Abstract
The World Health Organization states that in a widespread report that “in developed countries, adherence among patients suffering chronic diseases averages only 50%”. We followed the quoted references to this statement. The data basis for this statement is one randomized controlled trial (RCT) on hypertensive steel workers in Canada published in 1975 and one study dealing with neurotic outpatients in Pennsylvania, USA published in 1965. Both studies are not suitable to assume such generalized adherence estimation and are not for different reasons transferable to today’s patient care.
Keywords: patient compliance, medication adherence, chronic disease, evidence-based medicine, information science, behavior
Abstract
Die Weltgesundheitsorganisation (WHO) gibt in einem sehr verbreiteten Bericht an, dass die Therapietreue bei Patienten mit chronischen Erkrankungen bei durchschnittlich 50% in entwickelten Ländern liegt. Wir haben anhand der Literaturhinweise die Basis dieser Aussage verfolgt. Die Basis dieser Aussage ist lediglich eine randomisierte kontrollierte Studie (RCT) an kanadischen Stahlarbeitern mit Hypertension von 1975 sowie eine US-amerikanische Studie an neurotischen Patienten von 1965. Beide Studien sind nicht geeignet eine derart generalisierte Aussage zu treffen und darüber hinaus nicht auf die gegenwärtige Patientenversorgung übertragbar.
Main text
Adherence is an often discussed issue nowadays. Also the World Health Organization (WHO) is concerned with the problem of poor adherence. In one of its reports the magnitude of adherence is described and examples for different adherence estimates for various chronic conditions are given. Furthermore the WHO states in this context, that: “a number of rigorous reviews have found that, in developed countries, adherence among patients suffering chronic diseases averages only 50%” [1]. According to Google scholar the WHO report has already been cited for more than 100 times in 2012. Moreover the above mentioned statement is still frequently quoted (see among others [2], [3], [4]). Thus it seems that many researchers don’t check this statement or its origin. We made an effort to follow the quoted references to this statement and found the data basis quite doubtful in the end.
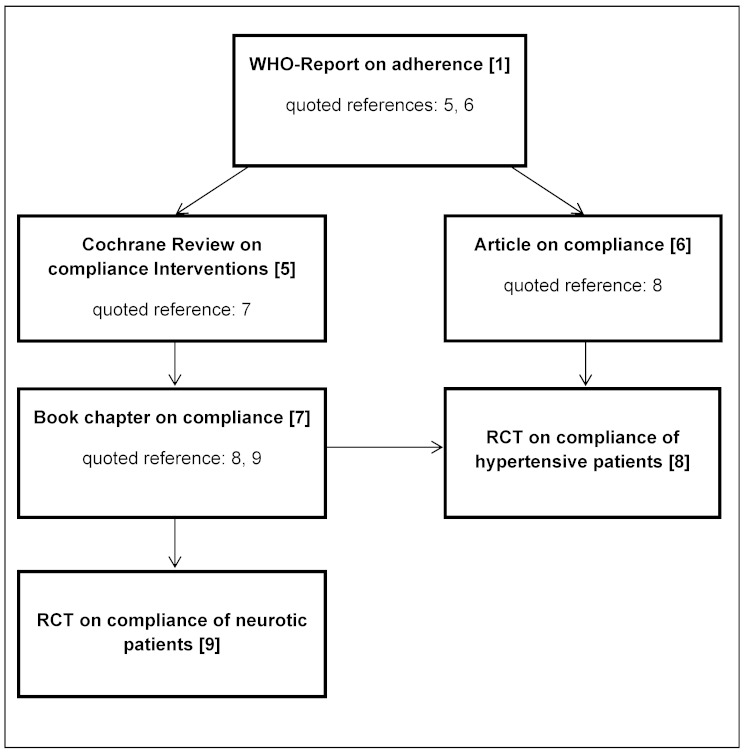
In the article by the WHO two references are given for this specific statement. The first one is a Cochrane Review on interventions to enhance patient compliance [5] and the second one is an article on improving patient compliance to antihypertensive regimes [6]. The statement in the Cochrane Review is: “Typical adherence rates for prescribed medications are about 50% with a range from 0% to over 100%“ [5]. But the statement doesn’t refer to chronic conditions or certain countries, as suggested by the WHO statement. In the other article it is stated that “only about half (...) taking (…) 80% or more of their (...) drugs” [6]. Both articles are not the original sources of the information, but refer to other references. The Cochrane Review refers to a chapter of a book on the magnitude of patient compliance published in 1979 [7] and the other article refers to a randomized controlled trial (RCT) conducted in 1975 [8]. The book chapter lists a great number of studies on compliance and persistence among others for long-term chronic conditions (12 studies), of which is deduced that “compliance with different long-term medication regimes for different illnesses in different settings converge to approximately 50% (…) when the estimation is not based on self-reports” (for a better understanding of citation way see Figure 1 (Fig. 1)). The adherence rates of listed studies are in a range between 33% and 94%. In consideration of the WHO’s definition of adherence and excluding “remaining in care” as adherence measure, finally two studies could be the potential basis of data for the WHO statement, originated from the Cochrane review. One of these two studies is a RCT on hypertensive steel workers in Canada published in 1975 (see above) [8], while the second study deals with neurotic outpatients in Pennsylvania, USA published in 1965 [9]. The adherence rates (proportion of adherent patients) are indeed 53% and 56% respectively. Apart from the fact that throughout the way of citation the original statement has changed like whispers down the lane, both studies are not suitable to assume such generalized adherence estimation.
Figure 1. Flow chart of citation way.
In the last decades treatments for most diseases have changed fundamentally. An easier intake regime as well as better safety profile is often the consequence. Both factors are considered as adherence influencing factors [10], [11]. Therefore, results seem to be out of date (published in 1965 and 1975) and cannot be transferred to today’s situation. Also study populations vary widely between the different studies. One study deals with hypertensive steal workers and the other one with neuropathic patients who receive tranquillisers. Various diseases implicate distinct intake regimes and drug reactions with consequences on adherence [12]. Furthermore, the required adherence rate and the necessary adherence dimensions (time, dosage and concurrent circumstances) depend on the condition and the treatment and therefore different reference levels (required adherence rates) exist. Moreover, patient characteristics in particular regarding sex and mental health are very heterogeneous between studies. For both factors an influence on adherence has been demonstrated (see among others [13], [14], [15], [16]). Hypertensive steel workers take their medicine for secondary prevention. This fact is a further restriction because adherence to medication for secondary prevention can be lower due to the absence of symptoms or in other words due to the low perceived benefit of drugs by patients. This has been proven in stroke patients for example [17]. Moreover, definitions of adherence vary and consequently hamper a comparison. According to the study on the hypertensive steel workers a patient who takes ≥80% of the prescribed pills is defined as adherent whereas in the study on neurotic patients >75% of the prescribed caps had to been taken to be classified as adherent. The different definitions could have a great influence on summarized rates.
If all mentioned factors are taken into account one could sum up that deducing generalized adherence estimation for all chronic conditions is not possible and should be avoided. In addition, due to its complexity adherence estimates need to be described in detail. Even in the WHO report further references as examples are given for various chronic conditions that show a wide range of adherence estimates and the mentioned issues are partly addressed. Nevertheless, this generalized non-evidence based adherence estimation is given.
To generate valid and therefore convincing and interpretable adherence estimates, patient characteristics, the treatment, the mathematical definition and the measurement of adherence has to be described. Adherence should be defined on the basis of the clinical background for example by proving the required proportion of doses taken to reach a substantial clinical effect.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.World Health Organisation. Adherence to long-term therapies: evidence for action. Geneva: WHO; 2003. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/ [Google Scholar]
- 2.Defulio A, Silverman K. The use of incentives to reinforce medication adherence. Prev Med. 2012 Nov;55 Suppl:S86–S94. doi: 10.1016/j.ypmed.2012.04.017. Available from: http://dx.doi.org/10.1016/j.ypmed.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011 Apr;86(4):304–314. doi: 10.4065/mcp.2010.0575. Available from: http://dx.doi.org/10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Carroll R, Dennis M, Johnston M, Sudlow C. Improving adherence to medication in stroke survivors (IAMSS): a randomised controlled trial: study protocol. BMC Neurol. 2010 Feb 24;10:15. doi: 10.1186/1471-2377-10-15. Available from: http://dx.doi.org/10.1186/1471-2377-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haynes RB, Montague P, Oliver T, McKibbon KA, Brouwers MC, Kanani R. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2001;(1):CD000011. doi: 10.1002/14651858.CD000011. Available from: http://dx.doi.org/10.1002/14651858.CD000011. [DOI] [PubMed] [Google Scholar]
- 6.Sackett DL, Haynes RB, Gibson ES, Taylor DW, Roberts RS, Johnson AL. Patient compliance with antihypertensive regimens. Patient Couns Health Educ. 1978 1st Quart;1(1):18–21. doi: 10.1016/s0738-3991(78)80033-0. [DOI] [PubMed] [Google Scholar]
- 7.Sackett DL, Snow JC. Compliance in Health Care. In: Haynes D, Taylor W, Sackett DL, editors. Compliance in Health Care. Baltimore: Johns Hopkins University Press; 1979. [Google Scholar]
- 8.Sackett DL, Haynes RB, Gibson ES, Hackett BC, Taylor DW, Roberts RS, Johnson AL. Randomised clinical trial of strategies for improving medication compliance in primary hypertension. Lancet. 1975 May 31;1(7918):1205–1207. doi: 10.1016/S0140-6736(75)92192-3. Available from: http://dx.doi.org/10.1016/S0140-6736(75)92192-3. [DOI] [PubMed] [Google Scholar]
- 9.Lipman RS, Rickels K, Uhlenhuth EH, Park LC, Fisher S. Neurotics who fail to take their drugs. Br J Psychiatry. 1965 Nov;111(480):1043–1049. doi: 10.1192/bjp.111.480.1043. Available from: http://dx.doi.org/10.1192/bjp.111.480.1043. [DOI] [PubMed] [Google Scholar]
- 10.Penning-van Beest FJ, Erkens JA, Olson M, Herings RM. Determinants of non-compliance with bisphosphonates in women with postmenopausal osteoporosis. Curr Med Res Opin. 2008 May;24(5):1337–1344. doi: 10.1185/030079908X297358. Available from: http://dx.doi.org/10.1185/030079908X297358. [DOI] [PubMed] [Google Scholar]
- 11.Sung JC, Nichol MB, Venturini F, Bailey KL, McCombs JS, Cody M. Factors affecting patient compliance with antihyperlipidemic medications in an HMO population. Am J Manag Care. 1998 Oct;4(10):1421–1430. [PubMed] [Google Scholar]
- 12.Kardas P. Rozpowszechnienie nieprzestrzegania zalecen terapeutycznych wsrod pacjentow leczonych z powodu wybranych schorzen przewleklych. [Prevalence of non-adherence to medication among patients treated for selected chronic conditions]. Pol Merkur Lekarski. 2011 Oct;31(184):215–220. [PubMed] [Google Scholar]
- 13.Sclar DA, Robison LM, Skaer TL, Dickson WM, Kozma CM, Reeder CE. Sulfonylurea pharmacotherapy regimen adherence in a Medicaid population: influence of age, gender, and race. Diabetes Educ. 1999 Jul-Aug;25(4):531–2, 535, 537. doi: 10.1177/014572179902500406. Available from: http://dx.doi.org/10.1177/014572179902500406. [DOI] [PubMed] [Google Scholar]
- 14.Granger BB, Ekman I, Granger CB, Ostergren J, Olofsson B, Michelson E, McMurray JJ, Yusuf S, Pfeffer MA, Swedberg K. Adherence to medication according to sex and age in the CHARM programme. Eur J Heart Fail. 2009 Nov;11(11):1092–1098. doi: 10.1093/eurjhf/hfp142. Available from: http://dx.doi.org/10.1093/eurjhf/hfp142. [DOI] [PubMed] [Google Scholar]
- 15.Springer SA, Dushaj A, Azar MM. The Impact of DSM-IV Mental Disorders on Adherence to Combination Antiretroviral Therapy Among Adult Persons Living with HIV/AIDS: A Systematic Review. AIDS Behav. 2012 Nov;16(8):2119–2143. doi: 10.1007/s10461-012-0212-3. Available from: http://dx.doi.org/10.1007/s10461-012-0212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ortego C, Huedo-Medina TB, Santos P, Rodríguez E, Sevilla L, Warren M, Llorca J. Sex differences in adherence to highly active antiretroviral therapy: A meta-analysis. AIDS Care. 2012 Dec;24(12):1519–1534. doi: 10.1080/09540121.2012.672722. Available from: http://dx.doi.org/10.1080/09540121.2012.672722. [DOI] [PubMed] [Google Scholar]
- 17.O'Carroll R, Whittaker J, Hamilton B, Johnston M, Sudlow C, Dennis M. Predictors of adherence to secondary preventive medication in stroke patients. Ann Behav Med. 2011 Jun;41(3):383–390. doi: 10.1007/s12160-010-9257-6. Available from: http://dx.doi.org/10.1007/s12160-010-9257-6. [DOI] [PubMed] [Google Scholar]