Abstract
Background
The postpartum period may be critical for the development of midlife obesity. Identifying factors associated with postpartum weight change could aid in targeting women for healthy lifestyle interventions.
Methods
Data from Active Mothers Postpartum (AMP), a study of overweight and obese postpartum women (n=450), were analyzed to determine the effect of baseline characteristics, breastfeeding, diet, physical activity, and contraception on weight change from 6 weeks to 12, 18, and 24 months postpartum. The repeated measures mixed model was used to test the association of these effects with weight change.
Results
Although mean weight loss was modest (0.49 kg by 24 months), the range of weight change was striking (+21.5 kg to −24.5 kg, standard deviation [SD] 7.4). Controlling only for baseline weight, weight loss was associated with breastfeeding, hormonal contraception, lower junk food and greater healthy food intake, and greater physical activity. Only junk food intake and physical activity were significant after controlling for all other predictors.
Conclusions
Eating less healthy foods and being less physically active put overweight and obese women at risk of gaining more weight after a pregnancy.
Introduction
Postpartum weight retention can be a significant contributor to the development of obesity.1,2 Weight retention associated with pregnancy can vary greatly, with as many as 20% of women retaining ≥5 kg.1 The most important predictors of postpartum weight retention are a high prepregnancy body mass index (BMI), excessive gestational weight gain, and being African American,1–7 whereas breastfeeding can contribute modestly to weight loss.8–10
Strategies to prevent postpartum weight retention include behaviors associated with weight control in the general population, primarily improved diet and increased physical activity.11 In the Stockholm Pregnancy and Weight Study, women who retained more weight 1 year postpartum were less likely to report regular exercise and more likely to report inconsistent meals and between-meal snacking.12,13 Olson et al.14 found that frequency of physical activity and overall energy intake were associated with weight retention, and Oken et al.15 found that more television watching, less walking, and more trans fat intake were associated with likelihood of retaining >5 kg at 12 months postpartum.
Active Mothers Postpartum (AMP) was a randomized controlled behavioral intervention trial to enhance weight loss in overweight or obese postpartum women.16 The intervention was based on the premise that the postpartum period may be a teachable moment for making weight-related lifestyle changes; however, it had modest and not statistically significant effects on behavioral outcomes and weight loss by 12 months17 and no effect at 24 months postpartum (the effects are shown in Tables 2 and 3). Regardless of arm, however, there was remarkable variability in weight change during the 2-year study period, ranging from 21.5 kg weight loss to 24.5 kg weight gain. Therefore, we sought to identify predictors associated with successful weight loss from baseline (6 weeks postpartum) to 12, 18, and 24 months postpartum in the overall sample of overweight and obese mothers.
Table 2.
Mean Weight Change (kg) from Baseline (6 Weeks) to 12, 18, and 24 Months Postpartum, by Category of Predictor
| Predictors | Weight change at 12 months mean (SE) n=315 | Weight change at 18 months mean (SE) n=323 | Weight change at 24 months mean (SE) n=348 |
|---|---|---|---|
| Overall weight change | −0.87 (0.33) | −0.90 (0.37) | −0.56 (0.40) |
| Minimum, maximum | −13.9, 14.3 | −20.8, 19.8 | −21.5, 24.5 |
| Age, years | |||
| 18–24 | 2.77 (1.05)** | 3.24 (1.18)** | 3.42 (1.05)* |
| 25–35 | −1.37 (0.41) | −1.70 (0.49) | −1.62 (0.54) |
| ≥35 | −1.00 (0.58) | −0.99 (0.59) | −0.48 (0.66) |
| Race | |||
| White/ other | −2.23 (0.40)*** | −2.56 (0.45)*** | −2.61 (0.52)*** |
| African American | 1.09 (0.49) | 1.12 (0.57) | 1.65 (0.57) |
| Education | |||
| High school or less | 2.87 (0.87)*** | 2.15 (0.93)*** | 2.34 (0.88)*** |
| Some college | 0.63 (0.67) | 1.20 (0.72) | 1.05 (0.80) |
| College degree | −2.42 (0.37) | −2.69 (0.43) | −2.20 (0.49) |
| Marital status | |||
| Unmarried | 2.42 (0.70)*** | 2.76 (0.90)*** | 2.84 (0.90)*** |
| Married/cohabiting | −1.61 (0.35) | −1.84 (0.38) | −1.47 (0.43) |
| Parity | |||
| One child | −1.24 (0.48) | −1.36 (0.60) | −0.16 (0.68) |
| Two children | −0.99 (0.55) | −0.81 (0.61) | −1.15 (0.63) |
| Three or more children | 0.00 (0.72) | −0.33 (0.74) | −0.24 (0.80) |
| Body mass index, kg/m2 | |||
| 25–29.9 (overweight) | −2.55 (0.43)** | −2.63 (0.46)** | −2.21 (0.48)** |
| 30–34.9 (obese class I) | −1.69 (0.60) | −1.41 (0.67) | −1.73 (0.74) |
| 35–39.9 (obese class II) | 2.62 (0.77) | 2.52 (0.92) | 2.84 (1.08) |
| 40+ (obese class III) | 2.90 (0.91) | 2.15 (1.35) | 3.45 (1.26) |
| Gestational weight gain | |||
| Below IOM recommendations | 0.95 (0.65)*** | 1.90 (0.73)*** | 2.01 (0.83)*** |
| Within IOM recommendations | −0.57 (0.62) | −0.03 (0.74) | −0.16 (0.83) |
| Over IOM recommendations | −1.57 (0.45) | −2.14 (0.49) | −1.57 (0.53) |
| Pregnancy since baseline | |||
| No | −0.86 (0.34) | −0.93 (0.39) | −0.86 (0.45) |
| Yes | −3.51 (1.31) | −1.01 (1.25) | 0.95 (0.79) |
| Study arm | |||
| Control | −0.49 (0.48) | −1.07 (0.56) | −0.81 (0.61) |
| AMP intervention | −1.21 (0.45) | −0.75 (0.50) | −0.33 (0.52) |
| Junk food scorea | |||
| Low (lower quartile) | −3.46 (0.56)*** | −4.33 (0.66)*** | −3.81 (0.73)*** |
| Average (middle quartiles) | −0.31 (0.44) | −0.69 (0.49) | −0.06 (0.56) |
| High (upper quartile) | 1.36 (0.71) | 2.55 (0.75) | 1.90 (0.76) |
| Healthy food scorea | |||
| Low (lower quartile) | 0.71 (0.74)* | 1.23 (0.81)** | 1.57 (0.85)** |
| Average (middle quartiles) | −1.15 (0.42) | −1.36 (0.49) | −1.27 (0.55) |
| High (upper quartile) | −1.64 (0.67) | −1.91 (0.74) | −1.21 (0.72) |
| Physical activitya | |||
| <1 day per week | 1.34 (1.66)** | 2.91 (2.49)* | 7.09 (1.44)** |
| 1–4 days per week | −0.57 (0.37) | −0.58 (0.39) | −0.28 (0.43) |
| 5–7 days per week | −2.47 (0.74) | −3.16 (1.05) | −3.41 (1.01) |
| Lactation score | |||
| 0 | 0.43 (0.67)* | 0.58 (0.81)* | 1.64 (0.79)* |
| 1–5 | −0.21 (0.80) | 0.04 (0.87) | −0.75 (0.85) |
| 6–11 | −1.30 (0.66) | −1.53 (0.74) | −1.75 (0.87) |
| 12–17 | −1.17 (0.80) | −1.69 (0.87) | −0.51 (0.99) |
| 18–24 | −2.85 (0.71) | −3.00 (0.77) | −2.59 (0.89) |
| Hormonal contraception (at 12 months) | |||
| No | −0.31 (0.41) | −0.32 (0.48) | −0.24 (0.55)* |
| Yes | −2.30 (0.73) | −2.64 (0.85) | −3.17 (1.01) |
Statistical significance at each time point from mixed linear model, controlling only for the baseline weight (using continuous versions of variables where available): *p<0.05; **p<0.01; ***p<0.0001.
Mean of measures reported at prior and current time points.
SE, standard error.
Table 3.
Mean Covariate-Adjusted Weight Change (kg) from Baseline (6 Weeks) to 12, 18, and 24 Months Postpartum due to Unit Change in Predictor
| Predictors | Weight change at 12 months β coefficient (SE) | Weight change at 18 months β coefficient (SE) | Weight change at 24 months β coefficient (SE) |
|---|---|---|---|
| Reference groupa | 6.08 (1.6) | 6.43 (1.3) | 5.95 (1.3) |
| Age (per year) | −0.04 (0.1) | 0.01 (0.1) | 0.06 (0.1) |
| African American | 0.25 (0.8) | 0.05 (0.8) | 0.57 (0.8) |
| Some college | −0.84 (1.1) | −0.25 (1.1) | −0.04 (1.0) |
| College degree | −2.48* (1.1) | −2.36* (1.1) | −2.17* (1.0) |
| Married/cohabiting | −1.79 (1.0) | −2.56** (0.9) | −2.01* (0.9) |
| Two children | −0.12 (0.7) | 0.08 (0.7) | −0.76 (0.7) |
| Three or more children | −1.97* (0.9) | −2.11* (0.9) | −2.20* (0.9) |
| Baseline weight (per 10 kg) | 0.82*** (0.0) | 0.74** (0.0) | 0.64** (0.0) |
| Height (per 10 cm) | −0.55 (0.1) | −1.08* (0.1) | −1.11* (0.1) |
| Pregnancy weight gain (per kg) | −0.19*** (0.0) | −0.21*** (0.0) | −0.19*** (0.0) |
| Pregnancy since baseline | 0.34 (1.5) | −0.33 (1.0) | 1.51* (0.7) |
| Study intervention arm | −0.04 (0.6) | 0.51 (0.6) | 0.79 (0.6) |
| Junk food scoreb | 0.90* (0.4) | 1.20** (0.4) | 1.34** (0.4) |
| Healthy food scoreb | 0.02 (0.4) | −0.35 (0.4) | −0.36 (0.3) |
| Physical activityc | −0.91*** (0.2) | −0.84** (0.2) | −1.09*** (0.2) |
| Lactation score (per unit) | −0.03 (0.0) | 0.00 (0.0) | 0.02 (0.0) |
| Hormonal contraception (at 12 months) | −1.17 (0.7) | −1.32 (0.7) | −1.45 (0.7) |
Significant effects in bold: *p<0.05; **p<0.01; ***p<0.0001.
Mean age (30.9 years); not African American; high school education or less; single; one child; mean weight (88.8 kg); mean height (163.8 cm); mean pregnancy weight gain (14.9 kg); mean junk food or healthy food score (zero); zero days per week of physical activity; lactation score of zero (never breastfed); not using hormonal contraception; in study control arm.
Per junk food or healthy food score unit (1 SD); mean of current and prior scores.
Per days per week of physical activity; mean of measures reported at current and prior time points.
The studies by Olson et al.,14 Oken et al.,15 and Ohlin and Rössner12,13 were conducted primarily among white women followed through 12 months postpartum. Our study fills a gap by presenting outcomes in a racially diverse cohort followed through 24 months after delivery. Additionally, it uses standardized measurements of height, weight, and behavioral risk factors that many observational studies do not.
Materials and Methods
The AMP intervention included 10 physical activity group sessions, 8 healthy eating classes, and 6 telephone counseling sessions over a 9-month period, supplemented by a workbook and an exercise stroller.16 Four hundred fifty overweight or obese women were enrolled between September 2004 and April 2006, recruited from the three largest obstetric clinics and through posters in the Durham, North Carolina, area.
Of the 2821 women prescreened from patient records, 1695 were eligible for screening; 798 of those were reached by phone, 148 refused screening, and 136 did not meet inclusion criteria. Interested women were met by study staff at their 6-week postpartum appointment (baseline), where height and weight were measured using a Seca portable stadiometer and Tanita BWB-800 digital scale. Eligible women had a measured BMI of ≥25, were at least 18 years of age, and were English literate. Medical records were reviewed to confirm the absence of any medical condition which might preclude participation.18,19 Of the 514 who signed the study consent form, 64 did not complete the baseline assessments and were not randomized.
The study was approved by the Duke University Medical Center Institutional Review Board.
Predictor variables
Data collected at baseline (6 weeks postpartum) included age, race (dichotomized here as African American vs. other), marital status (married/living with partner vs. other), parity, education (high school or less, some college, college graduate), self-reported prepregnancy weight and self-reported gestational weight gain (weight at birth was later derived by adding the latter two). Whether the woman had been pregnant or delivered a subsequent child at any time during the follow-up period was also recorded. A brief food frequency questionnaire (FFQ), adapted from one used by the North Carolina Women's, Infants', and Children's (WIC) program,20 was used to assess intake of fruits, vegetables, chips and French fries, fast food, sodas, other sweetened beverages, and milk at baseline and at 12, 18, and 24 months postpartum.
Principal components analysis with varimax rotation was used to reduce the items in the FFQ to a smaller number of food intake factors. Factors were retained if their eigenvalues were at least 1.0, several variable loadings were at least 0.50, and minimum explained variances were at least 10%. For each retained factor, the standardized (mean 0, standard deviation [SD] 1) score was used as a predictor of weight change in the subsequent analyses. This analysis resulted in a two-factor solution, a pattern consistent when tested across each time point. Each item loaded ≥0.50 on only one of the two factors, final communalities ranged from 0.32 to 0.64, and the total explained variance was 46%. Servings of soda, sweetened drinks, French fries and chips, fast food, and serving size of soda/sweet drinks loaded strongly on the first component, whereas servings of milk, fruit, and vegetables loaded strongly on the second. Therefore, we term the first component the “junk food” score, as it is most strongly influenced by the consumption of unhealthy foods, and the second component the “healthy food” score.
Questions assessing physical activity, adapted from the Behavioral Risk Factor Surveillance System (BRFSS),21 were asked at baseline and at 12, 18, and 24 months. Number of days per week of moderate or vigorous activity (such as brisk walking, bicycling, or anything causing increases in breathing or heart rate) was used as the primary physical activity measure.
At baseline, women reported their current breastfeeding status (full breastfeeding, breastfeeding and formula feeding [mixed feeding], or formula feeding only). At 12 months postpartum, women reported how their infants were fed during each month of life: full breastfeeding, mixed feeding, or formula feeding only. Amount of breastfeeding was summarized by a lactation score, a measure of breastfeeding intensity combining the duration and exclusivity of breastfeeding.22 A value was assigned for each month: 0 if formula fed, 1 if mixed, and 2 if fully breastfed (total score range 0–24). The resulting score has a possible range of 0–24, and more explanatory power than a simple measure of duration. For women not seen at 12 months, breastfeeding report from baseline was used. Women reporting formula feeding only were assigned a score of 0, assuming that they would not be initiating lactation after fully formula feeding. Women reporting full breastfeeding or mixed feeding were not included in the analysis, as we could not determine when the infants were weaned. Other researchers22,23 have used this type of assessment of breastfeeding in examining predictors of weight change during the postpartum period. At 12 months, women were also asked if they were using contraception and if so, which type; women were categorized as using hormonal contraception (oral contraceptives, contraceptive patch, Depo-Provera, or Nuvaring) or not.
Because weight change is influenced by food intake and physical activity across time (i.e., thoughout the follow-up period rather than at one point in time), each woman's food intake and physical activity predictors were created as follows. For the outcome of weight change from baseline to 12 months, food intake and physical activity were calculated as the mean of their baseline and 12-month values. For weight change from baseline to 18 months, they were calculated as the mean of all values except that of 24 months. For weight change from baseline to 24 months, they were calculated as the mean of all four values.
Outcome
At 12, 18, and 24 months postpartum, all participants were again weighed by study personnel. For this analysis, the primary outcomes are weight change (kg) from baseline to each of the follow-up time points.
Analyses
Each woman contributed up to four weight values (baseline and 12, 18, and 24 months postpartum). Women missing one or more follow-up weights still contributed nonmissing weights to the primary analyses. If a woman was pregnant or had delivered another baby <60 days before any follow-up, the weight at that point was excluded (the first 2 months after delivery are often associated with retention of fluids and generally elevated weights).24
As the primary analysis (denoted the covariate-adjusted analysis), a single repeated measures mixed linear model with a random intercept term was used to model weight change from baseline to each of the three follow-up time points, simultaneously, as a function of the entire set of predictors. Thus, in this model, follow-up time was a repeated measure. Predictors included baseline weight, treatment arm, age, race, education, marital status, parity, gestational weight gain, height, lactation score, food intake, physical activity, and contraceptive use. All predictors were kept in the model regardless of their p value, as recommended by Harrell.25 Statistical tests of interest from this model included the association of each predictor with weight change at all of the three times simultaneously (a 3 degree of freedom [df] global test) and with weight change at each of the three times separately (a 1 df test). In secondary covariate-unadjusted analyses, each predictor was tested in its own separate mixed model, controlling only for baseline weight; the tests of interest were the association of each predictor with weight change at each of the three times separately (1 df test).
Associations of weight change with each predictor were presented in two ways. First, we displayed covariate-unadjusted weight change from baseline to each of the follow-up time points, according to categories of the predictors. For purposes of presentation only, the following categories were made. Prepregnancy BMI was categorized according to National Heart, Lung and Blood Institute (NHLBI) guidelines26: (1) overweight (BMI 25–29.9), (2) obese I (BMI 30–34.9), (3) obese II (BMI 35–39.9), or (4) obese III (BMI of 40+). Gestational weight gain was categorized according to the Institute of Medicine (IOM) guidelines.27 The IOM suggests a weight gain between 15 and 25 pounds for women who are overweight (based on their BMI before pregnancy) and 11–20 pounds for women who are obese. Second, using the regression coefficients from the repeated measures mixed model described above, we presented mean covariate-adjusted weight change due to a unit change in the predictor of interest. As a sensitivity analysis, we fit a model excluding any women who became pregnant again at any time during the follow-up period.
Because of the large number of analyses, p values are presented as descriptive rather than inferential statistics. However, tests with two-sided p<0.05 are singled out for closer scrutiny. All analyses were performed using SAS 8.2 (Cary, NC).
Results
The number of women included in the weight change analysis at each time point varied as a result of subsequent pregnancies in addition to those who were lost-to-follow-up. At 12 months postpartum, 315 women were included in the analysis, 323 at 18 months, and 348 at 24 months. The analysis sample was 45% African American and relatively well educated, although 21% had a high school diploma or less (Table 1). Most women had a baseline BMI≥30 (weight 88.8±18.5 kg, height 163.8±6.4 cm) and gained in excess of the 2009 IOM recommendations for gestational weight gain.27
Table 1.
Sample Characteristics
| Variable | %(n)a |
|---|---|
| Age, years, mean, (SD) | 30.9 (5.6) |
| 18–24 | 14.2 (64) |
| 25–34 | 55.8 (251) |
| 35+ | 30.0 (135) |
| Race | |
| White | 52.7 (237) |
| African American | 45.1 (203) |
| Other | 2.2 (10) |
| Education | |
| High school graduate or less | 20.7 (93) |
| Some college | 24.4 (110) |
| College degree | 54.9 (247) |
| Marital status | |
| Unmarried | 20.4 (92) |
| Married/cohabitating | 79.6 (358) |
| Parity | |
| One child | 41.1 (185) |
| Two children | 36.0 (162) |
| Three or more children | 22.9 (103) |
| Baseline weight, kg, mean (SD) | 88.8 (18.5) |
| Baseline height, cm, mean (SD) | 163.8 (6.4) |
| Body mass index, kg/m2, mean (SD)25 | 33.0 (6.4) |
| 25–29.9 (overweight) | 40.0 (180) |
| 30–34.9 (obese class I) | 31.3 (141) |
| 35–39.9 (obese class II) | 15.6 (70) |
| 40+ (obese class III) | 13.1 (59) |
| Gestational weight gain, kg, mean (SD)24 | 14.9 (8.7) |
| Below IOM recommendations | 19.6 (88) |
| Within IOM recommendations | 20.8 (93) |
| Above IOM recommendations | 59.6 (267) |
| Study arm | |
| Control | 50.0 (225) |
| AMP intervention | 50.0 (225) |
| Pregnancy since baseline (at 24 months) | |
| No | 82.2 (346) |
| Yes | 17.8 (75) |
| Physical activity (at 12 months, mean (SD) | 3.5 (1.8) |
| <1 day per week | 6.2 (24) |
| 1–4 days per week | 66.9 (259) |
| 5–7 days per week (meet ACSM guideline)26 | 26.9 (104) |
| Lactation score (at 12 months), mean (SD) | 8.2 (8.7) |
| 0 | 33.8 (140) |
| 1–5 | 15.7 (65) |
| 6–11 | 16.9 (70) |
| 12–17 | 14.5 (60) |
| 18–24 | 19.1 (79) |
| Hormonal contraception (at 12 months) | |
| No | 74.3 (271) |
| Yes | 25.7 (94) |
Measured at baseline, except where noted.
Presented as %(n), except where noted.
AMP, Active Mothers Postpartum; ASCM, American College of Sports Medicine; IOM, Institute of Medicine; SD, standard deviation.
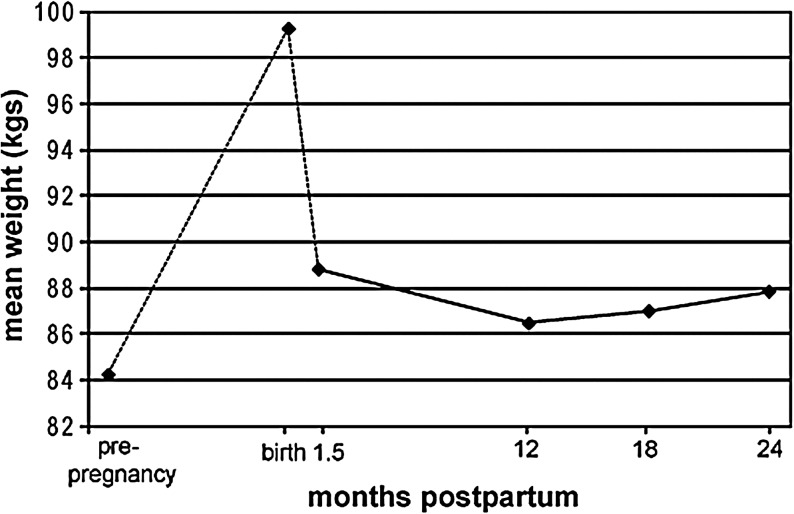
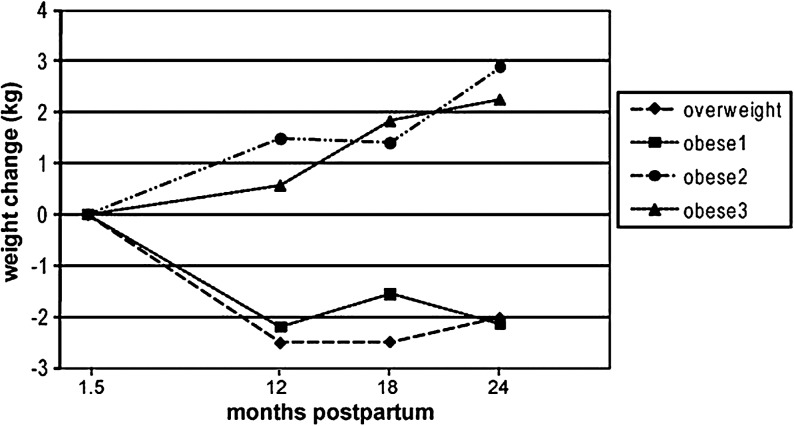
Figure 1 shows the trajectory of mean weight change over time. Figure 2 shows weight change by BMI category. The women retained on average 3.8 kg (SD 8.8) at 24 months postpartum compared to their weights before conception (Fig. 1). When analyzed by BMI category,26 there was a clear difference in weight change from 6 weeks postpartum to the follow-up time points between the lowest BMI categories (overweight, obesity class I) and the highest categories (obesity classes II and III), with the former experiencing a mean weight loss, and the latter having equally sizable weight gains.
FIG. 1.
Average maternal weight change from prepregnancy to 24 months postpartum.
FIG. 2.
Body mass index category (at 6 weeks postpartum) and weight change during the postpartum period.
As shown in the covariate-unadjusted means in Table 2, women who were older (≥25), white, living with a partner, or more educated (having obtained a college degree) were more likely to lose weight postpartum. Women with the lowest baseline BMIs (overweight category) and women who exceeded their recommended gestational weight gain (anything over the IOM guideline based on their prepregnancy BMI) lost more weight after delivery than those who were in any of the obese BMI classes or those who were within or below the IOM weight gain guidelines. Participants with lower junk food and higher healthy food scores, more days of physical activity, longer duration of breastfeeding, and use of hormonal contraception experienced greater postpartum weight loss.
In the repeated measures mixed model (Table 3) (n=397), having a college degree, lower baseline weight, greater gestational weight gain, lower junk food intake, and more physical activity remained associated with weight loss regardless of time point (the p value for the 3 df global test of association was <0.05 for all except education). At selected time points, having a partner also remained associated with weight loss (the 3 df global test of association was <0.05 for partner status). The 1 df effects of race, age, having a higher healthy food intake, breastfeeding, and hormonal contraception that had p values <0.05 when controlling only for baseline weight were mitigated in the repeated measures mixed model that controlled for all predictors. After controlling for all other predictors, women with three or more children lost more weight than women with fewer children. The effect of baseline weight tended to diminish over time, whereas the effects of height and junk food intake tended to increase. The results from the sensitivity analysis that excluded all women who became pregnant again at any time during follow-up were very similar to those from the primary analysis (results not shown).
Discussion
Although there was no statistically significant intervention effect on weight change at any time point,17 there was broad variability in postpartum weight change in this sample of overweight and obese women. Relative to weight at 6 weeks after delivery, mean weight change at each time point was within 0.5–3 kg but ranged from a 21.5 kg loss to a 24.5 kg gain by 24 months postpartum. This pattern and range of postpartum weight change are consistent with other observational studies of postpartum weight retention.1,2,14,15,28,29 Although mean weight retention was modest, 29% of the women in our sample retained ≥5 kg at 24 months postpartum. On average, the women in our study did not return to their prepregnancy weights, and most of their postpartum weight loss occurred within 6 weeks of delivery (Fig. 1).
Weight retained postpartum was positively associated with baseline weight and negatively associated with gestational weight gain at all time points in both the covariate-adjusted and unadjusted analyses. Maternal age and race were associated with weight change at each time point in the unadjusted analyses, but these effects were mitigated in the covariate-adjusted analysis. The effect of living with a partner remained significant in the covariate-adjusted model (at the 18 and 24 month points). The association with marital status has been found elsewhere16 and suggests that single women are at higher risk for long-term pregnancy-related weight retention.
Our study measures weight change beginning at 6 weeks postpartum. A significant part of weight change up to this point represents a natural return to prepregnancy physical status, that is, a loss of retained fluid and other products of pregnancy, whereas weight change after this point is more likely to represent change in accumulated fat stores. In our sample, much of the observed weight loss occurred before 6 weeks postpartum, and for each additional kilogram of weight gained during pregnancy, <0.2 kg was lost from 6 weeks to 24 months postpartum. Further, it is notable that the more obese women were at 6 weeks, the less weight they lost by 24 months; in fact, obese women in classes II and III were likely to gain weight in this period (Fig. 2). Our data suggest that for obese women, pregnancy and the postpartum period compound their obesity problem. This is consistent with the findings of Gunderson et al.,7 who showed that overweight and obese women experienced similar weight loss to normal weight women at 6 weeks postpartum but did not continue to lose and even gained weight in the late (median 2 years) postpartum period. They concluded that these later changes in weight explained heavier women's greater postpartum weight retention.
Although our intervention had limited effect on potentially modifiable behavioral risk factors including diet and physical activity,17 these factors were associated with postpartum weight change. Although an early study by Boardley et al.5 found no such associations, more recent studies support the conclusion that modifiable risk factors do contribute to postpartum weight change. In a study of 540 women, Olson et al.14 found that women who reported exercising often (as compared to never, p=0.03) and eating a lot less over the previous 6 months (as opposed to no change, p=0.008) retained significantly less weight at 12 months postpartum. Among 902 women enrolled in the longitudinal Project Viva, Oken et al.15 found that several behaviors reported at 6 months were independently associated with weight retention at 12 months postpartum. Women who watched less than 2 hours of television daily, walked at least 30 minutes, and consumed trans fats below the median had an odds ratio (OR) of 0.23 (95% confidence interval [CI] 0.08-0.66) of retaining ≥5 kg.15 In our study, both a low junk food score (minimal fast food and soda) and a high healthy food score (high fruit, vegetable, and milk intake) affected postpartum weight loss, although limiting junk food appeared to have a more sizable effect than increasing fruit and vegetables.
Schauberger et al.30 followed a cohort of women to a mean of 8.5 years postpartum. Although they found no effect of physical activity or breastfeeding on weight change at 6 months postpartum in this cohort, both behaviors were associated with reduced weight retention at long-term follow-up.31 Linné et al.32 recontacted their sample 15 years postpartum and did not find an effect of diet or physical activity but did find that breastfeeding after the index pregnancy was associated with reduced weight retention at long-term follow-up. Although there is a substantial effect of breastfeeding in the covariate-unadjusted analysis, this is mitigated in the covariate-adjusted analysis. This is a common finding; the effect of breastfeeding is in general found to be positive but small and easily confounded with other variables, including caloric intake.33–35
Hormonal contraception was associated with greater weight loss in unadjusted analyses at 24 months, but this relationship was only borderline significant (p=0.06) in the adjusted analysis. Although data regarding the effects of hormonal contraception on weight have varied, Berenson and Rahman36 recently followed a cohort of women using oral contraceptives, depot medroxyprogesterone acetate (DMPA), or nonhormonal methods for up to 3 years. Women using DMPA gained more weight compared to women in the other two groups, and women using oral contraceptives actually lost weight at 12 and 24 months while those using nonhormonal methods gained weight at each time point. The potential benefit of hormonal contraception on weight loss warrants further investigation.
Study strengths include the relatively large sample, good representation of both white and African American women, a long (24 month) follow-up period, and good follow-up rates. Furthermore, the study had standardized, objective measurements of weight (at four times points) and height as well as information on behavioral risk factors, which many observational studies do not.13–15 This study did not collect gestational age, which is a limitation, as we could not adjust gestational weight gain calculations for gestational age.
Implications
The perinatal period is one of substantial weight change and retention for women of all weights, but particularly for overweight and obese women. Furthermore, postpartum weight change is associated with behavioral risk factors, such as diet and physical activity, that are modifiable and, therefore, suitable targets for behavioral intervention. Our intervention showed a modest, nonsignificant effect on weight by 12 months, which was not sustained by 24 months. The intervention was relatively elaborate for a public health strategy (in contrast to a clinical strategy), and most participants found it difficult to engage with the intervention in the first year postpartum. Those who did engage in the program, however, lost more weight than those who did not.17 The risk factors associated with this weight gain are to a large extent the same factors that make it more difficult to engage in a formal intervention postpartum, namely, being single or having less education (suggesting less support and fewer financial resources). Our results emphasize the importance of this period in obese women's lives for additional weight gain and the importance of weight control interventions in the postpartum period. Based on the experience with AMP, however, we believe that community-based interventions delivered outside the home are unlikely to impact postpartum weight loss, and more accessible programs delivered in the home via telephone, mail, or internet/e-mail may be more feasible for postpartum women and, therefore, more successful.17
Conclusions
Women who are obese before pregnancy and after birth are at great risk of gaining even more weight in the 2 years after delivery. We found that two modifiable weight-related factors, namely, reduced junk food and increased physical activity, are predictors of postpartum weight loss. The multiple physiologic, psychologic, and social changes taking place in the lives of new mothers theoretically constitute a teachable moment for healthy lifestyle changes,16 although development of suitable public health interventions that can fit seamlessly into their busy lives remains a challenge.17
Acknowledgments
We thank Dr. Laura Fish and Dr. Margaret Savoca for helpful advice regarding principal components analysis, Dr. Colleen McBride, Dr. Lori Bastian, Dr. Miriam Morey, and Ms. Rebecca Brouwer for their involvement in the development of the Active Mothers Postpartum study, and Ms. Marissa Stroo for helpful editing and preparation assistance.
The trial through which these data were collected is registered with ClinicalTrials.gov (NCT00212251).
Disclosure Statement
No competing financial interests exist.
References
- 1.Gunderson EP. Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 1999;21:261–275. doi: 10.1093/oxfordjournals.epirev.a018001. [DOI] [PubMed] [Google Scholar]
- 2.Gore SA. Brown DM. West DS. The role of postpartum weight retention in obesity among women: A review of the evidence. Ann Behav Med. 2003;26:149–159. doi: 10.1207/S15324796ABM2602_07. [DOI] [PubMed] [Google Scholar]
- 3.Viswanathan M. Siega-Riz AM. Moos M-K, et al. (Prepared by RTI International–University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016.) AHRQ Publication No. 08-E-09. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Outcomes of maternal weight gain, Evidence Report/Technology Assessment No. 168. [Google Scholar]
- 4.Parker JD. Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81:768–774. [PubMed] [Google Scholar]
- 5.Boardley DJ. Sargent RG. Coker AL, et al. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86:834–838. doi: 10.1016/0029-7844(95)00283-W. [DOI] [PubMed] [Google Scholar]
- 6.Smith DE. Lewis CE. Caveny JL, et al. Longitudinal changes in adiposity associated with pregnancy—The CARDIA study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 7.Gunderson EP. Abrams B. Selvin S. Does the pattern of postpartum weight change differ according to pregravid body size? Int J Obes. 2001;25:853–862. doi: 10.1038/sj.ijo.0801631. [DOI] [PubMed] [Google Scholar]
- 8.Dewey KG. Cohen RJ. Brown KH, et al. Effects of exclusive breastfeeding for four versus six months on maternal nutritional status and infant motor development: Results of two randomized trials in Honduras. J Nutr. 2001;131:262–267. doi: 10.1093/jn/131.2.262. [DOI] [PubMed] [Google Scholar]
- 9.Dewey KG. Heinig MJ. Nommsen LA. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr. 1993;58:162–166. doi: 10.1093/ajcn/58.2.162. [DOI] [PubMed] [Google Scholar]
- 10.Baker JL. Gamborg M. Heitmann BL, et al. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr. 2008;88:1543–1551. doi: 10.3945/ajcn.2008.26379. [DOI] [PubMed] [Google Scholar]
- 11.Amorim AR. Linne YM. Lourenco PM. Diet or exercise, or both, for weight reduction in women after childbirth. Cochrane Database Syst Rev. 2007;3:CD005627. doi: 10.1002/14651858.CD005627.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Ohlin A. Rössner S. Trends in eating patterns, physical activity and socio-demographic factors in relation to postpartum body weight development. Br J Nutr. 1994;71:457–470. doi: 10.1079/bjn19940155. [DOI] [PubMed] [Google Scholar]
- 13.Rössner S. Ohlin A. Pregnancy as a risk factor for obesity: Lessons from the Stockholm Pregnancy and Weight Development Study. Obes Res. 1995;3(Suppl 2):267s–275s. doi: 10.1002/j.1550-8528.1995.tb00473.x. [DOI] [PubMed] [Google Scholar]
- 14.Olson CM. Strawderman MS. Hinton PS, et al. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int J Obes Relat Metab Disord. 2003;27:117–127. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 15.Oken E. Taveras EM. Popoola FA, et al. Television, walking, and diet: Associations with postpartum weight retention. Am J Prev Med. 2007;32:305–311. doi: 10.1016/j.amepre.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Østbye T. Krause KM. Brouwer RJN, et al. Active Mothers Postpartum (AMP): Rationale, design and baseline characteristics. J Womens Health. 2008;17:1567–1575. doi: 10.1089/jwh.2007.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Østbye T. Krause KM. Lovelady CA, et al. Active Mothers Postpartum (AMP): A randomized controlled weight loss intervention trial. Am J Prev Med. 2009;37:173–180. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wing RR. Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- 19.American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Exercise during pregnancy and the postpartum period. ACOG Committee Opinion No. 267. Obstet Gynecol. 2002;99:171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 20.www.fns.usda.gov/wic/ www.fns.usda.gov/wic/
- 21.National Center for Chronic Disease Prevention and Health Promotion. Behavioral Risk Factor Surveillance System. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. www.cdc.gov/brfss/ www.cdc.gov/brfss/
- 22.Ohlin A. Rössner S. Maternal body weight development after pregnancy. Int J Obes. 1990;14:159–173. [PubMed] [Google Scholar]
- 23.Baker JL. Gamborg M. Heitmann BL. Lissner L. Sorensen TI. Rasmussen KM. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr. 2008;88:1543–1551. doi: 10.3945/ajcn.2008.26379. [DOI] [PubMed] [Google Scholar]
- 24.Butte NF. Ellis KJ. Wong WW. Hopkinson JM. Smith EO. Composition of gestational weight gain impacts maternal fat retention and infant birth weight. Am J Obstet Gynecol. 2003;189:1423–1432. doi: 10.1067/s0002-9378(03)00596-9. [DOI] [PubMed] [Google Scholar]
- 25.Harrell FE. Regression modelling strategies with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 26.National Heart, Lung and Blood Institute. Obesity Education Initiative Expert Panel. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH publication No. 98-4083. National Institutes of Health. 1998.
- 27.Institute of Medicine. Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 28.Linné Y. Barkeling B. Rössner S. Long-term weight development after pregnancy. Obes Rev. 2002;3:75–83. doi: 10.1046/j.1467-789x.2002.00061.x. [DOI] [PubMed] [Google Scholar]
- 29.Schmitt NM. Nicholson WK. Schmitt J. The association of pregnancy and the development of obesity—Results of a systematic review and meta-analysis on the natural history of postpartum weight retention. Int J Obes (Lond) 2007;31:1642–1651. doi: 10.1038/sj.ijo.0803655. [DOI] [PubMed] [Google Scholar]
- 30.Schauberger CW. Rooney BL. Brimer LM. Factors that influence weight loss in the puerperium. Obstet Gynecol. 1992;79:424–429. doi: 10.1097/00006250-199203000-00020. [DOI] [PubMed] [Google Scholar]
- 31.Rooney BL. Schauberger CW. Excess pregnancy weight gain and long-term obesity: One decade later. Obstet Gynecol. 2002;100:245–252. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- 32.Linné Y. Dye L. Barkeling B. Rössner S. Weight development over time in parous women—The SPAWN study—15 years follow-up. Int J Obes Relat Metab Disord. 2003;27:1516–1522. doi: 10.1038/sj.ijo.0802441. [DOI] [PubMed] [Google Scholar]
- 33.Dewey KG. Heinig MJ. Nommsen LA. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr. 1993;58:162–166. doi: 10.1093/ajcn/58.2.162. [DOI] [PubMed] [Google Scholar]
- 34.Ip S. Chung M. Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess. 2007;153:1–186. [PMC free article] [PubMed] [Google Scholar]
- 35.Winkvist A. Rasmussen KM. Impact of lactation on maternal body weight and body composition. J Mammary Gland Biol Neoplasia. 1999;4:309–318. doi: 10.1023/a:1018706131168. [DOI] [PubMed] [Google Scholar]
- 36.Berenson AB. Rahman M. Changes in weight, total fat, percent body fat, and central-to-peripheral fat ratio associated with injectable and oral contraceptive use. Am J Obstet Gynecol. 2009;200:329.e1–329.e8. doi: 10.1016/j.ajog.2008.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]