Acute kidney injury (AKI) is a common problem associated with increased mortality and health care costs. Renal replacement therapy (RRT) is often necessary to maintain patients. Continuous RRT and intermittent hemodialysis (HD) are the modalities most commonly used in developed countries (1). Worldwide, peritoneal dialysis (PD) is an underutilized modality for AKI, but PD is frequently used in developing countries because of its lower cost and minimal infrastructure requirements (2–4); PD is also more frequently used in pediatric patients (5). Recently, interest in using PD to manage patients with AKI has been increasing. It has been postulated that PD may be more physiologic and less inflammatory than HD in AKI because of the absence of contact between blood and synthetic membranes (6), and that PD may better preserve local renal hemodynamics. Those factors could theoretically contribute to better outcomes: improved survival and renal recovery, for example. A recent randomized study showed a shorter duration of dialysis dependence among AKI patients treated with PD (7), stimulating renewed interest in PD for AKI.
We conducted a pilot study whose objective was to survey the opinions and practice patterns of an international group of physicians and other health professionals regarding PD in AKI.
METHODS
An anonymous self-administered questionnaire was distributed to attendees at three dialysis meetings held in 2009. The questionnaires were distributed to all attendees at the 18th International Vicenza Course on PD (Vicenza, Italy, June 2009) and to convenience samples of attendees at the North American Chapter meeting of the International Society for Peritoneal Dialysis [ISPD (Vancouver, Canada, August 2009)] and the Second Congress of the International Society for Hemodialysis [ISHD (Hong Kong SAR, PR China, August 2009)]. At the ISPD and ISHD meetings, the questionnaires were made available at the main registration desk and were completed at the discretion of the attendees.
Binary (yes/no) and multiple-choice questions addressed actual practice and opinions regarding the use of PD for AKI in the intensive care unit (ICU) and the wards, PD modality and dose, and demographics of the respondents. Completed questionnaires were reviewed by three of the investigators (DNC, FOF, MdC) for accuracy and consistency before encoding began. Data were then encoded and analyzed using a commercially available software application, the Statistical Package for Social Sciences (SPSS, version 14: SPSS, Chicago, IL, USA). Aggregated data are summarized using descriptive statistics and are presented as numbers or percentages of respondents as appropriate.
RESULTS
Of the 464 correctly completed questionnaires included in the analysis, 378 (81.5%) were from the Vicenza PD course [378 of 387 attendees (97.7% response rate)], 47 (10.1%) were from the ISHD Hong Kong congress, and 39 (8.4%) were from the ISPD Vancouver meeting. A response rate could not be calculated for the latter two meetings because of the nature of the responses as convenience samples. Among respondents, more than 80% were physicians (n = 381), of whom 92.1% were nephrologists. Other specialties included general practice, general internal medicine, intensive care, and general pediatrics. Overall, 39 countries were represented: most respondents were from Europe (74%), followed by Asia–Pacific/Australasia (14%), and North America (11%).
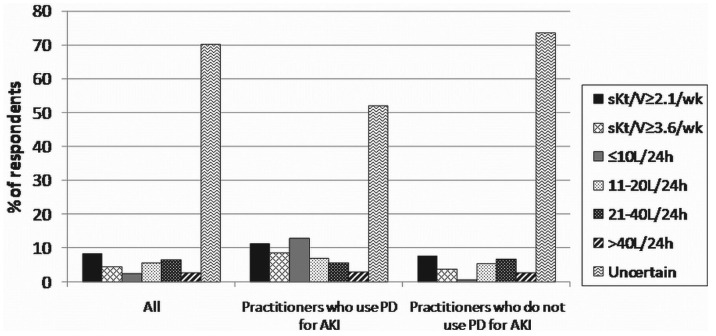
PD for AKI in the ICU: In response to the question “What is your opinion of PD for the management of AKI in the ICU,” 36.1% of all respondents considered PD to be a suitable therapeutic option in most cases of AKI. By contrast, only 15.7% actually used PD in the ICU (Figure 1). This discrepancy between opinion and actual practice was seen among physicians and non-physicians alike, but it varied by geographic area. Among respondents from Asia, there appeared to be concordance between opinion and practice, with 35% of practitioners using PD to treat AKI in the ICU. On the other hand, PD was used much less frequently in Europe (13.2%) and North America (8.2%), despite nearly 40% of practitioners reporting that they thought PD could be used for AKI in the ICU. Among those who used PD in AKI management, the most commonly applied modalities were acute intermittent PD (n = 48), and then either tidal PD or continuous equilibrated PD (n = 39).
Figure 1.
— Practitioner opinion compared with practitioner use of peritoneal dialysis (PD) for acute kidney injury (AKI) in the intensive care unit (ICU).
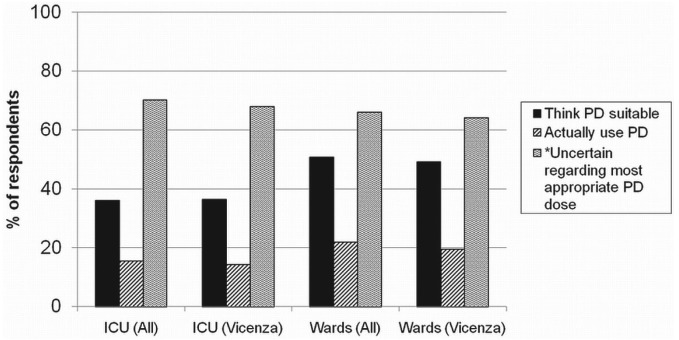
With regard to PD dose, 70.2% of respondents were not certain of the most appropriate dose for AKI in the ICU (Figure 2). However, when the analysis was limited to practitioners who actually used PD in the ICU, the proportion of physicians uncertain about the appropriate PD dose was slightly lower (52.1%). When a dose was indicated by the respondent, the dose most commonly thought to be appropriate for AKI in the ICU was a weekly standardized Kt/V of 2.1 or more (27.5%), followed by exchanges totaling 21 – 40 L in 24 hours (21.7%).
Figure 2.
— Practitioner opinion about the most appropriate peritoneal dialysis (PD) dose for acute kidney injury (AKI) in the intensive care unit (ICU). (Response to the question “In your opinion, what is the most appropriate PD dose for AKI in ICU?”) sKt/V = standardized Kt/V.
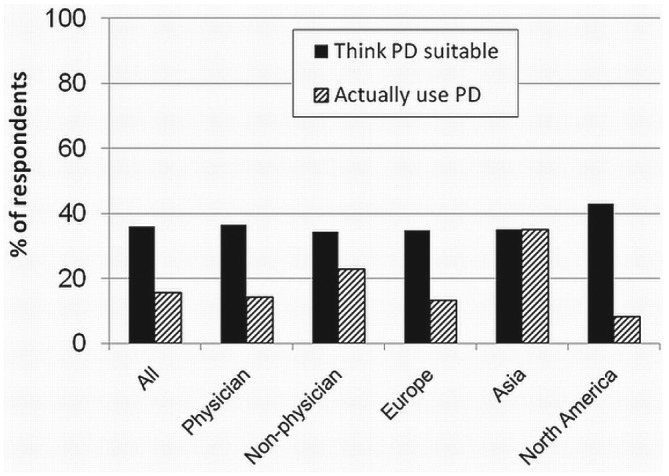
PD for AKI in the Wards: For use in the wards, 50.8% of respondents thought that PD is a suitable therapeutic option in most cases of AKI. By comparison, only 22% used it in their clinical practice (Figure 3). This discrepancy between opinion and actual practice was seen among physicians and non-physicians alike, and across different geographic areas. Again, the most striking discrepancy was noted in North America. As with PD for AKI the ICU, the use of PD for AKI in the wards was most common in the Asia–Pacific/Australasia region (45.9%) and less frequent in Europe (18.9%) and North America (12.2%). Similarly, the modalities most often used were either tidal PD or continuous equilibrated PD (n = 66), followed by acute intermittent PD (n = 62).
Figure 3.
— Practitioner opinion compared with practitioner use of peritoneal dialysis (PD) for acute kidney injury in the wards.
With regard to PD dose, 66.1% of all respondents were not certain of the most appropriate dose for AKI in the wards. Among PD users, the proportion was lower (36.8%). When a dose was indicated by the respondent, the most common response for an appropriate dose in the wards was a weekly standardized Kt/V of 2.1 (36.9%), followed by exchanges totaling 11 – 20 L in 24 hours (22.9%).
DISCUSSION
Our practitioner survey explored opinions and practice patterns with respect to PD in AKI. The key findings of our study are these:
Among responding practitioners, 36% – 51% considered PD to be a suitable option for most AKI cases (in the ICU and the wards respectively). By contrast, only 16% – 22% actually used PD in those circumstances.
At least limited use of PD was seen in all regions, but the modality was more commonly used in Asia than in other geographic areas.
More than half of all respondents were uncertain about the appropriate PD dose in AKI, regardless of whether they actually used PD for AKI management.
Interestingly, the divide between opinion about and actual practice of PD in AKI mirrors the situation seen in end-stage renal disease (ESRD). In a survey of American nephrologists, respondents agreed that, ideally, 40% of prevalent ESRD patients should be on PD to optimize cost effectiveness (8), and yet only 7.2% of prevalent ESRD patients in the United States are actually on PD (9). This discrepancy between opinion and actual practice was seen primarily among European and North American respondents; the difference was not as notable in Asian practitioners, but the limited number of respondents from Asia (n = 47) precludes definitive conclusions.
It is possible that a difference in the epidemiology of AKI between developing and developed countries may play a role in the observed discrepancy (10). In developing countries, AKI is more commonly attributed to medical conditions such as diarrheal illnesses, infections, and pregnancy. In the developed world, AKI is most often associated with multiorgan failure (10,11). Other reasons for the breach between opinion and practice are possible. Overall, good data on PD and AKI are in short supply, and the existing studies have shown conflicting results (7,12,13). Important concerns of physicians include potentially inaccurate fluid removal rates and inadequate solute clearances with PD, particularly in hypercatabolic patients (14). Most nephrologists may be more familiar— and therefore more comfortable—with modern HD machines and their precise volumetric systems that guide fluid removal. With regard to clearances, multiple studies have evaluated the dose of HD or continuous RRT for AKI (15–17), but virtually no data on the optimal dose of PD in that setting are available (2). It is therefore not surprising that nearly 70% of respondents were uncertain about an appropriate PD dose. As in ESRD, there is apprehension about the risk of peritonitis, especially among critically ill AKI patients. An additional concern in such patients is the potential effect of the presence of dialysate in the abdomen of mechanically ventilated patients. It can also be a problem to find a practitioner skilled in PD catheter insertion to urgently place a catheter in an acute setting; it is undoubtedly easier to find a person skilled in acute HD catheter insertion. In less experienced hands, a newly inserted PD catheter may possibly leak or fail to flow adequately, necessitating a switch to HD, often acutely in the middle of the night. Lastly, it is important to consider that exposure, or lack thereof, to a particular dialysis modality during fellowship training may influence future practice patterns. For example, with regard to PD in ESRD, some authors have suggested that many US renal training programs do not have enough PD patients or do not allocate appropriate training time to PD (18), potentially perpetuating a problematic cycle: physicians are not as comfortable with PD, thus further reducing the use of PD and, subsequently, training opportunities. The same may also be true of AKI. Indeed, a recent survey of self-perceived competency after nephrology fellowship training showed that only 30.1% of new nephrologists in the United States reported feeling well trained and competent in performing acute PD, and only 3.8% reported feeling well trained for placement of a PD catheter (19). By comparison, more than 90% felt well trained and competent in acute HD, and more than 60% and 90% felt competent for the placement of femoral and internal jugular HD catheters respectively.
Our study makes an important contribution to the body of information on PD and AKI. To our knowledge, only one other practitioner survey from Canada had specifically looked at the use of PD for AKI (20). Those investigators noted that PD was an infrequent choice of treatment for AKI and that the reported use of PD diminished to 3% from 8% during 1995 – 2000. The present study explores the discrepancies between opinion about, and actual utilization of, PD for AKI from an international perspective. Our results, derived from an international group of respondents, highlight the discrepancy between practitioner opinion and practice and also some important knowledge gaps.
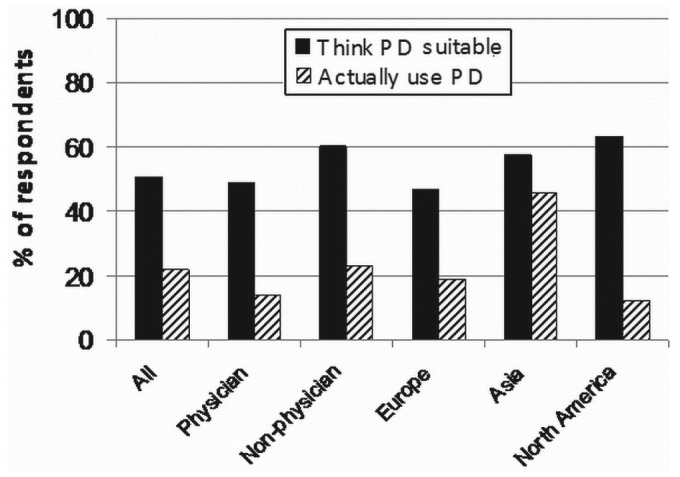
We acknowledge limitations in the present study. First, the survey was administered during dialysis meetings. Attendees are obviously interested in PD, therefore their opinions and practice are less likely to be representative of the nephrology community as a whole. Second, the numbers of respondents from Europe (74%) and from the Vicenza meeting (81.5%) are disproportionately higher. Our results may therefore not be fully generalizable. And yet we made an attempt—albeit limited—to broaden the range of respondents by including other meetings held on other continents. Indeed, one of the meetings was a HD-oriented meeting. But we acknowledge that the numbers of respondents from the ISPD and ISHD meetings were low, making interpretation difficult. Limiting the analysis to only the Vicenza meeting produced results similar to those observed in the combined analysis (Figure 4). Third, in a deliberate effort to keep the questionnaire brief, we obtained only restricted demographic information on the respondents. We therefore could not analyze the results by adult and pediatric nephrologists, by size of hospital, and so on. Fourth, the proportion of respondents from countries that frequently use PD in AKI situations (for example, Latin America) was very low (<5%); we therefore lack data from practitioners more accustomed to using PD in AKI settings.
Figure 4.
— Practitioner opinion compared with practitioner use of peritoneal dialysis (PD) and the most appropriate PD dose for acute kidney injury (AKI) in the intensive care unit (ICU) and wards, all meetings compared with the 18th International Vicenza Course on PD. (*Response to the question “In your opinion, what is the most appropriate PD dose for AKI?”)
SUMMARY
In the management of AKI, PD remains an important modality, especially in developing countries, which may lack the resources and technical support to perform HD (3). Interest in PD for AKI is being renewed, given recent studies showing excellent outcomes with the use of PD (7). Our pilot study found only limited use of PD for AKI, even though a significant portion of practitioners considered PD to be a suitable therapy. This is similar to the current situation in ESRD. We also found variability in the PD modalities used and considerable ambiguity about the appropriate PD dose for AKI. Those important issues deserve further study.
DISCLOSURES
DNC has received honoraria from Alere for speaking assignments. CR is a consultant for Alere, and a member of the speakers bureau for Abbott Diagnostics. The other authors have no conflicts of interest to declare.
REFERENCES
- 1. Basso F, Ricci Z, Cruz D, Ronco C. International survey on the management of acute kidney injury in critically ill patients: year 2007. Blood Purif 2010; 30:214–20 [DOI] [PubMed] [Google Scholar]
- 2. Chionh CY, Ronco C, Finkelstein FO, Soni SS, Cruz DN. Acute peritoneal dialysis: what is the “adequate” dose for acute kidney injury? Nephrol Dial Transplant 2010; 25:3155–60 [DOI] [PubMed] [Google Scholar]
- 3. Ash SR. Peritoneal dialysis in acute renal failure of adults: the under-utilized modality. Contrib Nephrol 2004; 144:239–54 [DOI] [PubMed] [Google Scholar]
- 4. Sharma SK, Manandhar D, Singh J, Chauhan HS, Koirala B, Gautam M, et al. Acute peritoneal dialysis in eastern Nepal. Perit Dial Int 2003; 23(Suppl 2):S196–9 [PubMed] [Google Scholar]
- 5. Bonilla–Félix M. Peritoneal dialysis in the pediatric intensive care unit setting. Perit Dial Int 2009; 29(Suppl 2):S183–5 [PubMed] [Google Scholar]
- 6. de Cal M, Cruz DN, Corradi V, Nalesso F, Polanco N, Lentini P, et al. HLA-DR expression and apoptosis: a cross-sectional controlled study in hemodialysis and peritoneal dialysis patients. Blood Purif 2008; 26:249–54 [DOI] [PubMed] [Google Scholar]
- 7. Gabriel DP, Caramori JT, Martim LC, Barretti P, Balbi AL. High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney Int Suppl 2008; (108):S87–93 [DOI] [PubMed] [Google Scholar]
- 8. Charest AF, Mendelssohn DC. Are North American nephrologists biased against peritoneal dialysis? Perit Dial Int 2001; 21:335–7 [PubMed] [Google Scholar]
- 9. United States Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Division of Kidney, Urologic, and Hematologic Diseases. USRDS 2007 Annual Data Report. Atlas of End-Stage Renal Disease in the United States. Bethesda, MD: United States Renal Data System; 2007. [Google Scholar]
- 10. Chugh KS, Sakhuja V, Malhotra HS, Pereira BJ. Changing trends in acute renal failure in third-world countries— Chandigarh study. Q J Med 1989; 73:1117–23 [PubMed] [Google Scholar]
- 11. Abreo K, Moorthy AV, Osborne M. Changing patterns and outcome of acute renal failure requiring hemodialysis. Arch Intern Med 1986; 146:1338–41 [PubMed] [Google Scholar]
- 12. Phu NH, Hien TT, Mai NT, Chau TT, Chuong LV, Loc PP, et al. Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Engl J Med 2002; 347:895–902 [DOI] [PubMed] [Google Scholar]
- 13. Gabriel DP, Nascimento GV, Caramori JT, Martim LC, Barretti P, Balbi AL. High volume peritoneal dialysis for acute renal failure. Perit Dial Int 2007; 27:277–82 [PubMed] [Google Scholar]
- 14. Evenepoel P, Bammens B, Verbeke K, Vanrenterghem Y. Superior dialytic clearance of β2-microglobulin and p-cresol by high-flux hemodialysis as compared to peritoneal dialysis. Kidney Int 2006; 70:794–9 [DOI] [PubMed] [Google Scholar]
- 15. Palevsky PM, Zhang JH, O’Connor TZ, Chertow GM, Crowley ST, Choudhury D, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 2008; 359:7–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lo S, et al. Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 2009; 361:1627–38 [DOI] [PubMed] [Google Scholar]
- 17. Vesconi S, Cruz DN, Fumagalli R, Kindgen–Milles D, Monti G, Marinho A, et al. Delivered dose of renal replacement therapy and mortality in critically ill patients with acute kidney injury. Crit Care 2009; 13:R57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blake PG, Finkelstein FO. Why is the proportion of patients doing peritoneal dialysis declining in North America? Perit Dial Int 2001; 21:107–14 [PubMed] [Google Scholar]
- 19. Berns JS. A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 2010; 5:490–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hyman A, Mendelssohn DC. Current Canadian approaches to dialysis for acute renal failure in the ICU. Am J Nephrol 2002; 22:29–34 [DOI] [PubMed] [Google Scholar]