Abstract
Although behavioral couples therapy (BCT) has considerable support in treating alcohol use disorder (AUD), studies have not examined BCT for dual problem couples in which both partners have current AUD. This study compared outcomes after BCT for dual problem couples (n = 20) with outcomes for single problem couples in which only one partner had AUD (n = 386). Results showed that dual problem and single problem couples did not differ significantly on degree of improvement in abstinence following BCT. A case example illustrates the application of BCT when both partners have a current AUD.
Keywords: Alcoholism, Couples Therapy, Treatment Outcomes
Multiple studies in the last 35 years have supported the efficacy of behavioral couples therapy (BCT) for treating married or cohabiting individuals seeking treatment for an alcohol use disorder (AUD). A meta-analysis showed that BCT produced better outcomes than more typical individual-based treatment (IBT) for married or cohabiting alcoholic patients, with a medium effect size favoring BCT over IBT (Powers, Vedal & Emmelkamp, 2008). More specifically, patients who received BCT had less alcohol use and fewer alcohol-related problems through 12-month follow-up than patients who received IBT (Epstein & McCrady, 1998; O’Farrell & Clements, 2012). However, a major limitation of BCT is that it has not been studied for the substantial number of alcoholic patients in which both members of the couple have a current alcohol problem.
BCT has traditionally been used to treat couples in which one member has a current alcohol use disorder (AUD) and the other member does not. Using this approach, BCT therapists typically teach the non-alcoholic partner to reinforce and build support for the alcoholic individual’s abstinence (O’Farrell & Schein, 2011). Following this approach, nearly all BCT studies have excluded so called “dual problem couples” in which both partners have a current AUD. The one exception was McCrady’s study of BCT with women alcoholic patients, in which 13% had male partners with a current AUD, but the impact of dual problem status on outcome was not examined (McCrady, Epstein, Cook, Jensen, & Hildebrandt, 2009). Therefore, it remains unclear whether the demonstrated efficacy of BCT among couples in which one member has an AUD will translate to treating dual problem couples in which both members have an AUD.
Whether BCT can successfully treat dual problem couples is an important clinical issue. One reason BCT is not well-utilized by clinicians (McGovern, Fox, Xie, &. Drake, 2004) may be the opinion that BCT studies have not included complex, difficult patients. When clinics and studies were treating mostly male AUD patients with 15–20% having female partners with an AUD, excluding these dual problem couples from BCT did not seem like a big problem. However, when clinics and studies began treating more female AUD patients with 40–70% or more having male partners with an AUD (Jacob & Bremer, 1986), excluding dual problem couples from BCT became an important unresolved problem. If BCT could be extended to dual problem couples, it would substantially increase the number of patients that could benefit from BCT and it would remove a barrier to clinical utilization of BCT.
As a first step to examine outcomes for BCT with dual problem couples, we expanded inclusion criteria in a naturalistic study of BCT outcomes. Specifically, we included a subset of dual problem couples which we thought might be treated successfully in BCT. These were couples in which both partners had a current AUD and both agreed to enter BCT to pursue abstinence. The rationale was that these couples in which both partners were motivated to pursue abstinence may be able to work together in BCT to support each other in achieving abstinence in a similar fashion as couples in which only one member has an AUD.
Using data from this naturalistic study of BCT, the present exploratory study compared drinking outcomes before and in the year after BCT for alcoholic patients in dual problem couples (in which both members had a current AUD) with outcomes for alcoholic patients in single problem couples (in which only one member had a current AUD). The purpose of the present study was to explore whether levels of improvement in days abstinent following BCT differed for patients in dual problem couples versus patients in single problem couples. Also, since prior studies have not described the application of BCT for dual problem couples, we provide a clinical case example to illustrate the application of BCT for a couple in which both partners had current AUD and both wanted to achieve sobriety.
Method
Participants
Participants were 406 alcoholic patients and their spouses or cohabiting partners who entered the Counseling for Alcoholics’ Marriages (CALM) Project at 1 of 4 addiction treatment centers throughout Massachusetts. The CALM Project was designed to naturalistically examine factors that predict outcome following BCT. Inclusion criteria included (a) patient and spouse were ages 21 to 65; (b) couple was married or living together for at least 1 year; (c) patient met current alcohol abuse or dependence diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R; American Psychiatric Association, 1987); (d) patient (or both patient and partner in dual problem couples) agreed to the goal of abstinence while participating in BCT. More details regarding inclusion criteria can be found elsewhere (see Chase, O’Farrell, Murphy, Fals-Stewart, & Murphy, 2003; and O’Farrell, Murphy, Stephan, Fals-Stewart, & Murphy, 2004). The 406 alcoholic patients (303 male and 103 female patients) in the study sample were mostly White (94%) with an average age of 42.19 (SD = 9.57), an average of 13.22 years of education (SD = 2.31), and had been married or living together an average of 12.22 (SD = 10.40) years to their current partner. Most of these couples were married (88%).
For the 406 patients, the DSM-III-R current (past 6 months) alcohol problem diagnosis at study entry was alcohol dependence for 380 patients (94% of sample), alcohol abuse for 6 patients (1%), alcohol dependence in partial remission for 9 patients (2%), and alcohol dependence in full remission for 11 patients (3%). Patients in full or partial remission had been abstinent or drinking in a limited fashion for the past 6–8 months before which time all had been seriously dependent on alcohol; they entered BCT to prevent relapse and deal with relationship issues. A diagnosis of current drug abuse or dependence was also present for 78 patients (19%).
Initially we excluded patients if the study intake interview indicated that the patient’s partner also had a current AUD problem. Partway through the study, we changed study criteria to include patients for whom the intake interview indicated the partner also had a current AUD – if both patient and partner agreed to work together in BCT sessions to achieve mutual abstinence. This broadened criteria resulted in 20 dual problem couples in which both members had a current AUD and the remaining 386 single problem couples in which only one member had an AUD. 1
Procedure
Patients and partners provided written, informed consent to participate in the study which was approved by Institutional Review Boards at Harvard Medical School and at VA Boston.
BCT treatment program
The BCT program (O’Farrell, 1993) of 20–22 weekly couple sessions over 5–6 months included a recovery contract to promote abstinence, instigation of positive couple activities, and training in communication skills. The recovery contract used a calendar to record completion of (a) a daily “trust discussion” in which the patient states an intent to stay abstinent that day and the spouse expresses support for the patient’s efforts and (b) other recovery activities (e.g., Alcoholics Anonymous (AA) meetings, disulfiram). Treating the dual problem couples required negotiating a dual (rather than single person) recovery contract with a joint trust discussion (in which each person stated their intent to stay sober with mutual thanking) along with recovery activities for each person.
Measures
Percentage days abstinent (PDA)
PDA was defined as the percentage of days on which the individual was not in a hospital, jail, or halfway house and remained abstinent from alcohol and other drugs. PDA was calculated from the Timeline Followback Interview (TLFB; Sobell & Sobell, 1996) for the 12 months preceding BCT, the pre- to post-treatment interval, and months 1–6 and 7–12 following BCT. TLFB retrospective daily reports of substance use have excellent test-retest and patient-collateral report reliability (Sobell & Sobell, 1996).
Analytic Strategy
To explore whether dual and single problem couples differed on levels of improvement after BCT, the study sample of 406 couples was divided into the following subgroups: (a) dual problem couples in which both partners had a current AUD (n = 20), (b) single problem couples in which the male partner had a current AUD but the female partner did not (n = 303), and (c) single problem couples in which the female partner had a current AUD but the male partner did not (n = 83). To control for the possible effects of gender on treatment outcomes, outcomes for male patients in dual problem couples were compared with outcomes for male patients in single problem couples, and outcomes for female patients in dual problem couples were compared with outcomes for female patients in single problem couples.
Individual growth modeling method with SAS PROC MIXED procedure (Singer, 1998; Singer & Willet, 2004) was used to examine changes over time in PDA outcomes and the effect of dual versus single problem status on PDA. Given its ability to handle correlated observations and its robustness regarding missing data, growth modeling is an ideal method for studying change over time (Atkins, 2005; Singer & Willet, 2004). We used a two-level growth model, with the Level-1 model characterizing within-couple changes over time in PDA outcomes and the Level-2 model testing the effects of dual versus single problem couples status on PDA outcomes. In all analyses, time was re-centered so that PDA during the 12 months prior to treatment represented the Level-1 model intercept. Given the exploratory nature of the study, all statistical trends (i.e., p’s smaller or approaching .10-level) When comparing effect size differences between dual versus single problem couples, we computed Cohen’s d and followed Cohen’s (1988) suggested guidelines in interpreting these effect sizes (small = .20, medium = .50, large = .80).
Results
Preliminary Analyses
Table 1 shows the means and standard deviations for PDA for both male and female patient samples as a function of their single or dual problem couple status. Among female patients, there were no significant differences on PDA between dual and single problem couples at treatment entry (i.e., at Pre assessment): t(101) = .28, p = .78. Among male patients at treatment entry, the male patients from the single problem couples had marginally lower PDA; t(321) = 1.67, p = .095. Thus, dual problem status was added as a predictor of PDA intercept when examining PDA in the male alcoholic sample.
Table 1.
Means and standard deviations of PDA outcome measure for male and female patients as a function of “single” versus “dual” alcoholism couple status.
| Percentage days abstinent (PDA); M (SD)
|
||||
|---|---|---|---|---|
| Pre | Post | M6 | M12 | |
| Male (NS/ND) | 303/20 | 290/18 | 293/15 | 288/14 |
| Single alcoholism | 34.44 (28.82) | 92.60 (17.38) | 80.36 (28.94) | 74.66 (34.52) |
| Dual alcoholism | 45.52 (26.41) | 91.25 (20.80) | 85.68 (25.48) | 76.54 (26.44) |
|
|
||||
| Female (NS/ND) | 83/20 | 75/20 | 77/19 | 76/19 |
| Single alcoholism | 43.40 (29.18) | 92.47 (14.87) | 83.36 (26.42) | 78.28 (30.13) |
| Dual alcoholism | 41.43 (24.46) | 84.00 (28.75) | 82.48 (31.79) | 77.88 (36.31) |
Note. NS/ND indicates the sample size for two groups of interest at each assessment: i.e., “single”- (NS) vs. “dual”- (ND) problem couples. For example, for the percentage days abstinent measure at Pre assessment, data were available for the 303 single alcoholism and 20 dual alcoholism couples in the male patient sample, and data were available for the 83 single and 20 dual alcoholism couples in the female patient sample.
Growth Models
Table 2 shows the results for the Level-1 unconditional model, which characterized the effects of within-person change over time in PDA, and the Level-2 model, which included the effects of dual versus single problem couple status as a predictor of PDA. Results for male and female patients are presented, respectively, in the top and bottom half of Table 2.
Table 2.
Results for the individual growth model (percentage days abstinent - PDA) for male and female patients with alcoholism.
| Level-1 unconditional model | Level-2 dual problem model | ||||
|---|---|---|---|---|---|
|
| |||||
| Male Sample | Parameter estimate | SE | Parameter estimate | SE | d |
| Fixed Effects | |||||
| Intercept | 38.66*** | 1.52 | 38.18*** | 1.54 | |
| Dual | 7.67 (ns) | 4.84 | .108 | ||
| Linear Slope | 58.26*** | 2.17 | 58.49*** | 2.18 | |
| Dual | −2.99 (ns) | 3.34 | .039 | ||
| Quadratic Curve | −15.85*** | .64 | −15.85*** | .64 | |
| Dual | -- | -- | |||
| Random Effects | |||||
| Intercept | 293.01*** | 69.40 | 289.56*** | 69.17 | |
| Linear Slope | 328.16* | 154.26 | 326.73* | 154.11 | |
| Quadratic Curve | 8.75 (ns) | 14.25 | 8.70 (ns) | 14.24 | |
| AIC | 11656.4 | 11645.0 | |||
|
| |||||
| Female Sample | Parameter estimate | SE | Parameter estimate | SE | d |
|
| |||||
| Fixed Effects | |||||
| Intercept | 45.67*** | 2.64 | 45.67** | 2.64 | |
| Dual | -- | -- | |||
| Linear Slope | 49.39*** | 3.82 | 50.80*** | 4.01 | |
| Dual | −6.89 (ns) | 5.98 | .107 | ||
| Quadratic Curve | −13.27*** | 1.06 | −13.70*** | 1.12 | |
| Dual | 2.09 (ns) | 1.83 | .153 | ||
| Random Effects | |||||
| Intercept | 404.56*** | 111.33 | 404.84*** | 111.24 | |
| Linear Slope | 651.56** | 245.03 | 654.61** | 245.17 | |
| Quadratic Curve | 29.04f | 20.63 | 29.30f | 20.63 | |
| AIC | 3588.4 | 3580.1 | |||
Note.
p = .079;
p < .05;
p < .01;
p < .01.
Note that “dual” status was only added as a predictor of the initial status male sample, because preliminary analyses showed that only male but not female patients from single and dual alcoholism couples significantly differed in PDA at Pre assessment. d (standardized effect size) = standardized fixed-effect parameter divided by squared root of the corresponding random effect (cf. Atkins et al., 2005; Raudenbush & Xiao-Feng, 2001).
Male Patient Sample
Examination of the fixed effects in the unconditional model showed that male patients entered treatment with an average PDA of 38.66%, p < .0001; that they increased in PDA by an average 58.26% for each assessed 6-month period, p < .0001; and that they experienced an average curvature of −15.85%, p < .0001. Examination of random effects showed a significant variation around these average values for the intercept and linear slope (all p’s < .05), but not for the quadratic change function (p = .27). Given the lack of individual variation around the quadratic change function, it was not warranted to add dual problem couple status as a predictor of quadratic change.
When dual partner status was added to the equation, the results showed that male patients from single vs. dual problem couples did not differ significantly on PDA from one another at study entry, 7.67%, p = .12, or in rates of linear change, −2.99%, p = .37. According to Cohen’s guidelines (1988) the effect size differences between male patients from single vs. dual problem couples were quite small at study entry (d = .108) and in rates of linear change (d = .039) following treatment (see top half of Table 2 & Figure 1). To further explain the very small effect size (ES) we found when we compared single vs. dual problem couples on improvement in PDA for male patents following BCT, we considered the following. Cohen (1988) describes d = .20 as a small ES that accounts for 1.00% of variance. The ES we found for rate of linear change was d = .039, an ES that accounts for only 0.04% of variance.
FIGURE 1.
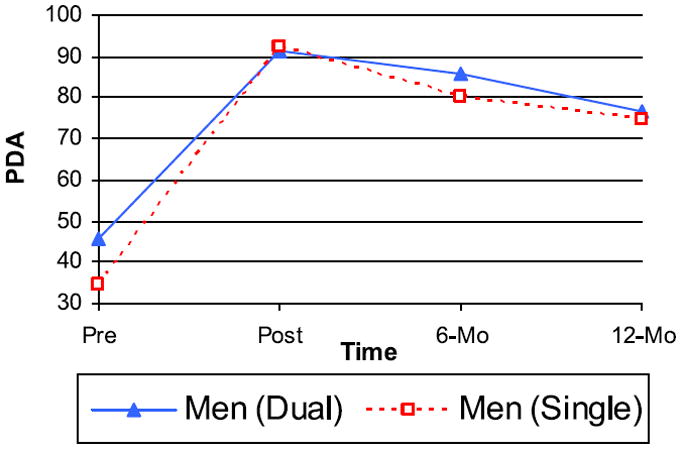
Male patient sample observed mean values for percent days abstinent (PDA) outcomes of dual versus single problem couples. Triangles represent the PDA mean value at four assessment points for male patients in dual problem couples; squares represent the PDA mean value at four assessment points for male patients in single problem couples. (color figure available online)
Female Patient Sample PDA
Examination of the fixed effects in the unconditional model showed that female patients entered treatment with an average abstinence rate of 45.67%, p < .0001); that they increased in PDA by an average of 49.39% for each assessed 6-month period, p < .001; and that there was a negative average curvature as well of −13.27%, p < .0001. Examination of random effects showed a significant variation around each of these averages (in the intercept and linear slope, p < .001; in quadratic curvature, p = .079) and therefore, further addition of the substantive predictor was meaningful.
When dual partner status was added to the equation, the results showed that female patients from single vs. dual problem couples did not differ significantly from one another in rates of either linear, −6.89%, p = .25, or quadratic change, 2.09%, p = .25. The effect size differences between female patients from single vs. dual problem couples were quite small with regard to rates of linear (d = .107) and quadratic (d = .153) change on PDA (see bottom half of Table 2 & Figure 2). To further explain these very small effect sizes, we considered the following. The ES we found for rate of linear change was d = .107, an ES that accounts for only 0.29% of variance; and d = .153 for rate of quadratic change, an ES that accounts for only 0.58% of variance.
FIGURE 2.
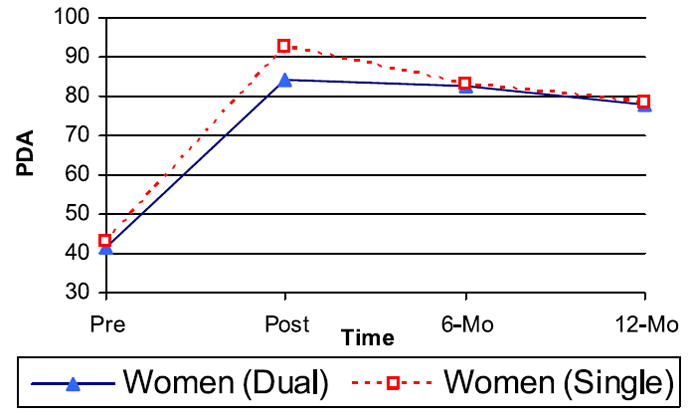
Female patient sample observed mean values for percent days abstinent (PDA) outcomes of dual versus single problem couples. Triangles represent the PDA mean value at four assessment points for female patients in dual problem couples; squares represent the PDA mean value at four assessment points for female patients in single problem couples. (color figure available online)
Case Example of BCT with a Dual Problem Couple When Both Wanted to Change
The following case example illustrates the use of BCT with a dual problem couple when both partners sought sobriety. Sue and Gene2 were in their mid 30’s, married 16 years, with 3 children ages 5 to 11. Sue was referred to the BCT counselor after a hospital detox for very heavy daily drinking plus 3–4 times per week cocaine and regular marijuana use. She also used and overused tranquilizers prescribed by her family doctor for stress. At the first couple session, the counselor learned that Gene had similar substance problems except his alcohol use was not quite as heavy so he had not been detoxed. Both had decided to “quit for good” to try to get their kids back.
They had lost custody of their 3 children a month earlier when Gene was arrested for drunk driving. Sue and the 3 kids were in the car, and Sue also was obviously intoxicated. They had been out partying at their local bar on Friday night, had picked up the kids from a friend’s house, and were driving home. The police made a complaint of suspected child neglect and endangerment to social services. Investigation and interviews of neighbors and family revealed that both Sue and Gene frequently drank and used cocaine or marijuana when caring for their kids. Social services placed the children temporarily with Sue’s parents for 6–12 months with the possibility they could regain custody if they got treatment and stayed abstinent.
Sue and Gene came to BCT sessions weekly for 6 months. With the counselor’s help, they set up the “dual recovery contract” shown in Figure 3. In this contract they agreed to (a) do a daily trust discussion in which each promised the other to stay abstinent that day, (b) take Antabuse daily together, (c) attend 3 times weekly 12-step meetings (not necessarily together), and (d) have weekly urine screens. As shown on their recovery contract calendars in Figure 4, they were pretty faithful to the contract once it got in full force after the first few weeks. Neither of them drank while in weekly BCT.
FIGURE 3.
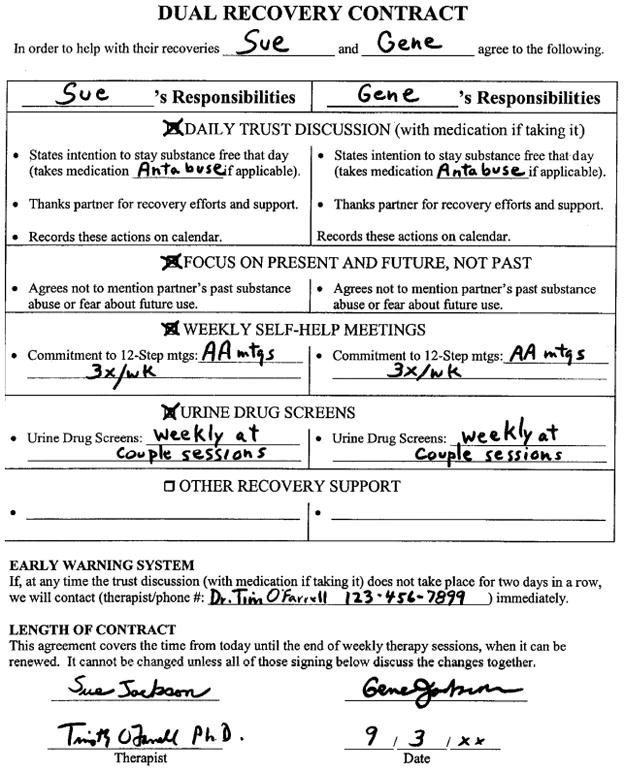
Dual Recovery Contract for a dual problem couple, Sue and Gene. From page 201 of Behavioral Couples Therapy for Alcoholism and Drug Abuse by T. J. O’Farrell and W. Fals-Stewart, copyright 2006 by Guilford Press. Reprinted with permission of The Guilford Press.
FIGURE 4.
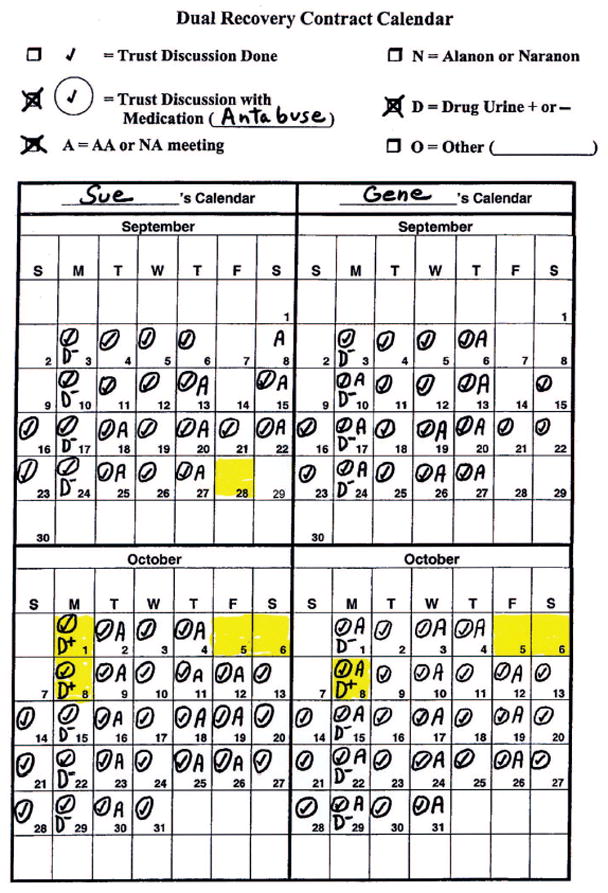
Dual Recovery Contract calendar for a dual problem couple, Sue and Gene. Sshaded days on the calendars indicate days on which cocaine was used or a urine test was positive for cocaine. From page 201 of Behavioral Couples Therapy for Alcoholism and Drug Abuse by T. J. O’Farrell and W. Fals-Stewart, copyright 2006 by Guilford Press. Reprinted with permission of The Guilford Press. (color figure available online)
About 4 weeks after starting BCT, Sue used cocaine on Friday night when she went by herself to the local bar with a girlfriend (see Figure 4). She reported this at the next BCT session and her urine taken that session was positive for cocaine. They agreed in session that the bar and the girlfriend were high risk triggers for using that they should avoid. However, the following Friday found them both in the bar. They had decided to go together to the bar. They had pledged to each other not to drink or use cocaine but just to socialize, watch TV sports, and play pool. They planned to help each other if either was tempted. Once at the bar, they ran into the girlfriend who had given Sue cocaine the previous week. When it was offered to them they didn’t refuse, but told each other “we’ll just do a line each”. They stuck to this limit. However, the next night on Saturday they went to the bar again. This time they each used multiple lines of cocaine.
At the following BCT session they discussed this relapse. At first they each blamed the other. Gene blamed Sue for going back to the bar and for giving in to her girlfriend’s influence. Sue blamed him for not stopping her from using cocaine, for not being stronger himself. Then the counselor suggested they analyze their mutual relapse – triggers that led to it, damage impact, and things learned for the future. They reflected that this level of use was not nearly as much as before starting BCT. However, they were heading back to their old pattern with use on weekends escalating into use during the week. They realized they would not get their children back if this continued. Even if someone saw them in the bar and reported them to social services, this could be quite damaging.
This relapse was a turning point for Sue and Gene. Realizing how close they came to “starting the madness again” as Gene put it, they got more committed to their recovery. They planned specific things to do Friday and Saturday evenings, starting with an AA meeting together on Friday evening. Sue called the girlfriend to say she wasn’t going to the bar or using drugs, that she wanted to get her children back. Gene called the woman’s boyfriend and delivered the same message. They each decided to get a sponsor and to socialize more with sober friends.
They also benefitted from relationship-focused parts of BCT, especially work on communication. Now that they were both abstinent, conflict between them was pretty low. They had not realized how much alcohol and drug use had caused problems between them. Their most bitter arguments and a few occasion of minor violence had always occurred when both were under the influence of alcohol and cocaine.
After 6 months of weekly BCT, Sue and Gene returned to see the counselor for regular checkups for 2 more years. They re-gained custody of their children. They stayed abstinent except for a few isolated days for Gene and a 5-day relapse for Sue, which led to a few crisis sessions with the BCT counselor to help them get back on track.
Discussion
Using a naturalistic sample of AUD patients seeking BCT, this study compared outcomes after BCT for dual problem couples with outcomes for single problem couples in which only one partner had AUD. Results showed that dual problem and single problem couples did not differ significantly on degree of improvement in abstinence following BCT. In addition, effect size differences with regard to the degree of improvement in abstinence were quite small when dual and single problem couples were compared. These results are promising in showing that BCT is adaptable to treat couples in which both partners exhibit AUD and both are willing to commit to the goal of abstinence. The present study suggests that simultaneously engaging both partners in BCT may be a promising approach to improving treatment outcomes for individuals with substance-use disorders who also have a partner with a substance-use problem.
Although the present results suggest that BCT may be effectively implemented among dual problem couples in which both partners have AUD, the current study has several limitations. The small sample size of dual problem couples may have led to less stable parameter estimates than would have been obtained if a larger sample size had been used. Therefore, future research using a larger sample of dual problem couples is needed to replicate these findings.
In addition, it is important to note that the current results were obtained with a select subsample of dual problem couples, namely those in which both partners were willing to work toward a goal of abstinence from alcohol. For dual problem couples to qualify for BCT in the current study, both partners had to agree to enter BCT to pursue a goal of abstinence from alcohol. Therefore, results for dual problem couples in the current study cannot be extended to couples in which one member is currently unmotivated to become sober. As there is some evidence that continued drinking or drugging by one partner can influence that of the other partner (Leonard & Mudar, 2003), it is likely that within dual problem couples, one partner continuing to drink or drug will place the other partner at risk for continued substance use as well. Motivational discordance toward sobriety with dual problem couples may need to be addressed before BCT can be used. For example, in such couples, therapies aimed at motivational enhancement toward sobriety (e.g., Miller & Rollnick, 2002) may be a necessary precursor to BCT in order for BCT to be maximally effective.
Given that many substance-abusing individuals are also likely to have partners who are substance-abusing (Greenfield et al, 2007; Jacob & Bremer, 1986), results of the current study are important in suggesting that BCT may be an efficacious treatment for dual problem couples in which both partners share the goal of abstinence from alcohol and drugs. These results are also promising when considering treatment cost effectiveness, in that BCT could be used to simultaneously treat both partners in dual problem couples, whereas individual treatment approaches would accrue to the costs of treating each partner separately. Clearly, more research is needed to extend the findings of the current study and determine whether BCT may be a clinically efficacious and cost effective treatment for dual problem couples in which both partners have AUD.
Acknowledgments
This research was supported by grants to the second author from the National Institute on Alcohol Abuse and Alcoholism (grants AA08637, AA10356, K02AA0234) and by the Department of Veterans Affairs. Support in preparing this manuscript was also provided by grant CDA-2-019-09S awarded to the first author by the Department of Veterans Affairs.
Portions of this article were presented at the Annual Meeting of the Association for the Advancement of Behavioral and Cognitive Therapies, Chicago, November, 2006; and at the Annual Convention of the American Psychological Association, Boston, August, 2008.
Footnotes
All 386 single problem couples were judged, by the Master’s level clinicians who conducted the study intake interviews, not to have a partner with a current clinically significant alcohol or drug problem. These judgments were made on a clinical basis during the intake interview without reliance on the SCID. However, SCID results completed after the intake interview as part of the baseline research assessment showed that the partner in 18 of these 386 couples did have a current (past 6 months) abuse or dependence on alcohol or another drug. These 18 partners had mild severity alcohol and drug problems as defined by DSM-III-R – i.e., they had few, if any, symptoms in excess of those required to make the diagnosis. In addition, these partners for the most part had already stopped or substantially reduced problem drinking or other drug use for 2–3 months when the couple completed the intake interview for the BCT program, and they intended to maintain these changes. Further, follow-up data showed that most of these 18 partners did maintain low or no use through 6- and 12-month follow-up. Therefore, given our goal to test BCT with clinically challenging dual problem couples, we decided to treat these 18 couples in BCT as single problem couples focusing only on the substance use of the patient identified in the screening interview and to include them in the single couple group in the analyses reported in this article.
This case example is a composite case with individual identities disguised to protect the privacy and anonymity of the couple. This case example draws very heavily from page 200–202 of the book Behavioral Couples Therapy for Alcoholism and Drug Abuse by T.J. O’Farrell and W. Fals-Stewart, copyright 2006 by Guilford Press. This material is used with permission of The Guilford Press.
Contributor Information
Jeremiah A. Schumm, Cincinnati VA Medical Center and University of Cincinnati, Cincinnati, Ohio USA.
Timothy J. O’Farrell, VA Boston Healthcare System and Harvard Medical School, Brockton Massachusetts, USA.
Jasmina Burdzovic Andreas, Department of Community Health, Brown University, Providence, Rhode Island USA.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental Disorders. 3. Washington, DC: Author; 1987. revised. [Google Scholar]
- Atkins DC. Using multilevel models to analyze couple and family treatment data: Basic and advanced issues. Journal of Family Psychology. 2005;19:98–110. doi: 10.1037/0893-3200.19.1.98. [DOI] [PubMed] [Google Scholar]
- Chase KA, O’Farrell TJ, Murphy CM, Fals-Stewart W, Murphy M. Factors associated with partner violence among female alcoholic patients and their male partners. Journal of Studies on Alcohol. 2003;64:137–149. doi: 10.15288/jsa.2003.64.137. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Epstein EE, McCrady BS. Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clinical Psychology Review. 1998;18:689–711. doi: 10.1016/s0272-7358(98)00025-7. [DOI] [PubMed] [Google Scholar]
- Greenfield SA, Brooks JA, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele MM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Bremer DA. Assortative mating among men and women alcoholics. Journal of Studies on Alcohol. 1986;47:219–222. doi: 10.15288/jsa.1986.47.219. [DOI] [PubMed] [Google Scholar]
- Leonard KE, Mudar P. Peer and partner drinking and the transition to marriage: A longitudinal investigation of selection and influential processes. Psychology of Addictive Behaviors. 2003;17:115–125. doi: 10.1037/0893-164x.17.2.115. [DOI] [PubMed] [Google Scholar]
- McCrady BS, Epstein EE, Cook S, Jensen N, Hildebrandt T. A randomized trial of individual and couple behavioral alcohol treatment for women. Journal of Consulting and Clinical Psychology. 2009;77:243–256. doi: 10.1037/a0014686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Fox TS, Xie H, Drake RE. A survey of clinical practices and readiness to adopt evidence-based practices: Dissemination research in an addiction treatment system. Journal of Substance Abuse Treatment. 2004;26:305–312. doi: 10.1016/j.jsat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- O’Farrell TJ. A behavioral marital therapy couples group program for alcoholics and their spouses. In: O’Farrell TJ, editor. Treating alcohol problems: Marital and family interventions. New York: Guilford Press; 1993. pp. 170–209. [Google Scholar]
- O’Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment of alcoholism. Journal of Marital and Family Therapy. 2012;38:122–144. doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. New York: Guilford Press; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM, Stephen S, Fals-Stewart W, Murphy M. Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: The role of treatment involvement and abstinence. Journal of Consulting and Clinical Psychology. 2004;72:202–217. doi: 10.1037/0022-006X.72.2.202. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Schein AZ. Behavioral couples therapy for alcoholism and drug abuse. Journal of Family Psychotherapy. 2011;22:1–23. [Google Scholar]
- Powers M, Vedel E, Emmelkamp P. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review. 2008;28:952–962. doi: 10.1016/j.cpr.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Xiao-Feng L. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001;6:387–401. [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Behavioral and Educational Statistics. 1998;24:323–355. [Google Scholar]
- Singer JD, Willet JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2004. [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]


