Abstract
Background:
Early diagnosis of left ventricular mass (LVM) inappropriateness and left ventricular hypertrophy (LVH) can result in preventing diastolic left ventricular dysfunction and its related morbidity and mortality. This study was performed to determine if diastolic dysfunction is associated with LVH and inappropriate LVM.
Materials and Methods:
One hundred and twenty five uncomplicated hypertension from Isfahan Healthy Heart Program underwent two-dimensional echocardiography. Inappropriate LVM was defined as an LVM index greater than 88 g/m2 of body-surface area in women and greater than 102 g/m2 in men. LVH-defined septal and posterior wall thickness greater than 0/9 cm in women and greater than 1 cm in men, respectively. Echocardiographic parameters, including early diastolic peak velocity (E)/late diastolic peak velocity (A), deceleration time (DT), and E/early mitral annulus velocity (E′) were measured.
Results:
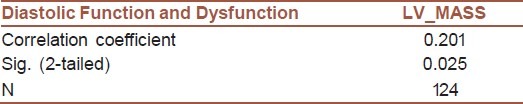
The mean systolic and diastolic blood pressure at the patients’ admission day were 142.87 ± 18.12 and 88.45 ± 9.18 mmHg, respectively. Totally, 21.7% of subjects had inappropriate LV mass that moderate and severe abnormal LV mass was revealed in 5.6% and 5.6%, respectively. The mean of age and BMI was significantly higher in patients with moderate left ventricular hypertrophy (P < 0.05). Adjusted by age, gender, BMI, and systolic and diastolic blood pressures, both E/A ratio and deceleration time were higher in those with the severer ventricular hypertrophy. Subjects with severe showed significantly higher BMI 33. 7 ± 3.7 (P < 0.001). There was a slight difference between the grade of diastolic dysfunction and the severity of inappropriate LV mass (P = 0.065). But no significant difference was found between E/A, E/E′, and deceleration time and the level of inappropriate LV mass (P > 0.05). Spearman's Rank test was used to test the correlation between diastolic dysfunction and LV mass (P = 0.025).
Conclusion:
LVH is correlated with the severity of diastolic dysfunction manifested by the E/A value and deceleration time, but inappropriate LVM can slightly predict diastolic dysfunction severity in uncomplicated hypertension.
Keywords: Echocardiographic, left ventricular mass, left ventricular hypertrophy, Diastolic dysfunction
INTRODUCTION
Inappropriateness of left ventricular mass (LVM) as well as left ventricular hypertrophy has been identified to be important prognostic factors for cardiovascular events in patients with acute myocardial infarction or progressive heart failure.[1] Physiological studies revealed that LVM is potentially influenced by some hemodynamic factors, such as high blood pressure, stroke work, as well as constitutional factors, including body size, female gender, and advanced age.[2,3] According to this fact that the left ventricular hypertrophy and its inappropriate mass continues to be a strong predictor of life-threatening cardiovascular end points, assessing the ventricular structure based on echocardiography seems to be necessary.[4] Importantly, this assessment is vital in patients with diastolic function impairment, because it has been suggested that the diastolic dysfunction can lead to the impairment of ventricular filling, reducing stroke volume and cardiac output, and even progressive pulmonary congestion and edema that are main causes of heart failure and even cardiac death. Besides, evaluation of relationship between ventricular morphology and diastolic function indices is important because the overall prevalence of left ventricular diastolic dysfunction has been shown in about one-third of general population and in the majority of those with the evidences of cardiovascular ischemia.[5,6] Therefore, ventricular abnormality and dysfunction could be useful in preventing diastolic and systolic heart failure and its related morbidity and mortality. In this study, we tried to assess the association of left ventricular hypertrophy and ventricular mass appropriateness with the appearance of diastolic dysfunction in a sample of Iranian patients based on the information from Isfahan Healthy Heart Program (IHHP).
MATERIALS AND METHODS
In the ongoing case control, cross-sectional, noninterventional trial are part of the IHHP. IHHP as a comprehensive community-based intervention program that was designed to improve behaviors lifestyle, and to control CVD and its risk factors have showed positive results. IHHP design and interventions have been previously reported in detail.[6] Totally, 600 hypertensive subjects were involved in IHHP. This substudy was done from April 2009 to December 2009 in Hypertension Research Center, Isfahan Cardiovascular Research Institute. Participants were selected from IHHP data base. In this trial, the exclusion criteria were defined as having diabetes mellitus, secondary hypertension, recent surgery, any chronic disease, unstable and stable angina, any valvular heart disease, pericardial disease, cardiomyopathy based on the echocardiographic findings, congestive heart failure, known coronary artery disease and incomplete clinical data, or unwillingness to participate or inability for logistic reasons.
Also hypertension can induced premature coronary artery disease as smoking with respect to number of vessel involvement and left main disease but[7] participants underwent a comprehensive noninvasive diagnostic workup at the baseline, including echocardiography, exercise stress test, and cardiovascular computed tomography (CT). Baseline characteristics were collected by interviewing at the admission time and height, weight, abdominal circumference, blood pressure, and heart rate were measured before echocardiography. Systolic and diastolic blood pressures were measured two times in 1 minute interval by the same instrument. The study protocol was approved by the Institutional review board of Isfahan Cardiovascular Research Institute. Informed consent was obtained from each patient regarding the process of the examination and use of the data.
Two-dimensional echocardiogram was performed on each participant by a single cardiologist with a commercially available machine with a 1–5 MHz transducer. The left ventricular internal end-diastolic dimension (EDD), the end systolic dimension (ESD), and the septal and posterior wall thicknesses (IVSd, LVPWd) were measured on the leading edge-to-the leading edge, according to the guidelines of the American Society of Echocardiography.
Observed left ventricular mass was calculated by the following equation: Without measuring the major axis of the LV, LV mass is obtained from the LV short-axis dimension and a simple geometric cube formula. The following equation provides a reasonable determination of LV mass in grams:
1.04×((LVID+PWT+ IVST)3-LVID3)×0.8+0.6[8]
where LVID is the internal dimension, PWT is posterior wall thickness, IVST is interventricular septal thickness,1.04=specific gravity of the myocardium, and 0.8 is the correction factor. All measurements are made at end- diastole (at onset of the R wave) in centimeters
Besides, predicted left ventricular mass was calculated by the following equation: 55.37+6.64×height (m2)+0.64×stroke work (g-m/beat)–18.07×gender; where male=1 and female=2. Observed LVM (oLVM) was divided by predicted LVM (pLVM) and was expressed as a percentage (oLVM/pLVM). oLVM/pLVM was categorized using the 5th and the 95th percentiles of the distribution in the normotensive, normal- weight reference adult population.
Inappropriate LVM was defined as an LVM index greater than 88 g/m2 of the body-surface area in women and greater than 102 g per square meter in men[9].
LVH-defined septal and posterior wall thickness greater than 0/9 cm in women and greater than 1 cm in men, respectively.
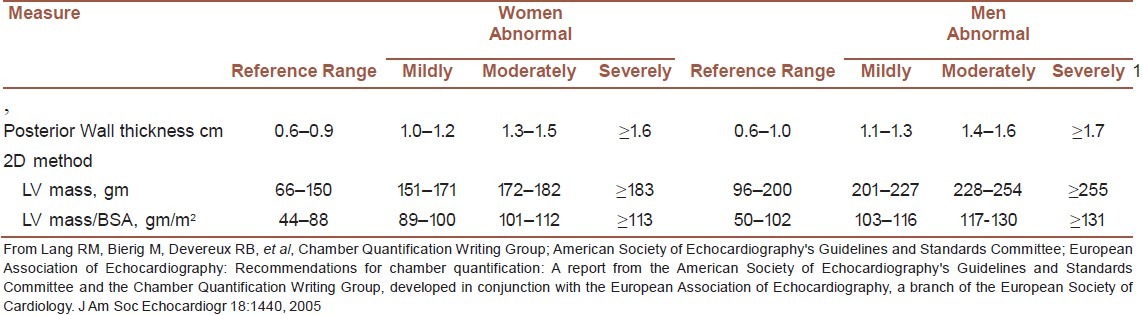
Further division to mild, moderate, and severe LVM and LVH was down according to Table 1.
Table 1.
Reference limits and partition values of left ventricular (LV) mass and geometry[17]
Doppler echocardiography was performed and Early (E) and late (A) diastolic peak velocities, deceleration time (DT), and early-to-late diastolic peak velocity ratio (E/A) were determined. Early mitral annulus velocity (E’) was measured at the septal portion of the mitral annulus in an apical four chamber view using a tissue Doppler technique.[10,11] Diastolic dysfunction was graded as mild (Grade I) with abnormal relaxation and moderate (Grade II) with the pseudonormal function and higher grades were not included into the study.
Results are presented as mean ± SD (standard deviation) for quantitative variables, and are summarized by absolute frequencies and percentages for categorical variables. Continuous variables between the groups were compared using the ANOVA test. Categorical variables across the study groups were compared using the chi-square test or Fisher's exact test if required. Spearman's Rank test was used to test the correlation between diastolic dysfunction and LV mass. The statistical software SPSS version 16.0 for windows (SPSS Inc., Chicago, IL) was used. All P-values were two- tailed with statistical significance defined by P ≤ 0.05.
RESULTS
The average age of the study subjects was 51.96 ± 9.32 years and 56.0% of them were females. The mean of body mass index in the patients was 29.39 ± 4.44 kg/m2. At the visit time, 20.8% had systolic blood pressure >140 mmHg and 18.2% of them had diastolic blood pressure > 100 mmHg. The mean systolic and diastolic blood pressure at the patients’ admission day were 142.87 ± 18.12 mmHg and 88.45 ± 9.18 mmHg, respectively. Abnormal electrocardiogram was observed in 8.8% of the patients. In 26.4% of the subjects, left ventricular hypertrophy was reported, where moderate and severe hypertrophy was found in 7.2% and 2.4% of them, respectively. Totally, 21.7% of subjects had inappropriate LV mass that moderate and severe abnormal LV mass was revealed in 5.6% and 5.6%, respectively.
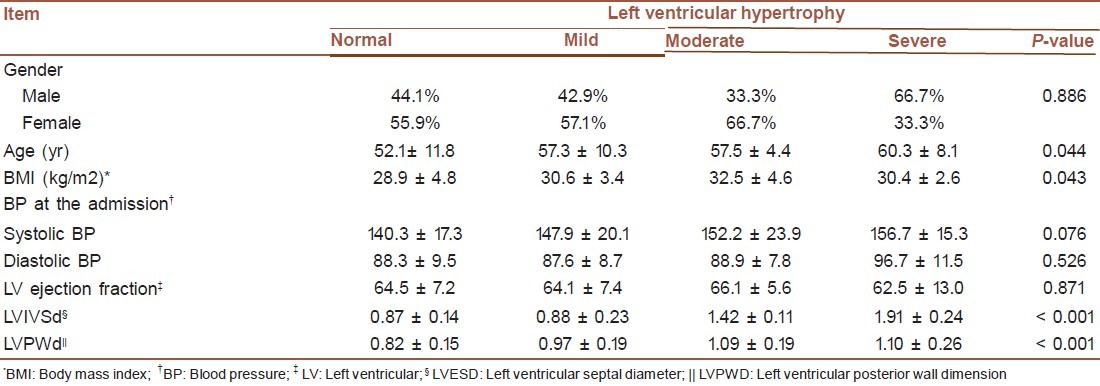
The mean of age and BMI was significantly higher in patients with moderate left ventricular hypertrophy (P < 0.05) [Table 1]. Both systolic and diastolic blood pressures as well as left ventricular ejection fraction had not any differences based on the severity of left ventricular hypertrophy (P > 0.05), while left ventricular systolic diameter (LVESD) and LVPWD showed significant differences with severity of left ventricular hypertrophy (P < 0.001). With respect to the difference between the appearance of left ventricular hypertrophy and indices of diastolic function, significant difference were found between E/A and the severity of left ventricular hypertrophy 0.83 ± 0.06, respectively (P = 0.023) [Table 2]. When adjusted by age, gender, BMI, and systolic and diastolic blood pressures, both E/A ratio and deceleration time were higher in those with the severer ventricular hypertrophy.
Table 2.
Baseline characteristics in the patients with the different level of left ventricular hypertrophy
No significant differences were found in the sex ratio and mean age between the patients with appropriate LV mass and other ones (P > 0.05), whereas subjects with severe showed significantly higher BMI 33.7±3.7 [Table 3] (P < 0.001). The study groups base on inappropriate LV mass had similar systolic and diastolic blood pressures that measured at the admission time (P > 0.05). There was a slight difference between the grade of diastolic dysfunction and the severity of inappropriate LV mass [Table 4] (P = 0.065). However, no significant difference was found between E/A, E/E’, and deceleration time and the level of inappropriate LV mass (P > 0.05).
Table 3.
Parameter of diastolic function in patients with the different level of left ventricular hypertrophy
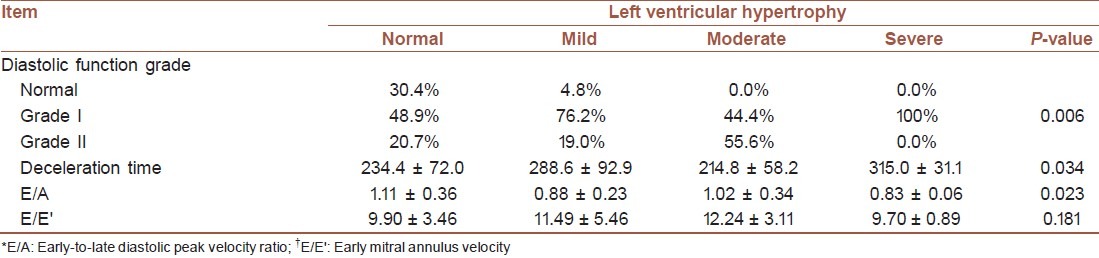
Table 4.
Baseline characteristics in the patients with the different level of inappropriate left ventricular mass
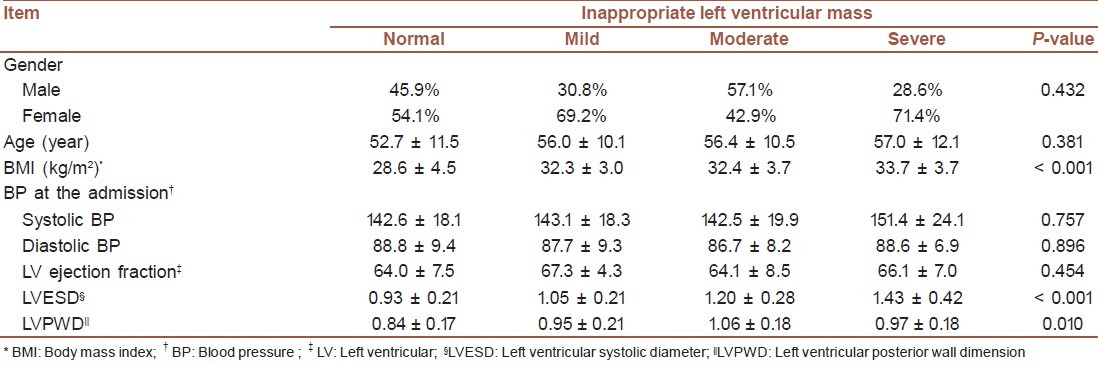
Table 5.
Parameter of diastolic function in patients with the different level of inappropriate left ventricular mass
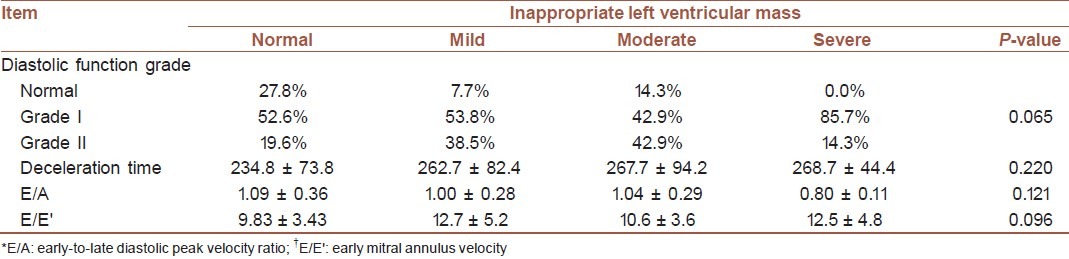
Table 6.
Association between the grade of diastolic dysfunction and the severity of inappropriate LV mass
DISCUSSION
This study was designed to determine if diastolic dysfunction is associated with left LVH and functional significance of the inappropriately increased LV mass using a tissue Doppler technique with the parameters of diastolic dysfunction.
Although heart failure with normal ejection traction (HFnlEF) has been thought to occur primarily in patients with LVH, studies that have carefully quantified LV mass report that echocardiographic criteria for LVH are met in less than 50% of patients.[12–13] Patients with HFnlEF have, on average, increased relative wall thickness and an increased mass-to-volume ratio,[12] but these findings often occur in the setting of normal LV mass. Thus, despite traditional teaching, LVH is not invariably present in HFnlEF, in which the cardiac phenotype is variable.
The findings showed that the inappropriateness of left ventricular mass is not an independent factor determining diastolic dysfunction, but left ventricular hypertrophy was evidenced to be a strong predictor for diastolic dysfunction, measured by deceleration time and E/A ratio even along with age, systolic and diastolic blood pressure, and gender. In fact, the adverse influence of left ventricular hypertrophy on the diastolic function was evidenced by the finding that the adjusted E/A value and deceleration time were higher in the left ventricular hypertrophic group; however, inappropriate left ventricular mass was not correlated with the severity of diastolic dysfunction. Although our result regarding predictive value of left ventricular hypertrophy was in agreement with other studies, but contrary to some previous studies, inappropriate ventricular mass could not predict severe diastolic function. In a study by Lim and colleagues,[1,13,14] inappropriateness of LV mass is independently associated with increased E/E’ that the resultant E/E’ ratio was lower in the inappropriate ventricular mass group than another group. Of course, slight observed correlations of the level of diastolic dysfunction and E/E’ ratio with inappropriate left ventricular mass may be attributable to the smaller sample size compared to previous studies.
Our findings suggested that inappropriateness of left ventricular mass might not have an additive or synergistic interaction with left ventricular hypertrophy. For sufficient statistical analysis of the interaction between appropriate left ventricular hypertrophy and inappropriate left ventricular mass, a study with a larger sample size is needed.
In this study, we found that a notable number of patients had normal systolic and diastolic blood pressure at the admission time. This finding demonstrated that left ventricular diastolic dysfunction might be demonstrated in patients with prehypertension, and even in normotensive individuals that was also confirmed in other studies.[14,16] These findings suggest that there may be other factors affecting left ventricular diastolic dysfunction than blood pressure itself.
CONCLUSION
left ventricular hypertrophy is correlated with the severity of diastolic dysfunction manifested by E/A value and deceleration time, but inappropriate left ventricular mass can slightly predict diastolic dysfunction severity.
ACKNOWLEDGMENTS
This study was supported by Isfafhan Cardiovascular Research Institute. The authors wish to thank the nursing staff at the Isfahan Cardiovascular Research Institute for having supported the study with their professional skilfulness.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lim YH, Lee JU, Kim KS, Kim SG, Kim JH, Lim HK, et al. Association between inappropriateness of left ventricular mass and left ventricular diastolic dysfunction: A study using the tissue doppler parameter, E/E’. Korean Circ J. 2009;39:138–44. doi: 10.4070/kcj.2009.39.4.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Simone G, Daniels SR, Kimball TR, Roman MJ, Romano C, Chinali M, et al. Evaluation of concentric left ventricular geometry in humans: Evidence for age-related systematic underestimation. Hypertension. 2005;45:64–8. doi: 10.1161/01.HYP.0000150108.37527.57. [DOI] [PubMed] [Google Scholar]
- 3.Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: A consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–50. doi: 10.1093/eurheartj/ehm037. [DOI] [PubMed] [Google Scholar]
- 4.Kuznetsova T. Prevalence of Left Ventricular Diastolic Dysfunction in a General Population. Circulation: Heart Failure. 2009;2:105–12. doi: 10.1161/CIRCHEARTFAILURE.108.822627. [DOI] [PubMed] [Google Scholar]
- 5.Rusconi C. Diastolic function of the left ventricle and congestive heart failure with normal systolic function. Ital Heart J Suppl. 2000;1:1273–80. [PubMed] [Google Scholar]
- 6.Sarrafzadegan N, Sadri GH, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Programme: A comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 7.Shemirani H, Separham K. The relative impact of smoking or hypertension on severity of premature coronary artery disease. Iran Red Cresent Med J. 2007;9:177–81. [Google Scholar]
- 8.Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Bonzi B, et al. Inappropriate left ventricular mass changes during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension. 2007;49:1077–83. doi: 10.1161/HYPERTENSIONAHA.107.087320. [DOI] [PubMed] [Google Scholar]
- 9.De Simone G, Verdecchia P, Pede S, Gorini M, Maggioni AP. Prognosis of Inappropriate Left Ventricular Mass in Hypertension. Hypertension. 2002;40:470–6. doi: 10.1161/01.hyp.0000034740.99323.8a. [DOI] [PubMed] [Google Scholar]
- 10.Marshall AC, Lock JE. Structural and compliant anatomy of the patent foramen ovale in patients undergoing transcatheter closure. Am Heart J. 2000;140:303–7. doi: 10.1067/mhj.2000.108236. [DOI] [PubMed] [Google Scholar]
- 11.Sohn DW, Choi YJ, Oh BH, Lee MM, Lee YW. Estimation of left ventricular end-diastolic pressure with the difference in pulmonary venous and mitral A durations is limited when mitral E and A waves are overlapped. J Am Soc Echocardiogr. 1999;12:106–12. doi: 10.1016/s0894-7317(99)70122-7. [DOI] [PubMed] [Google Scholar]
- 12.Gökçe M, Karahan B, Erdöl C, Kasap H, Ozdemirci S. Left ventricular diastolic function assessment by tissue Doppler echocardiography in relation to hormonal replacement therapy in postmenopausal women with diastolic dysfunction. Am J Ther. 2003;10:104–11. doi: 10.1097/00045391-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I: Diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105:1387. doi: 10.1161/hc1102.105289. [DOI] [PubMed] [Google Scholar]
- 14.Kurokawa S, Okuri H, Sasaoka T, Machida Y, Osada K, Kikawada R. Doppler echocardiographic method to determine early and late diastolic filling volume separately. Validation and relationship between filling velocity and volume. Jpn Heart J. 1998;39:489–501. doi: 10.1536/ihj.39.489. [DOI] [PubMed] [Google Scholar]
- 15.Ahn HS, Kim SJ, Kim MK, et al. The difference of left ventricular hypertrophy and diastolic function between prehypertensives and normotensives. Korean Circ J. 2006;36:437–42. [Google Scholar]
- 16.Cho KI, Park JH, Lee CK, et al. Isolated and combined influences of diabetes and hypertension on the myocardial function and geometry. Korean Circ J. 2006;36:411–7. [Google Scholar]
- 17.Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–63. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]


