Abstract
Purpose
Many factors such as lumbar instability and spinopelvic alignment are associated with low back pain. Our purpose was to analyze the pelvic incidence - one of spinopelvic alignment parameters- and spine instability correlations in patients with chronic low back pain.
Methods
Fifty-two patients suffering from chronic low back pain entered this case control study. Lateral spine radiography was taken from patients. pelvic incidence and L3, L4 and L5‘s vertebral body width were measured for all patients, and lumbar instability was evaluated in 3 different levels: L5-S1, L4-L5 and L3-L4.
Results
Thirty-two patients having lumbar instability formed group A and 20 patients without lumbar spine instability allocated to group B. Average age, mean weight, height, body mass index and mean vertebral width of both groups did not differ meaningfully. Pelvic incidence‘s mean amounts set to 53.9 in group B and 57.7 in group A without any significant difference; but pelvic incidence was significantly lower in patients with lumbar instability of L5-S1 origin (P=0.01).
Conclusions
Overall, pelvic incidence did not differ between two groups. However, separate evaluation of each level revealed lumbar instability of L5-S1 segment to be associated with lower pelvic incidence.
Keywords: Lumbar Vertebrae, Postural Balance, Low Back Pain, Spine, Pelvic Region
INTRODUCTION
Lumbar spinal instability (LSI) is known to be associated with chronic low back pain as one of its important causes [1]. Spinal instability is defined as the inability of the spine to maintain its orientation under physiological loads [2] and it's diagnosed by lumbar flexion/extension radiography in practice [3, 4]. In addition to instability, the relationship between postural factors and low back pain has been considered too. Many researches imply that spinopelvic alignment is of a great value for maintaining a good posture and subsequently, preventing low back pain [5–9].
Legaye described an anatomical parameter for assessing the spine alignment, called “Pelvic incidence”. He defines it as “the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axis of the femoral heads” [10]. The pelvic incidence is considered as a specific morphological parameter for each individual. It is not under the effect of posture or pelvis positioning and it is considered to be constant after cessation of growth. Pelvic incidence could also be measured by adding two other parameters: pelvic tilt and sacral slope [11].
Pelvic incidence and spinal alignment have been widely studied yet, mostly evaluating the normal ranges [12–15]. Some studies did not show any significant differences of pelvic incidence in spine diseases, in comparison with normal population [16, 17]. On the contrary, there are many studies showing pelvic incidence changes in spondylolisthesis [18, 19], low back pain, [20, 21] and disk diseases [22, 23].
Although many issues have been solved about pelvic incidence, the mechanism of its effect on spinal diseases is still unclear. Roughly, no scientific research has been mentioned in the literature regarding the evaluation of pelvic incidence in patients with or without lumbar spinal instability.
The aim of this study was to find a correlation between pelvic incidence and lumbar instability in patients with chronic low back pain.
METHODS AND SUBJECTS
Study design
This study is a case control study, investigating correlations between pelvic incidence and lumbar instability in patients with chronic low back pain.
Chronic low back pain was considered as a positive history of constant or intermittent low back pain for more than 3 months; or any pain onset less than one year, having at least 2 episodes of disabling low back pain during the past year.
All patients underwent complete examination. Height and weight of all 52 patients were measured and BMI was calculated. To evaluate instability, lateral spine radiography was taken in 3 different positions: neutral, full flexion and full extension. Dynamic translations of vertebra over each other and their rotations were computed as Dupuis explained, in 3 different levels: L5-S1, L4-L5 and L3-L4 [4] (Fig. 1).
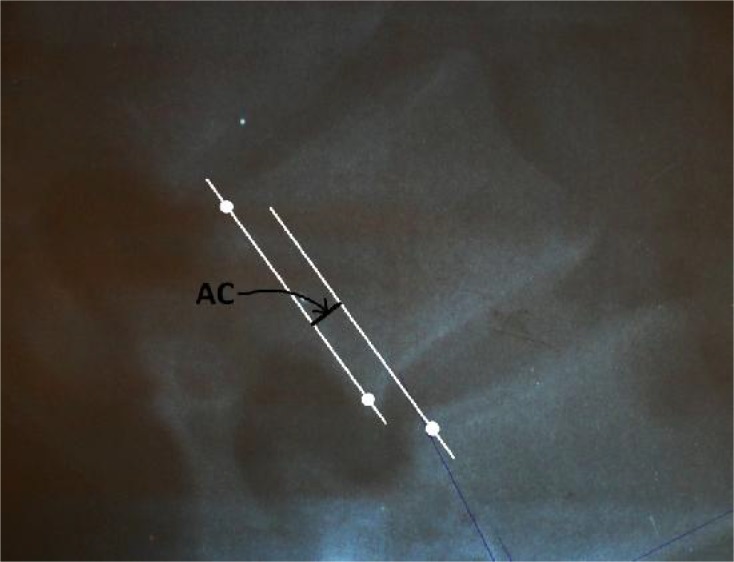
Fig. 1.
AC length describes absolute value of L4 translation over L5 in extension position
Numeral amount of translation was obtained from calculating absolute values of translation in both flexion and extension positions. To eliminate the magnification effect of radiographies, we also measured L3, L4 and L5‘s vertebral body width. So, through dividing the amount of translation by vertebra width we could report translation in percentage. Any translation more than 8% or any angulations more than 11 degrees were considered as lumbar spinal instability.
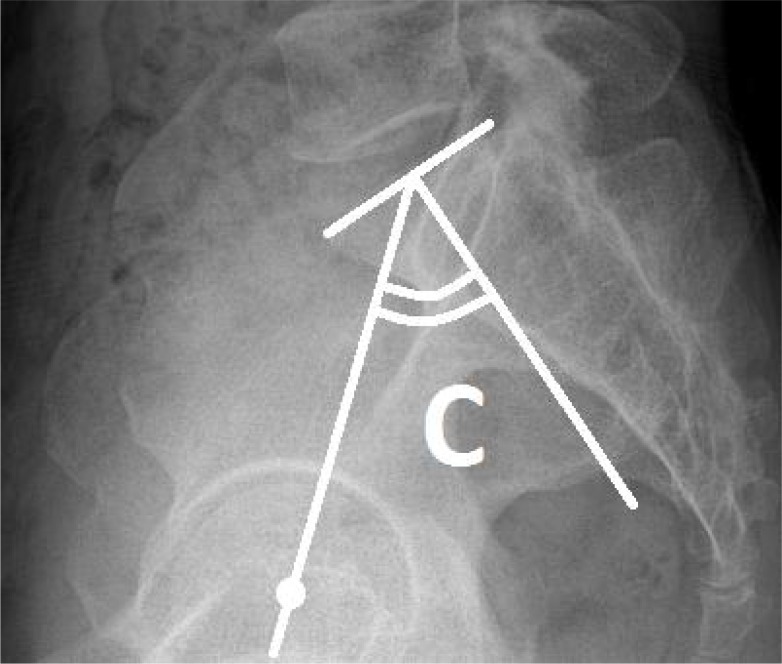
Concurrently, we measured pelvic incidence following Legaye's description [10] (Fig. 2). All measurements were done by one researcher and directly on the plain radiographs.
Fig. 2.
C angle shows pelvic incidence. Following Legaye's description pelvic incidence is “the angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the middle axis of the femoral heads”
Our study protocol was confirmed by the committee in charge of Tehran University of Medical Sciences research department and was approved by its ethics committee. All patients signed an informed consent too.
Settings
Subjects were examined in two spine clinics of Sina and Shafa hospitals in Iran between June 2010 and January 2012.
Subjects
Our study population consists of patients with chronic low back pain referred to our spine clinics. Our inclusion criteria were: not being older than 60 years old, no history of previous spine surgery, no contra indications for spine radiographies (such as pregnancy) and no limitations for doing complete spine movements (such as spasm or pain).
The patients also had to be able to understand they are participating in a study and they were provided with an informed consent.
Fifty-two subjects forming two groups were included in this study. Based on our findings 32 patients had lumbar spine instability, which formed group A: patients bearing nonspecific low back pain with lumbar instability. We formed another group called group B which comprises 20 Patients suffering from nonspecific low back pain without lumbar instability. These patients were matched for age and gender with group A.
Statistical analysis
To compare mean values of pelvic incidence between two groups, we performed student t-test using SPSS software (version 18.0). P value <0.05 was considered as the level of significance.
RESULTS
Fifty-two patients participated in this study from June 2010 till January 2012, including 30 males and 22 females. Our first group (Group A) consists of 32 patients suffering from non specific low back pain without lumbar instability (61.5%) and the next group (group B) comprises 20 patients diagnosed with non specific low back pain with lumbar instability (38.5%). Table 1 shows the descriptive data of the subjects. The groups were comparable in age, gender, height and weight.
Table 1.
Descriptive characteristics of the subjects
| Group | Age (y) | Female | Male | Height (m) | Weight (kg) | BMI (kg/m2) |
|---|---|---|---|---|---|---|
| Group A | 38.50 | 13 | 17 | 1.65 | 75.1 | 22.74 |
| Group B | 38.10 | 9 | 13 | 1.68 | 79.3 | 23.46 |
| P value | 0.2 | 0.4 | 0.7 | 0.3 | 0.08 | 0.9 |
BMI: Body Mass Index
Mean vertebral width of L3, L4 and L5 was 43.52±1.89, 44.12 ± 1.94 and 44.79 ±1.87 respectively and without any significant difference between two groups. Evaluating translations and angulations for each level separately, we observed most translations and angulations occur at L4-L5 level with 65% at both. Next point belongs to L3-L4 level with 30% of translations and 25% of angulations. The Least frequency pertains to L5-S1 level with 5% and 8% for translations and angulations, respectively.
At last by analyzing pelvic incidence, mean amounts set to 53.9 in group A and 57.7 in group B without any meaningful difference in both groups; but evaluating pelvic incidence separately for each level, we observed pelvic incidence is significantly lower in patients with lumbar instability of L5-S1 origin (P=0.01) (Table 2).
Table 2.
Mean pelvic incidence of both groups in different levels
| Level | Group A | Group B | P value |
|---|---|---|---|
| L3 – L4 Level | 55.69 | 55.39 | 0.9 |
| L4 – L5 Level | 57.04 | 53.92 | 0.4 |
| L5 – S1 Level | 55.81 | 38.33 | 0.01 |
DISCUSSION
Several authors tried to describe the spine movement through spine alignment. A normal lumbar spine movement follows a complex pattern during flexion and extension. Kanayama mentions each lumbar segment movement, follows a sequence which starts from superior levels and continues in lower segments with a specific delay[24]. Seven years later Wong states normal movement of lumbar spine occurs via simultaneous segmental motion [25]. Previous studies have also assessed postural factors in low back pain. Spine structure or spinopelvic alignments and their correlation with low back pain were of great concern for many authors [1, 5–9, 26], but the relationship between sagittal alignment and LBP is still poorly understood.
As an important parameter of spinopelvic alignment, pelvic incidence has been widely studied. This morphological index is not affected by the quality of the x-ray and is considered as a reliable parameter. Pelvic incidence is not affected by the posture or the pelvis position and considered as invariable for a subject after the end of growth. It is also perceived as a constant guide value to understand variations in the patient population [27].
These features made pelvic incidence as our variable of choice to evaluate spine instability. Many issues have been discussed about pelvic incidence. Many researches tried to publish a normal range but, there has not been an accepted range established yet [12–14, 28]. There are some studies which did not show any relation between pelvic incidence and spine disorders, but they also note other spinopelvic parameters to influence spine disease [16, 17]. Evaluating all three levels, we also did not found pelvic incidence to affect lumbar spine instability. Though there are many others who believe in the effect of pelvic incidence, as we do. Hansson et al and Labelle et al declare pelvic incidence is not only significantly higher in isthmic spondylolisthesis subjects in comparison with normal population but also meaningfully higher in high grade spondylolisthesis compared with the low grade form [18, 19]. Schuler also showed a significant higher pelvic incidence in degenerative spondylolisthesis [29]. Yoshimito denotes that in patients with hip osteoarthritis, pelvic incidence is significantly higher and concludes patients with higher pelvic incidences are at a higher risk for developing hip osteoarthritis in late life [30]. In 2007, some notable studies assessing pelvic incidence, low back pain and degenerative disk diseases were published. Barrey claimed that pelvic incidence is significantly lower in young patients with any disk diseases, opposing the healthy control population [22]. Waris shows a higher concurrence of degenerative disk diseases among low back pain patients [31]. Leone intimated disk shears are initially painful and can be presented as low back pain [32]. More than that, any disk damages can cause abnormal movements in the spine. So, pain and abnormal movements together, made a concept in which any lumbar instability can cause low back pain [20]. As it was mentioned before, lumbar segmental instability is one the important causes of chronic low back pain [1]. In this paper we tried to help better understanding of the spine instability. This study is the first study to evaluate pelvic incidence correlations in patients with lumbar instability versus patients without lumbar instability. It is also the first study to discuss separate evaluation of different levels in lumbar instability. In 2011 Chaleat-Valayer concluded patients with lower pelvic incidence are at a higher risk for low back pain. He ratiocinated as the pelvic incidence declines, lumbar lordosis decreases and disk pressure and degeneration increases, causing low back pain [21]. In 2012 Sevrain announced there is a significant relationship between pelvic incidence and shear stresses in intervertebral disks [23].
In this study we did not find pelvic incidence to be different in patients with lumbar instability versus patients without lumbar instability. However, separate evaluation of each level revealed lumbar instability of L5-S1 segment to be associated with lower pelvic incidence. As we mentioned before, only three patients had lumbar instability of L5-S1 segment, so it should be kept in mind that we were facing a limitation of quantity in this group.
CONCLUSION
As recent studies show, lower pelvic incidences are associated with spine disorders. Although more studies with larger sample sizes are needed to definitely conclude, but we think lower pelvic incidence is associated with lumbar instability in L5-S1 segment, too. It also seems logical to disclose a new concept in evaluating correlations of different levels of lumbar instability and pelvic incidence.
ACKNOWLEDGMENTS
Our study protocol was confirmed by the committee in charge of Tehran University of Medical Sciences research department. We would like to appreciate all those who collaborated with us in this study.
Conflict of interests: None
REFERENCES
- 1.O'Sullivan PB. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5:2–12. doi: 10.1054/math.1999.0213. [DOI] [PubMed] [Google Scholar]
- 2.Panjabi MM, Lydon C, Vasavada A, et al. On the understanding of clinical instability. Spine (Phila Pa 1976) 1994;19:2642–50. [PubMed] [Google Scholar]
- 3.Dvorak J, Panjabi MM, Novotny JE, et al. Clinical validation of functional flexion-extension roentgenograms of the lumbar spine. Spine (Phila Pa 1976) 1991;16:943–50. doi: 10.1097/00007632-199108000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dupuis P.R, Yong-Hing K, Cassidy JD, Kirkaldy-Willis WH. Radiologic diagnosis of degenerative lumbar spinal instability. Spine (Phila Pa 1976) 1985;10:262–76. doi: 10.1097/00007632-198504000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–7. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 6.Janssen MM, Drevelle X, Humbert L, et al. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34:E826–32. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 7.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J. 2011;20(Suppl 5):572–7. doi: 10.1007/s00586-011-1923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–53. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 9.Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–7. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–22. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mac-Thiong JM, Labelle H, Berthonnaud E, et al. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16:227–34. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neal CJ, McClendon J, Halpin R, et al. Predicting ideal spinopelvic balance in adult spinal deformity. J Neurosurg Spine. 2011;15:82–91. doi: 10.3171/2011.2.SPINE1018. [DOI] [PubMed] [Google Scholar]
- 14.Vrtovec T, Janssen MM, Pernuš F, et al. Analysis of Pelvic Incidence from Three-Dimensional Images of a Normal Population. Spine (Phila Pa 1976) 2012;37:E479–85. doi: 10.1097/BRS.0b013e31823770af. [DOI] [PubMed] [Google Scholar]
- 15.Berthonnaud E, Labelle H, Roussouly P, et al. A variability study of computerized sagittal spinopelvic radiologic measurements of trunk balance. J Spinal Disord Tech. 2005;18:66–71. doi: 10.1097/01.bsd.0000128345.32521.43. [DOI] [PubMed] [Google Scholar]
- 16.Gautier J, Morillon P, Marcelli C. Does spinal morphology influence the occurrence of low back pain? A retrospective clinical, anthropometric, and radiological study. Rev Rhum Engl Ed. 1999;66:29–34. [PubMed] [Google Scholar]
- 17.Rajnics P, Templier A, Skalli W, et al. The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002;26:104–8. doi: 10.1007/s00264-001-0317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Labelle H, Roussouly P, Berthonnaud E, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine (Phila Pa 1976) 2004;29:2049–54. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 19.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine (Phila Pa 1976) 2002;27:2026–9. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 20.Mulholland RC. The myth of lumbar instability: the importance of abnormal loading as a cause of low back pain. Eur Spine J. 2008;17:619–25. doi: 10.1007/s00586-008-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaleat-Valayer E, Mac-Thiong JM, Paquet J, et al. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J. 2011;20(Suppl 5):634–40. doi: 10.1007/s00586-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16:1459–67. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sevrain A, Aubin CE, Gharbi H, et al. Biomechanical evaluation of predictive parameters of progression in adolescent isthmic spondylolisthesis: a computer modeling and simulation study. Scoliosis. 2012;7:2. doi: 10.1186/1748-7161-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kanayama M, Abumi K, Kaneda K, et al. Phase lag of the intersegmental motion in flexion-extension of the lumbar and lumbosacral spine. An in vivo study. Spine (Phila Pa 1976) 1996;21:1416–22. doi: 10.1097/00007632-199606150-00004. [DOI] [PubMed] [Google Scholar]
- 25.Wong KW, Luk KD, Leong JC, et al. Continuous dynamic spinal motion analysis. Spine (Phila Pa 1976) 2006;31:414–9. doi: 10.1097/01.brs.0000199955.87517.82. [DOI] [PubMed] [Google Scholar]
- 26.Tuzun C, Yorulmaz I, Cindaş A, Vatan S. Low back pain and posture. Clin Rheumatol. 1999;18:308–12. doi: 10.1007/s100670050107. [DOI] [PubMed] [Google Scholar]
- 27.Blondel B, Jouve JL, Panuel M, et al. [Pelvic incidence reliability in spine sagittal balance] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:321–6. doi: 10.1016/j.rco.2008.01.005. Article in French. [DOI] [PubMed] [Google Scholar]
- 28.Mac-Thiong JM, Labelle H, Roussouly P. Pediatric sagittal alignment. Eur Spine J. 2011;20(Suppl 5):586–90. doi: 10.1007/s00586-011-1925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schuller S, Charles YP, Steib JP. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J. 2011;20:713–9. doi: 10.1007/s00586-010-1640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoshimoto H, Sato S, Masuda T, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 2005;30:1650–7. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 31.Waris E, Eskelin M, Hermunen H, et al. Disc degeneration in low back pain: a 17-year follow-up study using magnetic resonance imaging. Spine (Phila Pa 1976) 2007;32:681–4. doi: 10.1097/01.brs.0000257523.38337.96. [DOI] [PubMed] [Google Scholar]
- 32.Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245:62–77. doi: 10.1148/radiol.2451051359. [DOI] [PubMed] [Google Scholar]