Abstract
♦ Objectives: We explored the relationship between the experience level of nurses and the peritonitis risk in peritoneal dialysis (PD) patients.
♦ Methods: Our observational cohort study followed 305 incident PD patients until a first episode of peritonitis, death, or censoring. Patients were divided into 3 groups according to the work experience in general medicine of their nurses—that is, least experience (<10 years), moderate experience (10 to <15 years), and advanced experience (≥15 years). Demographic characteristics, baseline biochemistry, and residual renal function were also recorded. Multivariate Cox regression was used to analyze the association of risks for all-cause and gram-positive peritonitis with patient training provided by nurses at different experience levels.
♦ Results: Of the 305 patients, 91 were trained at the initiation of PD by nurses with advanced experience, 100 by nurses with moderate experience, and 114 by nurses with the least experience. Demographic and clinical variables did not vary significantly between the groups. During 13 582 patient–months of follow-up, 129 first episodes of peritonitis were observed, with 48 episodes being attributed to gram-positive organisms. Kaplan–Meier analysis showed that training by nurses with advanced experience predicted the longest period free of first-episode gram-positive peritonitis. After adjustment for some recognized confounders, the advanced experience group was still associated with the lowest risk for first-episode gram-positive peritonitis. The level of nursing experience was not significantly correlated with all-cause peritonitis risk.
♦ Conclusions: The experience in general medicine of nurses might help to lower the risk of gram-positive peritonitis among PD patients. These data are the first to indicate that nursing experience in areas other than PD practice can be vital in the training of PD patients.
Keywords: Peritonitis, nurse, training
For patients on peritoneal dialysis (PD), adequate training and ongoing support are extremely important (1–4), especially given the recent rapid increase in the number of elderly patients with significant learning disabilities and marked comorbidities (5). Although no standards had been published to guide the training and education process until recently (4), the importance of PD nurses as trainers has now been highlighted (2–4,6,7).
Peritonitis is the main cause of hospitalization, technique failure, and even mortality in PD patients. Given that peritonitis can be prevented by strengthening training in connection techniques and exit-site care (8–10), we hypothesized that a professional PD nursing team can lower the risk for peritonitis. However, evidence of an association between the experience of PD nurses and peritonitis rates is limited. In the only relevant study, Chow et al. observed a negative association between the length of time the nurse–trainer had been in PD practice and the peritonitis incidence (6). In that study, the authors defined “experience” as the number of years a nurse had been in practice in the dialysis unit. However, nursing experience in general medicine might be more helpful than experience in PD practice alone for dealing with PD patients having numerous comorbid conditions (4). In addition, communication and counseling skills, which are critical in establishing good nurse–client relations with patients and their family members so as to provide efficient training, are likely better in nurses with advanced experience in general medicine.
The PD program at the Peking University First Hospital has been in operation since 2002. In the first 2 years, nurses with varying durations of experience in general medicine were recruited from various wards and trained to be PD nurse specialists. We therefore had a unique chance to demonstrate, in a cohort study, the effect of nursing experience in general medicine on the risk of peritonitis in PD patients.
METHODS
SUBJECTS AND FOLLOW-UP
Our observational cohort study of incident PD patients was conducted between July 2002 and February 2007. All patients recruited had a dialysis vintage of more than 6 months and were regularly followed (at least once every 3 months). Patients were followed until they experienced a first episode of peritonitis or until censoring at death, transplantation, transfer to hemodialysis, or study end (April 2010).
Prophylactic cefazolin was administered before Tenckhoff catheter placement in all patients. Catheter and exit-site care in the postoperative period was performed as recommended (11). After catheter placement, dialysis was promptly initiated using a twin-bag connection system (Baxter Healthcare, Guangzhou, China) and lactate-buffered glucose PD solutions. The study was approved by the Medical Ethical Committee of Peking University. Written informed consent was obtained from every patient.
TRAINING AND RETRAINING PROGRAM
Training of a PD Nurse: During the first 2 years of operation of the new PD center, 10 female nurses (30.2 ± 6.5 years of age) were recruited and trained as PD nurse specialists. Before that, they had received basic training in nursing school for 3 years and had practiced in a medical ward for various durations. Specifically, the difference in the length of their PD practice was less than 2 years, but with regard to general medicine, 4 nurses had less than 10 years of experience (“least experience”), 3 had between 10 and 15 years of experience (“moderate experience”), and 3 nurses had more than 15 years of experience (“advanced experience”).
For 3 months, a full-time professional doctor coached the first 2 nurses on PD techniques, including PD concepts, catheterization, aseptic technique, exchange procedures, exit-site care, communication skills, and adult learning. The PD team also established a dialysis handbook for new PD patients, providing information about how to perform exchanges independently and correctly, and about aspects of volume control, blood pressure and glucose monitoring, diabetic foot care, travel, rehabilitation, and so on—all of which were extremely helpful for the nurses as well as the PD patients. Afterward, the first 2 nurses took charge of training, taught fresh PD nurses as part of their everyday practice (each for 1 month). Thus, in the first 2 years of center operation, 10 qualified PD nurses were trained. All the PD nurses also attended the continuing education sessions held by the hospital’s nursing department regardless of their experience level in general medicine.
Training and Retraining of a PD Patient: A primary nurse was randomly assigned to each patient at PD initiation. The nurses were not involved in selecting their patients; training assignments were made on a rotation basis. The standard initial training program lasts for 3 – 5 days or 5 – 7 sessions (1 – 2 hours per session). During the initial training, all patients receive video and verbal instruction on how to perform exchanges safely, how to recognize contamination or infection, and how to respond promptly to suspected contamination. Patients or their assistants are allowed to practice the PD procedure until it can be skillfully performed. Within the 1st month of PD, patients or their assistants can request to practice the procedure in the clinic if they need retraining, but home visits are not routinely arranged. Details of the training procedures have been published elsewhere (12). The ratio of nurses to patients in the training program was 1:1.
The retraining program consists of an exchange procedure check for patients who develop peritonitis, with individual retraining in exit-site care and connection techniques based on the findings during the procedure check, and group meetings focused on exit-site care and connection techniques periodically given by nurses and physicians to the entire cohort.
DEMOGRAPHIC AND BIOCHEMISTRY DATA
Demographics and comorbidities—including age, sex, height, weight, body mass index (BMI), literacy, annual income, need for assistance (exchanges performed by a family member or home assistant), diabetes, and Charlson comorbidity index (CCI)—were recorded within the week preceding PD catheter implantation (13,14). Albumin, hemoglobin, dialysis adequacy, residual renal function, and peritoneal transport rate were evaluated during the first 3 or 6 months as baseline values. One day before a clinic visit, 24-hour urine and effluent were collected.
Residual renal function was defined as the mathematical mean of renal clearance of urea and creatinine. Peritoneal transport rate was assessed as the 24-hour dialysate-to-plasma ratio (D/P) of creatinine. Peritoneal dialysate protein losses were measured using the 24-hour effluent collection. Biochemical parameters were examined using an automated analyzer.
PERITONITIS
The primary outcome was the incidence of peritonitis. Peritonitis was defined as the presence of at least 2 of the following conditions: abdominal pain or tenderness; presence of white blood cells in peritoneal effluent in excess of 100/mL, with at least 50% polymorphs; and positive dialysate culture results. Gram staining and cultures of dialysate effluent were performed for patients with peritonitis episodes. Peritonitis was treated using the standard recommended antibiotic protocol (11). Peritonitis rates were calculated by totaling the periods of PD treatment in all the study patients and dividing that total by the number of episodes of peritonitis that occurred during that time.
STATISTICAL ANALYSES
Statistical analyses were performed using SPSS for Windows (version 15.0: SPSS, Chicago, IL, USA). All continuous data are expressed as mean ± standard deviation. Nonparametric data are presented medians, with 25th – 75th percentile intervals. Categorical variables are expressed as percentages or ratios. Baseline differences between the study groups were assessed using the chi-square test for categorical variables and t-tests or Mann–Whitney tests for continuous variables, as appropriate. Kaplan–Meier survival curves were plotted for the hypothesized relationships, and differences between the groups were assessed using the log-rank test. A multivariate Cox proportional hazards regression model was used to predict the hazard of developing dialysis-related peritonitis. Analyses were censored at death, transplantation, and transfer to hemodialysis. The dependent variable was the time to first dialysis-related peritonitis. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated in the Cox models, which were adjusted for covariates that are believed to be potential confounders in peritonitis-free survival. On the basis of our previous work and that of others, variables that were used for modeling included age, sex, presence of diabetes mellitus, CCI, literacy, annual income, BMI, baseline albumin, hemoglobin, residual renal function, peritoneal protein loss, D/P creatinine, assisted PD, and training by nurses with various durations of experience in general medicine. All probabilities were two-tailed, and the level of significance was set at 0.05.
RESULTS
Table 1 provides information about the 305 patients who were eligible for inclusion in the study. This cohort [129 men; median age: 62 years (range: 19 – 94 years); 123 with diabetes; 115 (37.7%) being assisted with PD] had a total of 13 582 patient–months on PD. During that time, 129 first episodes of peritonitis occurred (48 gram-positive, 34 gram-negative, 3 fungi, 31 culture-negative, 13 with no culture result). The median time to first-episode peritonitis was 31 months (range: 18 – 52 months). The overall peritonitis rate during that time was 1 episode in 55.66 patient–months—that is, 244 episodes in 13 582 patient–months. The first-episode peritonitis led to 16 permanent transfers to hemodialysis (12.4%) and 17 deaths (13.2%); 96 patients remained on PD (74.4%).
TABLE 1.
Baseline Characteristics of the Study Patientsa
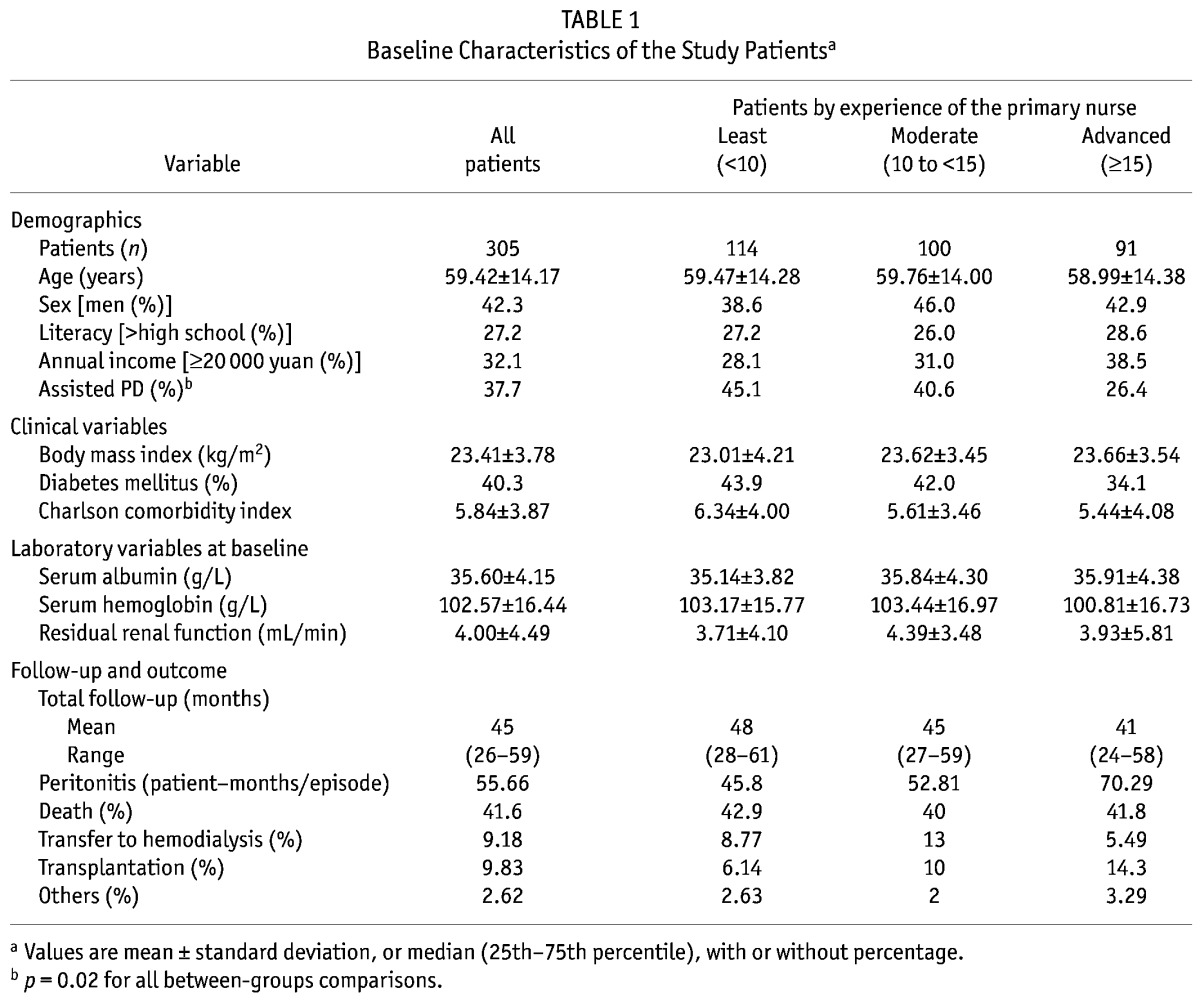
Of the study cohort, 91 patients were trained and managed by nurses with advanced experience, 100 by nurses with moderate experience, and 114 patients by nurses with least experience. Demographic and other clinical variables such as age, sex, literacy, annual income, BMI, presence of diabetes mellitus, CCI, baseline serum albumin, hemoglobin, and residual renal function did not vary significantly between those groups. Neither did the total follow-up period or the distribution of dropouts. The percentage of patients being assisted with PD was higher in the group taught by nurses with advanced experience (p = 0.02). In the least-, moderate-, and advanced-experience groups, the peritonitis rates were 1 episode in 45.8, 52.81, and 70.29 patient–months respectively.
We further analyzed the differences between the groups in the risk for all-cause and gram-positive peritonitis. Kaplan–Meier analysis showed that the patients trained by nurses with advanced experience had a significantly longer period free from gram-positive first-episode peritonitis (p = 0.02 compared with patients trained by nurses having moderate experience and p = 0.003 compared with those trained by nurses having least experience, Figure 1). After adjustments for age, sex, body mass index, residual renal function, hemoglobin, serum albumin, peritoneal protein loss, peritoneal transport rate, diabetes, CCI, education, income level, and assisted PD, peritonitis-free survival varied significantly with respect to the level of experience of the nurse providing PD training (Table 2). Compared with patients trained by nurses with advanced experience, those trained by nurses with moderate experience showed a trend to a higher risk for first-episode gram-positive peritonitis (HR: 2.69; 95% CI: 1.03 to 6.98, p = 0.04); patients trained by nurses with the least experience had a significantly higher risk (HR: 3.16; 95% CI: 1.20 to 8.30, p = 0.02). The difference in the risk for first-episode gram-positive peritonitis was not significantly different between the groups trained by nurses with moderate and least experience (p = 0.56). Being trained by a nurse with advanced experience did not result in a significantly longer time to first-episode all-cause peritonitis (Figure 2) or predict a lower peritonitis risk (Table 2) in a multivariate Cox regression model after adjustment for the earlier-mentioned variables. The gram-negative peritonitis risk did not vary between the groups (p = 0.27, data not shown).
Figure 1.
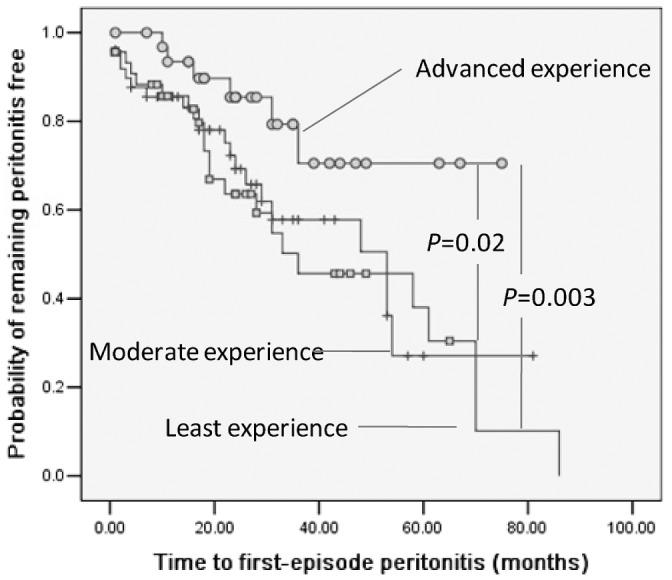
— Kaplan–Meier curves show the cumulative probability of gram-positive peritonitis–free survival according to the years of experience of the nurse providing care. Survival was significantly better in patients trained by nurses with 15 or more years of experience than in patients trained by nurses with between 10 and 15 years of experience and with less than 10 years of experience.
TABLE 2.
Independent Predictors of All-Cause and Gram-Positive Peritonitis (Cox Proportional Hazards Analysis)
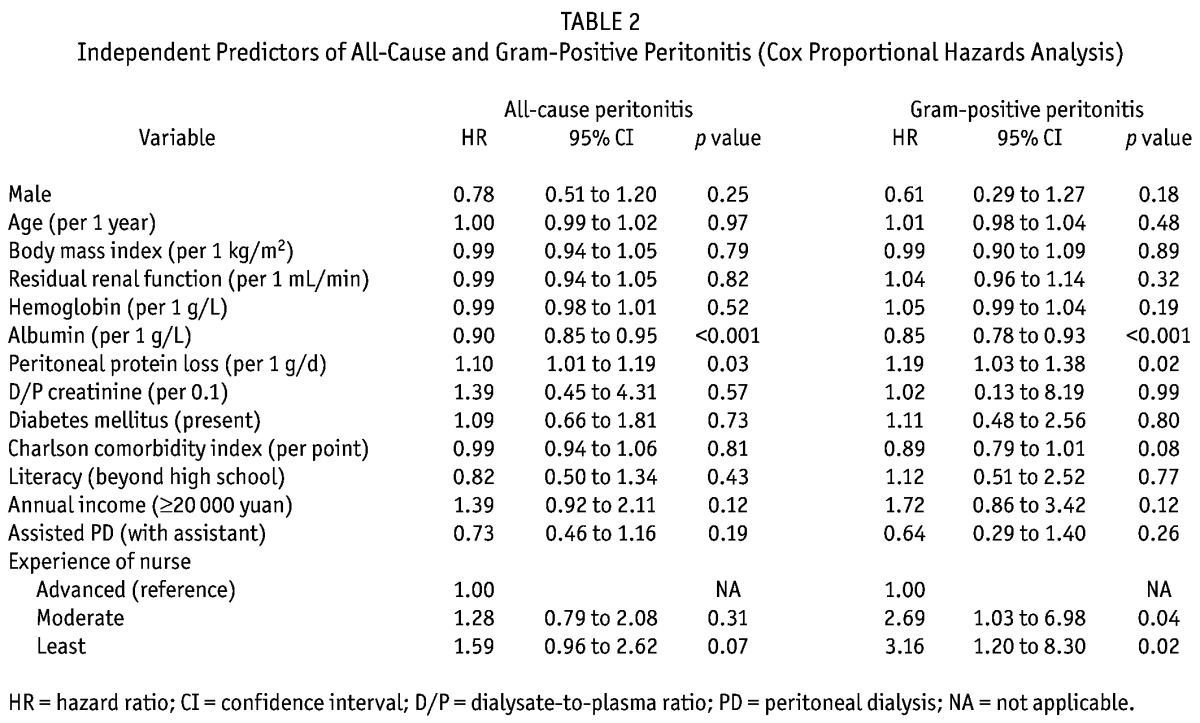
Figure 2.
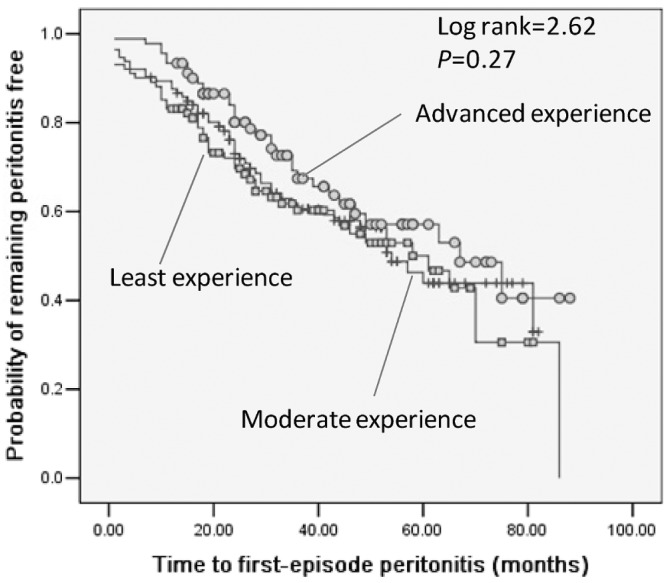
— Kaplan–Meier curves show the cumulative probability of all-cause peritonitis–free survival according to the years of experience of the nurse providing care. Survival was not significantly different in patients trained by nurses with 15 or more years of experience, with between 10 and 15 years of experience, and with less than 10 years of experience.
Baseline albumin independently predicted all-cause and gram-positive peritonitis (all-cause HR: 0.90; 95% CI: 0.85 to 0.95; p < 0.001; gram-positive HR: 0.85; 95% CI: 0.78 to 0.93; p < 0.001). Peritoneal protein loss was also associated with all-cause and gram-positive peritonitis (all-cause HR: 1.10; 95% CI: 1.01 to 1.19, p = 0.03; gram-positive HR: 1.19; 95% CI: 1.03 to 1.38; p = 0.02).
DISCUSSION
In this cohort study, a strong and independently positive association was found between the experience in general medicine of PD nurses and peritonitis-free survival in PD patients. Being trained and managed by nurses with advanced experience was associated with a decreased risk for gram-positive peritonitis (but not all-cause peritonitis), indicating a lesser possibility for touch contamination during exchanges. To the best of our knowledge, this study is the first to explore the relationship between the experience in general medicine of PD nurses and outcomes in PD patients.
Although our data cannot directly address the reason for the association between nursing experience in general medicine and peritonitis, several explanations are likely. First, the communication and counseling skills of more experienced nurses might be better than those of less experienced nurses. A nurse with advanced experience is more likely to be competent in teaching and helping patients to follow the instructional steps of sterile dialysis exchange technique. At the start of training, the nurse should first understand the physiologic and psychological status of each patient and judge whether that patient is really prepared to take in important information. During the training process, a nurse with advanced experience must be sensitive enough to recognize the obstacles encountered by patients in performing exchanges, such as weak eyesight, impaired functional ability, or cognitive dysfunction. Accordingly, a nurse with advanced experience will recommend a practical study plan using a negotiated care strategy, as they were observed to do in training on volume management (15). Also, a nurse with advanced experience might be good at inspiring patients to ask questions, providing immediate feedback during learner practice, and motivating patients or their assistants to do their best (16). During interactions, nurses with advanced experience can establish a good nurse–client relationship with patients and their family members (2), a step that has been cited as critical by all patients in terms of how those patients perceive the organization and structure of the PD facility (7). We presumed that all the foregoing skills might be strengthened with longer experience in nursing practice. A second reason for our finding is that broad-based experience in general medical or general surgical nursing (or both) are important for PD nurses (3,4). Given that various comorbidities are present throughout the PD population, nurses with advanced experience might help patients to detect peritonitis earlier and to prevent peritonitis episodes. However, the foregoing explanations must be further explored because we did not collect data to support these hypotheses.
Our findings suggest that an understanding of PD-related techniques is not enough for new PD nurses before they start to train PD patients. Formal preparation by education specialists in the principles of adult learning is very desirable for PD trainers (4). Because most health professionals have received no formal preparation for patient education (17), a PD nurse with advanced experience in general medicine has a critical role to play in continuously improving the quality of therapy through a well-constructed training program. To our knowledge, there are few clinical disciplines in which nurses play such a pre-eminent role in total patient care as in PD (3). The PD nurses are readily identified by patients as the principal source of advice on dialysis, medication, diet, and rehabilitation. Compliance with or adherence to therapy by patients depends chiefly on a successful therapeutic alliance: the contract established between patient and trainer (18). Therefore, nurses with advanced experience should share with other nurses their deep understanding of the importance of the nurse in helping patients to practice PD safely and of how mutual cooperation can ultimately facilitate successful PD (19). More studies need to be designed to further explore the efficacy of communication skills training for nurses in terms of improving the compliance of PD patients; such studies have already looked at the practice of nurses dealing with cancer patients (2,20).
The present study was a relatively large cohort study, and the first to evaluate the association between nursing experience and outcomes in PD patients, highlighting the role of nurses. Nursing practice in general medicine is an advantage for a PD nurse who must establish a strong and beneficial association with PD patients, suggesting that accumulation of experience is not limited to the PD specialty. Continuing education for PD nurses should always be emphasized.
We also recognize the limitations of our study. First, the observational design arguably cannot preclude bias. For example, patients trained by nurses with advanced experience were likely to need assistance with their exchanges. They also had a higher annual income compared with patients trained by the nurses with moderate and least experience. However, nurses who provided training did not select their patients; training occurs on a rotation basis in our unit. In any case, neither assisted PD not income level were predictors of peritonitis risk in the multivariate regression model. Second, our single-center study results cannot be extrapolated to other centers without confirmation with a sufficiently large sample size and long-term follow-up. Finally, this observational study lacked an objective assessment of the communication skills or training efficacy of the nurses, and further work should be done to explore the potential reasons for the association we observed.
CONCLUSIONS
Preparing patients to perform home dialysis safely and comfortably is a daunting task (4). Greater general medicine experience of nurses was found to be associated with a decreased risk for first-episode gram-positive peritonitis among PD patients. These data are the first to indicate that nursing experience outside of PD practice is vital in nurses who are training PD patients. The potential reasons for this association need to be further explored.
DISCLOSURES
The authors have no financial conflicts of interest to declare.
Acknowledgments
The authors express their appreciation to the patients and staff of the peritoneal dialysis center of First Hospital, Peking University, for their participation in this study.
REFERENCES
- 1. Chen TW, Li SY, Chen JY, Yang WC. Training of peritoneal dialysis patients—Taiwan’s experiences. Perit Dial Int 2008; 28(Suppl 3):S72–5 [PubMed] [Google Scholar]
- 2. Kong IL, Yip IL, Mok GW, Chan SY, Tang CM, Wong SW, et al. Setting up a continuous ambulatory peritoneal dialysis training program. Perit Dial Int 2003; 23(Suppl 2):S178–82 [PubMed] [Google Scholar]
- 3. Tan PC, Morad Z. Training of peritoneal dialysis nurses. Perit Dial Int 2003; 23(Suppl 2):S206–9 [PubMed] [Google Scholar]
- 4. Bernardini J, Price V, Figueiredo A. on behalf of International Society for Peritoneal Dialysis (ISPD) Nursing Liaison Committee. Peritoneal dialysis patient training, 2006. Perit Dial Int 2006; 26:625–32 [PubMed] [Google Scholar]
- 5. Jassal SV, Trpeski L, Zhu N, Fenton S, Hemmelgarn B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ 2007; 177:1033–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chow KM, Szeto CC, Law MC, Fun Fung JS, Li PKT. Influence of peritoneal dialysis training nurses’ experience on peritonitis rates. Clin J Am Soc Nephrol 2007; 2:647–52 [DOI] [PubMed] [Google Scholar]
- 7. Wuerth DB, Finkelstein SH, Kliger AS, Finkelstein FO. Patient assessment of quality of care in a chronic peritoneal dialysis facility. Am J Kidney Dis 2000; 35:638–43 [DOI] [PubMed] [Google Scholar]
- 8. Chow KM, Li PK. Peritoneal dialysis-related peritonitis: can we predict it? Int J Artif Organs 2007; 30:771–7 [DOI] [PubMed] [Google Scholar]
- 9. Bender FH, Bernardini J, Piraino B. Prevention of infectious complications in peritoneal dialysis: best demonstrated practices. Kidney Int Suppl 2006; (103):S44–54 [DOI] [PubMed] [Google Scholar]
- 10. Nasso L. Our peritonitis continuous quality improvement project: where there is a will there is a way. CANNT J 2006; 16:20–3 [PubMed] [Google Scholar]
- 11. Piraino B, Bailie GR, Bernardini J, Boeschoten E, Gupta A, Holmes C, et al. Peritoneal dialysis–related infections recommendations: 2005 update. Perit Dial Int 2005; 25:107–31 [PubMed] [Google Scholar]
- 12. Dong J, Chen Y. Impact of the bag exchange procedure on risk of peritonitis. Perit Dial Int 2010; 30:440–7 [DOI] [PubMed] [Google Scholar]
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–83 [DOI] [PubMed] [Google Scholar]
- 14. Fried L, Bernardini J, Piraino B. Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. Am J Kidney Dis 2001; 37:337–42 [DOI] [PubMed] [Google Scholar]
- 15. Quan L, Xu Y, Luo SP, Wang L, LeBlanc D, Wang T. Negotiated care improves fluid status in diabetic peritoneal dialysis patients. Perit Dial Int 2006; 26:95–100 [PubMed] [Google Scholar]
- 16. Oates DJ, Paasche–Orlow MK. Health literacy: communication strategies to improve patient comprehension of cardiovascular health. Circulation 2009; 119:1049–51 [DOI] [PubMed] [Google Scholar]
- 17. Bernardini J, Price V, Figueiredo A, Riemann A, Leung D. International survey of peritoneal dialysis training programs. Perit Dial Int 2006; 26:658–63 [PubMed] [Google Scholar]
- 18. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353:487–97 [DOI] [PubMed] [Google Scholar]
- 19. McCarthy A, Cook PS, Fairweather C, Shaban R, Martin–McDonald K. Compliance in peritoneal dialysis: a qualitative study of renal nurses. Int J Nurs Pract 2009; 15:219–26 [DOI] [PubMed] [Google Scholar]
- 20. Fukui S, Ogawa K, Ohtsuka M, Fukui N. A randomized study assessing the efficacy of communication skill training on patients’ psychologic distress and coping: nurses’ communication with patients just after being diagnosed with cancer. Cancer 2008; 113:1462–70 [DOI] [PubMed] [Google Scholar]


