biomicroscopic (Osram 64222; Carl Zeiss Canada, Don Mills, Ontario) and indirect ophthalmoscopic (Heine Omega 200; Heine Instruments Canada, Kitchener, Ontario) examinations were completed and no significant abnormalities could be detected. Corneal dystrophy was present; however, it was mild and had been present for several years and was not progressing. A routine photopic electroretinogram was completed and the a-waves were 35 microvolts and the b-waves were approximately 115 microvolts; these values are within normal reference ranges for a dog of this age (Figure 1).
Figure 1.
A photograph of the fundus of the left eye. The right fundus was similar in appearance.
What are your clinical diagnoses, differential diagnoses, diagnostic plan, and prognosis?
Our clinical diagnoses were blindness, and afferent pupillary defects which are consistent with optic nerve and optic chiasmal disorders including central nervous system neoplasms and inflammatory conditions including optic neuritis. A physical examination, complete blood cell count, serum biochemical profile, and urinalysis were completed; no significant abnormalities were detected. Routine sedation and general anesthesia were advised and contrast enhanced computerized tomography (CT scan) with iohexol, (Omnipaque; GE Health Care Canada, Mississauga, Ontario) of the cranium was done.
Discussion
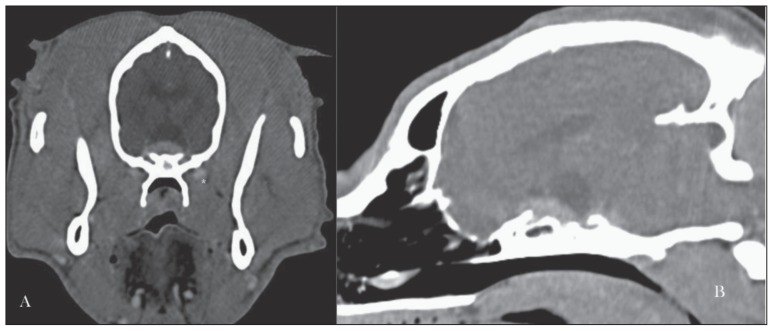
The CT images reveal a contrast enhancing extra axial tumor in the ventral brain which involves the optic chiasma and optic nerves (Figure 2). The tumor is creating mechanical obstruction of the third ventricle with secondary third and lateral ventricular enlargement. A dural tail sing (meningial enhancement) was not noted on the CT images. The appearance is most consistent with a neoplasm and meningioma, glioma, astrocytomas, and several metastatic neoplasms may be considered. The prognosis for this dog is guarded and external beam radiation was offered but declined. The owner declined further therapy and the dog is being managed conservatively.
Figure 2.
Computed tomography post-contrast transverse and saggital images of the cranium of a blind 7-year-old female boxer dog.
Neoplasms of the optic chiasmal neoplasia are a relatively uncommon cause of blindness in animals. However, its importance rises quickly in our differential diagnoses list when the electroretinogram and ophthalmoscopic examinations are within normal limits. These evaluations rule out intraocular disorders that commonly induce blindness including but not limited to cataracts, retinal detachments, and retinal degenerations. Sudden acquired retinal degeneration (SARD) is by far the most common cause of acute blindness in middle-aged dogs without clinically apparent intraocular lesions that could impair vision. SARD is confirmed by electroretinography which reveals no retinal activity. In this dog, the retinal electrical activity was within normal limits, which mandates sectional imaging of the optic nerves and chiasma to determine an etiologic diagnosis. The most common etiologies for these dogs are either optic chiasmal neoplasia or optic neuritis. These disorders can be differentiated by the sectional imaging manifestations. This dog manifested with a large tumor that was centered on the optic chiasma with extension down the optic nerves.
Unfortunately we were unable to confirm the type of neoplasm that invaded this optic nerve or attempt therapy such as external beam radiation. Optic nerve meningioma was considered one of the most likely primary neoplasms; however, many other primary and metastatic neoplasms are possible (1,2).
In conclusion, acute blindness in the absence of ophthalmoscopic detectable vision impairing lesions warrant an electroretinogram to confirm or negate SARD. When SARD has been ruled out, contrast enhanced sectional imaging (MRI or CT scans) is required to establish the diagnosis for afferent pupillary defects.
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Palmer AC, Malinnowski W, Barnett KC. Clinical signs including papilledema associated with brain tumours in twenty-one dogs. J Sm Anim Pract. 1974;15:359–386. doi: 10.1111/j.1748-5827.1974.tb06512.x. [DOI] [PubMed] [Google Scholar]
- 2.Mauldin EA, Deehr AJ, Hertzke D, Dubielzig RR. Canine orbital meningiomas: A review of 22 cases. Vet Ophthalmol. 2000;3:11–16. doi: 10.1111/j.1463-5224.2000.00087.x. [DOI] [PubMed] [Google Scholar]