Abstract
Home visits by trained personnel to patients undergoing home dialysis are required, but little is reported about the effectiveness of such home visits. We retrospectively reviewed home visits to 22 pediatric patients undergoing continuous cycling peritoneal dialysis (PD) at home. A trained dialysis nurse completed each home visit. An average of 1.5 pertinent dialysis findings and 1 pertinent medication finding was noted for each home visit to these patients. The interdisciplinary dialysis team reviewed the home visit findings and made specific recommendations after each home visit. In addition, the training process has been enhanced to incorporate visit findings for future home PD patients. Although not statistically significant in this small number of patients, peritonitis rates declined in the 6 months after initiation of the home visit program. The average cost for a dialysis nurse to complete a home visit is less than the cost of antibiotics for 1 episode of peritonitis. Home visits are valuable for improving clinical care in pediatric patients on home PD.
Keywords: Pediatric patients, home dialysis, adherence
Home peritoneal dialysis (PD), with the parent or the patient performing nightly dialysis treatment, is a common modality for children with end-stage renal disease, especially young children. Guidelines for European pediatric dialysis providers have included home visits before the initiation of PD (1). The Centers for Medicare and Medicaid Services guidelines require nephrology centers providing home dialysis to perform home visits, although specific methods for the home visits are not detailed, and home visits have been completed by fewer than 80% of U.S. dialysis programs completing a recent survey (2). Further, the literature contains few reports describing the usefulness of home visits in the care of children on PD (3). Here, we retrospectively review the outcomes of our recent home visits to 22 children on home continuous cycling PD (CCPD).
METHODS
To meet the Centers for Medicare and Medicaid Services guidelines, and after approval by the hospital nursing and legal administration, we began, in 2009, a home visit program for our pediatric CCPD patients. Between September and November 2009, 22 patients on home CCPD received their first home visit by a trained dialysis nurse. The home visit record for each visit completed by the dialysis nurse was retrospectively reviewed. This retrospective review was approved by the Institutional Review Board of the University of Arkansas for Medical Sciences.
Patient age, number of months on PD before the visit, number of episodes of peritonitis in the year before the home visit, and number of miles traveled by the nurse for each home visit were recorded. For none of the 22 patients was a home visit completed before home CCPD commenced. However, extensive training to perform PD at home had been completed for each family in the dialysis unit before the patient started on home CCPD, and the required equipment—including dialysis machine, weight scale, and thermometer—had been supplied to the family. In the United States, the responsibility for delivery of the supplies and dialysis machine for PD at home, and for the maintenance of the dialysis machine, is the responsibility of the supply company. Dialysis record sheets had also been provided to each family, and the dialysis nurse attempted to review those sheets with the family at each clinic visit. Once home PD was started, the primary dialysis nurse contacted the family by telephone at least every 2 weeks (more often if contacted by the family or if concerns arose about issues such as medication changes, laboratory values, and the scheduling of follow-up visits).
Before the home visit, the primary dialysis nurse for each patient recorded the dialysis prescription and the medications prescribed, which were to be evaluated at the home visit. At the dialysis clinic before the home visit, the patient and the family were informed about the home visit, and consent was obtained from the patient or guardian for the home visit. Additionally, the dialysis nurse scheduled the specific time for the visit and received specific directions to the home from the family. No patient or family refused a home visit.
At each home visit, the type of surrounding community was recorded. A community was defined as “urban” if the most recently recorded population was 2500 or more people. Families living in urban areas were further divided into those living in a “city” or a “small town” (based on the U.S. Census definition). The type of living quarters—single-family home, apartment, or trailer—was noted for each home visit.
Each home environment was evaluated for presence in the home of a properly working and clean dialysis machine, thermometer, smoke detector, and fire extinguisher. The room in which the nightly CCPD was performed was evaluated, and for each patient who had experienced an episode of peritonitis in the preceding year, the PD set-up by either the parent or the patient was observed by the dialysis nurse. The space for hand washing and disposal of fluids after completion of CCPD was also observed. The place for storage of dialysis supplies and the adequacy of the dialysis supplies available were noted, but a specific inventory of supplies was not done.
At each home visit, the dialysis nurse reviewed the medications for the patient, noting the presence of those medications in the home, correctness of the dose, date of prescription, and proper storage. In addition, the nurse reviewed stored intraperitoneal antibiotics prescribed to be used if peritonitis developed and the instructions to the family for the use of those antibiotics.
The home visit form was completed by the dialysis nurse at the end of the home visit, and recommendations for the home environment were communicated to the family, nephrology social worker, and primary nephrologist. The interdisciplinary team then made recommendations for follow-up based on the initial home visit.
RESULTS
The patients on CCPD receiving a home visit ranged in age from 7 months to 19 years (mean ± standard deviation: 14.5 ± 4.5 years). They had been on home CCPD for 2 - 60 months (mean: 21 ± 17 months) before the home visit. Of the 22 patients, 8 had experienced an episode of peritonitis within the preceding year, and thus dialysis set-up was observed for those patients during the home visit. In the preceding year, 1 patient had experienced 3 episodes of peritonitis; 5 had experienced 2 episodes each; and 2 patients had experienced 1 episode each.
The dialysis nurse performing the home visits traveled an average of 111 ± 78 miles one-way for the home visit (range: 6 - 300 miles). An average of 2 hours was spent performing each home visit, with an additional 30 minutes required if dialysis set-up had to be observed. For 4 of the 22 patients, Spanish was the primary language in the home, and the dialysis nurse communicated with the family during the home visit through a telephone connection to certified Spanish interpreter housed at the hospital. Based on the 2 hours of nursing time required for each home visit (plus 30 minutes for each patient whose CCPD set-up required monitoring), nursing travel time, and $0.52 per mile for travel, the estimated mean cost for each home visit was $362.71, not including pre-visit preparations and post-visit evaluation and follow-up.
Of the study patients, 18 lived in urban areas, and 4 lived in rural areas. Of the patients living in urban areas, 8 lived in cities, and 10 lived in small towns. Living quarters were single family houses for 13 patients, trailers for 3, apartments for 5, and a college dormitory room for 1.
During the home visit, smoke detectors were lacking in 6 of the 22 living quarters, and fire extinguishers were lacking in 16. Thermometers were lacking in 9 of the 22 living quarters despite the fact that a thermometer had been provided to each family at dialysis initiation. Fever being a sign of peritonitis or other illness, a thermometer in the home is essential for any patient on home PD. In addition, no working scale was present in 1 home despite the need to determine weight so that dialysis fluid choices can be made nightly; the dialysis supplier was contacted to provide a working scale for that family. For 2 patients, no dialysis record sheets were present in the living quarters despite the requirement to record weight, blood pressure, and dialysis fluid choices daily, and despite the attempt by the dialysis nurse to review records at each clinic visit. Repeat instruction on the need to record dialysis information was given to each of those families (Table 1).
TABLE 1.
Deficiencies Noted During 22 Home Visits to Pediatric Peritoneal Dialysis Patients
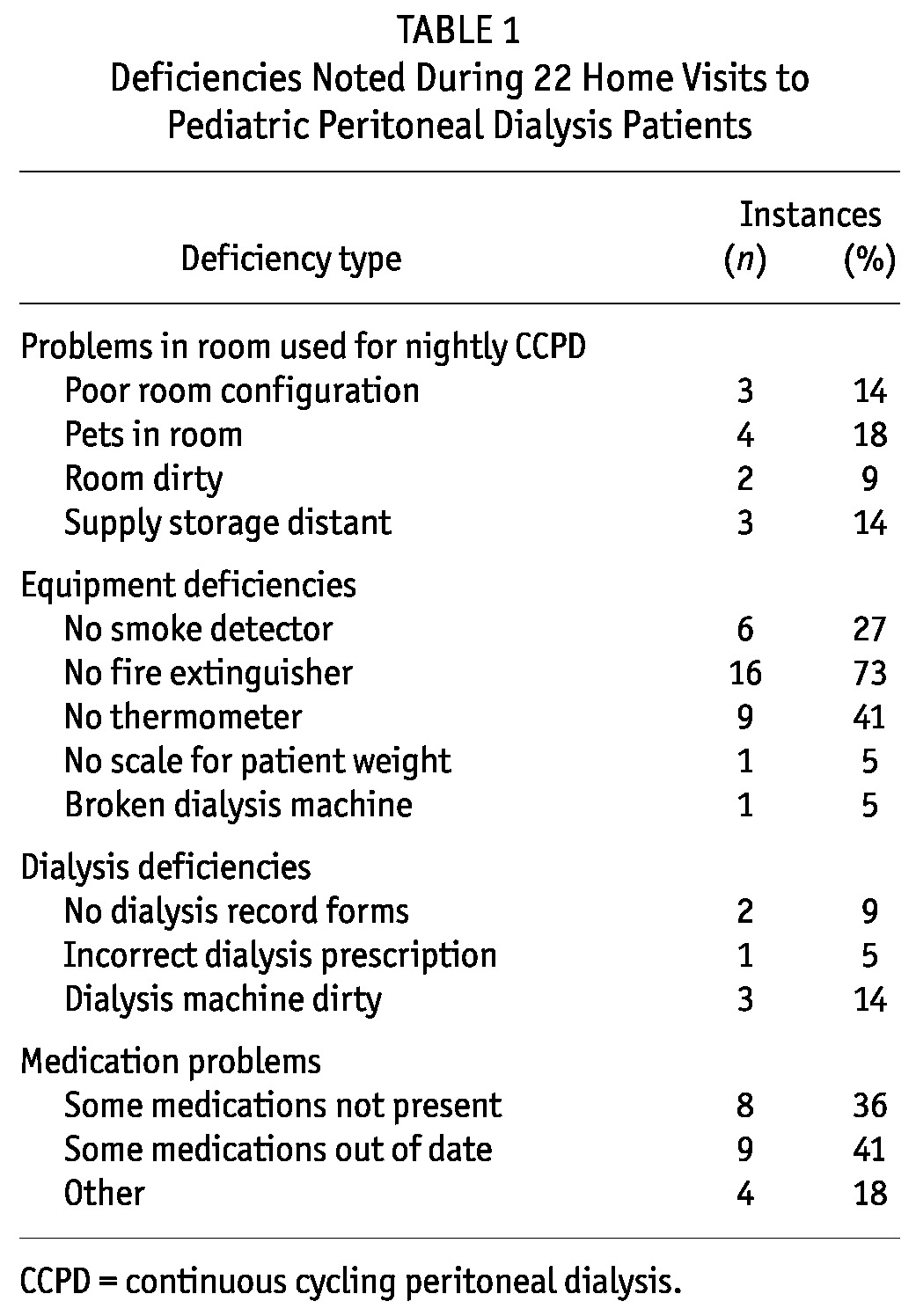
When the room used for nightly CCPD was observed, it was determined that reconfiguration of the room would improve dialysis efficiency in 3 homes. For example, in 1 home, the patient’s guardian was reaching over the patient to connect for nightly dialysis; this patient had experienced 3 recent episodes of peritonitis before the home visit; no episodes occurred after a change in the room configuration was accomplished at the home visit. In one of the other 2 homes, the dialysis machine was in a difficult-to-reach position, and in the other, no supplies for emergencies (such as masks or catheter caps) were available because all supplies were stored at a distant location.
The room for CCPD was noted to be dirty during 2 of the home visits, and pets were noted to be present in the room during dialysis on 4 visits. Cleaning of the room and removal of the pets from the room were prescribed in those situations. During 3 of the home visits, it was determined that CCPD was occasionally preformed in places other than the primary residence, usually the home of a close relative.
The dialysis machine itself was noted to be dirty in 3 homes; the families were instructed to clean the dirty machines. The dialysis machine was noted to be broken in 1 home; the patient was still completing CCPD with the broken machine and had not contacted the dialysis unit or the dialysis supplier about the problem. That dialysis equipment supplier was contacted to replace the broken machine. For 3 patients, storage of supplies was not in close proximity to the room in which dialysis was performed. At 1 home visit, the prescription in the dialysis machine was not as prescribed in the clinic. At 1 home visit, it was determined that, after nightly dialysis, the dialysate effluent was emptied into the rural backyard, where farm animals were present.
For 8 patients, at least some of the prescribed medications were not present in the home. In 9 of the home visits, some of the medications were out of date. For the patient living in the college dormitory, no refrigerator was available for storage of erythropoietin; access to a refrigerator for storage of erythropoietin was found during the home visit. For another patient, some of the medications were not stored in the dispensing bottle.
Although feedback from the families was not specifically sought, no family had complaints about the home visit, and at least 6 families had positive comments. These families particularly stated that ideas communicated by the dialysis nurse at the home visit about room configuration, supply storage, and fixing a broken dialysis machine were very helpful. One mother also commented that she was especially grateful that the home visit prompted her adolescent son to clean his room.
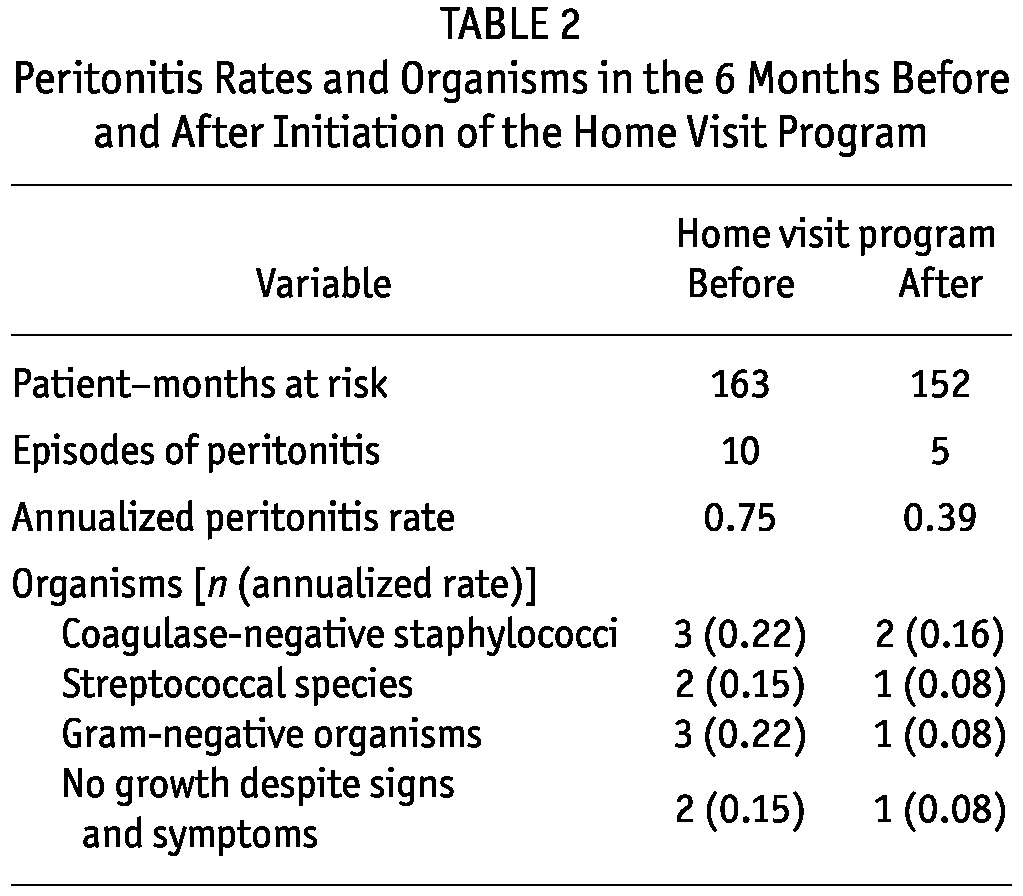
The peritonitis rate for our program in the 6 months before home visits were begun was 1 episode in 16.3 patient-months. In the 6 months after completion of the initial home visit, the peritonitis rate declined to 1 episode in 30.4 patient-months. Table 2 lists the annualized peritonitis rates and the organisms causing peritonitis in the 6 months before and after initiation of the home visit program. Poisson regression for the peritonitis rates between those time intervals showed that, in the 6 months after initiation of the home visits, patients developed peritonitis at a rate approximately 50% of the rate before the home visit program. However, that result was not statistically significant (incidence rate ratio: 0.53; standard error: 0.29; p = 0.25). At our center, the cost of 14 days of intraperitoneal antibiotics for 1 episode of peritonitis is $534.17 for the antibiotics alone. Thus, the average cost of a home visit was less than the cost of antibiotics for 1 episode of peritonitis.
TABLE 2.
Peritonitis Rates and Organisms in the 6 Months Before and After Initiation of the Home Visit Program
DISCUSSION
In the present study, we retrospectively evaluated home visits in 22 pediatric patients undergoing home CCPD. In our patients, an average of 1.5 pertinent dialysis findings and an average of 1 pertinent medication finding were uncovered per home visit. Peritonitis before the home visits could likely have been related to the room configuration for 1 patient and to a broken dialysis machine for another patient. Only in 2 home visits were no recommendations for change made.
In response to these home visit findings, our home training program has now been altered to discuss dialysis room configuration, dialysis supply storage, required cleaning of the dialysis room and equipment, and maintenance of the required equipment (for example, ensuring the presence of weight scale and thermometer while remaining on dialysis), and to further emphasize the importance of prescribed medications. Home visits soon after initiation of home CCPD have been continued, and follow-up home visits are planned for patients every 12 months, after episodes of peritonitis, or when other concerns arise at clinic visits. In an attempt to improve future peritonitis rates, the dialysis nurse will now evaluate the CCPD set-up during every home visit.
The Centers for Medicare and Medicaid Services requires dialysis centers in the United States providing home dialysis to conduct home visits, but no funding has been provided for those visits, and few data about the usefulness of home visits have been reported. In a survey of 670 American centers providing home PD, Bernardini and Dacko wrote that 78.4% of centers reported completing home visits and that no differences between centers making and not making home visits were observed with regard to the number of patients on home dialysis at the center, whether the center was urban or rural, and whether the center was university affiliated or not (2). Bernardini and Piraino also reported that two home visits 1 - 3 months apart in which dialysis supplies in the home were evaluated could provide a method of monitoring compliance with the dialysis prescription (4). Russo and colleagues reported that home visits in adult peritoneal dialysis patients were effective in discovering 25% partial compliance with drug therapy and 23% noncompliance with exchange protocol procedures (5). Nasso reported that a quality project, including creation of a home visit form, did not improve peritonitis rates; however, with further improvements, including development of a home visit protocol, peritonitis rates did improve (6). Ponferrada et al. noted that home visits to 36 patients resulted in an average of 10 pertinent observations and 4 recommendations for change per visit (7). Outcomes of home visits have also been reported in other countries, including India, Turkey, and Australia (8-10). Cuttell described a home nurse respite program for pediatric PD patients that began with funding from a charitable grant and continued because of positive parental response (3).
We report that home visits by a trained dialysis nurse to pediatric patients on home CCPD often uncover aspects of the home environment that may affect the clinical care of the patient. These concerning aspects of the home environment related to dialysis had not previously been uncovered during the intensive training provided by the dialysis nurse before home CCPD begins or during the frequent follow-up visits to the dialysis clinic. Previously, Farina noted that assessment of the home environment and compliance with the dialysis prescription were 2 advantages of home visits and that the time and costs of completing home visits are disadvantages (11). Although initiation of a home visit program may not be the sole reason, and although the change from one time period to the other was not statistically significant, we did note a decline in peritonitis rates after the home visit program for our small group of patients was started. We further note that our average cost for a home visit is less than the cost for antibiotic treatment of 1 episode of peritonitis. A home visit program for pediatric patients on CCPD may increase adherence with the prescribed dialysis prescription and medications, may lower the incidence of peritonitis, and may improve overall clinical care.
DISCLOSURES
No financial conflict of interest exists for any of the authors.
REFERENCES
- 1. Watson AR, Gartland C. on behalf of the European Paediatric Peritoneal Dialysis Working Group. Guidelines by an ad hoc European committee for elective chronic peritoneal dialysis in pediatric patients. Perit Dial Int 2001; 21:240–4 [PubMed] [Google Scholar]
- 2. Bernardini J, Dacko C. A survey of home visits at peritoneal dialysis centers in the United States. Perit Dial Int 1998; 18:528–31 [PubMed] [Google Scholar]
- 3. Cuttell K, Gartland C. Five years’ experience of a hospital-based home-care renal nursing service. Adv Perit Dial 1999; 15:258–61 [PubMed] [Google Scholar]
- 4. Bernardini J, Piraino B. Compliance in CAPD and CCPD patients as measured by supply inventories during home visits. Am J Kidney Dis 1998; 31:101–7 [DOI] [PubMed] [Google Scholar]
- 5. Russo R, Manili L, Tiraboschi G, Amar K, De Luca M, Alberghini E, et al. Patient re-training in peritoneal dialysis: why and when it is needed. Kidney Int Suppl 2006; (103):S127–32 [DOI] [PubMed] [Google Scholar]
- 6. Nasso L. Our peritonitis continuous quality improvement project: where there is a will there is a way. CANNT J 2006; 16:20–3 [PubMed] [Google Scholar]
- 7. Ponferrada L, Prowant BF, Schmidt LM, Burrows LM, Satalowich RJ, Bartelt C. Home visit effectiveness for peritoneal dialysis patients. ANNA J 1993; 20:333–6 [PubMed] [Google Scholar]
- 8. Nayak KS, Sinoj KA, Subhramanyam SV, Mary B, Rao NV. Our experience of home visits in city and rural areas. Perit Dial Int 2007; 27(Suppl 2):S27–31 [PubMed] [Google Scholar]
- 9. Ozturk S, Yucel L, Guvenc S, Ekiz S, Kazancioglu R. Assessing and training patients on peritoneal dialysis in their own homes can influence better practice. J Ren Care 2009; 35:141–6 [DOI] [PubMed] [Google Scholar]
- 10. Griffin D. Renal Home Support Scheme quality initiative. J Qual Clin Pract 1999; 19:179–81 [DOI] [PubMed] [Google Scholar]
- 11. Farina J. Peritoneal dialysis: a case for home visits. Nephrol Nurs J 2001; 28:423–8 [PubMed] [Google Scholar]


