Abstract
Previous observational research has indicated the effectiveness of a 12-step, dual-focus mutual aid group, Double Trouble in Recovery (DTR), for assisting individuals to recover from co-occurring substance use and psychiatric disorders. The current study extends this line of research by evaluating DTR with a quasi-experimental design; controlled designs are rare in studies of mutual aid. Patient outcomes in the same psychiatric day treatment program were compared for two consecutive admission cohorts characterized by high rates of co-occurring disorders. The first cohort did not have DTR available while the second cohort was exposed to DTR after it was established at the program. Both cohorts were assessed at program admission and at a six month follow-up. Using intent to treat analysis, the Post-DTR cohort as compared with the Pre-DTR cohort had significantly fewer days of alcohol and drug use, more frequent traditional 12-step groups outside of the program and higher psychiatric medication adherence. There were no differences in psychiatric symptoms or program retention, however. This study helps demonstrate the benefits of introducing 12-step, dual-focus mutual aid into psychiatric treatment programs that serve patients with co-occurring disorders.
Keywords: Co-occurring Disorders, Mutual Aid, Self-Help, 12-step Groups, Program Evaluation, Substance Abuse, Mental Illness, Treatment Outcomes
1. Introduction
About 5.2 million adults in the U.S. have a co-occurring substance use disorder and serious psychological distress, according to the National Survey of Drug Use and Health (1). Co-occurring disorders (COD) are more severe and chronic than single disorders (2, 3, 4, 5) and are highly predictive of poor treatment outcomes (6, 7, 8). Evidence indicates that 12-step groups, using the principles articulated by Alcoholics Anonymous [AA] (9), are useful in maintaining abstinence from substances of abuse (10, 11, 12, 13, 14) and in promoting recovery from mental illness (15, 16, 17, 18, 19, 20). But historically, traditional “single focus” 12-step groups have been underutilized by individuals with co-occurring disorders (21, 22, 23, 24). Research has also shown that clinicians are less likely to refer persons with COD than those with a substance use disorder only to traditional 12- step groups (25, 26, 27).
Traditional 12 step groups have substantial limitations for individuals with COD. Identifying and bonding with other members may be difficult for dually diagnosed individuals if they feel different from other group members. Persons with COD who are newcomers to 12-step meetings often find a lack of acceptance and empathy (21, 28). Some members with COD report receiving misguided advice about psychiatric illness and the use of medications, which are seen as “drugs” (e.g., 27, 29), although this is not the official view of AA and Narcotics Anonymous (NA) World Services (30, 31). Nevertheless, strong aversion remains against the use of psychoactive medications in local 12-step chapters, where the potential for abuse of certain medications makes any use unacceptable, whether for treatment of substance dependency or mental illness. This has concrete consequences, such as not being allowed to speak (or “testify”) at meetings. A survey of AA leaders revealed their belief that individuals should take their medications as prescribed, but most “felt that participation in a group especially [designed] for persons with a dual diagnosis would be more desirable than a traditional AA group” (32). Although there is some inconsistency in the research on participation in 12 step groups by patients with COD. (33, 34, 35), several investigators have concluded that specialized “dual focus” fellowships would be important to bringing the full benefits of 12-step mutual aid to the large population of person with COD (36, 32, 37).
Double Trouble in Recovery (DTR), a mutual aid program adapted from the 12 steps of AA, was founded in 1989 to meet the specialized needs of persons dually diagnosed with a mental illness and substance use disorder. DTR encourages members to discuss their addictions, mental illnesses, psychotropic medications, and experiences with formal treatment, without the shame or stigma they might encounter in traditional single focus 12-step groups such as AA or NA (28). Previous research has indicated that DTR affiliation is associated with increased abstinence from drugs/alcohol (38), better psychiatric medication adherence (39), and improved coping and quality of life (40). Specific self-help processes in DTR groups - helping others and mutual learning - were associated with better abstinence outcomes (41).
However, this previous research on the effectiveness of DTR was based on a naturalistic longitudinal study of DTR members recruited in existing DTR groups. The present study extends this line of research by using a quasi-experimental evaluation design. Treatment outcomes in the same program were compared for two consecutive admission cohorts of psychiatric outpatients characterized by a high rate of co-occurring disorders. The first cohort did not have a DTR group available while the second cohort was exposed to DTR after such a group was established. Both cohorts were assessed at admission to the program and at six month follow-up. The purpose of the study was to determine whether adding DTR mutual aid to a day treatment psychiatric program that primarily serves patients with COD improves patient outcomes.
2. Method
2.1. Setting
The setting was a psychiatric continuing day treatment program (CDTP) located in New York City. Patients in this program usually have a 3 times a week, half-day schedule, either in the morning or afternoon, and participate in one to four groups per day. Patients are offered breakfast and lunch on days they come to the program. The CDTP provides mental health services for persons with single psychiatric disorders as well for those dually diagnosed with psychiatric and substance use disorders. Specific groups are offered for dually diagnosed consumers, such as “Substance Abuse Awareness” and “Relapse Prevention;” more general mental health groups are offered to all consumers, such as “Coping with Mental Illness” and “Building Self Esteem.”
2.2. Study samples
Two cohorts of patients newly admitted to the CDTP were recruited, the first from March to December 2003 (termed the Pre-DTR cohort; N= 81) and the second from May 2004 to December 2005 (termed the Post-DTR cohort; N=148). The Post-DTR cohort was larger by design. Patients were referred and admitted to the CDTP from a variety of mental health and drug treatment settings, including inpatient psychiatric units, mental health residences, other outpatient mental health clinics, outpatient drug treatment clinics, or were self-referred through community contacts. Consecutive admissions to the study clinic were referred by a CDTP intake counselor to a study research assistant. CDTP patients were excluded from study participation if they were younger than age 18, did not understand or speak English, appeared intoxicated on drugs or alcohol, carried a diagnosis of mental retardation, were deemed actively psychotic by the clinic’s intake coordinator, or appeared unable to understand and give informed consent.
All patients who agreed to participate in the study signed an informed consent. Participants received compensation of $20.00 for a baseline interview and $40.00 for a 6-month follow-up interview. The study protocol was approved by the Institutional Review Boards (IRBs) of the host research site (Albert Einstein College of Medicine) and the organization that conducted the study (National Development and Research Institutes, Inc.).
2.3. Procedures
In order for the DTR group to reach a workable minimum size (6) and to avoid exposing Pre-DTR subjects to DTR, the DTR group was implemented two months before recruitment of Post-DTR subjects and four months after the last Pre-DTR subjects had been inducted in the study. Recently admitted CDTP patients were invited to start-up the DTR group; none of these patients were included in the Post-DTR cohort. This procedure ensured that all Post-DTR subjects would be able to join an “established” DTR group. None of the Pre-DTR subjects participated in DTR meetings within the first six months after their induction into the study.
The DTR group began in April 2004. After the two month DTR implementation period, the DTR group was voluntarily available to all consumers in the CDTP and was the only consumer-led group in the facility. The meetings were chaired by consumer facilitators who were oriented by H. S. Vogel, the Executive Director of Double Trouble in Recovery. DTR meetings follow a traditional 12-step format, described in detail in the manual (42).
2.4. Participant follow-up
All participants completed an extensive locator sheet at the baseline interview, which contained detailed information regarding how they could be located to schedule follow-up interviews (e.g., via telephone, email, regular mail, through friends, family, or other contacts). Efforts were made to contact and schedule all subjects for their 6 month follow-up interviews, whether or not they were still attending the CDTP
2.5. Study measures
At study intake subjects were administered a structured interview that obtained data on demographics, employment/support status, living arrangements, psychiatric diagnoses (43), psychiatric symptoms (44), psychiatric medication adherence (45), recent substance use, psychiatric and addiction treatment history and recent 12-step attendance. Program retention, defined as the number of days that subjects remained enrolled in the CDTP up to 6 months, was obtained from program records.
2.6. Analysis techniques
Intent to treat analysis was conducted to compare outcomes between the Pre-DTR and Post-DTR cohorts. The baseline equivalents of the dependent (outcome) measures were used as covariates in multiple regression. Other baseline measures were included as covariates only if significantly correlated with both cohort membership and an outcome variable. Highly skewed dependent variables – substance use and traditional 12-step attendance - were log-transformed. Clinic retention was analyzed using survival analysis based on Cox regression.
3. Results
3.1. Study condition assignment
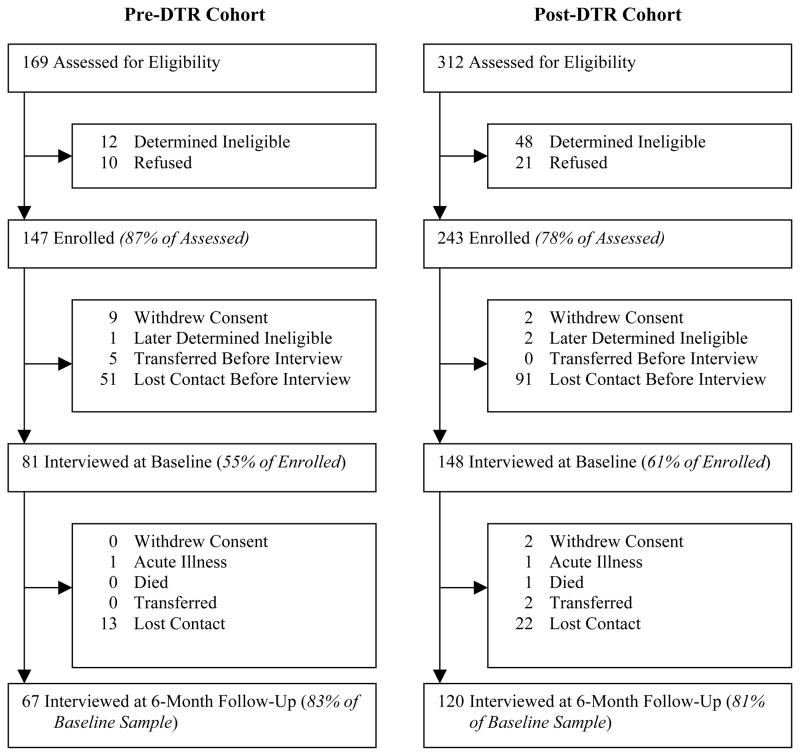
A total of 481 patients enrolling into the CDTP were screened for the study; 169 were screened prior to the implementation of DTR and 312 after DTR implementation (Figure 1). Of these, 229 patients met eligibility criteria, consented to participate, and completed the baseline interview. There were no significant differences between the cohorts in percent who refused or the distribution of reasons for refusal.
Figure 1.
Study flow of participants
3.2. Sample characteristics
Characteristics at study intake are shown in Table 1.
Table 1.
Sample characteristics at study intake
| Pre-DTR; n=81 | Post-DTR; n=148 | Total; N=229 | |
|---|---|---|---|
|
| |||
| Mean (SD) or % | Mean (SD) or % | Mean (SD) or % | |
| Age (years) | 39 (8.4) | 40 (9.4) | 39 (9.1) |
| Male | 57 | 63 | 60 |
| Hispanic | 44 | 40 | 41 |
| Black | 40 | 43 | 42 |
| White | 17 | 18 | 18 |
| Currently employed | 5 | 2 | 03 |
| Public assistance (welfare, disability) | 67 | 71 | 69 |
| Unstable housing (hotel, shelter, on the streets)** | 25 | 11 | 16 |
| Ever received substance abuse treatment | 79 | 76 | 77 |
| Ever received psychiatric treatment | 88 | 91 | 90 |
| Ever attended traditional 12-step group | 65 | 63 | 64 |
| Attended 12-step groups past 6 months | 33 | 32 | 33 |
| Number 12-step groups attended past 6 months | 4.7 (10.3) | 6.4 (16.5) | 5.8 (14.6) |
| Medication non-adherence (MARS)a* | 4.1 (2.3) | 3.5 (2.6) | 3.8 (2.5) |
| Colorado Symptom Index (CSI) | 2.8 (1.1) | 2.6 (1.0) | 2.7 (1.0) |
| Substance use past 90 days | |||
| Alcohol | 49 | 41 | 44 |
| Marijuana | 31 | 31 | 31 |
| Cocaine (powder or crack) | 35 | 33 | 34 |
| Heroin or other opioids | 15 | 13 | 14 |
| Other drugs | 12 | 06 | 08 |
| Any drug or alcohol use | 73 | 62 | 66 |
| Days used drugs or alcoholb | 28 (34.9) | 26 (34.5) | 27 (34.6) |
| Axis I psychiatric diagnosesc | |||
| Major Depressive Disorder | 28 | 23 | 25 |
| Bipolar Disorder | 12 | 13 | 13 |
| Other mood disorders* | 6 | 16 | 13 |
| Schizoaffective Disorder | 17 | 11 | 13 |
| Schizophrenia | 10 | 14 | 13 |
| Psychotic Disorder NOS | 7 | 7 | 7 |
| Anxiety Disorders | 5 | 2 | 3 |
| Substance Use Disorderd | 54 | 47 | 50 |
| PTSDd | 53 | 45 | 48 |
| Other disorders | 13 | 13 | 13 |
PTSD: Post-Traumatic Stress Disorder; NOS: Not otherwise specified.
Higher score means less adherence.
Represents sum of all substances used.
PTSD and Substance Use Disorder were determined by the Mini-International Neuropsychiatric Interview; other Axis I disorders are the primary psychiatric disorders as diagnosed by psychiatrists at the CDTP.
p < .05;
p < .01
Homogeneity of the cohorts was determined by comparing them on study intake characteristics. Pre-DTR subjects compared with Post-DTR subjects were significantly more likely to be unstably housed and to have received an “other mood disorder Axis I disorder by a CDTP psychiatrist. These two factors, however, were unrelated to any of the outcomes. The Pre-DTR cohort was also less adherent to psychiatric medication than the Post-DTR cohort; this factor is controlled in the analysis.
3.3. Follow-up
Eighty-two percent of the (187/229) of the subjects were interviewed for their 6 month follow-up; 83% of the Pre-DTR cohort, 81% of the Post-DTR cohort (n.s.). Among the subjects not followed-up, 35 were lost to contact, 2 transferred, 2 withdrew consent, 1 was too physically ill, and 1 died. Subjects who did not complete the six-month follow-up interview attended fewer traditional 12-step groups prior to baseline (1.1 vs. 6.9, t= − 3.85, p < .001) and were less likely to have a history of drug abuse treatment (57% vs. 80%, Chi-Square= 9.07, p = .003).
3.4. DTR attendance
Post-DTR subjects were encouraged but not mandated to attend the DTR group(s). (Other patients at the CDTP could also attend if they wished.) Of the 148 patients in the post-DTR cohort, 62% attended at least one DTR group and the mean number of groups attended was 3.2 (s.d. = 5.0, range 0–30). Reasons given on the six month interview for not attending were: scheduling conflict (20%), not interested (16%), insufficient awareness of DTR (9%), did not use drugs (7%), acute medical or psychiatric illness (5%); 19 (43%) had left the program before attending DTR or did not give a response. An average of 19 consumers (i.e., study and non-study CDTP patients) attended DTR on a weekly basis, with 30% on average being subjects in the Post-DTR cohort.
3.5. Outcomes
Results are shown in Table 2. At 6-month follow-up, the Post-DTR cohort had used drugs or alcohol on significantly fewer days, had attended traditional 12-step groups more frequently outside of the program, and had higher levels of psychiatric medication adherence, than the Pre-DTR cohort.
Table 2.
Effect of Pre-DTR vs. Post-DTR Cohort on Outcomes
| Baseline
|
6 Month Follow up
|
Regression analysise
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-DTR | Post-DTR | Pre-DTR | Post-DTR | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | β or b | P-value | |
| Days substance use, past 90 days | 25.7 | 33.4 | 25.3 | 34.1 | 26.4 | 35.1 | 18.6 | 31.4 | −0.12 | 0.04 |
| Psychiatric medication non-adherenceb,c | ||||||||||
| OLS Regression | 4.2 | 2.2 | 3.5 | 2.6 | 4.5 | 2.3 | 3.2 | 2.8 | −0.25 | 0.02 |
| FIML Regression | 4.2 | 2.2 | 3.5 | 2.6 | 4.5 | 2.3 | 3.2 | 2.8 | −0.99 | 0.046 |
| Number of 12-step groups attended, past 30 daysd | 2.9 | 7.7 | 2.1 | 5.7 | 1.3 | 3.7 | 3.1 | 6.6 | 0.17 | 0.01 |
| Colorado Symptom Index | 2.8 | 1.0 | 2.6 | 1.0 | 2.4 | 0.9 | 2.3 | 1.0 | 0.02 | 0.71 |
Represents subjects who were interviewed at baseline and follow-up (N=187); 67 Pre-DTR and 120 Post-DTR.
Medication Adherence Rating Scale (MARS); higher score means less adherence.
Fifteen subjects were not administered the MARS because they had not been prescribed psychiatric medication. An additional 25 Pre-DTR and 57 Post-DTR subjects have missing adherence data due to error in the interview skip pattern. A supplementary regression analysis (Full Information Maximum Likelihood; FIML) was conducted to compensate for missing data.
Traditional 12-step groups (AA, NA) attended outside of the index treatment program.
The baseline equivalent of the dependent (outcome) variable was entered as a covariate. The dependent variables for “substance use” and for “number of 12-step groups” were log transformed.
There was no cohort effect on psychiatric symptoms, and program retention at 6 months after enrollment did not differ significantly between the Pre-DTR (73%) and Post-DTR (66%) cohorts.
4. Discussion and Conclusions
This study is one of the few controlled designs evaluating mutual aid, and the only controlled study thus far evaluating dual focus mutual aid. Previous research has shown that mutual aid groups can complement, rather than compete with, professional mental health and addiction treatment (46, 47). The current study reinforces this conclusion and, despite its limitations, helps demonstrate the benefits of introducing 12-step, dual-focus mutual aid into psychiatric treatment programs that serve patients with COD.
The support of peers is a key element facilitating recovery from mental illness (19), and high level of social support has been associated with decreased substance use among persons participating in DTR (48). DTR is structured to create an accepting, non-judgmental environment where persons with active addictions and psychiatric diagnoses can identify with other members and explore their dual recovery needs (42).
Despite the positive outcomes achieved - decreased substance use, increased psychiatric medication adherence and increased 12-step meeting attendance outside the program - the degree of participation in DTR was somewhat disappointing. This was primarily due to logistical issues, however, rather than a lack of interest in DTR by patients. Early drop-out from the CDTP accounted for the largest proportion of non-attendance at DTR. This could have been avoided by limiting eligibility for the study to patients with a minimum length of study, say 3 months. However, it was believed clinically important to try to engage new patients as quickly as possible in DTR, partly for the objective of decreasing program drop-out. Unfortunately, this strategy did not succeed; program dropout appeared to be unaffected by the presence of DTR. Scheduling problems were the second most frequent reason for non-attendance. We hoped, perhaps naively, that Post-DTR cohort subjects with morning CDTP schedules would nonetheless attend the afternoon DTR group as well (transportation was reimbursed by the study), but this usually did not occur. Unfortunately, it was not feasible in the first phase of the study to institute a second, morning DTR group due to program space limitations. Greater and/or more convenient availability of DTR meetings in a program would probably increase attendance.
Although it would be tempting to examine outcomes only for the DTR participants, this would violate the logic of the intent to treat efficacy design, since it is impossible to know which subjects in the Pre-DTR cohort would have attended DTR had it been available to them. The apparent effectiveness of DTR for all participants, both those in the Post-DTR cohort and other CDTP patients, was studied with survey methods and is being reported separately (49).
The limitations of the study are the modest level of DTR attendance, discussed above; the conduct of the study in only one treatment setting; and the quasi-experimental comparative design which is less advantageous than a true experimental design. A true experiment to evaluate DTR has been proposed by the study team as a further step in this continuing line of research.
Acknowledgments
Funded by: Grant #5R01DA015912 from the National Institute on Drug Abuse
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2004 National Survey on Drug Use and Health: National findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2005. [Google Scholar]
- 2.Hagnell O, Grasbeck A. Comorbidity of anxiety and depression in the Lunby 25-year prospective study: The pattern of subsequent episodes. In: Maser JD, Cloninger CR, editors. Comorbidity of Mood and Anxiety Disorders. Washington, DC: American Psychiatric Press; 1990. pp. 139–152. [Google Scholar]
- 3.Hirschfeld RMA, Hasin D, Keller MB, Endicott J, Wunder J. Depression and alcoholism: Comorbidity in a longitudinal study. In: Maser JD, Cloninger CR, editors. Comorbidity of Mood and Anxiety Disorders. Washington, DC: American Psychiatric Press; 1990. pp. 293–304. [Google Scholar]
- 4.Kessler RC. The national comorbidity survey: preliminary results and future directions. International Journal of Methods in Psychiatric Research. 1995;5:139–151. [Google Scholar]
- 5.Murphy JM. Diagnostic comorbidity and symptom co-occurrence: the Stirling County Study. In: Maser JD, Cloninger CR, editors. Comorbidity of Mood and Anxiety Disorders. Washington, DC: American Psychiatric Press; 1990. pp. 153–176. [Google Scholar]
- 6.Gonzalez G, Rosenheck R. Outcome and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services. 2002;53(4):437–446. doi: 10.1176/appi.ps.53.4.437. [DOI] [PubMed] [Google Scholar]
- 7.McLellan AT, Luborsky L, Woody GE, O’Brien CP, Druley K. Predicting response to alcohol and drug abuse treatments: Role of psychiatric severity. Arch Gen Psychiatry. 1983;40:620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- 8.Rounsaville BJ, Kosten TR, Weissman MM, Kleber D. Prognostic significance of psychopathology in treated opiate addicts. Arch Gen Psychiatry. 1986;43:739–745. doi: 10.1001/archpsyc.1986.01800080025004. [DOI] [PubMed] [Google Scholar]
- 9.Alcoholics Anonymous. Twelve Steps and Twelve Traditions. New York, NY: Alcoholics Anonymous World Services, Inc; 1952. [Google Scholar]
- 10.Devine J, Brody C, Wright J. Evaluating and alcohol and drug program for the homeless: an econometric approach. Evaluation and Program Planning. 1997;20:205–215. [Google Scholar]
- 11.Fiorentine R, Hillhouse M. Drug treatment and 12-step program participation: The additive effects of integrated recovery activities. Journal of Substance Abuse Treatment. 2000;18(1):65–74. doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- 12.Humphreys K, Mankowski E, Moos R, Finney J. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Annals of Behavioral Medicine. 1999;21(1):54–60. doi: 10.1007/BF02895034. [DOI] [PubMed] [Google Scholar]
- 13.McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous. New Brunswick, NJ: Rutgers University Press; 1993. [Google Scholar]
- 14.Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: Comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. J Stud Alcohol. 2002;61:529–540. doi: 10.15288/jsa.2000.61.529. [DOI] [PubMed] [Google Scholar]
- 15.Sheffield A. Referral to a peer-led support group: An effective aid for mood disorder patients. Primary Psychiatry. 2003;10(5):89–94. [Google Scholar]
- 16.Carpinello SE, Knight EL, Markowitz FE, Pease EA. The development of the mental health confidence scale: A measure of self-efficacy in individuals diagnosed with mental disorders. Psychiatric Rehabilitation Journal. 2000;23(3):236–243. [Google Scholar]
- 17.Hays JR, Buckle KE. Self-efficacy among hospitalized mentally ill patients. Psychological Reports. 1992;70(1):57–58. doi: 10.2466/pr0.1992.70.1.57. [DOI] [PubMed] [Google Scholar]
- 18.Markowitz FE. Modeling processes in recovering from mental illness: Relationships between symptoms, life satisfaction, and self-concept. Journal of Health and Social Behavior. 2001;42(1):64–79. [PubMed] [Google Scholar]
- 19.Corrigan PW, Slopen N, Gracia G, Phelan S, Heogh CB, Keck L. Some recovery processes in mutual-help groups for persons with mental illness; II: Qualitative analysis of participant interviews. Community Mental Health Journal. 2005;41(6):721–35. doi: 10.1007/s10597-005-6429-0. [DOI] [PubMed] [Google Scholar]
- 20.Hansson L. Determinants of quality of life in people with severe mental illness. Acta Psychiatrica Scandinavica. 2006;113(s429):46–50. doi: 10.1111/j.1600-0447.2005.00717.x. [DOI] [PubMed] [Google Scholar]
- 21.Noordsy D, Schwab B, Fox L, Drake R. The role of self-help programs in the rehabilitation process of persons with severe mental illness and substance use disorders. Community Mental Health Journal. 1996;32(1):71–81. doi: 10.1007/BF02249369. [DOI] [PubMed] [Google Scholar]
- 22.Zaslav P. The role of self-help groups in the treatment of the dual diagnosis patient. In: Solomon J, Zimber S, Sholler E, editors. Dual Diagnosis. New York, NY: Plenum Publishing Corporation; 1993. pp. 105–126. [Google Scholar]
- 23.Minkoff K. An integrated treatment model for dual diagnosis of psychosis and addiction. Hosp Community Psychiatry. 1989;40(10):1031–6. doi: 10.1176/ps.40.10.1031. [DOI] [PubMed] [Google Scholar]
- 24.Minkoff K, Drake R. Dual diagnosis of major mental illness and substance disorder. In: Lamb HR, editor. New Directions in Mental Health Services. San Francisco, CA: Jossey Bass; 1991. [DOI] [PubMed] [Google Scholar]
- 25.Humphreys K. Clinicians’ referral and matching of substance abuse patients to self-help groups after treatment. Psychiatric Services. 1997;48(11):1445–1449. doi: 10.1176/ps.48.11.1445. [DOI] [PubMed] [Google Scholar]
- 26.Villano CL, Rosenblum A, Magura S, Laudet A, Fong C, Betzler T, Vogel H, Knight E. Mental health clinicians’ 12-step referral practices with dually diagnosed patients. International Journal of Self Help & Self Care. 2005;3(1–2):63–71. [Google Scholar]
- 27.Laudet A. Treatment providers’ referral to self-help: review and future empirical directions. International Journal of Self-Help and Self-care. 2000;1(3):195–207. doi: 10.2190/bqkv-x2hr-mvfd-1vpl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vogel HS, Knight EL, Laudet AB, Magura S. Double Trouble in Recovery: Self-help for the dually-diagnosed. Psychiatric Rehabilitation Journal. 1998;21:356–364. doi: 10.1037/h0095288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hazelden . The Dual Diagnosis Recovery Book. Center City, MN: Hazelden Foundation; 1993. [Google Scholar]
- 30.Alcoholics Anonymous. The AA Member - Medications and Other Drugs. New York, NY: Alcoholics Anonymous World Services, Inc; 1984. [Google Scholar]
- 31.Narcotics Anonymous. Times of Illness. New York, NY: Narcotics Anonymous World Services, Inc; 1992. [Google Scholar]
- 32.Meissen G, Powell TJ, Wituk SA, Girrens K, Arteaga S. Attitudes of AA contact persons toward group participation by persons with a mental illness. Psychiatr Serv. 1999;50(8):1079–81. doi: 10.1176/ps.50.8.1079. [DOI] [PubMed] [Google Scholar]
- 33.Jordan LC, Davidson WS, Herman SE, Bottsmiller BJ. Involvement in 12 step programs among persons with dual diagnosis. Psychiatric Services. 2002;53(7):894–896. doi: 10.1176/appi.ps.53.7.894. [DOI] [PubMed] [Google Scholar]
- 34.Ritsher JB, McKellar JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. Journal of Studies on Alcohol. 2002;63:709–715. doi: 10.15288/jsa.2002.63.709. [DOI] [PubMed] [Google Scholar]
- 35.Moggi F, Ouimette PC, Moos RH, Finney JW. Dual diagnosis patients in substance abuse treatment: relationship of general coping and substance-specific coping to 1-year outcomes. Addiction. 1999;94(12):1805–16. doi: 10.1046/j.1360-0443.1999.941218056.x. [DOI] [PubMed] [Google Scholar]
- 36.Kelly JF, McKellar JD, Moos R. Major depression in patients with substance use disorders: relationship to 12 step self-help involvement and substance use outcomes. Addiction. 2003;98(4):499–508. doi: 10.1046/j.1360-0443.2003.t01-1-00294.x. [DOI] [PubMed] [Google Scholar]
- 37.Bogenschutz MP. Specialized 12-Step programs and 12-Step facilitation for the dually-diagnosed. Community Mental Health Journal. 2005;41(1):7–19. doi: 10.1007/s10597-005-2596-2. [DOI] [PubMed] [Google Scholar]
- 38.Laudet A, Magura S, Cleland C, Vogel H, Knight E, Rosenblum A. The effect of 12-Step-based fellowship participation on abstinence among dually-diagnosed persons: A two-year longitudinal study. Journal of Psychoactive Drugs. 2004;36 (2):207–16. doi: 10.1080/02791072.2004.10399731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magura S, Laudet A, Mahmood D, Rosenblum A, Knight E. Medication adherence and participation in self-help groups designed for dually-diagnosed persons. Psychiatric Services. 2002;53(3):310–316. doi: 10.1176/appi.ps.53.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Magura S, Cleland C, Vogel HS, Knight EL, Laudet AB. Effects of “dual focus” mutual aid on self-efficacy for recovery and quality of life. Administration and Policy in Mental Health and Mental Health Services Research. 2007;34(1):1–12. doi: 10.1007/s10488-006-0091-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Magura S, Laudet A, Mahmood D, Rosenblum A, Vogel H, Knight E. Role of self-help processes in achieving abstinence among dually-diagnosed persons. Addictive Behaviors. 2003;28(3):399–413. doi: 10.1016/s0306-4603(01)00278-7. [DOI] [PubMed] [Google Scholar]
- 42.Vogel H. Double Trouble in Recovery Manual. 1993 www.doubletroubleinrecovery.org.
- 43.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The M.I.N.I.-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59 (Suppl 20):22–33. [PubMed] [Google Scholar]
- 44.Conrad KJ, Yagelka JR, Matters MD, Rich AR, Williams V, Buchanan M. Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Ment Health Serv Res. 2001;3(3):141–53. doi: 10.1023/a:1011571531303. [DOI] [PubMed] [Google Scholar]
- 45.Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–7. doi: 10.1016/s0920-9964(99)00130-9. [DOI] [PubMed] [Google Scholar]
- 46.Hodges JQ, Markward M, Keele C, Evans CJ. Use of self-help services and consumer satisfaction with professional mental health services. Psychiatric Services. 2003;54(8):1161–1163. doi: 10.1176/appi.ps.54.8.1161. [DOI] [PubMed] [Google Scholar]
- 47.Magura S. The relationship between substance user treatment and 12-step fellowships: current knowledge and research questions. Substance Use & Misuse. 2007;42(2–3):343–360. doi: 10.1080/10826080601142071. [DOI] [PubMed] [Google Scholar]
- 48.Laudet AB, Cleland CM, Magura S, Vogel HS, Knight EL. Social support mediates the effects of dual-focus mutual aid groups on abstinence from substance use. Am J Community Psychol. 2004;34(3–4):175–85. doi: 10.1007/s10464-004-7413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Magura S, Villano CL, Rosenblum A, Vogel HS, Betzler T. Consumer evaluation of dual focus mutual aid. Journal of Dual Diagnosis. doi: 10.1080/15504260802067032. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]