Cerebral malaria, acute lung injury, severe anemia, and acute kidney injury (AKI) influence the outcome of severe malaria cases (1). Although a number of studies have dealt with the first three complications, only a few have described the renal complications in malaria, and scant data from India are available (2-4).
Malaria-associated AKI may occur as the sole complication or as one of multiple complications (5). Some patients may have nonoliguric AKI, and they usually have a better prognosis even without renal replacement therapy (RRT); others may need RRT.
Acute kidney injury is associated with increased morbidity and mortality in malaria (1-5). In the presence of AKI, the fatality of cerebral malaria triples to 45% from 15% (4,5). Prognosis can be greatly improved by the institution of RRT. However, there is no consensus in the literature on the best RRT modality in AKI—and especially whether hemodialysis (HD) or peritoneal dialysis (PD) should be used. There are concerns about the inadequacy of PD on the one hand, and the intermittency of HD with the potential for hemodynamic instability on the other. Use of continuous RRT is becoming more commonplace in critically ill patients with AKI. In a study from Vietnam, survival was lower in malaria patients treated with PD than in those treated with hemofiltration (6).
We retrospectively analyzed the case records of malaria patients with AKI who received some form of RRT. Permission was obtained from the local ethics committee.
METHODS
Ispat General Hospital is located in Rourkela, in the western part of Orissa in India. This postgraduate teaching hospital has 650 beds and round-the-clock facilities for biochemical, radiologic, and blood-banking services. Its several clinical units include critical care and nephrology. In this retrospective observational study, records of all the patients who underwent RRT for AKI because of infection with falciparum malaria were collected.
Indications for dialysis in patients with malarial AKI were any combination of
serum creatinine greater than 3 mg/dL and anuria or oliguria for more than 12 hours,
fluid overload in form of pulmonary edema,
severe acidosis (pH 7.2 or less),
uremic encephalopathy, and
hyperkalemia.
Peritoneal dialysis was performed in patients who were hemodynamically unstable (systolic blood pressure ≤ 80 mmHg) or in those on ventilatory support for acute respiratory distress syndrome associated with AKI (because the critical care unit of the hospital has no HD facility).
Procedure for PD: With all aseptic measures and local anesthesia, a state of artificial ascites was created by introducing 1.5 - 2 L PD fluid into peritoneal cavity through a 18G intracatheter needle placed about 2 cm below the umbilicus. The aim of this step was to avoid injury to the internal organs during introduction of the trocar.
Through a small incision at the same site, the trocar with PD catheter was introduced into the abdomen. The catheter was directed toward and placed into the right iliac fossa region. The PD catheter was then connected to the tubing. Outflow was tested, and the catheter was secured with a purse string suture. The wound was then properly dressed.
In each exchange, 2 L PD fluid was introduced into the abdomen with 10 minutes of inflow, 30 minutes of dwell, and 20 minutes of outflow. The negative or positive balance for each dwell was recorded, and 36 - 48 such exchanges were carried out for each patient.
Procedure for HD: Hemodialysis was carried out using a double-lumen hemodialysis catheter introduced by a subclavian, jugular, or femoral approach and connected with tubing to a newer-version HD machine (AK 200S: Gambro Lundia AB, Lund, Sweden). The blood flow rate was about 200 mL/min, and the (bicarbonate) dialysate flow rate was 400 - 500 mL/min. Ultrafiltration was performed for patients with fluid overload. The duration of hemodialysis was 3 hours daily.
RESULTS
Of 26 patients who underwent RRT (19 men, 7 women; age range: 16 to 46 years), 11 received HD, and 15 received manual PD (Table 1). The period of illness before hospitalization was 3 - 13 days. There was no difference between the groups in the median duration of sickness before attending the hospital (p = 0.574).
TABLE 1.
Renal Replacement Therapy in Malaria-Related Acute Kidney Injury
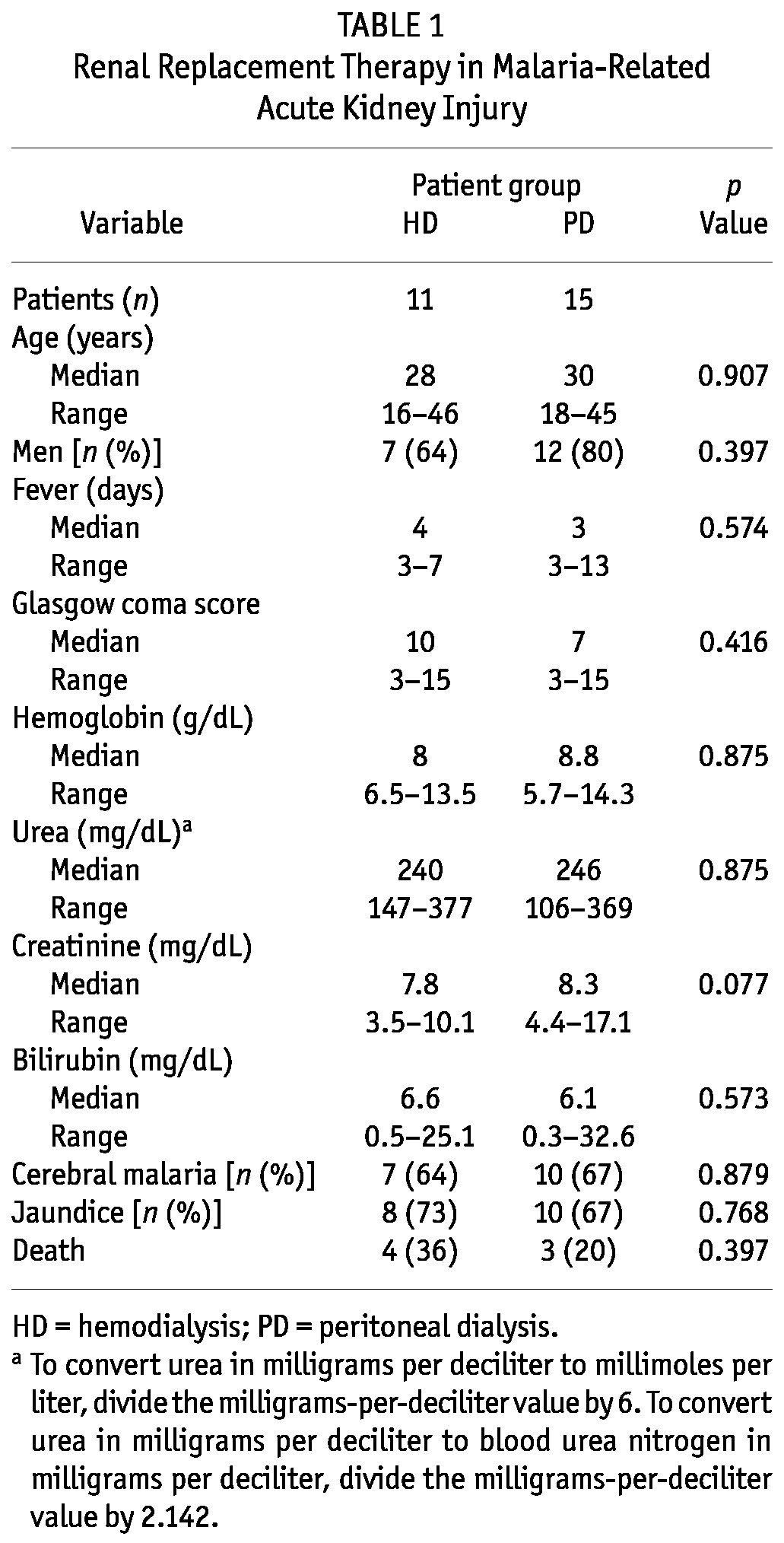
Cerebral malaria was present in 17 of the patients (65%), 10 in the PD group, and 7 in the HD group (p = 0.88). Jaundice was present in 18 (69%). Although anemia was observed in a few patients, severe anemia (hemoglobin < 5 g/dL) was not encountered. Blood urea ranged from 106 mg/dL to 377 mg/dL (reference value: 15 - 45 mg/dL), and serum creatinine was 3.5 - 17.1 mg/dL. Mortality was higher among patients who underwent HD (36% vs 20% in PD group, p = 0.397 by Fisher exact test). We observed no differences in age, sex, hemoglobin, urea, or creatinine between patients who survived and those who expired. Cerebral malaria was present in all patients who died (7 of 7), but in just 53% of those who recovered (10 of 19, p < 0.02). Multiple complications—specifically, jaundice and cerebral malaria—were more frequent in malaria patients in presence of AKI than in its absence (77% vs 19%, p < 0.001, and 59% vs 11%, p < 0.001, respectively). In a previous report, we observed that the concurrent presence of cerebral malaria and AKI increased mortality (2).
DISCUSSION AND CONCLUSIONS
Various therapeutic options are available for AKI. From a technical viewpoint, PD is the simplest form of RRT. Patients who are hemodynamically stable can be managed with intermittent HD, whereby relatively short (3- to 4-hour) dialysis sessions are performed daily or every other day. Patients who are hemodynamically unstable are best managed using PD or continuous RRT.
In many parts of the world, PD is widely used for RRT in AKI despite concerns about its inadequacy. But PD has been replaced in recent years by HD and, most recently, by continuous venovenous therapies.
In a prospective study conducted in a tertiary-care university hospital in Brazil (7), 120 patients with acute tubular necrosis were assigned to receive either continuous PD or daily HD. The primary endpoint was hospital survival rate; secondary endpoints were renal function recovery and metabolic, acid-base, and fluid control. Of the 120 patients, 60 were treated with continuous PD (group 1), and 60, with daily HD (group 2). The two groups were similar at the start of RRT with respect to age, sex, sepsis, shock, severity of AKI, Acute Tubular Necrosis Individual Severity Score, pre-dialysis blood urea nitrogen, and creatinine. They were also similar in metabolic and acid-base control. Despite the use of different dialysis methods and doses, the survival rate did not differ between the groups (58% in group 1 vs 52% in group 2). The authors concluded that continuous PD can be considered for use as a RRT modality in AKI.
Among the several advantages that PD offers, its relatively low cost is probably the most significant. Unlike the saw-tooth of HD treatment, PD delivers steady-state treatment that avoids wide fluctuation in plasma volume and solutes. Other advantages include technical simplicity, lack of a need for anticoagulation or placement of a central venous catheter, and excellent tolerance in hemodynamically unstable patients. Peritoneal dialysis also requires less expertise than HD, and nursing staff, technicians, and doctors can easily be trained in the technique. Despite certain limitations, PD still has much potential and can be successfully used in district hospitals and less accessible areas.
Although our study is smaller and retrospective in nature, its findings differ from those reported from Vietnam and should encourage resource-poor countries to undertake large prospective studies to evaluate the efficacy of PD in AKI. Several logistics problems are associated with HD, such as travel to a specialized center and wait times. There may be an inordinate delay in providing HD, but PD can be started immediately.
In situations resembling that in rural India, malaria is a major problem. The illness is often associated with AKI, which adversely influences outcomes whether the AKI is present alone or in combination with other complications. The prognosis can be greatly improved by timely institution of RRT. Peritoneal dialysis is a viable option to be considered and instituted early in the disease course. In our patients, PD improved survival to 36% from 20% and could be considered the first choice in this population. The present study, being retrospective, has some limitations. Still, in countries such as India, PD should not be ignored and must be instituted as early as possible.
DISCLOSURES
The authors have no financial conflicts of interest to declare.
Acknowledgments
We express our sincere thanks to the staff of the critical care unit and nephrology, including Dr. Rajya B. Pattnaik, Dr. Sanjib Mohanty, and Dr. Uma Devi for their support.
REFERENCES
- 1. Mishra SK, Panigrahi P, Mishra R, Mohanty S. Prediction of outcome in adults with severe falciparum malaria: a new scoring system. Malar J 2007; 6:24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mishra SK, Mahanta KC, Mohanty S. Malaria associated acute renal failure—experience from Rourkela, eastern India. J Indian Med Assoc 2008; 106:640–42,654 [PubMed] [Google Scholar]
- 3. Mishra SK, Das BS. Malaria and acute kidney injury. Semin Nephrol 2008; 28:395–408 [DOI] [PubMed] [Google Scholar]
- 4. Mishra SK, Dietz K, Mohanty S, Pati SS. Influence of acute renal failure in patients with cerebral malaria—a hospital-based study from India. Trop Doct 2007; 37:103–4 [DOI] [PubMed] [Google Scholar]
- 5. Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg 2000; 94(Suppl 1):S1–90 [PubMed] [Google Scholar]
- 6. Phu NH, Hien TT, Mai NT, Chau TT, Chuong LV, Loc PP, et al. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Eng J Med 2002; 347:895–902 [DOI] [PubMed] [Google Scholar]
- 7. Gabriel DP, Caramori JT, Martin LC, Barretti P, Balbi AL. Continuous peritoneal dialysis compared with daily hemodialysis in patients with acute kidney injury. Perit Dial Int 2009; 29(Suppl 2):S62–71 [PubMed] [Google Scholar]


