Peritoneal dialysis (PD) as treatment for patients with end-stage renal disease (ESRD) was adopted in India only in the mid 1990s. That timing was a result of initial misgivings about the viability of a home dialysis therapy in a predominantly rural, geographically vast country, with poor connectivity and access to health care, difficult sanitary conditions, and a tropical climate; however, the PD modality has shown impressive growth since then (1–3). By conservative estimate, about 250 of approximately 1000 nephrologists now prescribe PD to more than 6500 patients (4). This growth contrasts with the prevailing declining trend seen in most Western countries, including the United States, which has experienced a drop in the PD utilization rate to 7% in 2010 from 14% in 1995.
Today, a major challenge affecting the acceptance and outcomes of PD is the perceived “inaccessibility” on the part of the patient to the nephrologist and to the “mother unit” (MU)—more so in geographically large countries with remote and inaccessible habitations, as typified by India, the United States, and Canada, among others. Our PD unit has worked to innovate with practical and cost-effective solutions to overcome this barrier (5).
Rapid strides in communications connectivity have been made across the world: Internet and mobile phone technology now truly penetrate almost every geographic and socio-economic boundary extant, especially in India. We are using the mobile phone Short Messaging Service, inexpensive digital cameras, and the World Wide Web to address specific patient accessibility needs. Those technologies—coupled with a dedicated PD team (comprising medical and paramedical staff) and a regular home visit protocol (6)—have enabled us to develop a unique PD remote monitoring system. Patients are constantly in touch with their MU and nephrologist, communicating in real time, around the clock, with improved PD outcomes, especially in rural patients (7).
METHODS
From May 2003, 246 patients who had started on PD at our center and who had used this accessibility technology in their day-to-day care were retrospectively analyzed.
Every patient’s primary “caregiver” or additional skilled family member, or both, are compulsorily trained to use a digital camera, mobile phone camera, and the Internet to send images of PD solution bags, exit sites, and other aspects of interest.
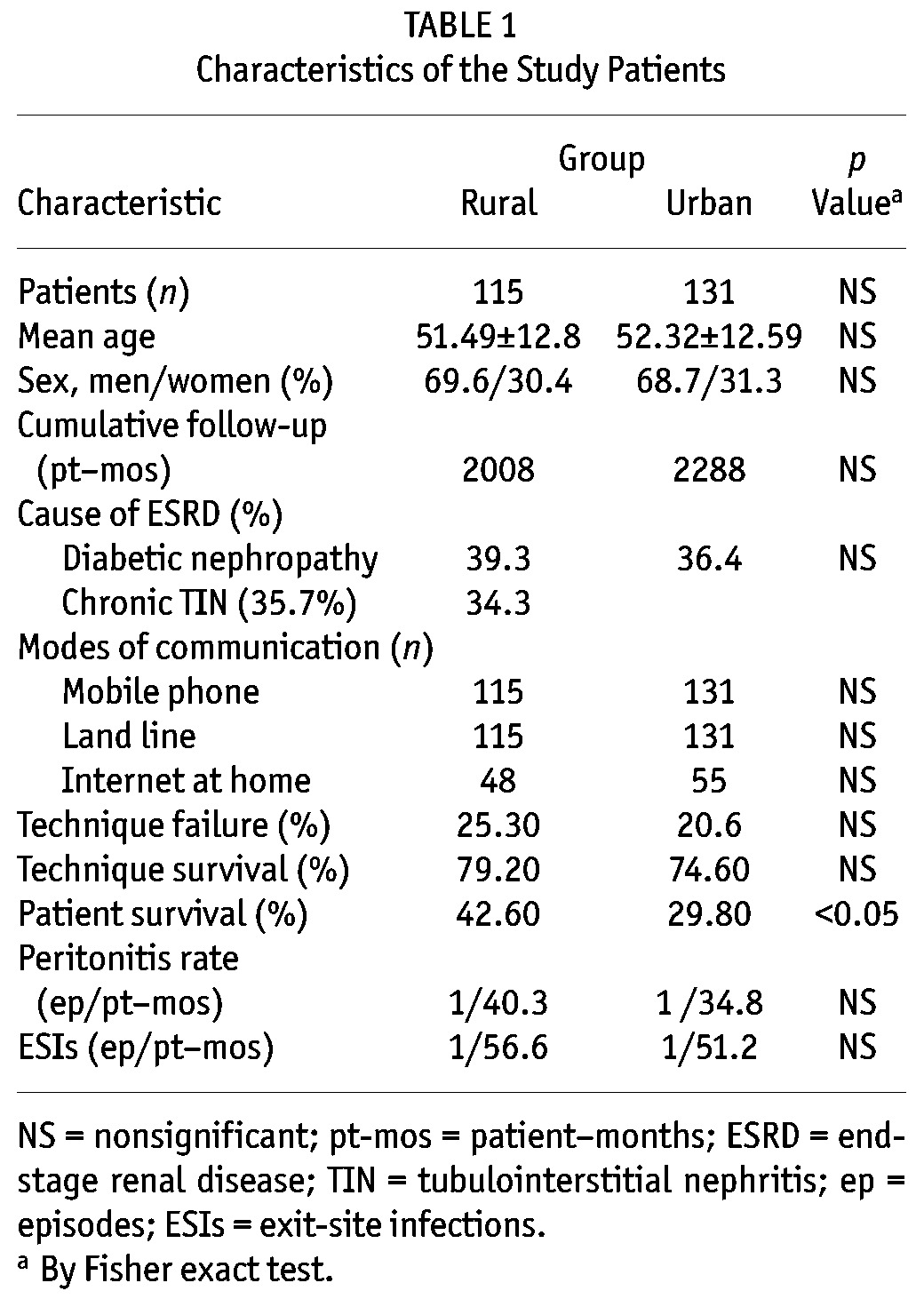
“Urban areas” are defined as places with a municipal corporation, municipal board, or cantonment board, or as regions in a notified town area. All other places that satisfy the criteria of having at least 75% of the male working population engaged in nonagricultural or allied activity, and a population density of at least 400/km2, are also considered urban. Areas that do not fall under those criteria are classified as rural (8). Using those criteria, we grouped patients into “rural” and “urban” categories. Their demographic data; ESRD diagnosis and cumulative follow up; mode of communication with the MU; PD technique survival and failure and patient survival rates (all at 5 years); and peritonitis and exit-site infection rates were analyzed (Table 1) using SPSS software application (version 16: SPSS, Chicago, IL, USA).
TABLE 1.
Characteristics of the Study Patients
The MU comprises these members, organized in a functional hierarchy, each with well-defined responsibilities:
The nephrologist oversees all the PD operations of the MU.
The clinical coordinator (CC), extensively trained in the field of PD, is in charge of about 20 PD patients. Working in shifts around the clock, CCs are the direct link between the MU and the patients at home. They report to the clinical head, who in turn reports to the nephrologist about the PD patients (6,7).
Well-structured home visit protocols ensure patient compliance and rehabilitation, adherence to proper technique, monitoring of nutrition status, and early detection of evolving comorbidities and complications (6,7). Patients and their families are made aware that continuous support is available. Home visits are scheduled by the clinical head and conducted by the CCs. The CCs are trained to follow a set protocol and are equipped with a standardized checklist for a step-by-step assessment of patient well-being during each visit. A detailed check of the patient’s PD logbook is made, and any conditions requiring the attention of the nephrologist are identified. All this information, together with a brief summary of the patient’s most current laboratory results, are conveyed to the nephrologist by Short Messaging Service from the patient’s home (Figure 1). The CC is instructed to wait till a response is received from the nephrologist (usually within 15 minutes) and then to counsel the patient accordingly. The CCs also assess and advise patients on nutrition, psychosocial well-being, and physical fitness and rehabilitation levels. Afterward, progress notes are entered into the MU computer records.
Figure 1.
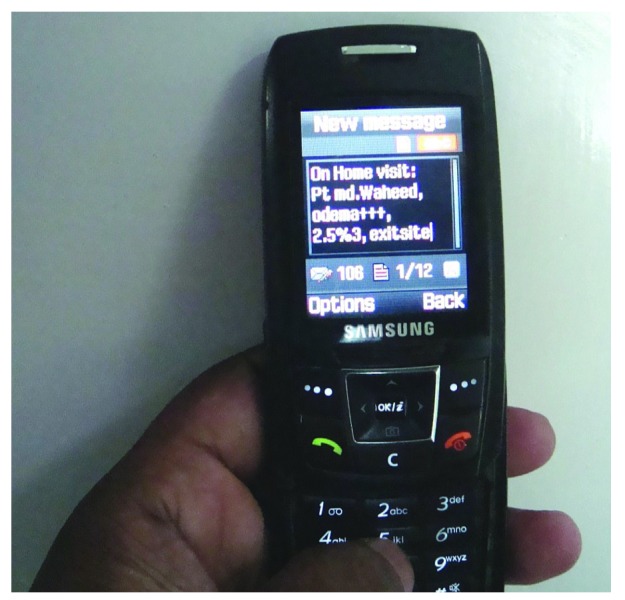
— Details for the patient on peritoneal dialysis, sent through the Short Messaging Service to the Mother Unit for response and follow-up.
The Internet-based remote monitoring system was created in our PD unit by our team to serve as a means of real-time interaction between patients and primary health care providers. It aims at integrating all services necessary for PD, making them easily accessible to the patients and the primary caregivers regardless of geographic distance from the MU. Those services include access to the nephrologist, clinical head, CC, urologist, and if needed, microbiologist, nutritionist, and so on. Each enrolled caregiver has a dedicated user name and password, through which they use the site for one-on-one communication with patients and with each other. Privacy of information and patient records is ensured, the software being compliant with HIPAA (the Health Insurance Portability and Accountability Act). Access to the technology is through the computer or the mobile phone using an Android- or iPhone-based application. After signing into the website with a user name and password assigned at the end of the PD initiation period, the patients and caregivers are directed to a personalized home page from which they can navigate the site to
enter personal details, health records, and lab test results.
maintain an online log of body weight, blood pressure, heart rate, and biochemical parameters.
access current health records and prescription and procedure history at any time.
schedule appointments with the MU, nephrologist, and laboratory.
schedule home visits through the clinical head.
raise concerns and health complaints.
upload relevant photographs of the exit site, PD effluent bag, and ankle edema (after indenting over the medial malleolus) to the site.
be alerted to appointments, test results, and replies from the nephrologist and the clinical head.
Health complaints made by patients using the site receive immediate responses. They are directed to a page where they are instructed to complete a basic description of their current concerns and answer certain pertinent questions. Patients are taught to check the condition of the exit site in terms of color, dryness, presence or absence of pain, swelling, leakage, and visibility of the external cuff, and to enter relevant information. The two main infectious complications encountered being peritonitis and exit-site infections, patients and their caregivers or attendants are trained during their initial PD period to use their own mobile phone cameras or digital cameras to take relevant photographs of the PD effluent bag and exit site for uploading from their personal home computer or from a computer at the nearest Internet café along with their health complaint. Most standard phones and computers are compatible to use this technology.
Exit-Site Evaluation: Owing to darker colored skin and a tendency to keloid formation, inflammation and crusting associated with exit-site infections assume a very different appearance in Indian patients than in Caucasian patients (7). Our center is developing its own “Ready Reckoner” flip-chart of compiled images of various exit sites, normal and infected, together with a baseline view of the patient’s unique exit site stored in that individual’s image gallery, to aid in arriving at an accurate grading of exit-site infection. A zoom application incorporated into the software helps in examining the exit site in greater detail. We have found this approach to be more useful than that using the standardized flip-chart as a comparator.
Peritonitis Evaluation: Training given at the MU during the break-in period teaches patients to photograph PD effluent bags placed on a white sheet of paper printed with black Times Roman type. This image of the effluent bag is visualized, recorded, and uploaded as a baseline image for future follow up. Generally, a 14- to 16-point typeface seen clearly through the effluent bag indicates clarity and no peritonitis. Complaints about potential peritonitis are sent to the nephrologist and CC, who receive an alert both by e-mail and by cell phone. An immediate assessment and response is sent to the patient, and to the clinical head or CC, who schedules a home visit to follow up. A horizontal and vertical image gallery of the exit site and PD bag is created and stored in each patient’s electronic medical record (EMR). With every health complaint, this gallery is updated, thus providing comprehensive and current information about the patient’s clinical status (Figures 2 and 3).
Figure 2.
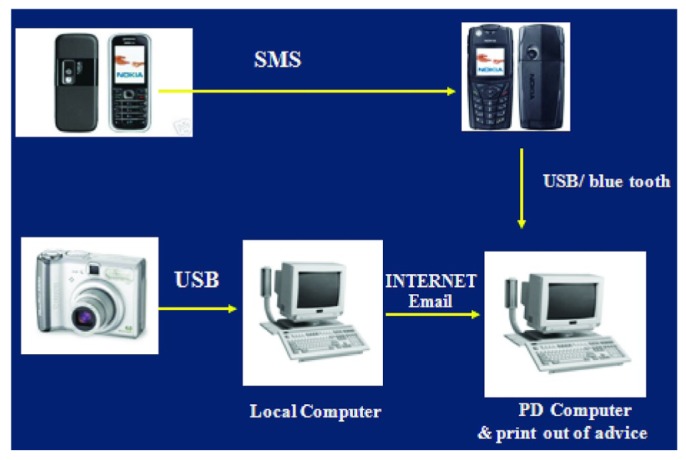
— Process overview of the peritoneal dialysis remote monitoring system. SMS = Short Messaging Service; USB = universal serial bus connection technology; PD = peritoneal dialysis.
Figure 3.
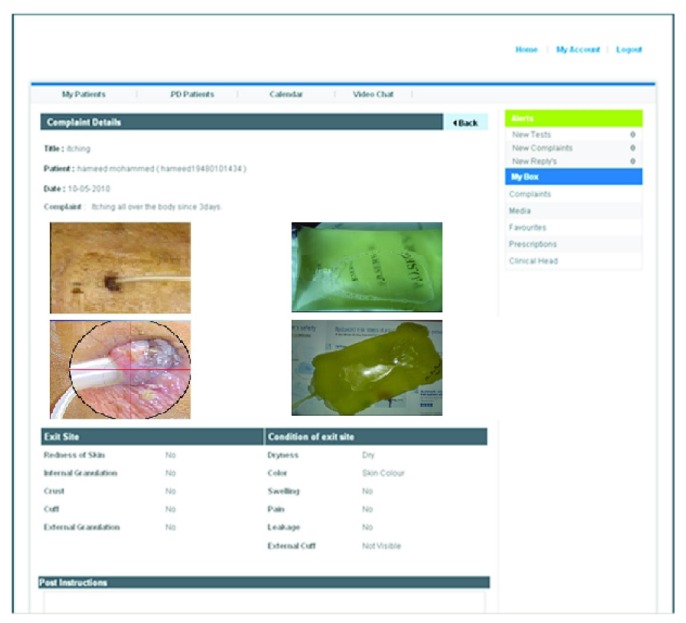
— The interface shows patient details and peritoneal dialysis images in horizontal and vertical orientation, with zoom available for closer inspection and a print background for effluent clarity determination.
RESULTS
The patient cohort who used the remote monitoring system on a day-to-day basis included 115 rural and 131 urban patients. Mean follow-up was 4296 patient–months (2008 in the rural group, 2288 in the urban group). Mean age was 51.49 ± 12.8 years in the rural group and 52.32 ± 12.59 years in the urban group. The most common cause of ESRD was diabetic nephropathy in both groups (39.3% in the rural group, 36.4% in the urban group). Chronic tubulointerstitial nephritis was the second most common diagnosis in both groups (35.7% in the rural group, 34.3% in the urban group). Technique failure rates were 25.3% and 20.6% in the rural and urban groups respectively (p > 0.05), and peritonitis rates were 1 episode in 40.3 patient–months (rural) and 1 episode in 34.8 patient–months (urban, p > 0.05). Exit-site infections occurred at a rate of 1 episode in 56.6 patient–months (rural) and 1 episode in 51.2 patient–months (urban, p > 0.05). Patient survival at 5 years was significantly better in rural patients (42.6% vs 29.8% in the urban group, p < 0.05, Table 1). Overall, rural patients performed well on PD and had significantly better survival rates than did their urban counterparts, contrary to what might have been expected. Our monitoring strategies allow for earlier diagnosis of infectious PD complications, thus promoting prompt treatment initiation and response. Most of our rural patients visit the unit once in 3 – 6 months on an “as needed” basis.
DISCUSSION
Studies comparing outcomes of chronic kidney disease patients have consistently shown poorer results in rural than in urban patients (9,10), although there is paucity of data comparing those two groups on PD. Our center used remote monitoring strategies to target the major bottlenecks affecting penetrance and technique survival rates in rural patients: lack of connectivity and health awareness. That our rural patients achieved results as good as those of the urban patients (if not better) on PD therapy is testimony to the utility of the remote monitoring system.
The application of telemedicine in the monitoring of PD patients in Japan was published by Nakamoto (11). The most recent system described uses a D converter to monitor patient blood pressure, heart rate, body weight, blood glucose, and exercise levels (11). Patients use the unit website to check their data. That application addresses mainly the issues of remote monitoring of vital signs and patient compliance. Our system aims primarily to achieve early diagnosis and management of common infectious complications of PD (which has a far greater effect on PD technique survival), with integration of relevant health services and promotion of supervised autonomy.
Gallar et al. published a 2-year experience with telemedicine in the follow-up of patients on home PD in 2007 (12). Their study focused mainly on video conferencing and teleconsultation as a means of communication, clearly demonstrating the clinical advantages of communications technology in the follow-up of that patient population. Mean hospitalization rates were significantly lower in the telemedicine group. Our model, primarily designed for application in geographically vast countries such as India, the United States, Canada, Australia, and China, has shown promising preliminary results. Given the changing scenario, especially in the United States, we believe that, with a strong commercial incentive, health care providers will have to “reach out” to PD patients, increasing the interaction between patients and the MU in a bid to remove the perception of inaccessibility that the PD patients may have. We believe that our PD remote monitoring tool may be a ground-breaking driving force for promoting PD as the preferred dialysis modality.
DISCLOSURES
The authors declare that no financial conflict of interest exists.
REFERENCES
- 1. Abraham G, Bhaskaran S, Soundarajan P, Ravi R, Nitya S, Padma G, et al. Continuous ambulatory peritoneal dialysis. J Assoc Physicians India 1996; 44:599–601 [PubMed] [Google Scholar]
- 2. Nayak KS. Asia, a melting pot for peritoneal dialysis practices: redefining and expanding peritoneal dialysis horizons in Asia. Perit Dial Int 2004; 24:422–3 [PubMed] [Google Scholar]
- 3. Nayak KS, Prabhu MV, Sinoj KA, Subhramanyam SV, Sridhar G. Peritoneal dialysis in developing countries. Contrib Nephrol 2009; 163:270–7 [DOI] [PubMed] [Google Scholar]
- 4. Abraham G, Pratap B, Sankarasubbaiyan S, Govindan P, Nayak KS, Sheriff R, et al. Chronic peritoneal dialysis in south Asia: challenges and future. Perit Dial Int 2008; 28:13–19 [PubMed] [Google Scholar]
- 5. Aditi NK, Sinoj AK, Prabhu MV. Improving peritoneal dialysis (PD) outcomes in rural patients compared to urban by employing novel and practical initiatives [Abstract]. Perit Dial Int 2010; 30(Suppl 2):S65 [Google Scholar]
- 6. Nayak KS, Sinoj KA, Subhramanyam SV, Mary B, Rao NV. Our experience of home visits in city and rural areas. Perit Dial Int 2007; 27(Suppl 2):S27–31 [PubMed] [Google Scholar]
- 7. Nayak KS. Key success factors for a quality peritoneal dialysis program. Perit Dial Int 2007; 27(Suppl 2):S9–15 [PubMed] [Google Scholar]
- 8. Dreze J, Murthi M. Fertility, education, and development: evidence from India. Popul Dev Rev 2001; 27:33–63 [Google Scholar]
- 9. Zhang W, Gong Z, Peng X, Tang S, Bi M, Huang W. Clinical characteristics and outcomes of rural patients with ESRD in Guangxi, China: one dialysis center experience. Int Urol Nephrol 2010; 42:195–204 [DOI] [PubMed] [Google Scholar]
- 10. Tonelli M, Hemmelgarn B, Culleton B, Klarenbach S, Gill JS, Wiebe N, et al. Mortality of Canadians treated by peritoneal dialysis in remote locations. Kidney Int 2007; 72:1023–8 [DOI] [PubMed] [Google Scholar]
- 11. Nakamoto H. Telemedicine system for patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2007; 27(Suppl 2):S21–6 [PubMed] [Google Scholar]
- 12. Gallar P, Vigil A, Rodriguez I, Ortega O, Gutierrez M, Hurtado J, et al. Two-year experience with telemedicine in the follow-up of patients in home peritoneal dialysis. J Telemed Telecare 2007; 13:288–92 [DOI] [PubMed] [Google Scholar]


