Abstract
Introduction:
The metabolic syndrome has known as an independent risk factor of stroke. The occurrence of this syndrome is due to genetic factors and lifestyle. This study was performed on the frequency of metabolic syndrome prevalence in ischemic stroke patients compare to control.
Materials and Methods:
one hundred ischemic stroke patients and 100 controls (with the same age and sex) were evaluated for this study.
Result:
62% of patient and 34% of controls had metabolic syndrome criteria according to National Cholesterol Education Program (NCEP) {OR: 3.2; 95% CI (1.9–9.7), P=0.001} Prevalence of metabolic syndrome in women was more than men (52% vs. 44%) {OR: 0.72; 95% CI (0.4, 1.3)}. Beside of metabolic syndrome, prevalence of metabolic syndrome components was significantly higher in stroke patients compare to controls.
Conclusion:
metabolic syndrome prevalence are more common in stroke patients compare to controls, but it should be noticed that the controls are in a risk of future stroke so they need special treatment to prevent it.
Keywords: Metabolic syndrome, prevalence, stroke
INTRODUCTION
Stroke is the most common reason of disability affects of more than 700 000 individuals and the third cause of death in the world per year.[1] The ischemic stroke risk factors are classified as modifiable and unmodifiable ones and include arterial hypertension, diabetes mellitus dyslipidemia, cigarette smoking, alcohol consumption, oldness, male gender, etc. Furthermore, metabolic syndrome (MetS) is known as an independent risk factor of CAD and stroke either.[2,3] The MetS rate depends on genetic and nongenetic[4,5] and the metabolic syndrome characterizes by cluster of risk factors including obesity,insulin resistance, hypertension, hypertriglyceridemia and low HDL cholesterol.[6] Hwang IC et al. demonstrated that according to NECP criteria FBS was the most important factor of increasing cardiovascular disease.[7] Intrinsically the frequency of MetS in the United States is more than 47 million individuals and it increases with age for instance 6.7% in 20–29 years old compare to 43.5% in 60–69 ones.[7]
MetS is associated with different kind of diseases such as development of myocardial ischemia, ischemic stroke, extra and intracranial atherosclerotic, and asymptomatic carotid atherosclerotic plaques.[8–12]
Some studies showed that lifestyle can affect on the MetS occurrence, so the risk of ischemic stroke decreases consequently by changing it; however, Safarzadegan et al. showed there was no significant correlation between lifestyle and MetS.[13,14]
So to identify the MetS rate, lifestyle changing and medical treatment decrease the stroke attack.[11]
This study was preformed to evaluate the metabolic syndrome rate in ischemic stroke patients compare to controls
MATERIALS AND METHODS
This case-control study was performed from 2008 to 2009 in neurology ward of Alzahra hospital, Isfahan.
One hundred ischemic stroke patients were enrolled randomly among the patients of neurologic ward. Ischemic stroke diagnosis was made by neurologist and confirmed by brain CT scan in more than 45-years old patients. Exclusion criteria were past history of previous stroke or using Statins during past three months and sever cardiorenal or nutritional disorder that would affect blood pressue or lipid and glucose. One hundred controls with the same sex and age that had negative history of cerebrovascular disease and myocardial infarction were recruited.
After taking an informed written consent, conforming to the current revision of the declaration of Helsinki from the patients or their relatives the baseline data were collected by questionnaire. The Ethical Review Committee of Isfahan University of Medical Sciences approved the study protocol.
Blood pressure was measured after 48 h of initiation symptoms and repeated two times by 10-min interval, in calm and comfortable situation.
FBS, TG, and HDL were measured 72 h after admission under a fast condition.
Waist circumference was measured by tape-measure from 10 cm above anterior superior iliac spine (ASIS).
Definition of metabolic syndrome
We used revised National Cholesterol Education Program (NCEP) criteria for definition of the metabolic syndrome, patients who had three of following symptoms suffered from metabolic syndrome:
Abdominal obesity (waist circumference >90 cm for men or >80 cm for women).
Triglycerides >150 mg/dL.
HDL <40 mg/dL for men or <50 mg/dL for women.
Systolic blood pressure >130 or diastolic blood pressure >85 mmHg.
FBS > 100 mg/dL or receiving antihypertensive treatment.
Statistical analysis
Data were analyzed by SPSS version 16.0; chi-square test and t-student were used for Comparisons between two groups.
RESULTS
In each group 50% of subjects were male and 50% were female, mean age was 62.24(±9.9) in case group and 61.24(±8.5) in controls. Sixty-two percent of patients and 34% of controls had metabolic syndrome criteria according to NCEP {OR: 4.3CI (1.9, 9.7), P=0.001}.
Totally prevalence of MetS in women was more than men (52% vs. 44%) but there is no significant difference between them {OR: 0.72 CI (0.14, 1.3)}.
Mean average of fasting blood glucose was 132.66 (±53.03) in patients and 103.01(±27.681) in controls (P-value =0.001).
Fifty-seven percent of patients and 23% of controls had FBS higher than 110 (P-value =0.001) [Table 1].
Table 1.
Characteristics of patients and controls
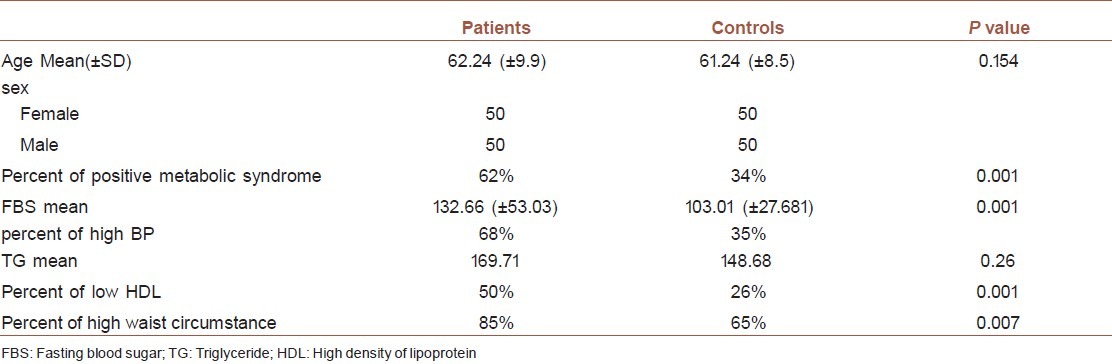
Mean average of TG was 169.71 in patients and 148.68 in controls (P-value =0.26).
The HDL level in patients was significantly lower than control (50% vs. 26%) (P-value =0.001).
Waist circumstance quantify in patients were higher than controls, 85% of patients and 65% of controls had high waist circumference (P-value= 0.007).
Sixty-eight percent of patients and 35% of controls had hypertension (P-value =0.001) [Table 1].
Prevalence of smoking is higher in patients {OR: 4.3 CI (1.9, 9.7)}
DISCUSSION
The result of our study showed significant differences in metabolic syndrome among stroke patients and controls in Isfahan.
Although it is not clear how MetS can increase the rate of CVD and its mechanism is in doubt but MetS is known as a CVD independent risk factor and associates with high risk of CVD events in ischemic stroke patients in many studies. Liu suggested a dose–response correlation between MetS components and risk of CVD event.[15,16]
In our study generally metabolic syndrome was higher in stroke patients but different components of this syndrome were significantly high either.
Prevalence of hypertension was significantly high in stroke patients compare to controls (68% vs. 35%) and FBS measurement was more (>110) in stroke patients (57%) than in controls (23%).
Jia et al. showed that the metabolic syndrome was associated with first-ever stroke in middle-aged and elderly, but blood pressure was more significantly than metabolic syndrome in this patients,[17] in other study in Korea, Hwang et al. demonstrated that metabolic syndrome and FBS were the highest predicting factors of CVD.[6]
Generally in this study, it was demonstrated that the frequency of MetS in women was not more than men, like other studies (most of them) the correlation of CVD and MetS proved in both gender. Moreover, male patients with the metabolic syndrome had higher mortality than others, even in the absence of CVD baseline and diabetes.[18]
Our finding consists other studies that showed more important roles of metabolic syndrome and higher risk of stroke in MetS patients in both gender compare to controls[14] according to these studies, the frequency of stroke, CHD, and MI diseases became three times higher than others.[19]
As MetS increases intracranial atherosclerosis so can be associated with higher risk of stroke, Ovbiagele et al. showed that half of patients with symptomatic intrac ranial atherosclerotic disease had metabolic syndrome.[20] On the other hand, prevalence of brain silent ischemic lesions increases in MetS independent of other risk factors.[21,22]
The metabolic syndrome is currently more frequent and a large number of people in worldwide are in danger[13,16]; therefore, it is necessary to pay attention about the frequency of this syndrome in different part of world in order to control the CVD prevalence, especially in the elderly.[23,24]
CONCLUSION
As the frequency of metabolic syndrome in stroke patients is higher than controls, it is important to change the lifestyle in order to control this syndrome.
ACKNOWLEDGEMENTS
We extend our thanks to the Isfahan Neuroscience research centre and Isfahan Endocrine and Metabolism Research Center.
Obesity: waist circumference above 90 cm in men and 88 cm in women
Insulin resistance: FBS more than or equal 100 mg/dL.
Hypertension (systolic blood pressure more than 130 mmHg and diastolic blood pressure greater than 85 mmHg).
Hypertriglyceridemia: above 150 mg/dL.
HDL cholesterol: less than 40 mg/dL in male and less than 50 mg/dL in female.
Footnotes
Source of Support: This study supported by Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Air EL, Kissela BM. Diabetes, the metabolic syndrome, and ischemic stroke: Epidemiology and possible mechanisms. Diabetes Care. 2007;30:3131–40. doi: 10.2337/dc06-1537. [DOI] [PubMed] [Google Scholar]
- 2.Soler EP, Ruiz VC. Epidemiology and risk factors of cerebral ischemia and ischemic heart diseases: Similarities and differences. Curr Cardiol Rev. 2010;6:138–49. doi: 10.2174/157340310791658785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cortez-Dias N, Martins S, Belo A, Fiuza M. Comparison of definitions of metabolic syndrome in relation to risk for coronary artery disease and stroke. Rev Port Cardiol. 2011;30:139–69. [PubMed] [Google Scholar]
- 4.AO Konradi, Rotar OP, Korostovtseva LS, Ivanenko VV, Solntcev VN, Anokhin SB, et al. Prevalence of Metabolic Syndrome Components in a Population of Bank Employees from St. Petersburg, Russia. Metab Syndr Relat Disord. 2011;9:337–43. doi: 10.1089/met.2011.0028. [DOI] [PubMed] [Google Scholar]
- 5.Vassy JL, Shrader P, Yang Q, Liu T, Yesupriya A, Chang MH, et al. Genetic associations with metabolic syndrome and its quantitative traits by race/ethnicity in the United States. Metab Syndr Relat Disord. 2011;9:475–82. doi: 10.1089/met.2011.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hwang IC, Kim KK, Jee SH, Kang HC. A comparison of predictability of cardiovascular events between each metabolic component in patients with metabolic syndrome based on the revised National Cholesterol Education Program criteria. YonseiMed J. 2011;52:220–6. doi: 10.3349/ymj.2011.52.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 8.Al Suwaidi J, Zubaid M, El Menyar AA, Singh R, Rashed W, Ridha M, et al. Prevalence of the metabolic syndrome in patients with acute coronary syndrome in six middle eastern countries. J Clin Hypertens (Greenwich) 2010;12:890–9. doi: 10.1111/j.1751-7176.2010.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aoki J, Uchino K. Treatment of risk factors to prevent stroke. Neurotherapeutics. 2011;8:463–74. doi: 10.1007/s13311-011-0054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golden SH, Folsom AR, Coresh J, Sharrett AR, Szklo M, Brancati F. Risk factor groupings related to insulin resistance and their synergistic effects on subclinical atherosclerosis: The atherosclerosis risk in communities study. Diabetes. 2002;51:3069–76. doi: 10.2337/diabetes.51.10.3069. [DOI] [PubMed] [Google Scholar]
- 11.Grundy SM. Metabolic syndrome: Connecting and reconciling cardiovascular and diabetes worlds. J Am Coll Cardiol. 2006;47:1093–100. doi: 10.1016/j.jacc.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 12.Park JH, Kwon HM, Roh JK. Metabolic syndrome is more associated with intracranial atherosclerosis than extracranial atherosclerosis. Eur J Neurol. 2007;14:379–86. doi: 10.1111/j.1468-1331.2007.01682.x. [DOI] [PubMed] [Google Scholar]
- 13.Khang YH, Cho SI, Kim HR. Risks for cardiovascular disease, stroke, ischaemic heart disease, and diabetes mellitus associated with the metabolic syndrome using the new harmonised definition: findings from nationally representative longitudinal data from an Asian population. Atherosclerosis. 2010;213:579–85. doi: 10.1016/j.atherosclerosis.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Sarrafzadegan N, Gharipour M, Ramezani MA, Rabiei K, Zolfaghar B, Tavassoli AA, et al. Metabolic syndrome and health- related quality of life in Iranian population. J Res Med Sci. 2011;16:254–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Ding EL, Smit LA, Hu FB. The metabolic syndrome as a cluster of risk factors: Is the whole greater than the sum of its parts?: comment on “The metabolic syndrome, its component risk factors, and progression of coronary atherosclerosis”. Arch Intern Med. 2010;170:484–5. doi: 10.1001/archinternmed.2009.552. [DOI] [PubMed] [Google Scholar]
- 16.Liu C, Feng M, Fang XH, Mu LY, Liu HJ, Zhang HM, et al. [Metabolic syndrome is an independent risk factor for cardiovascular disease events in patients with ischemic stroke] Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:358–62. doi: 10.3760/cma.j.issn.0253-3758.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 17.Jia Z, Wu S, Zhou Y, Wang W, Liu X, Wang L, et al. Metabolic syndrome and its components as predictors of stroke in middle-aged and elderly Chinese people. Neurol Res. 2011;33:453–9. doi: 10.1179/016164111X13007856083882. [DOI] [PubMed] [Google Scholar]
- 18.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 19.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–9. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 20.Ovbiagele B, Saver JL, Lynn MJ, Chimowitz M. Impact of metabolic syndrome on prognosis of symptomatic intracranial atherostenosis. Neurology. 2006;66:1344–9. doi: 10.1212/01.wnl.0000210530.46058.5c. [DOI] [PubMed] [Google Scholar]
- 21.H , Yamaguchi S, Iijima K, Nagai A, Oguro H. Metabolic syndrome is associated with silent ischemic brain lesions. Stroke. 2008;39:1607–9. doi: 10.1161/STROKEAHA.107.508630. [DOI] [PubMed] [Google Scholar]
- 22.Park K, Yasuda N. Association between metabolic syndrome and minimal leukoaraiosis. Stroke. 2009;40:e5. doi: 10.1161/STROKEAHA.108.531012. [DOI] [PubMed] [Google Scholar]
- 23.Chen Q, Liu Y, Yin Y, Huang W, Li G, Ke D. Relationship between metabolic syndrome (MS) and coronary heart disease (CHD) in an aged group. Arch Gerontol Geriatr. 2008;46:107–15. doi: 10.1016/j.archger.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Gupta A, Gupta V. Metabolic syndrome: What are the risks for humans? Biosci Trends. 2010;4:204–12. [PubMed] [Google Scholar]


