Editor:
Malfunction of the peritoneal dialysis (PD) catheter is a common occurrence after insertion, often delaying patient training for PD (1–3). Several factors may be responsible for malfunction, including catheter malposition or migration, intraluminal obstruction (by fibrin strands or blood clots), and extraluminal obstruction (by omental wrapping or adhesions) (1).
After failure of conservative measures (such as the use of laxatives and an aggressive bowel routine) to restore catheter patency, stiff-wire manipulation under fluoroscopic guidance may be performed. This procedure is generally well tolerated and safe and has been reported to produce acceptable short-term results (4–6).
Here, we present the case of a 71-year-old man with end-stage renal failure because of polycystic kidney disease, on hemodialysis (HD) for approximately 8 years before undergoing kidney transplantation. He developed allograft failure 3 years afterward and was referred for initiation of PD. The patient underwent insertion of a spiral-tip, double-cuff, swan-neck PD catheter under fluoroscopic guidance. The procedure was tolerated well, with no complications.
Immediately after catheter insertion, successful inflow and outflow was achieved. However, after a 3-week healing period, inflow was noted to be slow, with no outflow possible. Additionally, a significant amount of fibrin was noted in the catheter. Conservative measures such as use of laxatives and recurrent catheter flushes with heparinized saline were unsuccessful. Abdominal radiography demonstrated that the tip of the PD catheter was appropriately located in the mid-pelvis (Figure 1).
Figure 1.
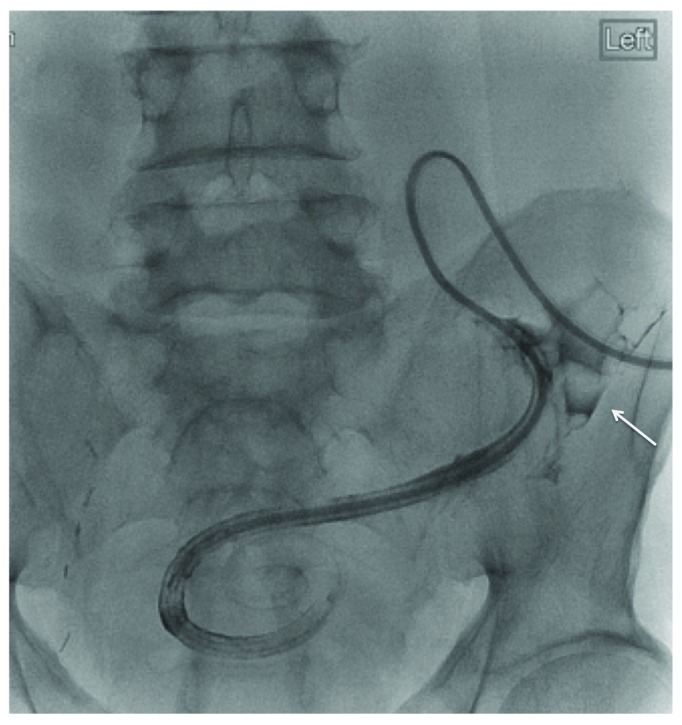
— Before manipulation, the peritoneal dialysis catheter is positioned in the mid-pelvis. Injected contrast is seen tracking retrograde along the catheter to the site of spillage in the lower left quadrant (white arrow).
Despite the appropriate position of the PD catheter, a decision was made to proceed to catheter manipulation under fluoroscopic guidance. The time interval from catheter insertion to manipulation was approximately 1 month. At the time of catheter manipulation, it appeared that the PD catheter was completely encased in a fibrin sheath. Injected contrast was seen tracking retrograde along the catheter to the site of spillage in the lower left quadrant (Figure 1). A stiff guidewire was therefore used to manipulate the catheter, displacing the catheter into the left paracolic gutter, with its tip near the splenic flexure. The PD catheter was intact, and in this new position, free injection and aspiration of fluid from the catheter, with excellent inflow and outflow, was attained. Interestingly, after the PD catheter was repositioned, the fibrin sheath from the catheter’s initial position remained in the pelvis (Figure 2).
Figure 2.
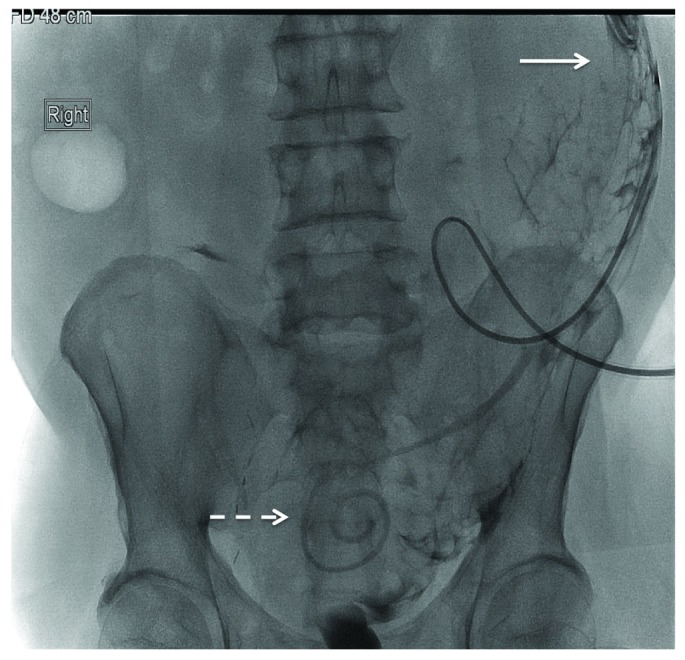
— After stiff-wire manipulation, the peritoneal dialysis catheter is visualized in its new position in the left paracolic gutter (white solid arrow). In the mid-pelvis, a contrast-filled fibrin sheath from the initial PD catheter placement is seen (white dashed arrow).
DISCUSSION
To our knowledge, this is the second case report of PD catheter failure as a result of complete encasement of the catheter by a fibrin sheath. Kazory et al. (7) reported a similar finding of two-way primary catheter obstruction because of catheter encasement in a fibrin sheath. In our case, inflow was slow, but not as compromised as outflow. This situation contrasts with the earlier case, in which inflow and outflow obstruction both occurred (7).
We hypothesize that, under the influence of the negative pressure of outflow, the fibrin sheath was pulled toward the external wall of the catheter, occluding the side ports and thus preventing dialysate outflow. However, inflow was less problematic given that the tip of the catheter was still patent. In addition, dialysate inflow might perhaps push the fibrin sheath away from the catheter, allowing dialysate inflow to occur (albeit more slowly) between the internal wall of the fibrin sheath and along the external surface of the catheter.
This case also highlights the efficacy of fluoroscopic stiff-wire manipulation to restore PD catheter function even in the absence of malposition of the PD catheter on abdominal radiography. Although catheter manipulation was also attempted in the case reported by Kazory et al. (7), the catheter was completely immobile and manipulation was unsuccessful. It is tempting to speculate that the degree of fibrosis, the thickness of the fibrin sheath coating the catheter, and the ability to either extract the catheter from the fibrin sheath or to disrupt the fibrin sheath might be important factors influencing the success of fluoroscopic manipulation.
Our patient presented with a significant degree of fibrin in the catheter soon after insertion. That finding may be a marker of a profibrotic state and may predict the subsequent development of fibrin sheath formation.
CONCLUSIONS
Fibrin sheaths are a common occurrence among HD catheters and are a common cause of catheter malfunction. By contrast, fibrin sheaths encasing PD catheters may be underappreciated and should be considered in the differential diagnosis of patients presenting with PD catheter malfunction. Strategies to reduce fibrin sheath formation and to improve HD catheter function have been explored. The use of heparin locking solutions and thrombolytic therapies have been shown to improve HD catheter function (8). No clinical data have yet shown any benefit of antithrombotic coated HD catheters (9). It has been well demonstrated that the use of heparin decreases fibrin formation in PD patients (10,11). The effect of prophylactic instillation of heparin on fibrin sheath formation shortly after PD catheter insertion has not been explored and may improve primary PD catheter function, but will require further prospective study.
DISCLOSURE
JP has received an unrestricted educational fellowship from Baxter Healthcare Canada and speaking honoraria from Hemisphere, Baxter Healthcare Canada/USA, and Amgen Canada.
REFERENCES
- 1. Diaz–Buxo JA. Management of peritoneal catheter malfunction. Perit Dial Int 1998; 18:256–9 [PubMed] [Google Scholar]
- 2. Yilmazlar T, Kirdak T, Bilgin S, Yavuz M, Yurtkuran M. Laparoscopic findings of peritoneal dialysis catheter malfunction and management outcomes. Perit Dial Int 2006; 26:374–9 [PubMed] [Google Scholar]
- 3. Rosenthal MA, Yang PS, Liu IL, Sim JJ, Kujubu DA, Rasgon SA, et al. Comparison of outcomes of peritoneal dialysis catheters placed by the fluoroscopically guided percutaneous method versus directly visualized surgical method. J Vasc Interv Radiol 2008; 19:1202–7 [DOI] [PubMed] [Google Scholar]
- 4. Kappel JE, Ferguson GM, Kudel RM, Kudel TA, Lawlor BJ, Pylypchuk GB. Stiff wire manipulation of peritoneal dialysis catheters. Adv Perit Dial 1995; 11:202–7 [PubMed] [Google Scholar]
- 5. Diaz–Buxo JA, Turner MW, Nelms M. Fluoroscopic manipulation of Tenckhoff catheters: outcome analysis. Clin Nephrol 1997; 47:384–8 [PubMed] [Google Scholar]
- 6. Simons ME, Pron G, Voros M, Vanderburgh LC, Rao PS, Oreopoulos DG. Fluoroscopically-guided manipulation of malfunctioning peritoneal dialysis catheters. Perit Dial Int 1999; 19:544–9 [PubMed] [Google Scholar]
- 7. Kazory A, Cendan JC, Hollen TL, Ross EA. Primary malfunction of a peritoneal dialysis catheter due to encasement in an encapsulating sheath. Perit Dial Int 2007; 27:707–9 [PubMed] [Google Scholar]
- 8. Besarab A, Pandey R. Catheter management in hemodialysis patients: delivering adequate flow. Clin J Am Soc Nephrol 2011; 6:227–34 [DOI] [PubMed] [Google Scholar]
- 9. Dwyer A. Surface-treated catheters—a review. Semin Dial 2008; 21:542–6 [DOI] [PubMed] [Google Scholar]
- 10. Gries E, Paar D, Graben N, Bock KD. Intraperitoneal fibrinformation and its inhibition in CAPD. Clin Nephrol 1986; 26:209–12 [PubMed] [Google Scholar]
- 11. Tabata T, Shimada H, Emoto M, Morita A, Furumitsu Y, Fujita J, et al. Inhibitory effect of heparin and/or antithrombin III on intraperitoneal fibrin formation in continuous ambulatory peritoneal dialysis. Nephron 1990; 56:391–5 [DOI] [PubMed] [Google Scholar]


