Abstract
Among ethnic populations in Hawai‘i, Native Hawaiians continue to be over-represented with the highest rates in: morbidity and mortality, chronic health conditions, and the health risks of being overweight and obese. Focused on these two health risks, the investigation reported in this article has a specific aim of empirically determining whether social stigma as manifested in the form of perceived overt or covert discrimination is a contributing factor. Current studies focused on select ethnic populations, particularly African Americans point to discrimination as an important but understudied predictor of adverse health outcomes. Acknowledging the paucity of research on discrimination and its role in the health of Native Hawaiians, this investigation utilizes data from the 2007 Hawaiian Health Survey which was coordinated by the Department of Health, and the Office of Health Status Monitoring and implemented by SMS Hawai‘i. The weighted sample of Hawai‘i adults included measures of race/ethnicity and of everyday discrimination and the BMI (Body Mass Index). Logistic regression analyses were applied to determine if: (a) discrimination was significantly related to being overweight and/or obesity; and (b) whether this relationship remained a salient predictor after key demographic factors of gender, age, education, income, and length of time in the Islands were taken into account. This study confirmed the negative influence of overt discrimination as well as the protective nature of covert discrimination in explaining the variability in obesity/overweight in Native Hawaiians. The implications of this study for strategic interventions and research are discussed.
Keywords: Native Hawaiian, Overt/Covert Discrimination, Health Risk, Obesity/overweight, HHS
Introduction
Native Hawaiians have one of the poorest health statuses compared to all ethnic groups in the State of Hawai‘i.1 A leading factor affecting these health disparities is the prevalence of being overweight or obese. In 2009, the Hawai‘i Department of Health2 pointed to the alarming statistic that Native Hawaiians had a prevalence rate of 69.6% for being overweight or obese. In complementing the national interest and scientific effort to identify contributors to these specific health risks, this investigation has specifically aimed to empirically determine if social stigma as manifested in the form of perceived overt or covert discrimination is a unique contributing factor to health risks for indigenous Hawaiians. This investigation attempts to address contributing factors to the health risk of Native Hawaiians, an indigenous and ethnic population with life experiences of colonization accompanied by loss of culture, identity, and sense of place. The goal is to determine if discrimination may explain the variability in these health risks. Additionally this study applies a discrimination measure to the Native Hawaiian population and provides the respective psychometric properties associated with this indigenous group.
Health Risks, Discrimination, and Native Hawaiians
For the past few decades, Native Hawaiians struggled with multiple health disparities. Studies continue to associate Native Hawaiians with higher death rates compared to the nation and deaths at younger ages compared to other ethnic groups in the nation and the state of Hawai‘i.3–5 A leading cause for higher death rates includes increased rates of obesity and obesity-related diseases.3–9 Common obesity-related diseases include hypertension, diabetes, asthma, and cardiovascular disease.5,8,9 Health disparities10 and shortened life expectancy have also been linked to social and demographic characteristics including age, socio-economic status, gender, geographical location/residence, and the self-identified race/ethnicity. Individuals born with social disadvantages (eg, lower social ranking status based on gender, race, and socioeconomic status) tend to develop more health problems than those born with more cumulative social advantages such as higher education, higher income, and being a member of the majority racial group.
Perceived racial or ethnic discrimination continues to receive attention as an understudied contributor to physical and mental health outcomes and health disparities among people of color.11 The majority of prior investigations on perceived discrimination focused almost exclusively on major acute acts of subordination such as racial profiling. Over time, blatant acts against ethnic minorities have been suppressed or even eliminated, but acts of “everyday discrimination” persist, accompanied by adverse outcomes.12 Everyday discrimination refers to minor, chronic, and daily experiences of interpersonal unfair treatment.12 Several researchers found everyday discrimination to be a stronger predictor of physical and mental health status than assessments of major experiences of discrimination.13–15 There is a growing body of research indicating that everyday discrimination adversely affects physical health.16–20 For instance, in a 6-year follow-up study of African American women, women under the age of 50 who reported frequent experiences of everyday discrimination were at a significantly higher risk of developing breast cancer than those who reported infrequent experiences.19 Additionally, everyday discrimination has been associated with higher levels of C-reactive protein, a marker of inflammation and well-known correlate of cardiovascular health among older African American adults even after controlling for other risk factors such as depression, smoking, heart disease, hypertension, and diabetes.18 The linkage of everyday discrimination (EDS) to psychological stress, perceived racism, and internalized racism as factors affecting body mass index (BMI) levels including being underweight, normal weight, overweight or obese have also been confirmed.22,23
Studies often examine ways discrimination may directly affect obesity-related diseases, rather than a pathway through BMI levels.17,25 Prior studies22 underscore the importance of various types of stressors which can activate physiological consequences that play a role in health problems specific to general obesity, abdominal obesity, and obesity outcomes including high-blood pressure, depression, anxiety, sleep problems, and coronary calcification. A factor that may influence large amounts of stress includes social disadvantages, which may be experienced through different stressors including racial discrimination and socio-demographic factors. The relationship between stress and health outcomes specific to abdominal obesity was demonstrated in an Afro-Caribbean population residing in Barbados.22 After accounting for demographical characteristics, the researchers found a significant correlation between internalized racism and both abdominal obesity and blood pressure. Moreover, the researchers found higher BMI levels for individuals with higher levels of internalized racism. After adjusting for age and education, the association of being overweight for those who internalized racism was two times greater and the odds of having abdominal obesity was 2.8 times greater. In another study,21 a positive relationship existed between discrimination and BMI levels within an Asian American population. Within this population, BMI levels were highest for those who reported weight discrimination, followed by racial discrimination, and finally, other types of discrimination within the everyday acts of discrimination scale. After adjusting for covariates such as socio-demographic characteristics, mental and physical illness, and social desirability bias, a significant positive relationship was found between racial discrimination and BMI.
In general, there remains a significant gap in the research, particularly studies examining indigenous populations and the impact of discrimination on health risk factors such as obesity or being overweight. Within indigenous research, a paucity of research exists on discrimination and health risk factors among Native Hawaiians.25 This study also addressed a key methodological issue: the conspicuous paucity of the application of psychometric measures (eg, exploratory factor analyses, confirmatory factor analyses, tests of invariance, and reliability) developed for one population (African American) to other populations (Hawaiians).26–28
Methods
The researchers used a weighted dataset from the Hawai‘i Health Survey (HHS) administered in 2007, which consisted of participants residing in the State of Hawai‘i. This analysis focuses on respondents who self-identified their ethnicity as Native Hawaiian. The HHS is a landline telephone survey conducted by the Hawai‘i Department of Health (DOH), Office of Health Status Monitoring (OHSM). The survey excludes persons living in group quarters, residents of the island of Ni‘ihau, a privately owned island in Hawai‘i, and homeless persons. The HHS measures demographic characteristics and the health status of Hawai‘i's residents to provide data to monitor health status of the ethnically diverse population, with the intention of planning health services in Hawai‘i, strategic design, and implementation of programs to ameliorate conditions that foster health risks and adverse health outcomes. The sample design is disproportionate by geography and survey data are statistically adjusted to match the geographic location and number of telephone lines, size of households and the age and gender of all household members.
The Native Hawaiian sub-sample is profiled (Table 1) as consisting of nearly an even distribution of men (46.6%) and women (53.4%) respondents with two-thirds represented by two age groups 34–54 years (40.7%) and over 55 years (25.5%). The majority (78.1%) of Hawaiians had annual household income represented by two groups ($35,000–$74,999; 38.0%) and those with incomes in excess of $75,000 (40.1%). The Hawaiians were nearly evenly divided between those with high school diploma (or GED) or less (52.0%) and those with college education or college degrees (48%). The majority (90.5%) of Hawaiian respondents have either lived in the state of Hawai‘i in excess of 20 years (9.9%) or their entire lives (81.6%).
Table 1.
Frequencies of the Demographic Variables for Native Hawaiians (Unweighted and Weighted Data)
| Unweighted Data | Weighted Data | |||
| Demographic Variable | N | Percent | N | Percent |
| Gender: Men | 118 | 32.2 | 69779 | 46.6 |
| Gender: Women | 249 | 67.8 | 80049 | 53.4 |
| Age (Level 1: 18–34) | 74 | 20.2 | 50621 | 33.8 |
| Age (Level 1: 35–54) | 152 | 41.1 | 60938 | 40.7 |
| Age (Level 3: 55+) | 141 | 38.4 | 38268 | 25.5 |
| Income (Level 0: less than $35,000) | 97 | 26.4 | 32798 | 21.9 |
| Income (Level 1: $35,000–74,999) | 134 | 36.5 | 56919 | 38.0 |
| Income (Level 2: $75,000 or more) | 136 | 37.1 | 60110 | 40.1 |
| Education (Level 0: HS/ED or less) | 180 | 49 | 77854 | 52.0 |
| Education (Level 1: Some College) | 111 | 30.2 | 40957 | 27.3 |
| Education (Level 2: College Graduate or more) | 76 | 20.7 | 31017 | 20.7 |
| Years Living in Hawai‘i (Level 0: 5 years or less) | 5 | 1.4 | 5113 | 3.4 |
| Years Living in Hawai‘i (Level 1: 5 to 20 years) | 14 | 3.8 | 7606 | 5.1 |
| Years Living in Hawai‘i (Level 2: 20+ years) | 44 | 12 | 14818 | 9.9 |
| Years Living in Hawai‘i (Level 3: Lifetime) | 304 | 82.8 | 122291 | 81.6 |
Measures: Discrimination and Criterion of Obese/Overweight
Exploratory Factor Analysis (EFA), Confirmatory Factor Analysis (CFA) and Test of Invariance (validity confirmations) were adopted as core requirements for the use of EDS in this investigation. AMOS 19.0,26 the IBM statistical program used in these analyses, requires the uses of unweighted data in the systematic analysis of the EDS (see Figure 1).
Figure 1.
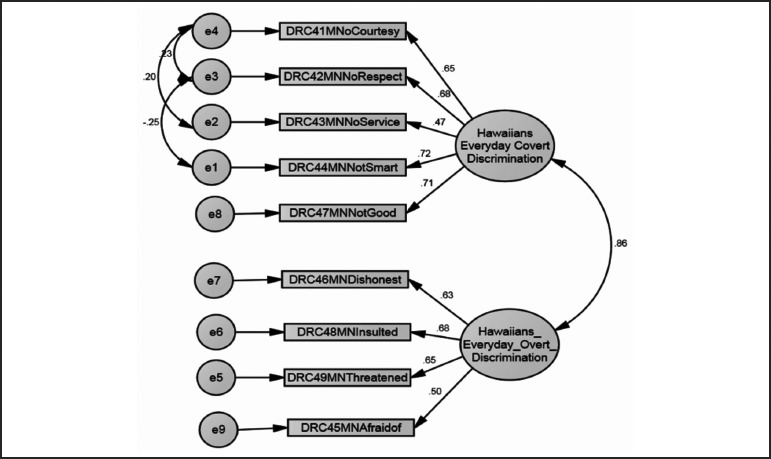
Confirmatory Factor Analysis of two factor model (overt and covert Discrimination) of Everyday Discrimination, Testing for Model Fit for Native Hawaiians (McCubbin, L. & McCubbin, 2012).*
The Everyday Discrimination Scale (EDS),25 adopted for this investigation, included 9 questions about the respondent's perceptions of and encounters with discrimination. The participants responded to a Likert-scale, ranging from never (1) to very often (5). Therefore, higher scores on the discrimination scale indicated a greater amount of everyday discrimination. The EFA revealed two latent variables (subscales) identified as overt and covert discrimination. The American Psychological Association29 refers to two dimensions of discrimination as blatant prejudice (racism) and hidden prejudice (micro-aggressions)29,30 respectively. The CFA29 confirmed the “fit of the two latent variable model” supported by CMIN//DF OF 3.698 (P <.05, GFi= .978, AGFi= .966, IFi= .974, CFi= .974, RMSEA = .034 with a confidence interval of .029 and .039 and PCLOSE = 1.000). The Overt Discrimination subscale consists of four items: “perceptions of being dishonest, one to be afraid of, called names or insulted, and harassed or threatened.” The Covert Discrimination subscale includes “receiving poorer service than other people at restaurants or stores, being treated with less respect than other people, being treated with less courtesy than other people, people act as if they think you are not as good as they are, and people act as if they think you are not smart.” Both subscales demonstrated acceptable levels of reliability (Cronbach's Alphas of .79) and validated with an independent report of perceived racial discrimination.
Criterion Measure of Health Risk: Overweight or Obese
The BMI data were applied to the classification of Native Hawaiians into two categories:31 (a) individuals who were considered underweight or normal (less than 18.5 kg/m2 to 24.9 kg/m2) (coded 0); or (b) overweight or obese (25.0 to more than 30 kg/m2) (coded 1).
Results
The analysis focused on the results derived from the use of weighted data, a strategy intended to reflect a more accurate representation of Native Hawaiians in the State of Hawai‘i and across the different islands. To address the two major questions for this investigation a two-model logistic regression analysis was conducted. The first model included the independent variables of gender, age, income, education level, and years in Hawai‘i. The second model consisted of adding the two types of discrimination, overt and covert acts of everyday discrimination to Model 1 to determine their unique contribution to explaining obesity/overweight. The results of this logistic regression are presented in Table 2.
Table 2.
Hierarchical Logistic Regression Examining Demographic Factors and Everyday Discrimination on Being Overweight and/or Obese Among Native Hawaiians (Weighted Data)
| Variables in the equation | B | Wald | P | Odds Ratio | CI | |
| Lower | Upper | |||||
| Model 1 | ||||||
| Gender: Women (Reference) | ||||||
| Gender: Men | 1.00 | 5759.88 | .00 | 2.73 | 2.66 | 2.80 |
| Age (Level 0: 18–34) | −.88 | 3108.10 | .00 | .41 | .40 | .43 |
| Age (Level 1: 35–54) | .25 | 262.25 | .00 | 1.29 | 1.25 | 1.33 |
| Age (Level 3: 55+) (Reference) | ||||||
| Income (Level 0: less than $35,000) | .90 | 2498.41 | .00 | 2.45 | 2.37 | 2.54 |
| Income (Level 1: $35,000–74,999) | −.12 | 82.03 | .00 | .89 | .86 | .91 |
| Income (Level 2: $75,000 or more) (Reference) | ||||||
| Education (Level 0: HS/ED or less) | −.18 | 117.82 | .00 | .84 | .81 | .86 |
| Education (Level 1: Some College) | −.26 | 209.82 | .00 | .77 | .75 | .80 |
| Education (Level 2: College Graduate or more) (Reference) | ||||||
| Years Living in Hawai‘i (Level 0: 5 years or less) (Reference) | ||||||
| Years Living in Hawai‘i (Level 1: 5 to 20 years) | .13 | 10.03 | .00 | 1.14 | 1.05 | 1.23 |
| Years Living in Hawai‘i (Level 2: 20+ years) | 1.70 | 1880.43 | .00 | 5.48 | 5.07 | 5.91 |
| Years Living in Hawai‘i (Level 3: Lifetime) | 1.55 | 2219.05 | .00 | 4.73 | 4.43 | 5.04 |
| Model 2 | ||||||
| Gender: Women (Reference) | ||||||
| Gender: Men | .77 | 3118.14 | .00 | 2.16 | 2.10 | 2.22 |
| Age (Level 0: 18–34) | −.92 | 3129.09 | .00 | .40 | .39 | .41 |
| Age (Level 1: 35–54) | .14 | 78.71 | .00 | 1.15 | 1.12 | 1.19 |
| Age (Level 3: 55+) (Reference) | ||||||
| Income (Level 0: less than $35,000) | .98 | 2839.09 | .00 | 2.68 | 2.58 | 2.77 |
| Income (Level 1: $35,000–74,999) | −.05 | 15.19 | .00 | .95 | .92 | .97 |
| Income (Level 2: $75,000 or more) (Reference) | ||||||
| Education (Level 0: HS/ED or less) | −.07 | 16.13 | .00 | .93 | .90 | .97 |
| Education (Level 1: Some College) | −.21 | 130.85 | .00 | .81 | .78 | .84 |
| Education (Level 2: College Graduate or more) (Reference) | ||||||
| Years Living in Hawai‘i (Level 0: 5 years or less) (Reference) | ||||||
| Years Living in Hawai‘i (Level 1: 5 to 20 years) | .34 | 70.05 | .00 | 1.40 | 1.29 | 1.52 |
| Years Living in Hawai‘i (Level 2: 20+ years) | 1.99 | 2501.92 | .00 | 7.28 | 6.74 | 7.87 |
| Years Living in Hawai‘i (Level 3: Lifetime) | 1.82 | 2988.54 | .00 | 6.19 | 5.80 | 6.61 |
| Overt Discrimination (low) (Reference) | ||||||
| Overt Discrimination (moderate/high) | 1.13 | 5640.63 | .00 | 3.08 | 2.99 | 3.17 |
| Covert Discrimination (low) (Reference) | ||||||
| Covert Discrimination (moderate/high) | −.42 | 582.12 | .00 | .66 | .63 | .68 |
In the logistic regression analysis of Model 1, inclusive of the demographic variables (age, education, income, and length of time in Hawai‘i), revealed significant odds ratios for all, thus confirming their importance in explaining the variability in the Hawaiians' health risks of obesity/overweight. The analysis confirmed good model fit (Omnibus test of Model Coefficients (χ2 = 20921.157, P = .0005) with the demographic predictors combined pseudo R2 indices to explaining between 13.0% (Cox & Snell pseudo R2) and 18.3% (Nagelkerke pseudo R2) of the variability in the criterion of obesity/overweight. The classification analysis reveals that Model 1 is able to predict the correct category (obesity/overweight) for the respondents in 74.8% of the cases.
Of importance, however, within this set of predictors, the statistically significant demographic predictors varied in the nature of their association with their relationship to the criterion of being obese/overweight. Specifically, being male (OR=2.73), between the ages of 35 and 54 (OR = 1.29), having a household income of $35,000 or less (OR = 2.45), and living in the Hawaiian Islands 6–20 years (OR = 1.29) were positively related to being obese/overweight. In contrast, being female, in the age group of 18–34 (OR = .41), with a household income of $35,000–$74,999 (OR = .89), and having an education level of high school diploma or less (OR = .84) or some college education (OR = .77) was negatively related to obesity/overweight. The odds of a Hawaiian reporting being obese/overweight decreases by being a female, between the ages of 18–34, with a household income between $35,000 and $74,999 and having an education level of high school or less or some college experience.
Model 2 inclusive of overt and covert discrimination, while controlling for gender, age, education, household income and length of time living in Hawai‘i, reveal the salience of both overt and covert discrimination in explaining the variability in Hawaiians reporting being obese/overweight. The logistic regression analysis of Model 2, revealed significant odds ratios for both overt and covert discrimination thus confirming their importance in explaining the variability in the Hawaiians' health risks of obesity/overweight. The analysis confirmed good model fit (Omnibus test of Model Coefficients (χ2 = 26743.275, P = .0005) with the demographic predictors combined pseudo R2 indices to explaining between 16.3% (Cox & Snell pseudo R2) and 22.9% (Nagelkerke pseudo R2) of the variability in the criterion of obesity/overweight. The classification analysis reveals that Model 2 is able to predict the correct category (obesity/overweight) for the respondents in 75.7% of the cases. As was true for demographic predictors however, the nature of the influence of overt and covert discrimination varies. Overt discrimination (OR = 3.08) is positively related to obesity/overweight and thus a factor in promoting or reinforcing obesity/overweight, all other factors being equal. In contrast, covert discrimination (OR = −.66) is negatively associated with obesity/overweight and thus a predictor of not reporting being obese/overweight. The results of the logistic regression with unweighted data is included in Table 3 for comparative purposes. The logistic regression reveals significant odds being limited to two predictors. Specifically, household income of $35,000 or less (OR = 1.88) and overt discrimination (OR = 2.19) are the only statistically significant predictors.
Table 3.
Hierarchical Logistic Regression Examining Demographic Factors and Everyday Discrimination on Being Overweight and/or Obese Among Native Hawaiians (Unweighted Data)
| Variables in the equation | B | Wald | P | Odds Ratio | CI | |
| Lower | Upper | |||||
| Model 1 | ||||||
| Gender: Women (Reference) | ||||||
| Gender: Men | .45 | 3.03 | .08 | 1.58 | .94 | 2.63 |
| Age (Level 0: 18–34) | −.44 | 2.02 | .16 | .64 | .35 | 1.18 |
| Age (Level 1: 35–54) | .36 | 1.74 | .19 | 1.43 | .84 | 2.43 |
| Age (Level 3: 55+) (Reference) | ||||||
| Income (Level 0: less than $35,000) | .60 | 3.51 | .06 | 1.82 | .97 | 3.41 |
| Income (Level 1: $35,000–74,999) | −.07 | .06 | .81 | .94 | .56 | 1.58 |
| Income (Level 2: $75,000 or more) (Reference) | ||||||
| Education (Level 0: HS/ED or less) | .04 | .02 | .90 | 1.04 | .56 | 1.95 |
| Education (Level 1: Some College) | −.27 | .69 | .41 | .76 | .4 | 1.45 |
| Education (Level 2: College Graduate or more) (Reference) | ||||||
| Years Living in Hawaii (Level 0: 5 years or less) (Reference) | ||||||
| Years Living in Hawaii (Level 1: 5 to 20 years) | −.16 | .02 | .88 | .85 | .10 | 7.10 |
| Years Living in Hawaii (Level 2: 20+ years) | .46 | .22 | .64 | 1.59 | .23 | 11.05 |
| Years Living in Hawaii (Level 3: Lifetime) | .60 | .41 | .52 | 1.83 | .29 | 11.41 |
| Model 2 | ||||||
| Gender: Women (Reference) | ||||||
| Gender: Men | .38 | 2.00 | .16 | 1.46 | .87 | 2.45 |
| Age (Level 0: 18–34) | −.41 | 1.68 | .20 | .66 | .36 | 1.24 |
| Age (Level 1: 35−54) | .30 | 1.17 | .28 | 1.35 | .78 | 2.32 |
| Age (Level 3: 55+) (Reference) | ||||||
| Income (Level 0: less than $35,000) | .63 | 3.79 | .05 | 1.88 | 1.00 | 3.55 |
| Income (Level 1: $35,000–74,999) | −.02 | .01 | .94 | .98 | .58 | 1.67 |
| Income (Level 2: $75,000 or more) (Reference) | ||||||
| Education (Level 0: HS/ED or less) | .13 | .16 | .69 | 1.14 | .60 | 2.16 |
| Education (Level 1: Some College) | −.26 | .62 | .43 | .77 | .40 | 1.49 |
| Education (Level 2: College Graduate or more) (Reference) | ||||||
| Years Living in Hawaii (Level 0: 5 years or less) (Reference) | ||||||
| Years Living in Hawaii (Level 1: 5 to 20 years) | .00 | .00 | 1.00 | 1.00 | .12 | 8.57 |
| Years Living in Hawaii (Level 2: 20+ years) | .68 | .47 | .50 | 1.98 | .28 | 13.95 |
| Years Living in Hawaii (Level 3: Lifetime) | .83 | .77 | .38 | 2.29 | .36 | 14.52 |
| Overt Discrimination (low) (Reference) | ||||||
| Overt Discrimination (moderate/high) | .78 | 8.27 | .00 | 2.19 | 1.28 | 3.72 |
| Covert Discrimination (low) (Reference) | ||||||
| Covert Discrimination (moderate/high) | −.49 | 2.34 | .13 | .62 | .33 | 1.15 |
Discussion
This investigation was framed as a study of stressors (discrimination) and their negative influence on health risks (obesity/overweight). The findings while supportive of this basic paradigm, suggests the value of reframing the investigation as a risk and protective factors paradigm, commonly associated with psychological theories of resilience represented by the classic works of Garmezy,32 Rutter,33 Werner & Smith,34 and the sociological perspective of salutogenesis developed by Antonovsky.35 Essentially, the findings suggest that explaining the variability in health risks of obesity/overweight of Native Hawaiians may be more fully understood and addressed as the combination and interacting influence of both risk and protective factors rather than a single negative causal influence of discrimination complemented by “controlling” other variables. On one hand the predictors of obesity/overweight represented by statistically significant and positive odds ratios, present an “at-risk” profile of Hawaiian men in the middle years between 35 and 54, with annual household income $34,000 or less, having lived in the Hawaiian Islands six years or more including a lifetime and confronted by moderate to high levels of overt discrimination. One could consider this cluster of predictors as that of a Hawaiian at-risk profile. The investigation also identified predictors of obesity/overweight, represented by statistically significant and negative odds ratios. They present a profile of Hawaiians with protective factors inclusive of being a woman, between the ages of 18 and 34, with an annual household income between $35,000 and $74,999, having a high school diploma or less education and some college, and confronted by moderate to high levels of covert discrimination.
The latter finding of covert discrimination — that for every incremental increase in covert discrimination the lower the probability of reporting being obese/overweight — deserves further discussion. This finding contradicts the commonly held notion that everyday discrimination has a negative impact on the health and well-being of persons of color living in a milieu in which racially based stigma may be a persistent part of life.12 One simple methodological explanation may well be that the Everyday Discrimination Scale when applied as a whole without considering its underlying overt and covert dimensions, is dominated by the overt discrimination elements of the scale. It is also reasonable to argue that covert discrimination represented by items inclusive of “being treated with less courtesy, receiving poorer service than others, acting as if people think you are not smart” while pejorative in nature may be perceived as falling short of invasive and undermining the individual's self-worth, integrity and identity. It may also be viewed as a motivator to overcome adversity and stigma. Why it would be a protective factor may well be explained by the Hawaiians “search for meaning” to use Frankl's36 concept of the ability to reframe negative life experiences into a constructive purpose to foster survival. In general these explanations remain unconfirmed and present challenges for future research.
While the HHS is one of the most valuable health surveys for Native Hawaiians in the State of Hawai‘i, limitations are noted. First, the survey involved interview data collected via random selection of respondents using landlines and excluded individuals living in group quarters, residents of Ni‘ihau, homeless persons, and Native Hawaiians (nearly half of the total Hawaiian population) who reside elsewhere and particularly on the continental United States. Even with application of weights intending to improve upon the representativeness of the population living in Hawai‘i, in light of these limitations, generalizability of these findings to the total Native Hawaiian population would not be appropriate. A nationally representative sample of Native Hawaiians inclusive of those living on the continental US would be an appropriate follow-up study.
The study of discrimination and BMI as well as other heath indices merits an examination of within group comparisons focused on the multi-ethnic nature of Native Hawaiians. National statistics37 point to the State of Hawai‘i as having one of the highest concentrations of multi-ethnic individuals and marriages indicating the importance of an additional source of stigmatization and a host of additional contributing factors to health outcomes inclusive of obesity/overweight. The variables of genetics, diet, historical trauma, cost of living, housing costs, to name a few, come into play in explaining the variability in these health risks for Indigenous Hawaiians, but were not included as part of this investigation.
These limitations should not distract from the findings of overt discrimination as an explanatory risk factor in being obese/overweight as an index of health risk. This finding gains importance in light of the population growth of Native Hawaiians, and the growing sentiment that the Hawaiians are adversely impacted by historical losses of identity, language, culture and land, and sense of place, all of which are important determinants as risk factors related to the health and well-being of this population. The pathways of discrimination to obesity deserve greater consideration in future research. While important to isolate and confirm the deleterious effect of discrimination, the psychological and social protective factors do come into play in reducing the adverse effects of the full range of social insults associated with discrimination.
Acknowledgments
This project was funded by the Berry Family Fellowship, Washington State University (Laurie McCubbin, PI) and by a grant from the University of Hawai‘i, Office of the Vice Chancellor for Research and the Office of Hawaiian Affairs (Hamilton McCubbin, PI). The authors acknowledge the contributions of Dr. Jason Sievers (Washington State University) and Dr. Hamilton McCubbin, University of Hawai‘i.
Footnotes
The numbers represent loadings (relationship between subscales and specific items for each subscale) and covariance coefficients (relationship between discrimination subscales and relationships among error terms.)
Conflict of Interest
The authors identify no conflict of interest.
References
- 1.Lassetter J. The integral role of food in Native Hawaiian migrants' perceptions of health and well-being. J Transcultural Nurs. 2011;22:63–70. doi: 10.1177/1043659610387153. [DOI] [PubMed] [Google Scholar]
- 2.Hawaii Department of Health, author. [May 15, 2011];2009 Survey Report Data (Tables and Figures) http://hawaii.gov/health/statistics/hhs/index.html. [Google Scholar]
- 3.Aluli N. Prevalence of obesity in a Native Hawaiian population. Am J Clin Nutr. 1991;53:1556S–1560S. doi: 10.1093/ajcn/53.6.1556S. [DOI] [PubMed] [Google Scholar]
- 4.Aluli N, Reyes P, Tsark J. Cardiovascular disease disparities in native Hawaiians. J Cardiometabolic Syndrome. 2007;2:250–253. doi: 10.1111/j.1559-4564.2007.07560.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson D, Oyama N, LeMarchand L, et al. Native Hawaiians mortality, morbidity, and lifestyle: comparing data from 1982, 1990, and 2000. Pac Health Dialog. 2004;11:120–130. [PubMed] [Google Scholar]
- 6.Kumanyika S. Special issues regarding obesity in minority populations. Ann Intern Med. 1993;119:650–654. doi: 10.7326/0003-4819-119-7_part_2-199310011-00005. [DOI] [PubMed] [Google Scholar]
- 7.Grandinetti A, Chang H, Chen R, et al. Prevalence of overweight and central adiposity is associated with percentage of indigenous ancestry among native Hawaiians. Int J Obesity. 1999;23:733–737. doi: 10.1038/sj.ijo.0800921. [DOI] [PubMed] [Google Scholar]
- 8.Mau M, Sinclair K, Saito E, et al. Cardiometabolic health disparities in native Hawaiians and other Pacific Islanders. Epidemiol Rev. 2009;31:113–129. doi: 10.1093/ajerev/mxp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCubbin H, Strom I, McCubbin L, et al. Multiethnicity and Multiethnic Families. Honolulu, HI: A Le‘a Publication; 2010. [Google Scholar]
- 10.Adler N. Health disparities through a psychological lens. Am Psychol. 2004;64:663–673. doi: 10.1037/0003-066X.64.8.663. [DOI] [PubMed] [Google Scholar]
- 11.Williams D, Mohammed S. Discrimination and racial disparities in health: evidence and needed research. J of Beh Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Essed P. Understanding everyday racism: An interdisciplinary theory. London: Sage Publications; 1991. [Google Scholar]
- 13.Williams D, Neighbors H, Jackson J. Racial/ethnic discrimination and health: findings from community studies. Am J Publ Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler R, Mickelson K, Williams D. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J of Health & Soc Beh. 1999;40:208. [PubMed] [Google Scholar]
- 15.Mossakowski K. Dissecting the Influence of Race, Ethnicity, and Socioeconomic Status on Mental Health in Young Adulthood. Res on Aging. 2008;30:649–671. [Google Scholar]
- 16.Williams D, Yu Y, Jackson J, Anderson N. Racial differences in physical and mental health: Socio-economic status, stress, and discrimination. J of Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 17.Guyll M, Matthers K, Bromberger J. Discrimination and unfair treatment: Relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20:315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- 18.Lewis T, Everson-Rose S, Powell L, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN heart study. Psy Med. 2006;68:362–268. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- 19.Lewis T, Aiello A, Leurgans S, et al. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Beh, and Imm. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor T, Williams C, Makambi K, et al. Racial discrimination and breast cancer incidence in US Black women. Am J of Epid. 2007;166:46–54. doi: 10.1093/aje/kwm056. [DOI] [PubMed] [Google Scholar]
- 21.Williams D, Gonzalez H, Williams S, Mohammed S, Moomal H. Perceived discrimination, race and health in South Africa. Soc Sci and Med. 2008;67(3):441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gee G, Ro A, Gavin A, et al. Disentangling the effects of racial and weight discrimination on Body Mass Index and obesity among Asian Americans. Am J Publ Health. 2008;98(3):493–500. doi: 10.2105/AJPH.2007.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tull E, Wickramasuriya T, Fraser H, et al. Relationship of internalized racism to abdominal obesity and blood pressure in Afro-Caribbean women. J Nat Med Assoc. 1999;91(8):447–452. [PMC free article] [PubMed] [Google Scholar]
- 24.Wise L, Palmer J, Rosenberg L. Perceived racism in relation to weight change in the black women's health study. Ann Epidemiol. 2009;19(6):379–387. doi: 10.1016/j.annepidem.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams D, Yu Y, Jackson J. Racial differences in physical and mental health: Soceio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 26.Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Application and Programing. 2nd ed. New York, NY: Routledge; 2010. [Google Scholar]
- 27.McCubbin LM, McCubbin HI. Overt and covert discrimination: Confirmatory factor analysis of the Everyday Discrimination Scale. In: McCubbin LM, McCubbin HI, Sievers JA, editors. Assessment Measures of Stress, Coping, and Resilience: Theory, Research, and Practice. Pullman, WA & Honolulu, HI: Washington State University and University of Hawaii; in press. [Google Scholar]
- 28.McCubbin LM, McCubbin HI. Family resilience and ethnicity. In: Beaver D, editor. Handbook on Resilience. New York, NY: Springer; 2012. [Google Scholar]
- 29.American Psychological Association, author. Dual pathways to a better America: Preventing discrimination and promoting diversity. [April 7 2012]. http://www.apa.org/pubs/info/reports/promoting-diversity.aspx.
- 30.Sue D, Sue D. Counseling the culturally diverse: Theory and Practice. Hoboken, NJ: Wiley & Sons; 2008. [Google Scholar]
- 31.Center for Disease Control and Prevention, author. Healthy Weight: Assessing Your Weight: Body Mass Index (BMI) [September 13, 2011]. http://www.cdc.gov/healthyweight/assessing/bmi/
- 32.Garmezy N. Stressors of childhood. In: Garmezy N, Rutter M, editors. Stress, Coping and Development in Children. New York, NY: McGraw Hill; 1983. [Google Scholar]
- 33.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsy. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 34.Werner E, Smith R. Overcoming the Odds: High Risk Children from Birth to Adulthood. Ithaca, NYL: Cornell University Press; 1992. [Google Scholar]
- 35.Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. San Francisco, CA: Jossey-Bass; 1987. [Google Scholar]
- 36.Frankl V. Man's Search for Meaning: An Introduction to Logotherapy. New York, NY: Beacon Press; 1963. [Google Scholar]
- 37.Census Data: http://hawaii.gov/dbedt/info/census/Census_2010/SF2/index_html. [January 2, 2012].


