Abstract
♦ Background: We sought to compare perioperative outcomes and 2-year survival in a cohort of peritoneal dialysis (PD) patients compared with matched hemodialysis (HD) patients who underwent cardiothoracic surgery at our institution.
♦ Methods: We obtained a list of all dialysis-dependent patients who underwent cardiac surgery (coronary artery bypass grafting, valve replacement, or both) at our center between 1994 and 2008. All patients undergoing PD at the time of surgery were included in our analysis. Two HD patients matched for age, diabetes status, and Charleston comorbidity score were obtained for each PD patient.
♦ Results: The analysis included 36 PD patients and 72 HD patients. Mean age, sex, diabetes status, cardiac unit stay, hospital stay, and operative mortality did not differ by dialysis modality. The incidence of 1 or more postoperative complications (infection, prolonged intubation, death) was higher for HD patients (50% vs. 28% for PD patients, p = 0.046). After surgery, 2 PD patients required conversion to HD. The 2-year survival was 69% for PD patients and 66% for HD patients (p = 0.73).
♦ Conclusions: Our findings suggest that, compared with HD patients, PD patients who require cardiac surgery do not experience more early complications or a lesser 2-year survival and that 2-year survival for dialysis patients after cardiac surgery is acceptable.
Keywords: Hemodialysis, cardiac surgery, coronary artery bypass grafting, survival
The number of end-stage renal disease (ESRD) patients undergoing cardiothoracic surgery (CTS) has increased in recent years, but there are biases and concerns pertaining to the outcomes, during the immediate postsurgical period, of patients treated with peritoneal dialysis (PD). It is not uncommon for surgeons to request that PD patients be transferred to hemodialysis (HD) in the immediate postsurgical period because of a belief that PD will fail to provide adequate ultrafiltration and that intubation time may be prolonged. Another potential concern is that the surgical incision may extend down to the peritoneal cavity, leading to the possibility of infection and dialysate leaks.
In patients undergoing CTS, those with ESRD have been shown to have higher postoperative morbidity and mortality (1,2); however, outcomes demonstrate that cardiac surgery can be performed with acceptable short- and long-term results in that population (3,4). Estimates of perioperative mortality (in-hospital or 30-day mortality) in ESRD patients undergoing CTS have been reported to range between 7% and 18%, depending on the study (1,4–7). Length of hospital stay does not appear to be excessively prolonged in ESRD patients (8). A recent study showed that early postoperative recovery after elective coronary artery bypass grafting (CABG) was delayed by only 1 day in dialysis patients, and that delay was thought to be a result of the HD treatment that usually occurred on postoperative day 1 (9).
Most studies of outcomes in ESRD patients undergoing CTS have been retrospective and have included primarily HD patients. Few studies have focused specifically on postsurgical outcomes in PD patients. We therefore sought to examine perioperative outcomes and 2-year survival in a cohort of PD patients compared with matched HD patients who underwent CTS at our institution over a 15-year period.
METHODS
STUDY PATIENTS
We obtained a list of all ESRD patients who received CTS at Southern California Permanente Medical Group, Los Angeles Medical Center, between 1 January 1994 and 31 December 2008. Southern California Permanente Medical Group is a large health care maintenance organization providing care to approximately 3.5 million members in southern California. The cardiac surgery unit at Los Angeles Medical Center serves as a tertiary care center to nearly all of those members. Our study enrolled ESRD patients who underwent CABG, valve replacement, or combined CABG and valve replacement. All PD patients who underwent CTS during the study period were included in the analysis. From the pool of HD patients who underwent cardiac surgery during the study period, 2 HD controls were obtained for each PD case. The controls were matched based on age (up to ±5 years), diabetes status, and score on the modified Charlson comorbidity index (±2 points) (10).
DATA AND OUTCOMES RECORDED
For patients who underwent cardiac surgery before 2008, data were obtained primarily from paper charts. For patients who underwent surgery after 2008 and to verify follow-up data (including date of death), electronic medical records were used (our institution transitioned to electronic medical records in 2007). We also examined the admitting history and physicals and the discharge summaries in the electronic medical records to determine whether PD patients had been prescribed a diuretic during their hospital stay. We noted patient age, sex, dialysis vintage, surgery type, and dialysis modality at the time of surgery (predictor variables) and also whether surgery was elective or not. Vintage was defined as the number of days between the date of dialysis start and the date of surgery, divided by 30 to yield months.
Surgeries that were routinely scheduled were deemed elective; non-elective surgeries were those performed as soon as possible after the decision to operate was made. The primary outcome studied was operative mortality, which was defined as death within 30 days of surgery or during the same hospital stay. Secondary outcomes included length of stay (LOS) on the cardiac surgical unit, hospital LOS, median intubation time (recorded in hours, generally as a multiple of 24), incidence and type of postoperative infection, and need for conversion to HD or to continuous renal replacement therapy.
DIALYSIS PRESCRIPTION
Most PD patients in our study received automated PD (APD) after cardiac surgery, because after early 1999, the hospital used only APD. We estimate that approximately 10% of the PD study patients received manual exchanges (before 1999). The patients who performed APD at home were generally continued on their existing dialysis prescription; those who performed manual exchanges at home were converted to APD during their hospital stay. Dialysate dextrose concentration varied according to the patient’s volume status. Icodextrin was generally continued for the longest dwell if the patient had been using it before hospitalization.
Although no data were collected regarding the timing of dialysis resumption after surgery, institution policy regarding provision of dialysis was this: To prevent fluid or electrolyte problems (or both), HD patients received dialysis the night before or the morning of surgery. If the cardiac team requested dialysis for a HD patient in the immediate postoperative period, then the nephrology team assessed the patient and provided HD if indicated. The PD patients received dialysis (usually APD) the night before surgery. Most PD patients were taken to surgery with a “dry” abdomen. Peritoneal dialysis was generally resumed the afternoon or the night after surgery.
PATIENT SURVIVAL
Patient survival was determined by calculating the difference between the date of surgery and either the date of death or of the end of follow-up (1 September 2010), dividing by 30 to yield months. Living patients were censored from the total surviving patients at the end of follow-up (denominator) if their postsurgical survival was less than 24 months at that time. The study was approved by our institutional review board.
STATISTICS
The Student t-test was used to compare normally distributed continuous variables (reported as mean ± standard deviation). The Wilcoxon rank sum test was used to compare non–normally distributed continuous variables [reported as median and interquartile range (IQR)]. The Yates chi-square, corrected for continuity, was used to compare categorical variables, and the Fisher exact test was used when cell entries were small (<5). A Kaplan–Meier survival analysis was used to compare 2-year survival between the dialysis modalities. The log-rank test was used to compare the significance of the difference in the 2-year survival curves between the dialysis modalities.
RESULTS
During the study period, 204 dialysis patients underwent cardiac surgery (36 PD patients, 168 HD patients).
The mean age in the HD cohort was 61.1 ± 9.7 years and the mean Charlson comorbidity score was 7.1 ± 2.3. In the HD cohort, 65% of the patients were men, and 75% had a diagnosis of diabetes mellitus at the time of surgery. Median intubation time for HD patients was 24 hours (IQR: 24 – 48 hours), median cardiac surgical unit LOS was 4 days (IQR: 2 – 6 days), and median hospital LOS was 10 days (IQR: 7 – 15.25 days). During their hospital stay, 40 HD patients (23%) experienced an infection, and 15 patients died (9%).
All 36 PD patients and 72 matched HD patients were included in the final analysis. Table 1 shows the baseline patient demographics for all analyzed patients (n = 108). Most of these patients underwent non-elective surgery (56%), and most underwent CABG (69%).
TABLE 1.
Baseline Patient Demographics
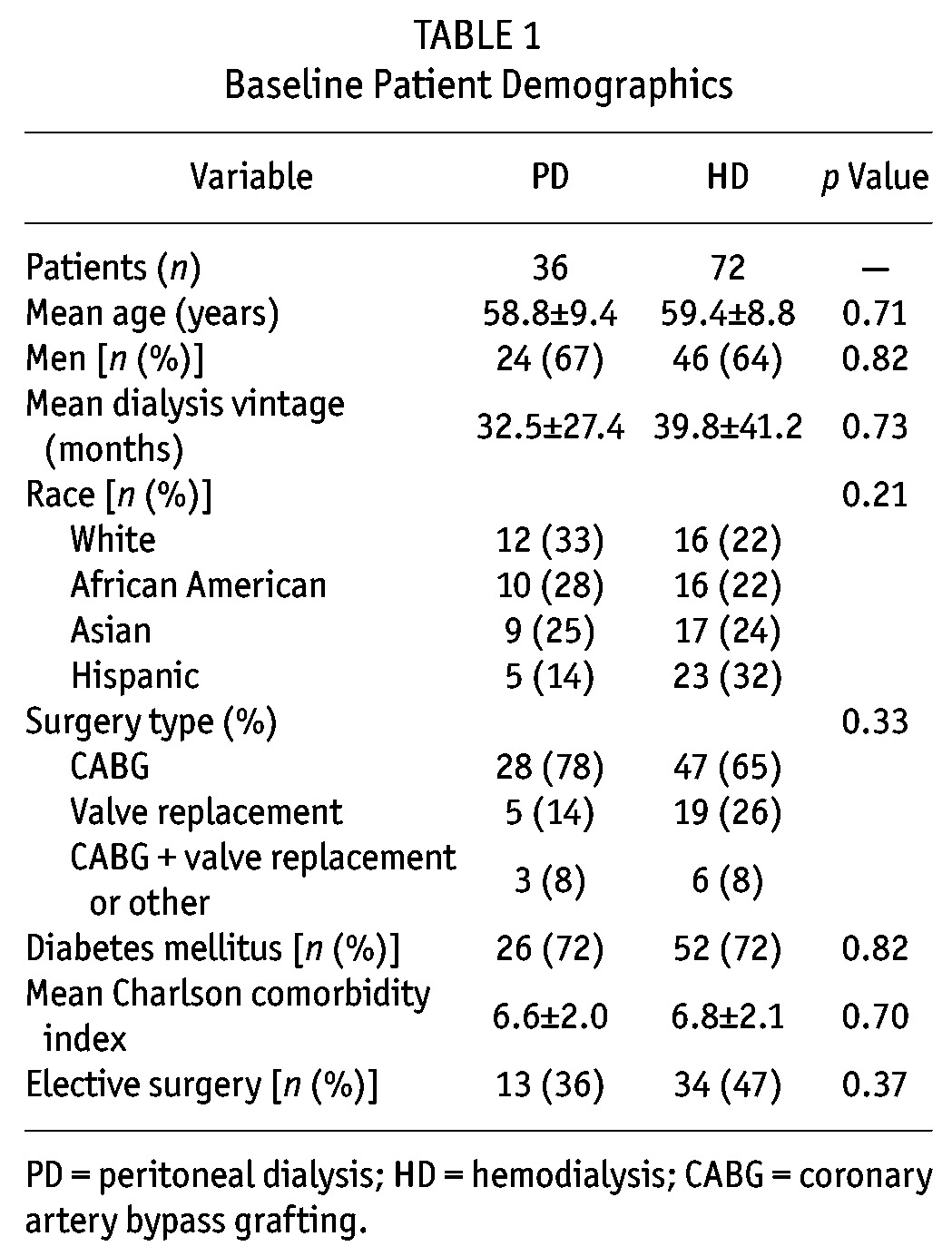
Table 2 compares early postoperative complications by dialysis modality. The incidence of postoperative infection was 19% for HD patients and 6% for PD patients, p = 0.08. Compared with patients who underwent non-elective surgery, those who underwent elective surgery experienced fewer postoperative infections (4% vs 23%, p = 0.011). The incidence of any postoperative complication (including prolonged intubation time, postoperative infection, or death) was higher for HD patients (50%) than for PD patients (28%), p = 0.046.
TABLE 2.
Early Postoperative Outcomes by Dialysis Modality
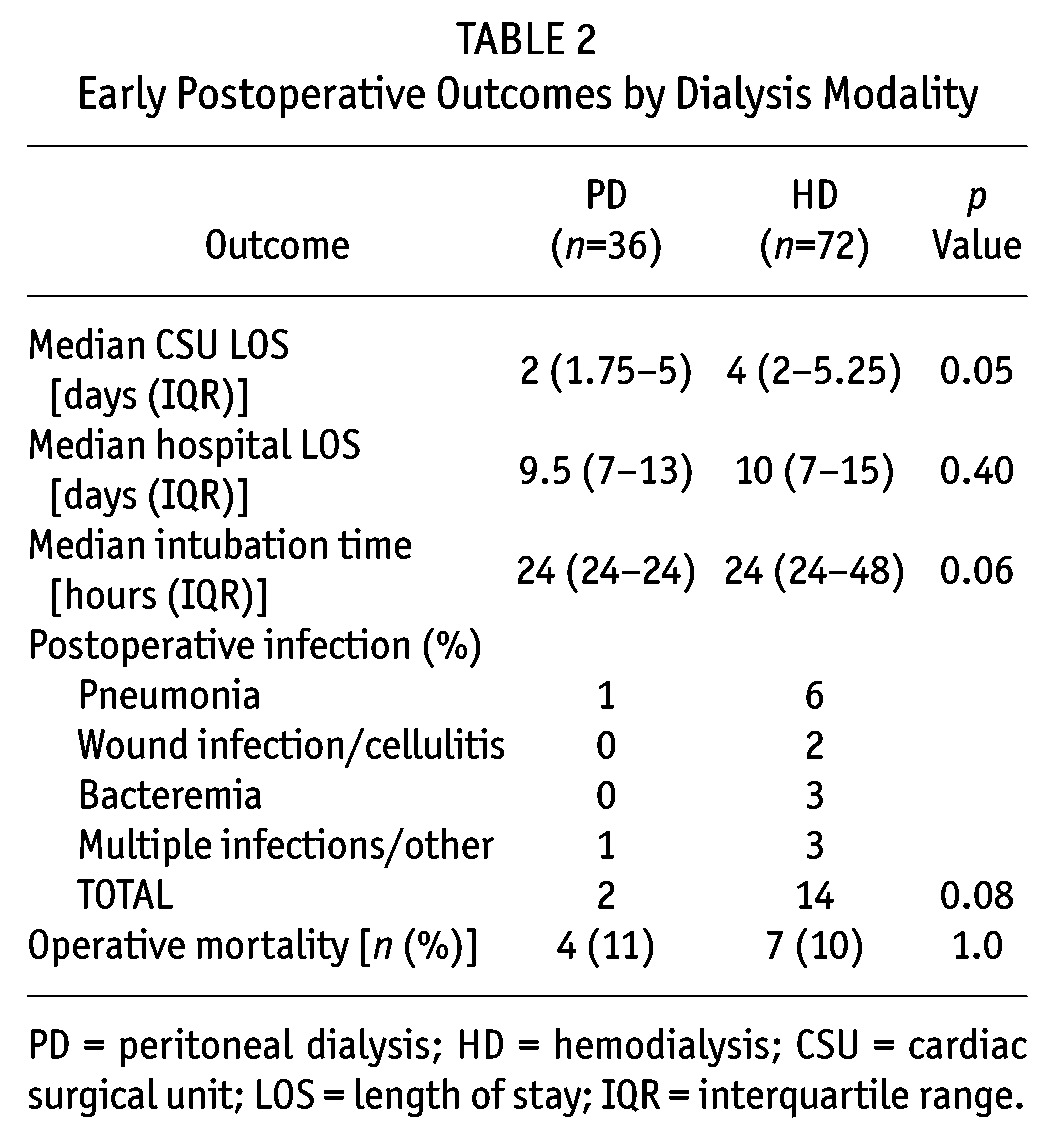
Conversion to HD after cardiac surgery was required in 2 PD patients (6%): 1 for dialysate leakage, and 1 for uncontrolled azotemia. Otherwise, HD was not performed at any point during admission for the other PD patients. Just 1 HD patient required conversion to continuous renal replacement therapy after cardiac surgery because of hemodynamic instability. During their hospital stay, 6 PD patients (17%) received a diuretic.
Operative mortality was 10% for all patients studied, and the rates for patients undergoing elective and non-elective surgery were similar (3% vs 7% respectively, p = 0.34). The mean age of the patients who experienced operative mortality was 58.4 ± 8.5, their mean Charlson comorbidity score was 6.3 ± 2.4, and 55% were men.
The HD patients were followed for a median of 30.6 months (IQR: 16.6 – 44.8 months); PD patients were followed for a median of 34.8 months (IQR: 20.8 – 57.6 months). The 1-year survival was 81% for PD patients and 78% for HD patients (p = 0.92), and the 2-year survival was 69% for PD patients and 66% for HD patients (p = 0.73). Figure 1 illustrates the 2-year survival percentages.
Figure 1.
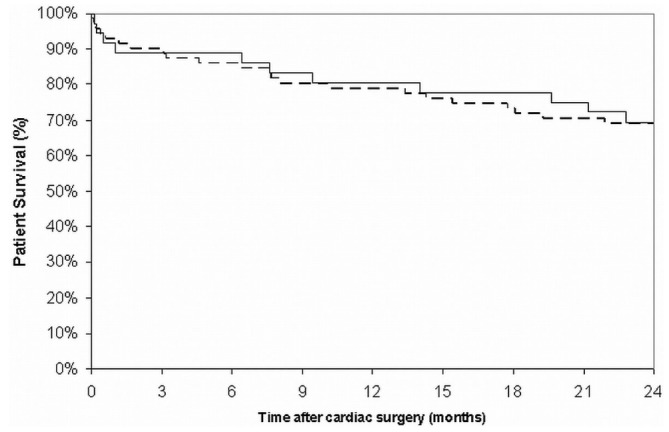
— Two-year patient survival after cardiac surgery for peritoneal dialysis patients (solid line) and hemodialysis patients (dashed line).
DISCUSSION AND CONCLUSIONS
Cardiovascular disease is frequently associated with chronic kidney disease, and it remains the single most common cause of death in dialysis patients (11). Coronary artery bypass grafting procedures have been shown to be effective in the management of symptomatic ischemic heart disease and to improve life expectancy in patients with left main or multivessel disease (12), although not specifically in dialysis patients. But when compared with percutaneous coronary interventions, CABG may be associated with better long-term survival in dialysis patients, especially those with diabetes (13).
Before the 1990s, very few HD patients (and even fewer PD patients) underwent cardiac surgery, but surgeons now appear to be more willing to operate on dialysis patients. Event rates for coronary revascularization procedures (including bypass surgery) in ESRD patients doubled between 1993 and 2003 in patients between the ages of 45 and 74 years (11). More recently, event rates for bypass surgeries have fallen by approximately 15% in the same age group, suggesting a new reluctance to operate on dialysis patients.
In our study patients, 2-year survival was comparable to the 2-year survival (all-cause mortality) reported for all ESRD patients in the US Renal Data System’s 2009 annual report. Despite the obvious surgical risks and early postoperative mortality, our patients experienced a 2-year survival rate of nearly 70%. Operative mortality in our study was 10%, similar to the 11% reported by Chertow et al. (14), but lower than the 18% reported by Kogan et al. (1). Our lower operative mortality rate probably reflects the hospital and surgeon volumes at our institution, because patients are funneled from a large geographic area to our center.
Our findings contrast with some commonly held beliefs regarding CTS in PD patients. We found a lower incidence of early postoperative complications in our PD population. No episodes of bacteremia, cellulitis, or wound infection occurred in the PD patients, although the overall difference in postoperative infections by modality did not achieve statistical significance. One possible explanation of our findings is that PD patients tend to differ from HD patients in subtle ways, especially in terms of motivation, education, and compliance with treatment. Compared with patients initiating HD, patients initiating PD in the United States tend to be healthier at the start of dialysis, possibly because of patient selection or better pre-dialysis care (15). Our patients appeared well-matched in terms of the major predictors of survival in PD patients (including age, diabetes status, race, and comorbidity scores). Comparisons of outcomes based on dialysis modality remain difficult, however, because the risk of death varies with time on dialysis and the presence of various comorbid conditions and risk factors (16).
For postsurgical patients, PD does afford some potential advantages over HD. It avoids the fluctuations in blood pressure seen with HD, thereby limiting cardiac stress. Other potential drawbacks of HD after cardiac surgery are the need for anticoagulation with treatment and the potential for endocarditis (especially after valve replacement surgery).
Our study demonstrates that, compared with HD patients, PD patients who require cardiac surgery do not experience higher rates of early postoperative complications, including operative mortality. The PD patients do not appear to be at increased risk for postoperative infections despite the presence of an indwelling catheter in proximity to a fresh surgical wound. Intubation time and cardiac surgical unit LOS were not prolonged in our PD patients, suggesting that extracellular volume was well controlled in the PD subgroup. The 2-year survival rate in our PD patients was similar to that in matched HD controls. Despite the presence of significant cardiovascular disease, the 2-year survival for our dialysis patients who underwent CTS was comparable to the 2-year survival reported by the US Renal Data System. Our data suggest the need for larger-scale studies to evaluate clinical outcomes after CTS in dialysis patients.
DISCLOSURES
None of the authors has any conflict of interest associated with the contents or publication of this manuscript. The first author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgments
The authors thank Susana M. Mendoza, md, for her valuable contribution to this manuscript.
REFERENCES
- 1. Kogan A, Medalion B, Kornowski R, Raanani E, Sharoni E, Stamler A, et al. Cardiac surgery in patients on chronic hemodialysis: short and long-term survival. Thorac Cardiovasc Surg 2008; 56:123–7 [DOI] [PubMed] [Google Scholar]
- 2. Zimmet AD, Almeida A, Goldstein J, Shardey GC, Pick AW, Lowe CE, et al. The outcome of cardiac surgery in dialysis-dependent patients. Heart Lung Circ 2005; 14:187–90 [DOI] [PubMed] [Google Scholar]
- 3. Suehiro S, Shibata T, Sasaki Y, Murakami T, Hosono M, Fujii H, et al. Cardiac surgery in patients with dialysis-dependent renal disease. Ann Thorac Cardiovasc Surg 1999; 5:376–81 [PubMed] [Google Scholar]
- 4. Gelsomino S, Morocutti G, Masullo G, Cheli G, Poldini F, Da Broi U, et al. Open heart surgery in patients with dialysis-dependent renal insufficiency. J Card Surg 2001; 16:400–7 [DOI] [PubMed] [Google Scholar]
- 5. Zhong H, David T, Zhang AH, Fang W, Ahmad M, Bargman JM, et al. Coronary artery bypass grafting in patients on maintenance dialysis: is peritoneal dialysis a risk factor of operative mortality? Int Urol Nephrol 2009; 41:653–62 [DOI] [PubMed] [Google Scholar]
- 6. Rahmanian PB, Adams DH, Castillo JG, Vassalotti J, Filsoufi F. Early and late outcome of cardiac surgery in dialysis-dependent patients: single-center experience with 245 consecutive patients. J Thorac Cardiovasc Surg 2008; 135:915–22 [DOI] [PubMed] [Google Scholar]
- 7. Horst M, Mehlhorn U, Hoerstrup SP, Suedkamp M, de Vivie ER. Cardiac surgery in patients with end-stage renal disease: 10-year experience. Ann Thorac Surg 2000; 6:96–101 [DOI] [PubMed] [Google Scholar]
- 8. Strijack B, Mojica J, Sood M, Komenda P, Bueti J, Reslerova M, et al. Outcomes of chronic dialysis patients admitted to the intensive care unit. J Am Soc Nephrol 2009; 20:2441–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kobayashi J, Ikebuchi M, Fujita Y, Irie H. Early postoperative recovery by chronic dialysis patients after coronary artery bypass grafting. Ann Thorac Cardiovasc Surg 2009; 15:243–6 [PubMed] [Google Scholar]
- 10. Hemmelgarn BR, Manns BJ, Quan H, Ghali WA. Adapting the Charlson comorbidity index for use in patients with ESRD. Am J Kidney Dis 2003; 42:125–32 [DOI] [PubMed] [Google Scholar]
- 11. United States Renal Data System (USRDS). Annual Data Report, 2009. Bethesda, MD: USRDS; 2009. [Available online at: http://www.usrds.org/adr_2009.htm; accessed 23 July 2010] [Google Scholar]
- 12. Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United States after coronary angioplasty, coronary artery stenting, and coronary artery bypass surgery and impact of diabetes. Circulation 2002; 106:2207–11 [DOI] [PubMed] [Google Scholar]
- 13. Coronary artery surgery study (CASS): a randomized trial of coronary artery bypass surgery. Quality of life in patients randomly assigned to treatment groups. Circulation 1983; 68:951–60 [DOI] [PubMed] [Google Scholar]
- 14. Chertow GM, Johansen KL, Lew N, Lazarus JM, Lowrie EG. Vintage, nutritional status, and survival in hemodialysis patients. Kidney Int 2000; 57:1176–81 [DOI] [PubMed] [Google Scholar]
- 15. Xue JL, Chen SC, Ebben JP, Constantini EG, Everson SE, Frazier ET, et al. Peritoneal and hemodialysis: I. Differences in patient characteristics at initiation. Kidney Int 2002; 61:734–40 [DOI] [PubMed] [Google Scholar]
- 16. Vonesh EF, Snyder JJ, Foley RN, Collins AJ. The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int 2004; 66:2389–401 [DOI] [PubMed] [Google Scholar]


