Abstract
Little is published about dietary intake of children of ethnic populations found in Hawai‘i, due to an absence of national statistics collected on Hawai‘i's population. This information is needed to focus planning of food, agriculture and health programs aimed to prevent obesity and related chronic disease and to improve health. Dietary patterns of 156 Native Hawaiian (n=110), Filipino (n=28) and White (n=18) children and their caregivers were compared using socio-demographic, annual “food season,” and 24 hour dietary recall data from a baseline survey of four lower income communities selected for an intervention program in rural Hawai‘i. Ethnic differences were found in the Healthy Eating Index (HEI) dairy component, and in calcium and vitamin C nutrient intakes among caregivers only (adjusting for food season). Whites always had higher intakes of these foods and nutrients than Filipinos or Native Hawaiians. Vitamin C intake remained significantly different among ethnic groups after further adjusting for dairy food group intake. Dietary patterns showed low intake of fruits and vegetables, fiber and dairy foods among these understudied populations.
Introduction
The prevalence of obesity in the United States has more than doubled in the past three decades, and reveals ethnic disparity.1,2 The Early Childhood Longitudinal Study, Birth Cohort (ECLS-B) reported racial/ethnic disparity in obesity in US children as young as four years, with the highest prevalence of obesity found in American Indian/Native Alaskan children. Indeed, obesity has been found to be twice as common in American Indian/Native Alaskan children as in non-Hispanic White or Asian children.3 There are few data on dietary intake of Native Hawaiian or Filipino children in Hawai‘i, though available data from the Pacific region suggests diets of poor nutritional quality and children with high rates of obesity.4 Dietary patterns of Native Hawaiian and Filipino populations are not described in national food consumption surveys, nor are such data routinely collected in Hawai‘i. Therefore, the purpose of this paper is to examine the ethnic differences (Native Hawaiian, Filipino and White) in food group, nutrient and healthy eating index dietary components among 6–13 year old children and their caregivers in selected rural communities in Hawai‘i where these ethnic groups predominate.
Methods
The study was approved by the Institutional Review Board at the University of Hawai‘i at Manoa, and informed consent and assent were obtained. Health center personnel made the initial contact with eligible child-caregiver pairs, and scheduled study visits were in compliance with Health Insurance Portability and Accountability Act privacy rules. Through the fall of 2005 and summer of 2006, interviews were conducted at the health center or at the respondent's home, according to their preference and availability.
Participants were drawn from two rural sites on O‘ahu and two sites on the Big Island of Hawai‘i in the state of Hawai‘i, selected for rural location and high proportion of Native Hawaiian population. On the island of O‘ahu, child-caregiver pairs were selected from local health center patient databases. In these communities, eligibility criteria included: (1) Child had an encounter with the health care facility during the past 2 years, and (2) Child was 8–12 years old at the time of the pre-intervention survey interview.
For the two sites on the Big Island of Hawai‘i, sampling was done according to census tracts.5 A random cluster sampling technique was used to identify how many children from each census block would be recruited. Within the selected census block cluster, data collectors went systematically from door to door to obtain the specified proportion of respondents, until the desired sample was achieved. The overall response rate was 80%. In total, 183 child - caregiver pairs were interviewed.
Questionnaires were administered to both the caregiver and the child. There is a high level of ethnic mixing in Hawai‘i. Thus, care-givers were asked the standard ethnic identity question, “What ethnic or racial group do you most identify with?” However, they were permitted to identify more than one group. The following ethnic groups were provided on the questionnaire: Native American, African American/Black, Chinese, Filipino, Japanese, Korean, Hispanic, Hawaiian/Part-Hawaiian, Other Pacific Islander, and White. The following algorithm was used to define ethnicity for the presented analyses:
Native Hawaiian - if the subject checked Hawaiian/Part-Hawaiian. (However, this group could be mixed with other ethnic groups, which were White, Chinese, Filipino, Japanese, Korean, Hispanic, Pacific Islander, Native American or African American. Only Hawaiian ethnicity was reported by 85 of 110 individuals, while 18/110 reported one other ethnicity, six reported two other ethnicities and three reported three other ethnicities).
Filipino - if the subject checked Filipino and did not check Hawaiian/Part-Hawaiian. (This group could be mixed with other ethnic groups which included White, Chinese, Japanese, Korean, Hispanic, Pacific Islander, Native American or African American. Filipino ethnicity only was reported by 22 of 28, while 6 of 28 reported one other ethnicity).
White - if the subject checked White and did not select Hawaiian/Part-Hawaiian or Filipino. (This group could be mixed with the Chinese, Japanese, Korean, Hispanic, other Pacific Islander, Native American or African American. However, no other ethnic group was reported for any White participant).
Twenty-seven child-caregiver pairs who did not meet the ethnic criteria for this analysis were excluded due to small sample size of that ethnic group (those who were either 100% Chinese, Japanese, Korean, Hispanic, other Pacific Islander, Native American, African American, or who they said they were mixed but were unable to specify the mixture). Thus, 156 child-caregiver pairs were included in the analysis (18 White, 28 Filipino, 110 Native Hawaiian). Among those who had specified the type of caregiver (144 out of the 156 caregivers), 82% (118 out of 144) were a parent.
A single 24-hour dietary recall was collected from each child and then from their caregiver using a modified USDA five-step multiple pass methodology.6 Children were interviewed directly, but the assistance of caregivers was accepted when the child could not remember. To decrease the length of time for the food recall, time and occasion of food and beverage consumption were collected in combination with either the first or third step, yielding a four-step method. A simple set of measuring instruments and plastic food models was used to aid in quantification of amount consumed and a list of commonly “forgotten foods” was used as a prompt during the last stage of the recall. One-sixth of recalls were collected on Mondays, in order to include (recalled) weekend intake. All other recalls reflected weekdays. Data collectors were trained staff from the Healthy Living in the Pacific Islands, Healthy Pacific Child Project, and Healthy Foods Hawai‘i Project at the University of Hawai‘i at Manoa (Novotny R, PI). Healthy Eating Index (HEI) component scores were calculated for nine HEI components: grain, vegetables, fruits, dairy, meat, total fat, saturated fat, cholesterol, and sodium, with a score of 1–10 for each component.7
In addition, data for education and socio-demographic characteristics of the caregiver (birth date, sex, marital status, and years of education) were collected. The completed number of years of school and the employment status were recorded. If employed, the caregiver was asked for hours/week worked, which was classified as: 1 = Seasonally/Occasionally employed; 2 = Part time (less than 30 hrs/wk); 3 = 30–40 hrs/wk; 4 = More than 40 hrs/wk. Due to the high number of unemployed persons and the prevalence of bartering for goods in the community, a material style of living score developed for use in rural, semi-subsistence economies was computed to estimate socio-economic status based on ownership of various items (TV, car, microwave, etc) in working condition available in their household.8
To determine if the study samples were homogeneous, differences between the community of residence, material style of living, and caregiver education among the three ethnic groups were tested using Fisher's exact test in SAS (version 9.1.3, 2002–2003, SAS Institute Inc, Cary, NC) PROC FREQ.
Before performing statistical analysis, the data for dietary intakes were processed using the University of Hawai‘i Cancer Center's food composition database, which contains local foods and recipes not found in the USDA standard reference.9 Food group data were compared to Food Guide Pyramid reference values that were used at the time of analysis.10 To determine if there were ethnic differences in the average dietary intakes, first the overall ethnic effect on any of the food groupings (or the nutrients, or the HEI scores) was simultaneously tested using multivariate analysis of variance (MANOVA). Statistical analyses were conducted using SAS PROC GLM. For both children and caregivers, three independent MANOVAs were performed for food groups, nutrients, and HEI scores. If the results of MANOVA indicated that there was a significant overall ethnic effect, then individual ANOVA were performed to test if the individual elements of the food/nutrient/HEI score was influenced by ethnic group. Multiple comparisons were adjusted for at p<0.05 using the methods of Benjamini and Hochberg.11 Following the individual ANOVA tests, pairwise comparisons (Tukey's honest significance test) were performed on those that showed significant ethnic effect to determine magnitude of effect. All models were adjusted for the potential confounders of age, sex, and “food season.” To adjust for expected “seasonal” (holiday) variation in dietary intake, “food season” variables were created and defined as follows:
Halloween (yes, if measured between October 31, 2005 and November 10, 2005; or no for any other date)
Winter holiday (yes, if measured between November 20, 2005 and January 7, 2006; or no for any other date)
Summer vacation (yes, if measured during June, July, or August in 2006; Or no for any other date)
School year (yes, if measured between January 8 and January 31, February, March, April, May, September October, and between November 11 and November 19 in 2005 or 2006).
Results
Table 1 summarizes the demographic characteristics of children and caregivers in the analysis. On average, children were 10 years old, ranging from 6 to 13 years old. The average age of caregivers was 40, ranging from 15 to 78 years old. Seventy percent of caregiver respondents were Native Hawaiian and 96% were females. Forty percent of caregiver respondents were unemployed and 30% worked full time (40 hrs/wk or more). The average number of years of education among caregivers was 12.5 years and ranged from 0 to 18 years. The calculated average score of material style of life was 4.7 on a scale of 1 to 7. No significant differences were found by community of residence, material style of living, or caregiver education among the three ethnic groups, indicating that this subset of population consisting Hawaiians, Filipinos, and Whites have similar socio-economic status.
Table 1.
Demographic characteristics of children (N=156) and caregiversa (N=156) in the study.
| Mean ± SD | Range | |
| Age | ||
| Child age, yrs | 9.96 ± 1.18 | 6.7–13 |
| Caregiver age, yrs | 40.18 ± 11.02 | 15–78 |
| Education | ||
| Caregiver education, yrs | 12.53 ± 2.37 | 0–18 |
| Material style of life scoreb (1–7) | 4.68 ± 1.08 | 1–7 |
| Ethnicity - Caregiver Ethnic Group | ||
| Native Hawaiian | 70% | |
| Filipino | 18% | |
| White | 12% | |
| Sex | ||
| Child sex, females | 47% | |
| Caregiver sex, females | 96% | |
| Employment | ||
| Unemployed | 40% | |
| Seasonally/Occasionally employed | 8% | |
| Employed less than 30 hrs/wk | 7% | |
| Employed for 30–40 hrs/wk | 15% | |
| Employed for more than 40 hrs/wk | 30% | |
| Food Seasonc | ||
| Halloween (Oct. 31st – Nov. 10th) | 3% | |
| Holiday (Nov. 20th – Jan. 7th) | 14% | |
| No school (Jun., Jul., & Aug.) | 11% | |
| Schoolc | 72% | |
Mother=111; Father=6; Foster parent=2; Foster grandparent=1; Grandmother=20; Aunt=2; Sibling=1; Babysitter=1 and Missing=12.
Ownership of various items (TV, car, microwave, etc…)
Food season in 2005–2006. School includes: January 8th to January 31st, February, March, April, May, September, October 1st to October 29th and November 11th to November 19th.
Mean nutrient intakes were described for children and for caregivers in Table 2 and were adjusted for the potential confounders of age, sex, and “food season.” Recommended intakes for comparison are for 9–13 and 31–50 year olds, based on the recommended dietary allowances or adequate intakes from US Department of Agriculture,12 except for sodium, which is the tolerable upper intake level. Percent of calories from protein, fat, and carbohydrate are acceptable macronutrient distribution ranges. Recommended energy level is based on women 25 – 50 years in Basiotis, et al.13 Recommendations for cholesterol and percent of calories from saturated fat are from the 2010 Dietary Guidelines.14 Seventy-two percent of respondents reported that the recorded intake was typical or “usual.”
Table 2.
Children and caregivers' nutrient intake (mean ± SE) by ethnic group and compared to recommended nutrient intakes for individuals. Means for “Total” are arithmetic means; Means for “Native Hawaiian,” “Filipino,” and “White” are least-squares means computed for each ethnic group after adjusting for age, sex, and food season.
| Child (n=156) | Caregiver (n=156) | |||||||||
| Nutrient Intake | Recommended Intake1 | Total (N=156) | Native Hawaiian (n=110) | Filipino (n=28) | White (n=18) | Recommended Intake | Total (N=156) | Native Hawaiian ( n=110) | Filipino (n=28) | White (n=18) |
| Energy, kcal | 2000 | 2195 ± 63 | 2213 ± 75 | 2137± 152 | 2175 ± 188 | 2200 | 1956 ± 79 | 1960 ± 93 | 1763 ± 185 | 2232 ± 231 |
| Protein, g | 0.76a | 75 ± 3 | 76 ± 3 | 71 ± 6 | 73 ± 8 | 0.66a | 76 ± 3 | 77 ± 4 | 71 ± 8 | 76 ± 10 |
| Total Fat, g | ND | 80 ± 3 | 81 ± 3 | 75± 7 | 77± 8 | ND | 76 ± 4 | 78 ± 4 | 63 ± 8 | 82 ± 10 |
| Cholesterol, mg | <300c | 273 ± 15 | 285 ± 19 | 248± 38 | 244 ± 47 | <300c | 320 ± 21 | 327 ± 25 | 265 ± 49 | 363 ± 62 |
| Carbohydrate, g | 100 | 300 ± 10 | 300± 12 | 298 ± 24 | 304 ± 30 | 100 | 245 ± 11 | 240 ± 13 | 232 ± 25 | 294 ± 31 |
| Total Fiber, g | 28b | 13 ± 1 | 13 ± 1 | 12 ± 2 | 15 ± 2 | 28b | 12 ± 1 | 12 ± 1 | 12 ± 1 | 16 ± 2 |
| Calcium, mg | 1100 | 858 ± 46 | 818 ± 52 | 831 ± 106 | 1141 ±131 | 800 | 592 ± 39 | 576 ± 45* | 416 ± 89** | 964 ± 111 |
| Phosphorus, mg | 1055 | 1177 ± 40 | 1180 ± 45 | 1093 ± 92 | 1285 ± 114 | 580 | 1029 ± 45 | 1033 ± 53 | 871 ± 106 | 1253 ± 133 |
| Iron, mg | 5.7–5.9 | 13 ± 1 | 14 ± 1 | 12 ± 2 | 15± 2 | 6–8.1 | 12 ± 1 | 12 ± 1 | 12 ± 2 | 13 ± 2 |
| Sodium, mg | 1500 | 3326 ± 139 | 3367 ± 162 | 3294 ± 331 | 3125 ± 409 | 1500 | 3200 ± 174 | 3272 ± 210 | 2814 ± 417 | 3365 ± 521 |
| Potassium, mg | 4.5 | 2242 ± 87 | 2188 ± 103 | 2179 ± 211 | 2667 ± 261 | 4.7 | 2190 ± 103 | 2142 ± 120 | 1916 ± 238 | 2914 ± 298 |
| Vitamin A RAEs, mcg | 420–445 | 807 ± 55 | 796 ± 66 | 712 ± 135 | 1022 ± 167 | 500–625 | 706 ± 52 | 683 ± 63 | 634 ± 124 | 954 ± 156 |
| Riboflavin, mg | 0.8 | 2 ± 0.1 | 2 ± 0.1 | 2 ± 0.2 | 3 ± 0.3 | 0.9–1.1 | 2 ± 0.1 | 2 ± 0.1 | 1.4 ± 0.2 | 2 ± 0.3 |
| Folate DFE, mcg | 250 | 453 ± 27 | 441 ± 32 | 397 ± 64 | 610 ± 79 | 320 | 384 ± 21 | 382 ± 25 | 293 ± 50 | 536 ± 62 |
| Vitamin C, mg | 39 | 118 ± 12 | 120 ± 15 | 93 ± 30 | 143 ± 37 | 60–75 | 130 ± 12 | 121 ± 14* | 93 ± 28** | 248 ± 35 |
| Vitamin D, mcg | 10 | 195 ± 14 | 182 ± 16 | 200 ± 32 | 266 ± 40 | 10 | 111 ± 12 | 118 ± 15 | 82 ± 30 | 111 ± 37 |
| % calories from protein | 10–30c | 14 ± 0.3 | 14 ± 0.4 | 14 ± 0.7 | 13 ± 1 | 10–35c | 16 ± 0.4 | 14 ± − 0.4 | 13 ± − 1 | 14 ± − 1 |
| % calories from fat | 25–35c | 33 ± 1 | 33± 1 | 33 ± 2 | 31 ± 2 | 20–35c | 35 ± 1 | 33 ± − 1 | 32. ± − 2 | 31 ± − 2 |
| % calories from saturated fat | <10c | 11 ± 0.3 | 11 ± 0.3 | 11 ± 1 | 11 ± 1 | <10c | 11 ± 0.3 | 11 ± − 0.3 | 10.8 1 | 11.2 ± − 1 |
| % calories from carbohydrate | 45–65c | 54 ± 1 | 54 ± 1 | 54 ± 2 | 57 ± 2 | 45–65c | 50± 1 | 54 ± −1 | 55 ± − 2 | 56 ± − 2 |
P-values for all pairwise comparisons among the three ethnic groups are adjusted by Tukey's method.
Recommended intakes are for 9–13 and 31–50 y, based on the Estimated Average Requirements (EAR), Recommended Dietary Allowances (RDAs, eg, for sodium) or Adequate Intakes (AIs, eg, potassium) (14), percent of calories from protein, fat, and carbohydrates are Acceptable Macronutrient Distribution Ranges (AMDRs). Recommendations for cholesterol and % of calories from saturated fat are from the 2010 Dietary Guidelines (12).
Estimated Average Requirement for protein is 0.76 per kilogram of body weight per day for girls and boys 9–13y, and is 0.66 per kilogram of body weight per day for adults 31–50y.
14g/1000 kcal
Acceptable Macronutrients Distribution Ranges for Energy, Carbohydrates, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (2002/2005).
Native Hawaiian significantly different from White (P=<0.05).
Filipino significantly different from White (P=<0.05).
The fiber content of both child and caregiver diets was particularly low (approximately half of the recommended levels), and sodium intakes were particularly high (especially among caregivers). Intakes of three food groups were low for children: fruits (1.78 ± .18 vs 2.7 recommended servings/d), vegetables (2.11 ± .16 vs 3.7 servings/d), and whole grains (.95 ± .11 whole grain servings/d vs 3 servings/day). Conversely added sugar intake was high (23.7 ± 1.2 vs < 10 teaspoons/d). Among caregivers, total grain intake (5.97 ± .28 vs 9 servings/d), vegetable intake (2.83 ± .19 vs 4 servings/d), fruit intake (1.8 ± .23 vs 3 servings/d), and dairy intake (.8 ± .09 vs 3 servings/d) were low.
The analysis results of MANOVA for children show that there was no significant overall ethnic effect on any food group, nutrients, or HEI scores. For caregivers, on the other hand, the overall effect of ethnic group on nutrients and HEI scores was significant at the P < .05 level, but not on food groups; in other words, the average consumption of nutrients and HEI scores were statistically different among the three ethnic groups. The values of Wilks' lambda and the associated P-value (in parentheses) were .59 (.071), 1.65 (.005), and 1.91 (.015) for food groups, nutrients and HEI scores, respectively. The summary statistics and test results of individual ANOVA and pairwise comparisons are presented in Table 2 for nutrients and in Figure 1 for HEI scores. Both children's and caregivers' data are presented.
Figure 1.
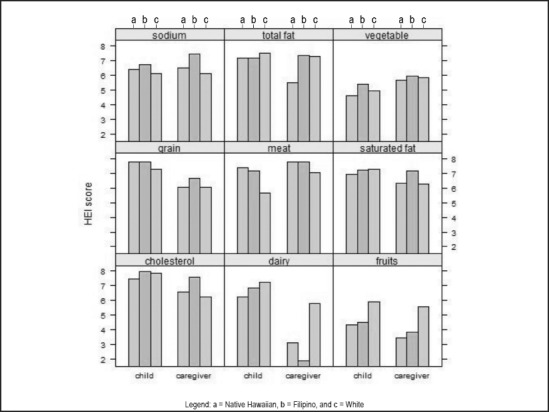
Child and caregiver Healthy Eating Index (HEI) individual component scores (range 1–9). Note that for sodium, total fat, and cholesterol, higher HEI scores mean lower intakes. Models are adjusted for age, sex, and food season; PROC GLM procedure. The dairy HEI scores for Native Hawaiians and Filipinos are both statistically different from White at P<0.05 level for caregivers.
For caregivers, the results of pairwise comparisons among the three ethnic groups indicate that the mean intakes of calcium among Native Hawaiians and Whites are statistically different at the P < .05 level, the mean intakes of vitamin C for Hawaiians and Filipinos are both statistically different from the mean intake of vitamin C for Whites, and the dairy HEI scores for Hawaiians and Filipinos are both statistically different from Whites at P-value < .05 level. White values were always higher.
Furthermore, to investigate if the differences between the mean intakes of calcium and vitamin C, and the dairy HEI scores for the three ethnic groups were due to total dairy consumption and not because of different ethnic group, total dairy consumption was included as one of the covariates in the model for caregivers. Indeed, the ethnic difference in calcium consumption and dairy HEI score was due to differences in total dairy consumption, but ethnic differences in vitamin C intake persisted (White values were higher).
Discussion
Caregiver's food intake varied by ethnicity but mixed ethnicity and lack of specificity of child's ethnic group may explain the lack of differences in dietary intakes between children of different ethnic groups. On the other hand, the finding may reflect a true lack of ethnic difference among children, a plausible occurrence due to Westernization or acculturation of dietary habits.15 Increased intake of dairy foods would improve dietary quality of the population and may be valuable in weight management.16 While the prevalence of lactose maldigestion is not known in this population, there are known strategies for consuming milk (such as consuming milk in small portions, or consuming live-culture yoghurt) that improve lactose tolerance and could be promoted, along with information about the substantial health promoting nutrients in dairy foods.17,18 Certainly culturally-favored food approaches to obtaining these nutrients should be prioritized. Increasing intake of fresh fish, root vegetables and fresh fruit (and decreasing canned meat) would be a good approach to improve dietary quality with foods familiar to the Pacific region. Measures of socioeconomic status and caregiver education did not explain differences in food and nutrient intake of children or caregivers, though our study sample is somewhat small and homogenous; still, no effect of socioeconomic status was found in larger studies with other Pacific ethnic groups.4 Although questionnaires and recalls were interviewer administered, dietary intake was self-reported with the potential for over and underreporting,19 especially among children whose cognitive processing of dietary information is likely limited.20 On the other hand, underreporting is less common in younger children than among older adolescents. This study employed trained interviewers who were familiar with local foods and customs, and used an established multiple pass method6 to improve accuracy.
The local foods and recipes that are carried on the Cancer Center of Hawai‘i's food composition database allowed for more accurate dietary nutrient estimates than if US Department of Agriculture14 alone had been used. We did not assess ethnic differences in the prevalence of nutrient inadequacy (ie, the prevalence of usual nutrient intakes below the Estimated Average Requirement) because the relatively small samples of Filipino and White children and caregivers precluded estimation of a usual intake distribution. However, Martin, et al, have reported the prevalence of nutrient inadequacy for the total sample of children in this study, and found inadequacy of intakes of vitamins A, C, and E as well as of phosphorus and magnesium to be of particular concern, which was partially ameliorated with dietary supplement use in the communities.8
Overall, intakes of fruits, vegetables, and whole grains were lower than those recommended for children, while added sugar intakes were high. However, intakes of food groups and nutrients did not differ by ethnic group. Caregivers' intakes of several food groups were low. White caregivers had higher food group intakes (especially dairy) and had more nutrient-rich diets (especially Vitamin C) compared to Filipino or Native Hawaiian caregivers of the same socioeconomic status. Dietary intakes of children and caregivers varied by food season, which may provide a target for future intervention. Increasing dairy, vegetable, and fruit intake would substantially improve dietary quality of both children and caregivers in this population.
Confict of Interest
The authors report no conflict of interest.
Funding
USDA Grant 2004-35215-14252 (Novotny R, PI)
References
- 1.Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Beydoun M. The obesity epidemic in the United States-gender, age, socio-economic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 3.Anderson S, Whitaker R. Prevalence of obesity among US preschool children in different racial and ethnic groups. Archives of Pediatrics and Adolescent Medicine. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 4.Paulino Y, Coleman P, Davison N, Lee S, Camacho T, Tenorio L, Murphy S, Novotny R. Nutritional characteristics and body mass index of children in the Commonwealth of the Northern Mariana Islands. Journal of the American Dietetic Association. 2008;108:2100–2104. doi: 10.1016/j.jada.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 5.US Census Bureau, author. United States Census 2000. 2000. http://www.census.gov.
- 6.Conway J, Ingwersen L, Vinyard B, Moshfegh A. Effectiveness of the US Department of Agriculture 5-step multiple pass method in assessing food intake in obese and non-obese women. The American Journal of Clinical Nutrition. 2003;77:1171–1178. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- 7.Murphy S. Unique nutrition support for research at the Cancer Research Center of Hawaii. Hawaii Med J. 2002;61:15–17. [PubMed] [Google Scholar]
- 8.DeWalt B. Modernization in a Mexican Ejido. A case study in economic adaptation. Cambridge, Massachusetts: Cambridge University Press; 1979. [Google Scholar]
- 9.Martin C, Murphy S, Novotny R. Contribution of dietary supplements to nutrient adequacy among children in Hawaii. Journal of the American Dietetic Association. 2008;108:1874–1880. doi: 10.1016/j.jada.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 10.US Department of Agriculture The Food Guide Pyramid 1992. http://fnic.nal.usda.gov/nal_display/index.php?info_center=4&tax_level=3&tax_subject=256&topic_id=1348&level3_id=5729.
- 11.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995;57:289–300. [Google Scholar]
- 12.USDA, author. Dietary guidelines for Americans, 2010. 7th ed. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 13.Basiotis P, Carlson A, Gerrior S, Lino M. The Healthy Eating Index: 1999–2000. US Department of Agriculture, Center for Nutrition Policy and Promotion: 2002. Tech. Rep. [Google Scholar]
- 14.USDA, author. USDA National Nutrient Database for Standard Reference, Release19. 2006. http://www.ars. usda.gov/ba/bhnrc/ndl.
- 15.Kivisto P. What is the canonical theory of assimiliation? Robert E Park and his Predecessors. Journal of the History of the Behavioral Sciences. 2004;40:149–163. doi: 10.1002/jhbs.20013. [DOI] [PubMed] [Google Scholar]
- 16.Zemel M, Miller S. Dietary Calcium and Dairy Modulation of Adiposity and Obesity Risk. Nutrition Reviews. 2004;62:125–131. doi: 10.1111/j.1753-4887.2004.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 17.Jackson S, Savaiano D. Lactose maldigestion, calcium intake and osteoporosis in African, Asian, and Hispanic Americans. Journal of the American College of Nutrition. 2001;20:198–207. doi: 10.1080/07315724.2001.10719032. [DOI] [PubMed] [Google Scholar]
- 18.Jarvis J, Miller G. Overcoming the barrier of lactose intolerance to reduce health disparities. Journal of Natural Medicines. 2001;94:55–66. [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson I, Rossner S. The Gustaf study: repeated, telephone administered 24-hour dietary recalls of obese and normal-weight men-energy and macronutrient intake and distribution over the days of the week. Journal of the American Dietetic Association. 1996;96:686–692. doi: 10.1016/S0002-8223(96)00189-7. [DOI] [PubMed] [Google Scholar]
- 20.Livingstone M, Robson P, Wallace J. Issues in dietary intake assessment of children and adolescents. British Journal of Nutrition. 2004;92:213–222. doi: 10.1079/bjn20041169. [DOI] [PubMed] [Google Scholar]


