Abstract
Background and aims
Muscular pain in the facial region is the most common cause of facial pains. Myofascial pain dysfunction syndrome (MPDS) is one of the most important facial muscle disorders comprising of signs and symptoms including pain during function, tenderness in the muscles of mastication and restricted jaw movement. Due to the lack of an accepted therapeutic approach, the purpose of this paper was to find an effective treatment to decrease the pain of such patients. Considering the analgesic and anti-inflammatory action of laser therapy, the effects of low level laser (Ga-Al-As) in the treatment of MPDS patients referred to Tehran University of Medical Sciences Faculty of Dentistry, were investigated in the present study.
Materials and methods
This study was a quasi-experimental research. Twenty-two MPDS patients were selected from those referred to Department of Oral Medicine, Tehran University of Medical Sciences Faculty of Dentistry. Clinical examination was performed at six stages in the following order: prior to the treatment, at 2 and 4 weeks after treatment, and monthly thereafter for a 3-months follow-up. All patients underwent low-level laser therapy for 4 weeks (12 sessions). Variables such as pain severity, pain of cheek region, pain frequency, tenderness of masticatory muscles, click, and mouth opening were evaluated at each stage. Numerical variables were investigated using Analysis of Variance test for repeated measures whereas ranking variables were studied by non-parametric Kruskal-Wallis test.
Results
At the end of treatment period, pain severity, pain of cheek region, pain frequency, tenderness of masseter, temporalis, medial pterygoid, and lateral pterygoid muscles showed significant improvement as compared with the commencement of any treatment which continued during the 3-months post-treatment (p<0.05).
Conclusion
It was shown that low-level laser (Ga-Al-As) therapy had the efficacy to alleviate pain and decrease the tenderness of masticatory muscles among MPDS patients through a continuous and regular therapeutic program.
Keywords: Low-level laser therapy, muscle tenderness, myofascial pain dysfunction syndrome, pain
Introduction
Myofascial pain dysfunction syndrome (MPDS) is the most common cause of facial pains. Patients with MPDS suffer from pain, restricted jaw movement and__ masticatory muscle tenderness. Psychological factors, occlusion imbalance and para-functional habits are mentioned as its most important underlying causes.1 Some investigators have suggested the patients’ psychological status as a predisposing factor for this syndrome and attributed a major role to stress in the incidence of bruxism disorder which in turn leads to masticatory muscles spasm.1 Occlusion imbalance serves as an accelerating factor in MPDS pathogenesis leading to more para-functional habits.
In order to eliminate the signs and symptoms of MPDS, both mental and physical treatments are necessary.1 Conservative treatments are generally useful to alleviate pain and dysfunction. Dentists employ different methods such as medicine therapy, occlusal splints, biofeedback, and physiotherapy in the treatment of this condition.1
Modern dentistry utilizes low-level lasers in tissue healing acceleration, pain alleviation, reducing inflammation and physiotherapy in the orofacial region. Gur2, Venanciorde3, Nunez4 and Dundar5 have shown that low-level laser plays an important role in the treatment of most musculofacial disorders and facial pain alleviation. The purpose of this study was to evaluate the effects of low-level laser (Ga-Al-As) on MPDS patients.
Materials and Methods
This was a quasi-experimental or interventional study due to the presence of a single group. Repeated measurements were conducted based on a time series method. Patients were selected from those referred to Departments of Oral Medicine, and Temporomandibular Joint (TMJ), Tehran University of Medical Sciences Faculty of Dentistry (2000-2001).
Admission criteria included a diagnosis of MPDS based on at least two of the following symptoms:1
Dull pain in the facial region
One or more masticatory muscles’ tenderness
Mandibular restriction or deviation upon mouth opening
Patients were checked for systemic diseases and none suffered from acute MPDS, degenerative joint disorders, chronic pain of head and face resulted from psychologic and neurologic disorders, along with vascular, dental or auricular lesions.
Relaxant, anti-inflammatory and sedative drugs had not been taken repeatedly by patients since one month prior to the treatment. Para-clinical examinations such as MRI and panoramic radiography were employed to differentiate MPDS from other diseases, if necessary. Patients were admitted to the study on the basis of an informed consent and had the authority to refrain from the treatment at any desired stage. Maximum sample size was calculated to be 12 people following the pilot study. A total of 28 patients were entered into this study, six of whom discontinued the treatment leaving twenty-two to be treated and followed-up.
All patients were examined clinically and the related information was recorded in their files. Clinical examinations were performed at six stages in the following order: prior to the treatment, at the end of 2-week trial period (mid-treatment), at the end of 4-week trial period (end of treatment), and monthly thereafter for a 3-month follow-up.
At each stage, clinical examination included the determination of pain location (temporal region, cheek, temporomandibular joint, neck), pain frequency (periodic, continuous), pain severity (based on visual analogue scale “VAS”), joint sound, the degree of mouth opening (by direct measurement of vertical distance between the cutting edge of upper and lower incisors), the degree of mandibular protrusion (horizontal distance between the cutting edge of upper and lower incisors), and muscle tenderness (masseter, temporal, medial pterygoid, lateral pterygoid, neck).
Patients underwent low-level Ga-Al-As laser therapy (Endolaser 456, wavelength = 780 mm) for 4 weeks (Figure 1).
Figure 1.
Endolaser 456 device.
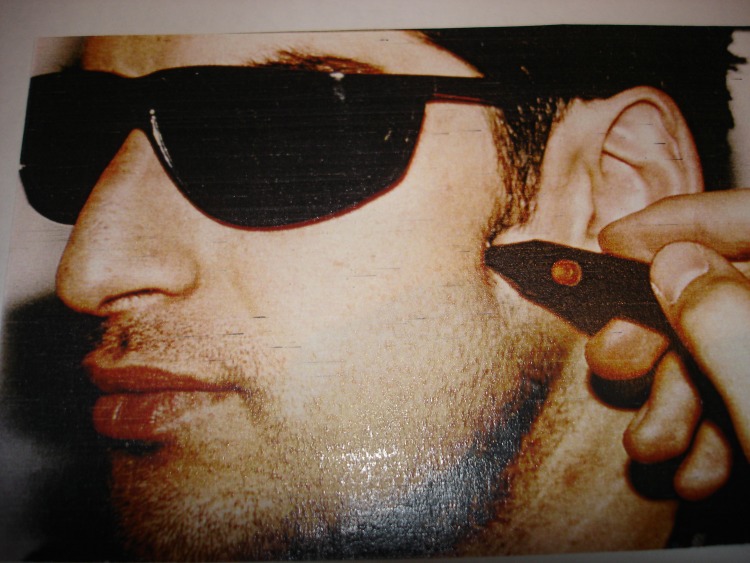
Therapeutic dose was 1200 milli-joules for each affected region. To alleviate pain, each region was initially radiated for 60 seconds, 10 milliwatts and 73 Hertz, then to reduce inflammation it was radiated for another 60 seconds, 10 milliwatts and 80 Hertz (Figure 2).
Figure 2.
The manner of laser radiation to extra-oral points.
Patients referred every other day for 12 sessions. At the twelfth session, the applied dose was reduced to half. 6
Considering that definite treatment is performed during 3-6 months following the elimination of signs and symptoms,7 these patients were referred to specialists after a 3-month follow-up. Numerical variables were investigated using Analysis of Variance test for repeated measures,8 whereas ranking variables were studied by non-parametric Kruskal-Wallis test.9
Results
The 22 studied patients (mean age=33.32) included 16 females and 6 males who were affected with this disorder for 14 months on average. Pain severity (p = 6.79 × 10-12), tenderness of temporalis (p = 5.84 × 10-5), masseter (p = 9.05 × 10-6), medial pterygoid (p = 2.87 × 10-5) and lateral pterygoid (p = 2.09 × 10-4) muscles decreased significantly at the end of treatment compared with the commencement to any treatment and this significant improvement continued up to 3 months post-treatment.
Variable such as mouth opening, mandibular protrusion, and tenderness of neck muscles, joint sound, temporomandibular joint pain, neck and temporal pain did not show any significant improvement. Alterations in the decrease of pain severity during therapeutic visits were considerable (Table1).
Table 1. Mean and median indices, standard deviation and variances of significant level of pain severity according to VAS.
| Descriptive Indices / Variable | Distribution | Range | Variance | Median | Mean |
| Pain severity (first stage) | % 91 | 2 - 10 | 4.12 | 6 | 6.14 |
| Pain severity (second stage) | % 13 | 1 - 8 | 3.59 | 5 | 4.45 |
| Pain severity (third stage) | % 34 | 0 - 8 | 4.32 | 3 | 2.68 |
| Pain severity (fourth stage) | % 61 | 0 - 9 | 5.27 | 2 | 2.68 |
| Pain severity (fifth stage) | % 58 | 0 - 8 | 4.99 | 2 | 2.68 |
| Pain severity (sixth stage) | % 45 | 0 - 7 | 4.55 | 2 | 2.5 |
Discussion
The sex ratio (16 females to 6 males) was in agreement with previous studies on MPDS as Sola reported its prevalence among females and males to be 55% and 45%, respectively10. Higher number of females, in this study, may be attributed to their more cooperation and attention to health compared to males.
The longest duration of MPDS problems was 24 months while the shortest was 6 months, with the average of 14 months. The results showed that the use of low-level laser (Ga-Al-As) in MPDS patients significantly decreased pain severity (p<0.0001), pain frequency (p=5.39×10-6), cheek pain (p=6.79×10-12), tenderness of temporalis (p=5.84×10-5), masseter (p=9.05×10-6), medial pterygoid (p=2.87×10-5) and lateral pterygoid (p=2.09×10-4) muscles at the end of treatment period compared to the commencement of any treatment and continued during the 3-months post-treatment.
The degree of mouth opening, mandibular protrusion, neck muscles’ tenderness on palpation, joint sound, pain of head, neck and TMJ region did not show statistically significant improvements.
Considering that pain severity has been the only variable showing significant improvement between the first and second measurements, it can be concluded that a decrease in pain severity is the first effect implemented by low laser therapy.
At the beginning of treatment, all patients showed a periodic or consistent pain whereas at the end of the sixth stage of measurement, more than half (54%) were completely pain free.
Some possible causes of pain decrease through low-level laser radiation can be summarized as hyperpolarization of neuron cell membrane and increasing stimulation threshold along with an increase in the secretion of morphine substances such as Encephalin and Endorphin which have an analgesic and anti-inflammatory action.11
Considering the theory that trigger points are caused by their inflammatory nature,6 it can be concluded that laser radiation leads to decrease of edema, inflammation and pain through reducing inflammatory products such as prosthoglandine (PGE2), prosthocycline, histamine, and kinine.12
Bian and Yu showed that the stimulation of acupuncture points by Ga-As low-level laser could cause an analgesic effect and an increase in pain threshold. Following venouse injection of Naloxan, they observed that the analgesic effect of laser radiation on acupuncture points was removed and concluded that pain relief could be due to a substance analogues to narcotics released from acupuncture points that its effects were removed due to Naloxon.1
On the other hand, Melzalc showed that in 71% of cases, trigger points superimposed on acupuncture points.14 According to the mentioned studies, one of the possible mechanisms for pain improvement, observed in this study, can be related to the superimposition of trigger point on acupuncture points and their stimulation by low-level laser radiation.
Although pain gate control theory may explain a part of laser analgesic effects during therapeutic visits of MPDS patients,6 the consistency of anti-pain effects during follow-ups, at fourth and fifth stages, is not justifiable.
Such a consistency can be attributed to the more removal of inflammatory and painful factors, improvement of muscle functions, decrease in painful muscle spasms and better employment of masticatory system.
An improvement in all muscles’ tenderness was observed in this investigation. One exception was the neck muscle that can be due to the small sample size.
Changes in the range of opening and protrusive movements did not reveal any statistically significant improvement which could be related to structural changes in the affected muscles and the creation of muscles taut bonds10 that prevents these muscles from lengthening. Non-significant changes of opening-protrusive movements could be explained by the absence of mechanical intervention such as muscle stretching.
Additionally, limitations in opening-protrusive movements can be attributed to capsular tightness seen in chronic disorders15and the absence of any increase in such movements can be due to the absence of mechanical interventions such as stretching and mobilization techniques.
Significant pain improvement in cheek region can be attributed to the more painful points existing in this region and significant decrease in the muscles’ tenderness such as masseter, medial pterygoid and lateral pterygoid is an indicative of significant treatment changes in this region. The degree of pain improvement in the temporal region was not significant, however, its p-value was fairly near the significant threshold. Low prevalence of disorder in the temporal region and probable pain circulation from TMJ can be reasoned for this observation, although temporal tenderness was significantly decreased.
The absence of pain improvement in TMJ region probably resulted from TMJ abnormal biomechanics as well as induced stresses on capsular and ligament structures leading to local pains in TMJ. Due to the absence of any mechanical intervention in this study, the presence of pain in TMJ region, even after treatment period, is justified.
The absence of any improvement in pain and tenderness in neck region may be due to the small sample size (six patients had neck pain and five showed tenderness in neck muscles). Joint sound did not show any significant improvement due to the small sample size and no mechanical intervention as well. Considering that mostly no significant differences were observed between the first and second stages of treatment and significant changes were found since the third stage, it can be concluded that some of the low-level laser effects do not appear in the early visits and the completion of treatment period is necessary, as confirmed by other reports.6
Conclusion
The most important findings of the present study are as follow:
Low-level laser therapy on MPDS patients’ trigger points requires a regular and precise program and the completion of treatment period is crucial in improving the situation.
The application of low-level laser reduces pain and masticatory muscles’ tenderness among MPDS patients; however, in order to maintain these therapeutic effects, the elimination of etiologic factors is essential.
Low-level laser therapy can not by itself, eliminate restricted TMJ movements and joint sound in MPDS patients. Simultaneous utilization of other appropriate treatments is recommended.
Pain and sensitivity of neck region, apart from laser therapy, require interventions such as correction of head and neck position.
Acknowledgments
We are indebted to Mr. Mahyar Salavati for the statistical consultation of this article.
References
- 1.Lynch M, Brightman V. Burket’s Oral Medicine. 9th ed. Philadelphia: JB Lippincott; 1994. 312-14,327-28 [Google Scholar]
- 2.Gur A, Sarac AJ, Cevik R, Altindag O, Sarac S. Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: a double-blind and randomize-controlled trial. Lasers Surg Med. 2004;35:229–35. doi: 10.1002/lsm.20082. [DOI] [PubMed] [Google Scholar]
- 3.Venanciorde A, Camparis C, Lizarerellirde F. Low intensity laser therapy in the treatment of temporomandibular disorders. Oral Rehabil. 2005;32:800–7. doi: 10.1111/j.1365-2842.2005.01516.x. [DOI] [PubMed] [Google Scholar]
- 4.Nunez SC, Garcez AS, Suzuki SS, Ribeiro MS. Management of mouth opening in patients with temporomandibular disorders. Photomed Laser Surg. 2006;24:45–9. doi: 10.1089/pho.2006.24.45. [DOI] [PubMed] [Google Scholar]
- 5.Dundar U, Eucik D, Samli F. The effect of gallium arsenide aluminum laser therapy in the treatment of temporomandibular joint disorders. J Cli Rhematol. 2006;33:229–35. [Google Scholar]
- 6.Michlovitz S. Thermal Agents in Rehabilitation. 2nd ed. Philadelphia: F.A. Davis; 1990. 22,34,200-12 [Google Scholar]
- 7.Kaplan A, Assael L. Temporomandibular Disorder, Diagnosis and Management. Philadelphia: Saunders; 1992. 550 [Google Scholar]
- 8.Steel RGD, Torrie JH. Principles and Procedures of Statistics. 2nd ed. New York: Mc Grow-Hill; 1980. 172-91 [Google Scholar]
- 9.Daniel W. Biostatistics Foundation for Analysis in the Heath Sciences. 6th ed. New York: John Wiley; 1995. 598-607 [Google Scholar]
- 10.Simons D, Travell J. Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. 12-13,70 [Google Scholar]
- 11.Saxen MA. Myofascial pain syndrome: characteristic, diagnosis and treatment. J Indiana Dent Assoc. 1998;77:9–12. [PubMed] [Google Scholar]
- 12.Cernavin I, Pugatschew A. Laser application in dentistry: a review of the literature. Aust Dent J. 1994;39:28–32. doi: 10.1111/j.1834-7819.1994.tb05543.x. [DOI] [PubMed] [Google Scholar]
- 13.Bian XP, Yu ZQ. The experiment studies of semi conductor Ga-As laser points irradiation the analgesic effect. J Pain. 1989;43:181–5. [PubMed] [Google Scholar]
- 14.Melzak R. Trigger points and acupuncture points for path: correlations and implications. Pain. 1979;3:3–23. doi: 10.1016/0304-3959(77)90032-X. [DOI] [PubMed] [Google Scholar]
- 15.Kessler R, Hertling D. Management of Common Musculoskeletal Disorders. 5th ed. Philadelphia: JB Lippincott; 1996. 444-45 [Google Scholar]