Editor:
A 55-year-old man with hypertension, coronary artery disease, and end-stage renal disease was initiated on automated peritoneal dialysis with 2.5% Dianeal solution [Baxter (India) Private, Haryana, India] 14 days after Tenckhoff catheter placement. On day 0 of initiation, the peritoneal effluent was cloudy. Newspaper print was not visible through the effluent (Figure 1). The patient had no complaints of abdominal pain, fever, loose stools, or vomiting. No fibrin clots were evident, and there were no cells in the effluent. Gram stain, Ziehl–Neelsen stain, and KOH mount of the effluent were negative. Cultures for bacteria and fungi were sterile.
Figure 1.
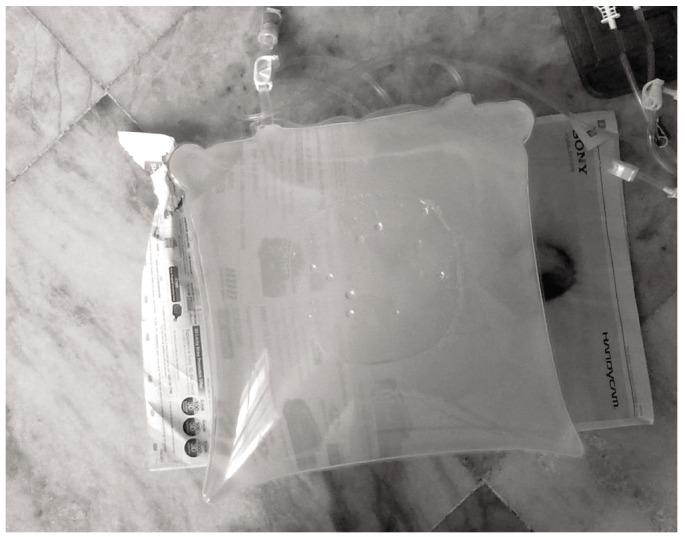
— Cloudy peritoneal fluid when diltiazem was being used.
The effluent remained cloudy for the next few days, but the patient had no symptoms. There were still no cells on repeat examination, and repeat staining and cultures of the effluent were also negative. The patient’s pulse was 78 bpm and his blood pressure was 130/80 mmHg. A clinical examination, including abdominal exam, was unremarkable. There were no clinical features suggestive of acute pancreatitis, solid-organ malignancy, or lymphoma.
Effluent triglycerides were measured. The levels were high at 54 mg/dL, 61 mg/dL, and 52 mg/dL on 3 consecutive days. Serum triglycerides were 134 mg/dL. Serum and effluent amylase levels were 12 U/dL and 10 U/dL respectively. In other investigations, serum creatinine was 8.8 mg/dL; blood urea nitrogen, 213 mg/dL; hemoglobin, 9.8 g/dL; and 24-hour urine protein, 230 mg. Contrast-enhanced computed tomography imaging of the abdomen revealed a normal pancreas. Effluent was also negative for malignant cells on repeat examination.
The surgeon reported that the catheter insertion had been atraumatic. The patient’s medications during this phase of cloudy peritoneal fluid were sevelamer carbonate, injection calcitriol, diltiazem, isosorbide mononitrate, aspirin, and vitamins.
Diltiazem, although not a dihydropyridine calcium channel blocker, was stopped. The next day, the effluent became translucent. There were no cells in the effluent. Effluent triglycerides fell to a normal level of 1.0 mg/dL. After 3 days, the diltiazem was added back to the patient’s medications. The effluent became cloudy again, and effluent triglycerides were now 55 mg/dL.
Cloudy peritoneal fluid is not always infection (1). An absence of cells excludes infection, intra- or juxta-peritoneal inflammation, allergic reaction to constituents of the dialysis system, air, and pharmaceuticals. Our patient was not using icodextrin, and so the cloudy effluent could not be attributed to that dialysate constituent. Traumatic insertion of the Tenckhoff catheter, acute pancreatitis, and malignancy were excluded. Other noninfectious causes of cloudy peritoneal fluid include radiation, sarcoidosis, retroperitoneal fibrosis, Whipple disease, dilated cardiomyopathy, nephrotic syndrome, congenital lymphatic abnormalities (2), Klippel–Trénaunay syndrome, primary lymphatic hyperplasia (3), amyloidosis (4), and systemic lupus erythematosus (5).
Dihydropyridine calcium channel blockers have been reported to produce cloudy (in fact almost white) effluent because of high triglyceride levels. The problem was first reported when manidipine was used (6). Subsequently, benidipine, nisoldipine, nifedipine (1), and lercanidipine (7) were also reported to produce cloudy dialysate (1). The present report is the first of cloudy effluent with the use of a non-dihydropyridine calcium channel blocker. The mechanism or mechanisms by which calcium channel blockers raise the triglyceride content in the peritoneal space is unknown (8). Data from the reported cases show triglyceride levels of 128.4 ± 133.0 mg/dL (7), 251 mg/dL (2), and between 12 mg/dL and 32 mg/dL (6) in peritoneal effluent when patients are receiving dihydropyridine calcium channel blockers.
DISCLOSURES
None of the authors have any relationships that could be perceived to represent a financial conflict of interest.
REFERENCES
- 1. Teitelbaum I. Cloudy peritoneal dialysate: it’s not always infection. In: Ronco C, Dell’Aquila R, Rodighiero MP, eds. Peritoneal Dialysis: A Clinical Update. Volume 150 Basel, Switzerland: Karger AG; 2006: 187–94 [DOI] [PubMed] [Google Scholar]
- 2. Tsao YT, Chen WL. Calcium channel blocker–induced chylous ascites in peritoneal dialysis. Kidney Int 2009; 75:868 [DOI] [PubMed] [Google Scholar]
- 3. Cheung CK, Khwaja A. Chylous ascites: an unusual complication of peritoneal dialysis. A case report and literature review. Perit Dial Int 2008; 28:229–31 [PubMed] [Google Scholar]
- 4. Sujan SS, Ruiz SR, Cobelo C, Campos CT. Chyloperitoneum: is secondary amyloidosis a possible cause? Perit Dial Int 2009; 29:582–3 [PubMed] [Google Scholar]
- 5. Graice R, Bargman JM. Regarding “calcium channel blocker–induced chylous ascites in peritoneal dialysis.” Kidney Int 2010; 77:165 [DOI] [PubMed] [Google Scholar]
- 6. Yoshimoto K, Saima S, Echizen H, Nakamura Y, Ishizaki T. A drug-induced turbid peritoneal dialysate in five patients treated with continuous ambulatory peritoneal dialysis. Clin Nephrol 1993; 40:114–17 [PubMed] [Google Scholar]
- 7. Yang WS, Huang JW, Chen HW, Tsai TJ, Wu KD. Lercanidipine-induced chyloperitoneum in patients on peritoneal dialysis. Perit Dial Int 2008; 28:632–6 [PubMed] [Google Scholar]
- 8. Yoshimoto K, Saima S, Nakamura Y, Nakayama M, Kubo H, Kawaguchi Y, et al. Dihydropyridine type calcium channel blocker-induced turbid dialysate in patients undergoing peritoneal dialysis. Clin Nephrol 1998; 50:90–3 [PubMed] [Google Scholar]


