Abstract
Objective:
The prevalence of anemia in HIV infected patients has not been well characterized in Iran. This study aimed to describe the prevalence of anemia and related factors in HIV positive patients.
Materials and Methods:
In a cross-sectional study, anemia prevalence and risk factors of 212 HIV positive patients were assessed, at the behavioral disease consulting center in Isfahan. The relationship between anemia, demographic variables, and clinical histories were analyzed. Mild to moderate anemia was defined as hemoglobin 8–13 g/dL for men and 8–12 g/dL for women. Severe anemia was defined as hemoglobin, 8 g/dL.
Results:
A total of 212 HIV positive patients with a mean±SD age of 36.1 ± 9.1 years were assessed. We found that hemoglobin levels were between 4.7 and 16.5 gr/dL. In this study, the overall prevalence of anemia was 71%, with the majority of patients having mild to moderate anemia. Mild to moderate anemia and severe anemia occurred in 67% and 4% of patients, respectively. The mean absolute CD4 count was 348 ± 267.8 cells/cubic mm. Sixty one of 212 patients were at late stage of HIV infection (males=51 and female=10). Of the 212 HIV positive patients enrolled, 17 (8%) had a positive history of tuberculosis. We found a strong association between anemia and death.
Conclusion:
Normocytic anemia with decreased reticulocyte count was the most common type of anemia in overall. Prevalence of anemia in this study is relatively higher than other similar studies. Such a high prevalence of anemia needs close monitoring of patients on a zidovudine-based regimen. Better screening for anemia and infectious diseases, and modified harm reduction strategy (HRS) for injection drug users are primary needs in HIV seropositive patients.
Keywords: AIDS, anemia, HIV positive
INTRODUCTION
Immediately after the first reports of the acquired immunodeficiency syndrome (AIDS) cases, cytopenias of all major blood cell lines were increasingly recognized in patients with HIV infection. Anemia is the most common hematologic abnormality associated with HIV infection, affecting 60% to 80% of patients in late- stage disease. While anemia may manifest as a mere laboratory abnormality in some individuals, others may experience typical symptoms (e.g., fatigue, dyspnea, reduced exercise tolerance, and diminished functional capacity) directly related to a reduction in hemoglobin concentration.[1] The pathophysiology of HIV-associated anemia may involve three basic mechanisms: decreased RBC production, increased RBC destruction, and ineffective RBC production. Generally these include bone marrow infiltration by neoplasm or infections, a decreased production of endogenous erythropoietin, hemolytic anemia, use of myelosuppressive medications such as zidovudine (ZDV), or development as a result of the use of numerous medications. Anemia may also result from nutritional deficiencies – most commonly, deficiencies in iron, folic acid, or vitamin B12. Vitamin B12 deficiency may result from malabsorption in the ileum or from gastric pathology caused by an array of infections or other conditions that affect the gastric mucosa in HIV-infected patients in patients with HIV disease, folic acid deficiency is generally caused by either dietary deficiency or jejunal pathology.[2]
Owiredu et al. reported that highly active antiretroviral therapy-HAART may increase serum B12 levels and patients with low serum B12 in their study did not display characteristic findings of vitamin B12 deficiency, namely macrocytic anemia and neuropathy.[3] Anemia decreases survival, independently (hazard ratio 2.6, 95% CI 1.9–3.4) accelerates disease progression, and increases mortality among HIV-infected individuals. Few studies have characterized this problem in developing countries.[4,5] In a review of more than 32 000 patients infected with HIV, the yearly incidence of developing anemia increased with disease progression, affecting 3% of all patients with asymptomatic HIV infection, 12% of asymptomatic patients with CD4 cell counts <200/μL, and 37% of patients with an AIDS-related illness.[6] The association between anemia and decreased survival has been found to be independent of CD4+, T-lymphocyte count, and plasma HIV RNA concentration. Anemic HIV-infected people who recover from anemia have better survival rates than those who do not recover.[7–11] Risk of anemia increased by African American race, age, body mass index, history of pneumonia, oral candidacies, history of fever, ZDV use, low CD4+ cells counts (<200 cells/mL), and higher HIV-1 RNA levels in plasma.[5,12,13] ZDV has been reported as a cause of hematological disorders, especially anemia,[14,15] that most often occurs within 4 to 12 weeks of ZDV initiation.[16,17]
This study was conducted to investigate the prevalence of anemia and its related factors in patients with HIV positive in Isfahan, Iran.
MATERIALS AND METHODS
This single-center population-based study was conducted in year 2010. Prevalence of anemia and correlated factors in total registered patients of 212 HIV positive were assessed, at the counseling center for behavioral diseases in Isfahan, Iran. The enrolled patients with HIV infection were subjects who tested with the enzyme-linked immuno-absorbent assays (ELISA) that were confirmed using the Western blot test. The study was approved by the medical university's ethics committee Isfahan University of Medical Sciences.
Laboratory and demographic data collected in the counseling center for behavioral disease such as hemoglobin, mean corpuscular volume-MCV, CD4 count, age, sex, marital status, education level, drug history (antiretroviral or nonantiretroviral and prophylactic), past medical history (treatment or documented infection with hepatitis B virus- HBV, hepatitis C virus-HCV, and mycobacterium tuberculosis), stage of the infection HIV, and AIDS based on statement of WHO stage IV HIV disease[18] and high-risk behaviors for HIV acquisition. Additional biochemical tests of serum ferritin, reticulocyte count, and serum level of B12 and folic acid were carried out for 50 available patients with anemia (41 men and 9 women).
Mild to moderate anemia was defined as hemoglobin 8–13 and 8–12 g/dL in men and women patients, respectively. Severe anemia was defined as hemoglobin ≤ 8 g/dL. Univariate comparisons between patients with anemia and patients without anemia were performed using Fisher's exact, Mann–Whitney, and logistic regression analysis tests. All tests of significance were two sided, and a P-value of less than 0.05 was considered significant using the statistical software SPSS version 18 for Windows.
RESULTS
We enrolled a total of 212 HIV positive cases, (males=179 (84.8%)) with a mean±SD age of 36.2 ±9.1 years (males=36.8± 8.5 years; females=32.9± 11.2 years). In these cases 126 (77.8%) were illiterate or had elementary education, 36 (22.2%) had high-school or university education. Demographic and laboratory data are summarized in [Table 1]. The rates (%) of injection drug users (IDU) and having homosexual and/ or heterosexual contact were 123/151 (81.5%) and 88/106 (83%), respectively. However, there were 61 and 106 patients missing information about the mentioned risk factors, respectively. From 98 patients, who answered the questions regarding the two risk factors, 61 (62.2%) responded positive to both of them.
Table 1.
Comparison of demographic and laboratory data between anemic and nonanemic HIV/AIDS patients
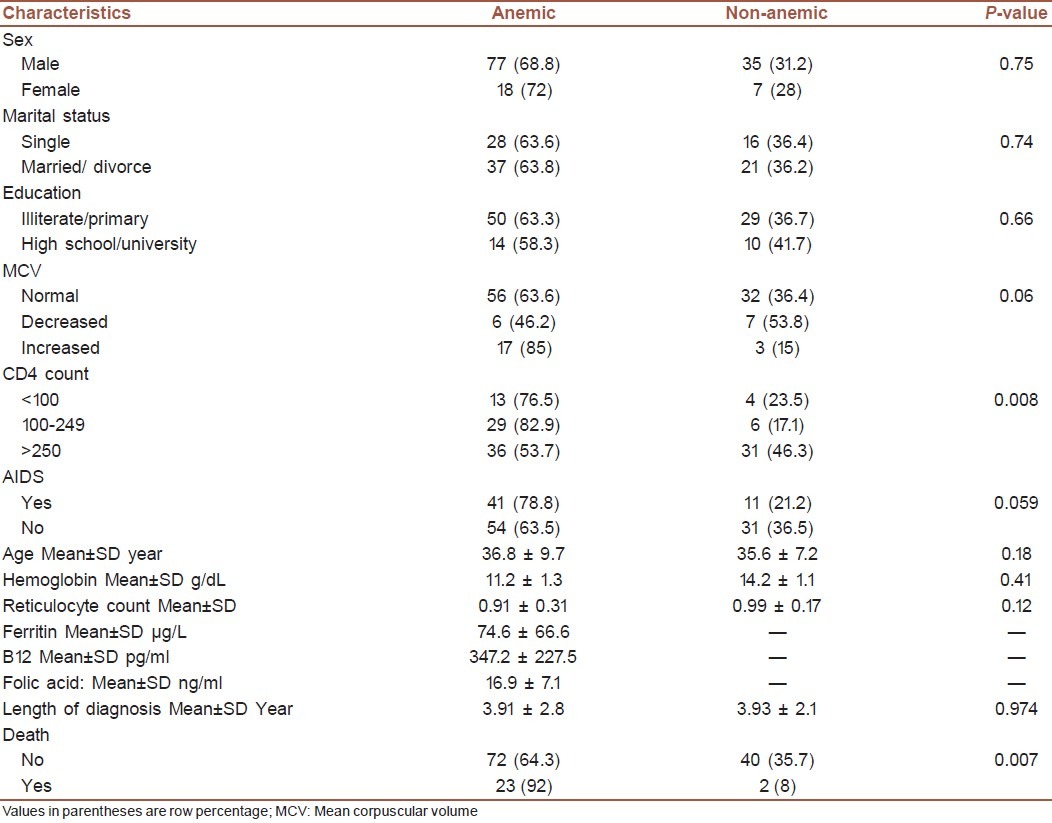
It was difficult to define precisely the timing of HIV infection acquisition but according to the time of diagnosis, Mean ± SD of duration of HIV diagnosis in anemic patients was 3.91±2.8 years and in nonanemic patients was 3.92±2.1 years, but this difference was not significant (P- value=0.74).
The overall prevalence of anemia was 71%, with the majority of patients having mild to moderate anemia. Mild to moderate anemia and severe anemia occurred in 67% and 4% patients, respectively.
Hemoglobin levels of the patients were between 4.7 and 16.5 g/dL. Mean ± SD of hemoglobin in anemic and nonanemic patients were 11.2 ± 1.3 and 14.22 ± 1.1 g/dL, respectively. However, the difference was not statistically significant (P-value = 0.41). Microcytosis was more common in women than men (19% vs. 15%; P-value=0.418). In this study, 88 (72.7%) anemic patients were normocytic with decreased reticulocyte (men = 74.3%, women = 62%). Twenty (16.5%) and 13 (10.7%) have microcytic anemia and macrocytic anemia, respectively.
The mean±SD absolute CD4 count was 348 ± 267.8 cells/ cubic mm (range 8–1594). Generally 54 patients had used ZDV (600 mg daily). In ZDV users 43(79.6%) were anemic (P-value=0.38).
Out of 212 patients, 75 patients missed to provide the CBC test. Of all anemic patients 40% had iron (ferritin<30 μg/L) and 23% had vitamin B12 (<200 pg/mL) deficiencies. There was no patient with folic acid deficiency (<6 ng/mL). Mean ± SD of folic acid, vitamin B12 and ferritin in anemic patient were 16.9 ± 7.1 ng/mL, 347.2 ± 227.5 pg/mL and 74.6 ± 66.6 μg/L, respectively.
Treated patients received triplet therapy included ZDV, Plus lamivudine, and Efavirenz except for 4% of treated patients that ZDV was replaced by stavudine. All patients with CD4<200 cells/μL received Co-trimoxazole in order to Toxoplasmosis prophylaxis. None of patient receivedanti-HCV therapy.
In addition, 57/212 (26.9%) of the cohort received ZDV (600 mg daily), 37/212 (17.5%) co-trimoxazole (SD tablet per 12 h), and 7/212 (3.3%) capsule fluconazole (100-200 mg daily). 41/57 (71.9%) and 27/36 (75.0%) of patients who took, respectively, ZDV and co-trimoxazole were anemic.
From 212 HIV positive patients enrolled, 61 (28.8%) were at a late HIV stage (AIDS), (males = 51 and female = 10). Out of 61 cases who were diagnosed as AIDS, 16 (26.2%) had CD4>200 cells/μL. However, because of oral trush or recurrent pneumonia allocated to the AIDS stage IV of HIV group. Anemia was more common in AIDS patients (41/52 (78.8%)) than others, this difference was marginally significant (P-value=0.055).
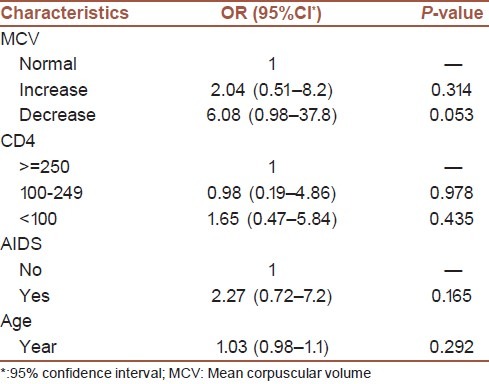
We found a strong association between anemia and death (P-value=0.007). In addition, the logistic regression was conducted to check the related factors with anemia. The variables that had the P-value more than 0.3 in the initial analysis were selected to enter the model. Goodness of fitting logistic regression was checked using the Hosmer and Lemeshow test. The chi-square test (8 degrees of freedom) was X2(8)=6.37 (P-value=0.606). The risk of anemia in the increased and decreased MCV were about two and six times more than the normal MCV, respectively, but not statistically significant (OR=2.04 and 6.08, respectively). More information has been shown in [Tables 1 and 2].
Table 2.
Summarized results of fitting logistic regression to 99 HIV/AIDS patients
DISCUSSION
Anemia is a frequent complication of infection with the human immunodeficiency virus type 1 (HIV-1), and could be clinically important. Multifactorial origin of anemia complicates determining its original cause and/or its proper treatment.[19] The prevalence of anemia in this study was 71% that was significantly higher than prevalence of anemia reported in similar studies not only in Iran but also in other countries.[20,21] In Iran, Ramezani et al. (2008) reported that mild anemia occurred in 46% of subjects while severe anemia was not observed.[22] In a study on 642 Iranian HIV positive patients, Jabbari et al. reported that the prevalence of anemia (defined as hemoglobin<10 mg/dL) was 10.3%.[23] Chakravarty et al. studied on 1256 patients ZDV; 203 (16.2%) (143 females) developed anemia (<8 g/dL). Severe anemia (<6.5 g/dL) was documented in 100 (7.9%) patients.[24]
A peripheral smear should be examined as it provides a great deal of information on cell morphology and can give clues to the cause of the alteration in hematopoiesis. According to our study normocytic, anemia with decreased reticulocyte count is the most common form of anemia in HIV positive patients in Isfahan. This form of anemia may be caused by medication toxicity, viral suppression, marrow infiltration by malignancy, mixed nutritional deficiencies, and chronic infections. Mata-Marin et al. reported normocytic normochromic anemia as the most common form of anemia (85%) in HIV positive patients, and in their study there was no case of macrocytic anemia.[25] In Iran, Jabbari et al. reported macrocytosis in 11%, normocytosis plus normochromia in 41.1%, and microcytosis plus hypochromia in 47.9% of the patients.[21] Chakravarty et al. reported a normocytic, normochromic picture in 42% of the patients and others showed macrocytic changes.[23]
We found anemia is slightly more common in women than men. Wills et al. and Diallo et al. showed that anemia was more frequent in women than in men.[26,27] Jabbari et al. reported borderline relationship between female sex and anemia and CD4 level (CD4 count of <200).[23] Mildvan et al. studied prevalence of anemia in 9690 HIV infected patients, and showed 39.5% (1721) of patient receiving no antiretroviral therapy and 35.5% (7252) of patients receiving HAART were anemic. They found anemia was more prevalent among men and patients with CD4<200 cells/mm3.[28] Mata-Marin et al. in a cross-sectional study in the Mexican population (54 men and 9 women) with no antiretroviral therapy, found anemia, and severe anemia in 20.3% and 1.58% of the patients, respectively.[25]
The proportion of anemia produced by iron deficiency may be underestimated in our study because the diagnosis of iron deficiency was based only on ferritin concentration. Ferritin is an acute phase protein, which is elevated in cases of infections.
Moore et al. analyzed data from 905 patients, and found HAART is an effective treatment of the anemia of HIV infection.[29]
Kiragaa and colleges in a study on 5494 patients suggest that baseline severe anemia (Hb ≤8 g/dL) should not be used as a criterion for avoiding the use of ZDV in initiating HAART in resource-limited settings.[20] They found early severe anemia occurred in 4% of patients during the first 6 months on ART, and baseline severe anemia OR = 5.27 (95% CI 3.00–9.26) associated with early severe anemia. Injection drug use was an independent risk factor for iron deficiency anemia among HIV positive cases.[30] We found anemia was more common in patients with advanced stages of disease (AIDS) rather than in HIV infection itself. Anemia is a predictor of death in HIV positive patients.[31,32] In our study, there was a strong association between anemia and death.
The main limitations of our study include lack of measurement in erythropoietin levels, viral load and parvovirus IgM titers and also relatively moderate to high amount of missing data of the cohort.
Prevalence of anemia in this study is relatively higher than other similar studies. Such a high prevalence of anemia needs close monitoring of patients on a ZDV-based regimen especially in women, IDUs and patients receiving drugs with bone marrow suppressant effect such as cotrimoxazole. Normocytosis with decreased reticulocyte is the most common form of anemia in Isfahan and may be due to medical toxicity, chronic infections, or mixed nutritional deficiency. Better screening for anemia and infectious diseases, and modified harm reduction strategy (HRS) for IDUs (especially in women) are the primary needs in HIV seropositive patients in Isfahan.
ACKNOWLEDGMENTS
We thank the Vice-Chancellor for Health of Isfahan University of medical sciences and members of Counseling center for behavioral diseases in Isfahan for their co-operations.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zon LI, Arkin C, Groopman JE. Haematologic manifestations of the human immunodeficiency virus (HIV) Br J Haematol. 1987;66:251. doi: 10.1111/j.1365-2141.1987.tb01307.x. [DOI] [PubMed] [Google Scholar]
- 2.Volberding PA, Levine AM, Dieterich D, Mildvan D, Mitsuyasu R, Saag M for the Anemia in HIV Working Group. Anemia in HIV Infection: Clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38:1454–63. doi: 10.1086/383031. [DOI] [PubMed] [Google Scholar]
- 3.Owiredu WKBA, Quaye L, Amidu A, Addai-Mensah O. Prevalence of anemia and immunological markers among Ghanaian HAART-naïve HIV-Patients and those on HAART. Afr Health Sci. 2011;11:2–15. [PMC free article] [PubMed] [Google Scholar]
- 4.Subbaraman R, Devaleenal B, Selvamuthu P, Yepthomi T, Solomon SS, Mayer KH, et al. Factors associated with anemia in HIV-infected individuals in southern India. Int J STD AIDS. 2009;20:489–92. doi: 10.1258/ijsa.2008.008370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berhane K, Karim R, Cohen MH, et al. Impact of Highly Active Antiretroviral Therapy on Anemia and Relationship Between Anemia and Survival in a Large Cohort of HIV-Infected Women: Women's Interagency HIV Study. J Acquir Immune Defic Syndr. 2004;37:1245. doi: 10.1097/01.qai.0000134759.01684.27. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: Results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91:301–8. [PubMed] [Google Scholar]
- 7.Buskin S, Sullivan P. Anemia and its treatment and outcomes in persons infected with human immunodeficiency virus. Transfussion. 2004;44:826–32. doi: 10.1111/j.1537-2995.2004.03359.x. [DOI] [PubMed] [Google Scholar]
- 8.Moses A, Nelson J, Bagby G. The Influence of Human Immunodeficiency Virus-1 on hematopoiesis. Blood. 1998;91:1479–95. [PubMed] [Google Scholar]
- 9.Koduri PR, Signa P, Nikolinakos P. Autoimmune hemolytic anemia in patients infected with human immunodeficiency virus-1. Am J Hematol. 2002;70:174–6. doi: 10.1002/ajh.10096. [DOI] [PubMed] [Google Scholar]
- 10.Belperio PS, Rhew DC. Prevalence and outcomes of anemia in individuals with human immunodeficiency virus: A systematic review of the literature. Am J Med. 2004;116(Suppl 7A):27S–43S. doi: 10.1016/j.amjmed.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Bain BJ. Pathogenesis and pathophysiology of anemia in HIV infection. Curr Opin Hematol. 1999;6:89–93. doi: 10.1097/00062752-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Levine AM, Berhane K, Masri-Lavine L, Sanchez M, Young M, Augenbraun M, et al. Prevalence and correlates of anemia in a large cohort of HIV-infected women: Women's Interagency HIV Study. J Acquir Immune Defic Syndr. 2001;26:28–35. doi: 10.1097/00126334-200101010-00004. [DOI] [PubMed] [Google Scholar]
- 13.Semba RD, Shah N, Klein RS, Mayer KH, Schuman P, Vlahov D, et al. Prevalence and cumulative incidence of and risk factors for anemia in a multicenter cohort study of human immunodeficiency virus-infected and -uninfected women. Clin Infect Dis. 2002;34:260–6. doi: 10.1086/338151. [DOI] [PubMed] [Google Scholar]
- 14.Richman DD, Fischl MA, Grieco MH, Gottlieb MS, Volberding PA, Laskin OL, et al. The toxicity of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS related complex. A double-blind, placebo-controlled trial. N Engl J Med. 1987;317:192–7. doi: 10.1056/NEJM198707233170402. [DOI] [PubMed] [Google Scholar]
- 15.Volberding PA, Lagakos SW, Koch MA, Pettinelli C, Myers MW, Booth DK, et al. Zidovudine in asymptomatic human immunodeficiency virus infection. A controlled trial in persons with fewer than 500 CD4-positive cells per cubic millimeter. The AIDS Clinical Trials Group of the National Institute of Allergy and Infectious Diseases. N Engl J Med. 1990;322:941–9. doi: 10.1056/NEJM199004053221401. [DOI] [PubMed] [Google Scholar]
- 16.Ssali F, Stohr W, Munderi P, Reid A, Walker AS, Gibb DM, et al. Prevalence, incidence and predictors of severe anaemia with zidovudine-containing regimens in African adults with HIV infection within the DART trial. Antivir Ther. 2006;11:741–9. doi: 10.1177/135965350601100612. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmann CJ, Fielding KL, Charalambous S, Sulkowski MS, Innes C, Thio CL, et al. Antiretroviral therapy using zidovudine, lamivudine, and efavirenz in South Africa: tolerability and clinical events. AIDS. 2008;22:67–74. doi: 10.1097/QAD.0b013e3282f2306e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hare CB. WHO Staging System for HIV Infection and Disease in Adolescents and Adults, Table 3; Clinical Overview of HIV Disease. In: Peiperl L, Coffey S, Volberding PA, editors. HIV InSite Knowledge Base [textbook online] San Francisco: UCSF Center for HIV Information; 2006. [Last accessed on 2006 Mar 23]. Available from: http://www.hivinsite.ucsf.edu/InSite?page=kb-03-01-01 . [Google Scholar]
- 19.Kreuzer KA, Rockstroh JK. Pathogenesis and pathophysiology of anemia in HIV infection. Ann Hematol. 1997;75:179–87. doi: 10.1007/s002770050340. [DOI] [PubMed] [Google Scholar]
- 20.Kiragga AN, Castelnuovo B, Nakanjako D, Manabe YC. Baseline severe anaemia should not preclude use of zidovudine in antiretroviral-eligible patients in resource-limited settings. J Int AIDS Soc. 2010;13:42. doi: 10.1186/1758-2652-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore RD, Creagh-Kirk T, Keruly J, Link G, Wang MC, Richman D, et al. Long-term safety and efficacy of zidovudine in patients with advanced humanimmunodeficiency virus disease. Zidovudine EpidemiologyStudy Group. Arch Intern Med. 1991;151:981–6. [PubMed] [Google Scholar]
- 22.Ramezani A, Aghakhani A, Sharif MR, Banifazl M, Eslamifar A, Velayati AK. Anemia Prevalence and Related Factors in HIV- Infected Patients: A Cohort Study. Iran J Pathol. 2008;3:125–8. [Google Scholar]
- 23.Jam S, Ramezani A, Sabzvari D, Moradmand-Badie B, Seyedalinaghi SA, Jabbari H, et al. A cross-sectional study of anemia in human immunodeficiency virus-infected patients in Iran. Arch Iran Med. 2009;12:145–50. [PubMed] [Google Scholar]
- 24.Agarwal D, Chakravarty J, Chaube L, Rai M, Agrawal NR, Sundar SH. High incidence of zidovudine induced anaemia in HIV infected patients in eastern India. Indian J Med Res. 2010;132:386–9. [PubMed] [Google Scholar]
- 25.Mata-Marín JA, Gaytán-Martínez JE, Martínez-Martínez RE, Arroyo-Anduiza CI, Fuentes-Allen JL, Casarrubias-Ramirez M. Risk factors and correlates for anemia in HIV treatment-naïve infected patients: A cross-sectional analytical study. BMC Res Notes. 2010;3:230. doi: 10.1186/1756-0500-3-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Diallo DA, Baby M, Dembélé M, Kéita A, Sidibé AT, Cissé IA, et al. Frequency, risk factors, and prognostic value of anemia associated with HIV/AIDS in the adult in Mali. Bull Soc Pathol Exot. 2003;96:123–7. [PubMed] [Google Scholar]
- 27.Wills TS, Nadler JP, Somboonwit C, Vincent A, Leitz G, Marino K, et al. Anemia prevalence and associated risk factors in a single- center ambulatory HIV clinical cohort. AIDS Read. 2004;14:305–10. 313-5. [PubMed] [Google Scholar]
- 28.Mildvan D, Creagh T, Leitz G. Prevalence of anemia and correlation with biomarkers and specific antiretroviral regimens in 9690 human-immunodeficiency-virus-infected patients: findings of the Anemia Prevalence Study. Curr Med Res Opin. 2007;23:343–55. doi: 10.1185/030079906X162683. [DOI] [PubMed] [Google Scholar]
- 29.Moore RD, Forney D. Anemia in HIV-infected patients receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;29:54–7. doi: 10.1097/00042560-200201010-00007. [DOI] [PubMed] [Google Scholar]
- 30.Dancheck B, Tang AM, Thomas AM, Smit E, Vlahov D, Semba RD. Injection drug use is an independent risk factor for iron deficiency and iron-deficiency anemia among HIV-seropositive and HIV-seronegative women. J Acquir Immune Defic Syndr. 2005;40:198–201. doi: 10.1097/01.qai.0000165909.12333.07. [DOI] [PubMed] [Google Scholar]
- 31.Johannessen A, Naman E, Ngowi BJ, Sandvik L, Matee MI, Aglen HE, et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008;8:52. doi: 10.1186/1471-2334-8-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saah AJ, Hoover DR, He Y, Kingsley LA, Phair JP. Factors influencing survival after AIDS: report from the Multicenter AIDS Cohort Study (MACS) J Acquir Immune Defic Syndr. 1994;7:287–95. [PubMed] [Google Scholar]


