Abstract
Study Objectives:
To investigate the prevalence and predictors of RLS in Hispanics of Mexican descent (HMD) and non-Hispanic whites (NHW).
Design:
A population-based random digit dialing telephone questionnaire.
Setting:
San Diego County California
Participants:
1,754 HMD and 1,913 NHW adults ≥ 18 years of age able to participate in a telephone interview in English or Spanish.
Interventions:
None.
Measurements and Results:
RLS was defined by the presence of all 4 criteria of the International Restless Legs Study Group. Sleepiness was measured by the Epworth Sleepiness Scale. Acculturation was evaluated using the Short Acculturation Scale for Hispanics. Risk factors for RLS were by self-report. The survey was conducted in the subject's language of choice. RLS prevalence was significantly lower in HMD than in NHW (14.4% vs.18.3%, p = 0.002). High acculturation HMD had a significantly greater RLS prevalence than the low acculturation group (17.4% vs. 12.8%, p = 0.008). Predictors of RLS varied between HMD and NHW. Female gender (OR 1.40, 95% CI 1.04, 1.90, p = 0.027), smoking (OR 1.82, 95% CI 1.27, 2.61, p = 0.001), and acculturation (OR 1.47, 95% CI 1.10, 1.97, p = 0.009) were independent predictors of RLS in HMD, while only older age (OR 1.01, 95% CI 1.0, 1.02) was an independent predictor of RLS for NHW.
Conclusion:
The prevalence of RLS was significantly lower in HMD than in NHW, and significantly greater in high acculturation HMD. Our data suggest that risk factors for RLS vary by race/ethnicity and acculturation is an independent risk for RLS in HMD.
Citation:
Sawanyawisuth K; Palinkas LA; Ancoli-Israel S; Dimsdale JE; Loredo JS. Ethnic differences in the prevalence and predictors of restless legs syndrome between Hispanics of Mexican descent and non-Hispanic whites in San Diego county: a population-based study. J Clin Sleep Med 2013;9(1):47-53.
Keywords: Restless legs syndrome, prevalence, ethnicity, acculturation, Hispanics of Mexican descent, non-Hispanic whites
Restless legs syndrome (RLS) has been described as a sensorimotor disorder of sleep-wake motor regulation.1 RLS, a major contributing factor to disturbed sleep, is characterized by the urge to move the legs due to a dysesthesia often described as creepy crawly sensations, occurring during periods of repose or rest, more pronounced in the evening, and completely or nearly completely resolved with movement.2,3 The severity and frequency of RLS can range from occasional mild symptoms to nearly constant and severely disruptive symptoms that can also involve the arms and torso and can severely impair daytime functioning and sleep.1,4 Restless legs syndrome is a clinical diagnosis that is determined by applying the four diagnostic questions of the International Restless Legs Syndrome Study Group,2,3 either by a face-to-face interview or a telephone interview.5 The etiology of RLS is unclear; however, disturbances of dopamine and iron metabolism and genetic predisposition have been implicated,6,7 and RLS has been associated with peripheral neuropathy, diabetes, iron deficiency, smoking, spinal cord injuries, pregnancy, Parkinson disease, older age, end-stage renal disease, and the use of some antidepressants.8–14
The prevalence of RLS reported in international epidemiological studies has varied widely from as low as 0.4% to 15% among the general population; however, the most often quoted range is from 5% to 15%.5,8,15,16 In a large epidemiological study that included 15,391 participants from the United States, France, Germany, Italy, Spain, and the United Kingdom, the overall prevalence of RLS utilizing the four-question criteria was 7.2%.5 However, in specific populations the prevalence has been substantially higher, with as many as 18.4% of hemodialysis patients and 31.2% of women during the third trimester of pregnancy reporting RLS.9,13
BRIEF SUMMARY
Current Knowledge/Study Rationale: There is a paucity of information on the relationship of ethnicity and RLS, and this relationship has not been systematically evaluated in Hispanics living in the U.S. The aim of this study was to compare the prevalence and determinants of RLS in Hispanics of Mexican descent and non-Hispanic whites living in the United States.
Study Impact: The prevalence and risk factors for RLS vary by race/ethnicity, and acculturation to the U.S. is an independent risk for RLS in Hispanics of Mexican descent.
Only a few epidemiological studies have assessed the racial/ethnic differences in the prevalence and determinants of RLS. In data from the 2005–2006 National Health and Nutrition Examination Survey, the physician-diagnosed prevalence of RLS in Hispanics was 0.1%, as compared to 0.5% for whites, 0.4% for blacks, and 0.7% for others. However, the low rates for all groups suggest a high likelihood of underdiagnosis of this condition, which would disproportionately affect ethnic minorities due to lack of access to health care.16 In the REST (RLS Epidemiology, Symptoms, and Treatment) study, the prevalence of RLS in Spain was 4.9%, as compared to 8.6% in the United Kingdom and 7.6% in the United States.5
The aim of this study was to compare the prevalence and determinants of RLS in Hispanics of Mexican descent (HMD) and non-Hispanic whites (NHW) living in the United States in San Diego County. To our knowledge this is the first large epidemiological study evaluating RLS in Mexican Americans.
MATERIALS AND METHODS
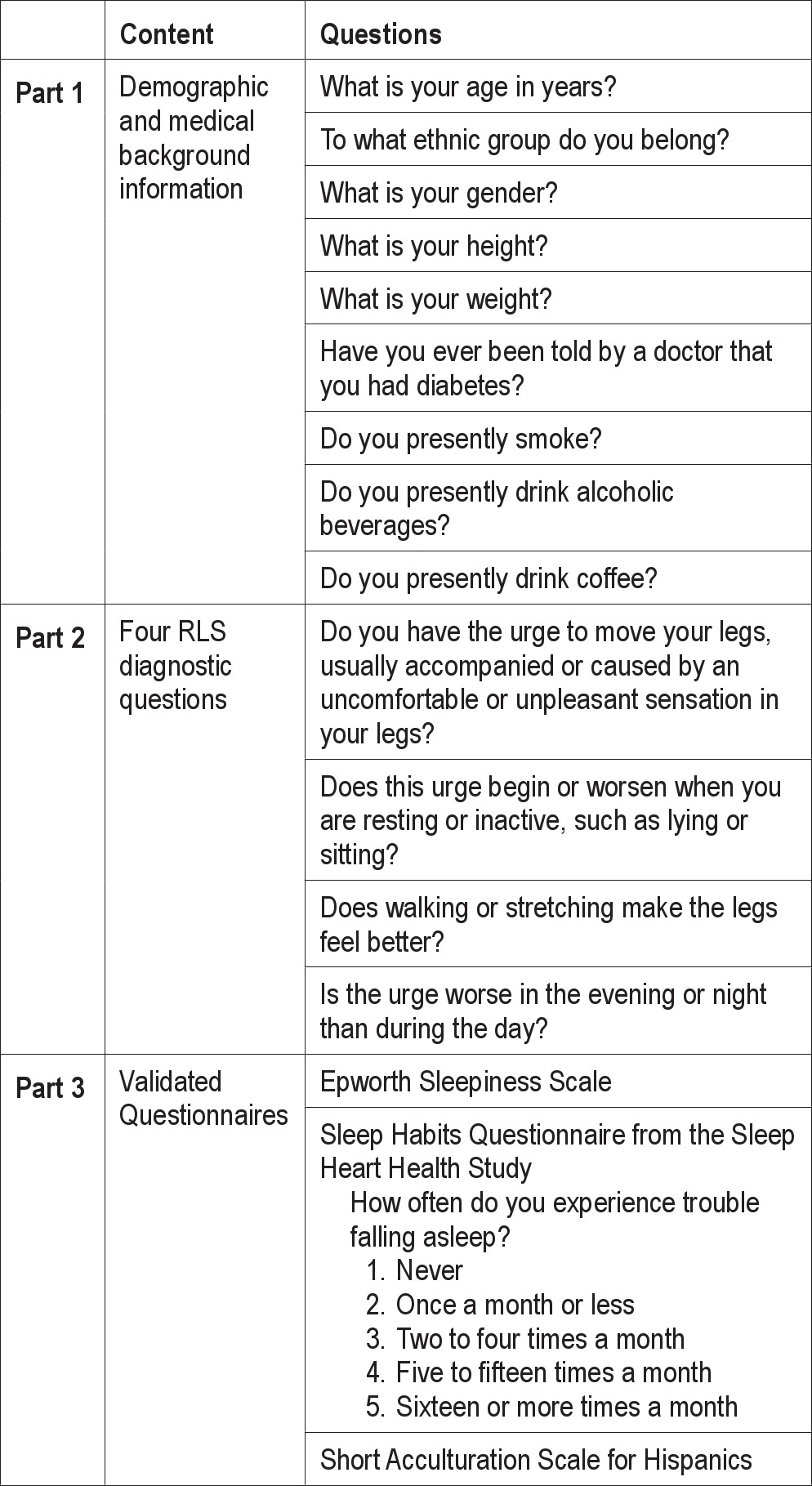
The Sleep Health and Knowledge in US Hispanics Project, was a large population-based survey conducted in San Diego County from January 2007 to September 2009. Adult (age ≥ 18 years) HMD and NHW men and women capable of participating in a telephone interview in English or Spanish were recruited. Recruitment was conducted by trained culturally competent telephone interviewers from the California Survey Research Services, Inc. (Van Nuys, CA) by random digit dialing utilizing a computer assisted telephone interview system. In order to adjust for the racial/ethnic distribution of the San Diego County population, zip codes with higher concentrations of Mexican Americans were oversampled to achieve a quota for HMD of 50% of the sample population. Once a qualifying household was identified, a randomization procedure was utilized to recruit one adult participant per household. Participants were asked to complete a questionnaire consisting of 3 parts (Table 1): (1) collection of background demographic and medical information, (2) the 4 diagnostic questions for RLS,2,3 (3) and questionnaires including the Epworth Sleepiness Scale (ESS)17 and the Sleep Habits Questionnaire from the Sleep Heart Health Study.18 The Short Acculturation Scale for Hispanics19 was used to measure acculturation in HMD. The scale consists of 12 items assessing language use (English, Spanish, or both), media (English, Spanish, or both), and ethnic social relations (Hispanics, Americans, or both). A 5-point Likert scale is used for each question with a possible response from 1-5, and the scores are averaged. Scores ≤ 2.99 are categorized as low acculturation, and scores > 2.99 are classified as high acculturation.19
Table 1.
Summary of the Sleep Health and Knowledge in US Hispanics Questionnaire: RLS
The diagnosis of RLS was defined by the presence of all 4 essential criteria by the International Restless Legs Study Group.2,3 The 4 diagnostic questions of the International Restless Legs Syndrome Study Group2,3 were translated into Spanish using the translation and blinded back-translation method by 3 bilingual culturally competent Mexican American medical professionals who were long-term residents of San Diego. The 4 questions were further refined in conjunction with culturally competent bilingual interviewers from the California Survey Research Services after a small telephone interview pilot trial before the study was started. Since then, the RLS criteria have been translated into Spanish by others and validated in Hispanic populations.20,21 The Spanish version of the ESS and the Short Acculturation Scale for Hispanics have been validated in Hispanic populations.19,22,23 The Spanish version of the Sleep Heart Health Study Sleep Habits Questionnaire was used in 296 Hispanics.24 Information was gathered on previously recognized risk factors for RLS including history of diabetes, hypertension, age, female gender, BMI, smoking, and use of alcohol and coffee.8,–27 All subjects were given the choice to answer the questionnaires in their language of preference (English or Spanish). The protocol was approved by the University of California, San Diego Human Research Protection Program.
Statistical Analyses
The analysis focused primarily on descriptive and Chi-Square statistics to compare RLS prevalence between HMD and NHW. Student t-tests were used to compare means. Multivariate logistic regression was employed to evaluate independent predictors of RLS for each ethnic group. When comparing prevalence of RLS, groups were stratified by age and gender. A p-value ≤ 0.05 was considered a significant result. The IBM SPSS Statistics 20.0 software package was used to perform the statistical calculations.
RESULTS
Sample Characteristics
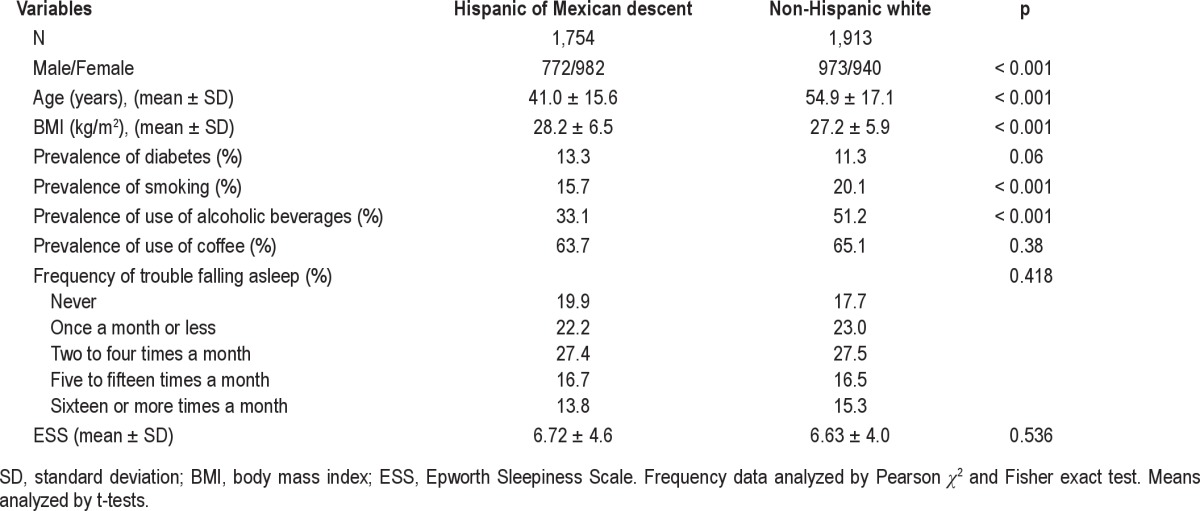
A total of 149,552 phone numbers were randomly dialed, from which 14,162 (9.5%) were working numbers of households that responded and showed interest in participating in the telephone survey. Of these, 10,495 (74%) were not qualified to participate because no one in the household was HMD or NHW or over quota for NHW in 59 cases. The rest, 3,667 (1,754 HMD and 1,913 NHW) completed the telephone survey. Approximately one-fourth of the subjects, all HMD, chose to answer the questionnaires in Spanish. Table 2 provides the subjects’ characteristics and potential risk factor for RLS by ethnicity. The male-to-female participation ratio was approximately 1:1 for NHW and 1:1.27 for HMD. On average, HMD were significantly younger than NHW by almost 15 years (41.0 ± 15.6 vs. 54.9 ± 17.1 years, p < 0.001); body mass index was in the overweight range for both ethnic groups, but HMD were significantly heavier (BMI 28.2 ± 6.5 vs. 27.2 ± 5.9, p < 0.001). The prevalence of smoking and alcohol use was significantly lower in HMD. Hispanics had a greater prevalence of diabetes mellitus. There were no ethnic differences in reported difficulties falling asleep, excessive daytime sleepiness, or use of coffee.
Table 2.
Subject characteristics and prevalence of risk factors for restless legs syndrome
Prevalence of RLS
The prevalence of RLS in the entire sample was 16.5%. When examined by ethnicity, the prevalence was significantly lower in HMD than in NHW (14.4% vs.18.3%, p = 0.002). The high acculturation HMD group had significantly higher prevalence of RLS than the low acculturation group (17.4% vs. 12.8%, p = 0.008). The prevalence of RLS in the high acculturation HMD group was not significantly different from that of the NHW (17.4% vs. 18.3%, p = 0.637).
To control for the age difference between HMD and NHW in our sample population and the known gender difference in RLS prevalence, subjects were divided as younger (ages 18 to 47) and older (ages 48 to 94) based on the median age for the entire population. Figure 1 depicts the prevalence of RLS in HMD and NHW by age and gender. In general, older men and older women had higher prevalence of RLS regardless of ethnicity. Younger HMD men had significantly lower prevalence of RLS than younger NHW men (10.9% vs. 14.9%; Pearson χ2 2-sided, p = 0.068; Fisher exact test, 1-sided, p = 0.043). The prevalence of RLS in older men and in women was not different regardless of ethnicity.
Figure 1. Prevalence of restless legs syndrome by ethnicity, age, and gender.
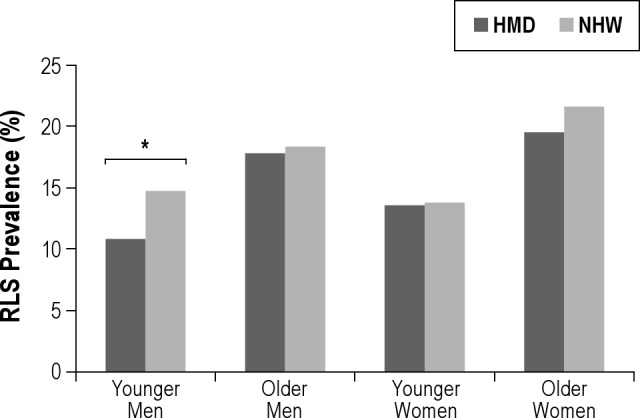
The RLS prevalence was significantly lower in HMD than in NHW (14.4% vs.18.3%, p = 0.002). Younger HMD men* (age 18 to 47 years) had significantly lower prevalence of RLS than younger NHW men (10.9% vs. 14.9%; Pearson χ2 2-sided, p = 0.068; Fisher exact test, 1-sided, p = 0.043). The prevalence of RLS was not different in older men and women regardless of ethnicity.
Figure 2 depicts the prevalence of RLS by acculturation and by age and gender. Overall, highly acculturated HMD had significantly higher prevalence of RLS when compared to the low acculturated subjects (17.4% vs. 12.8%, p = 0.008). However, when controlling for age and gender, the low acculturation younger men had a significantly lower prevalence of RLS than the high acculturation younger men (7.4% vs. 15.4%, p = 0.003). There was also a large difference in the prevalence of RLS in the low acculturated older men as compared to highly acculturated older men (15.1% vs. 23.3%), but this was not statistically significant (p = 0.147).
Figure 2. Prevalence of restless legs syndrome by acculturation, age, and gender.
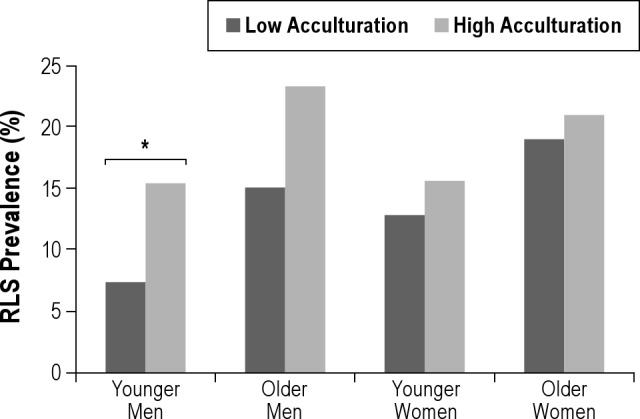
The high acculturation HMD group had significantly higher prevalence of RLS when compared to the low acculturation group (17.4% vs. 12.8%, p = 0.008). The low acculturation younger men* had significantly lower prevalence of restless legs syndrome (7.4% vs. 15.4%) than the high acculturation younger men (Pearson χ2, 2-sided, p = 0.003). There was also a large difference in the RLS prevalence of the low and high acculturation older men, but this was not statistically significant (p = 0.147).
Predictors of RLS
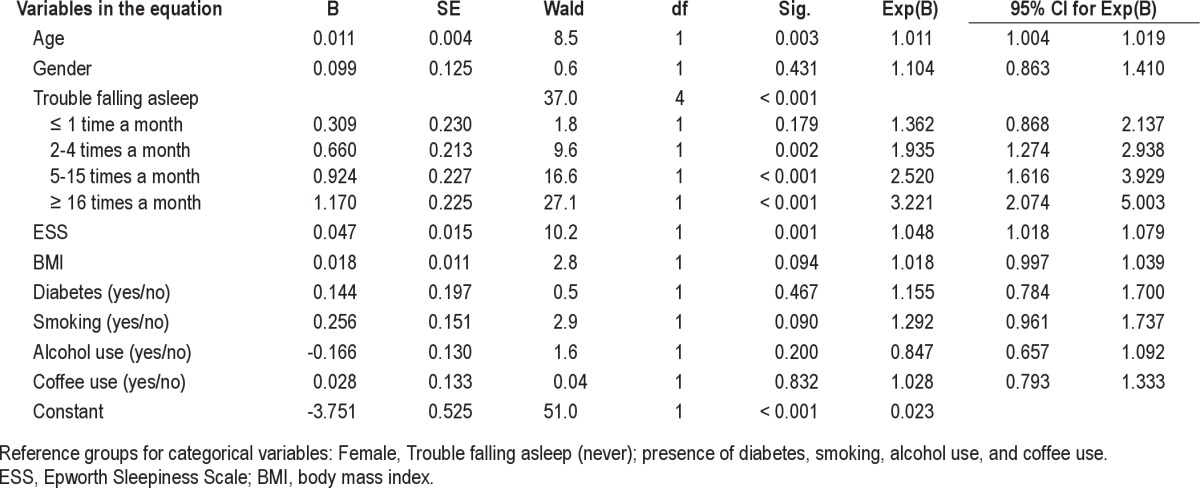
We compared potential predictors of RLS by ethnicity using multivariate logistic regression analyses. In HMD (Table 3), being female (p = 0.027), trouble falling asleep ≥ 2 nights per month (p < 0.001), higher ESS score (p < 0.001), smoking (p = 0.001), and high acculturation (OR 1.47, 95% CI 1.10, 1.97, p = 0.009) were independent predictors of RLS. Having trouble falling asleep was the strongest predictor of RLS with OR ranging from 2.42 (95% CI 1.49, 3.94, p < 0.001) for difficulty falling asleep 2-4 nights a month to an OR of 2.82 (95% CI 1.66, 4.79, p < 0.001) for difficulty falling asleep ≥ 16 nights a month. In NHW (Table 4), increasing age, trouble falling asleep ≥ 2 nights per month and higher ESS score were predictors of RLS (p ≤ 0.003), again with trouble falling asleep the strongest predictor.
Table 3.
Logistic regression analysis: predictors of restless legs syndrome in Hispanics of Mexican descent
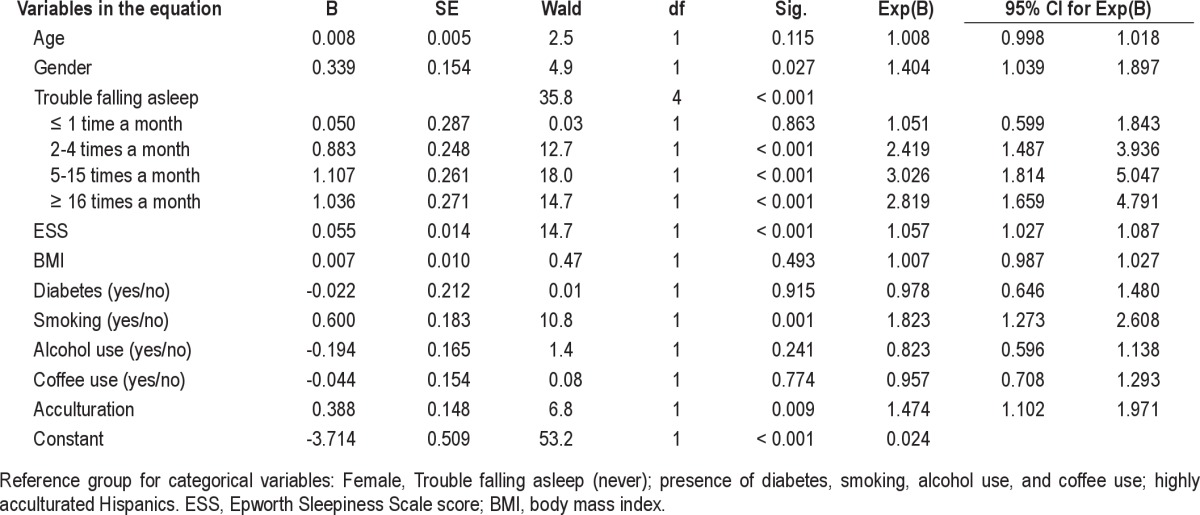
Table 4.
Logistic regression analysis: predictors of restless legs syndrome in non-Hispanic whites
DISCUSSION
To our knowledge, this is the largest epidemiological study directly evaluating the prevalence of RLS in HMD living in the United States. Our data show that RLS prevalence was significantly lower in HMD than in NHW and significantly higher in high acculturation HMD. Acculturation was an independent risk factor for RLS after controlling for a number of other potential risk factors.
Prevalence of RLS
The overall RLS prevalence of 16.5% found in the current study was higher than previously reported in the general US population. The current study used similar methodology as the study by Allen et al., who reported a much lower RLS prevalence for the US (7.6%). Allen et al. recruited a heterogeneous study sample population designed to represent a cross-section of the US.5 In comparison, we recruited homogenous populations for both HMD and NHW in San Diego County. The homogeneity of our study populations could account for the higher RLS prevalence we observed. This assertion is supported by a validation study of the four diagnostic RLS questions performed in a rural population of mostly white subjects in Idaho where the RLS prevalence was reported at 24%,28 which is comparable to the prevalence of 18.3% we observed in the white population in San Diego County. Comparable to the prior reports, we found higher RLS prevalence in women and in older subjects for both HMD and NHW.5,8,28 The constraints of this epidemiological study did not allow for methodology to screen out RLS mimics or cases of secondary RLS which could have affected the observed RLS prevalence.29,30
Ethnic Differences in RLS Prevalence
We found a significantly lower prevalence of RLS in HMD as compared to NHW in San Diego County, which appeared to be driven primarily by a lower RLS prevalence in younger HMD men (Figure 1). We found no studies investigating the prevalence of RLS in Mexicans in the US for comparison. However, there are a few studies evaluating the prevalence of RLS in South America. One study reported an RLS prevalence of 2% in native South Americans living in the costal and mountainous regions of Ecuador. Those living at higher altitude had a slightly higher RLS prevalence of 3.2%,20 but well below the RLS prevalence of 5 to 15% reported for populations of European ancestry.5,8,15,16 A more recent study reported an RLS prevalence of 20.2% in Buenos Aires, Argentina, where the Hispanic population is predominantly of European descent.28 The RLS prevalence we observed in HMD living in San Diego County is higher than the very low RLS prevalence reported for South American Native populations,20 and lower than the RLS prevalence reported for homogeneous populations of European descent living in North and South America.28,31 The majority of Mexicans are a mixture of Native American and European white ancestry which could account for the mid-range RLS prevalence we observed in the current study. Our findings and those of the available literature suggest that the prevalence of RLS may vary depending on the specific population and the homogeneity of the population in question.
Age-gender stratification of the sample population suggested that differences in RLS prevalence were primarily driven by a lower prevalence of RLS in younger HMD males. We found no other comparable report in the RLS literature to suggest possible mechanisms or hypotheses for this interesting observation. Stratification inevitably lowers statistical power, which could potentially make this observation unstable. More investigation is needed to clarify what is truly driving the lower prevalence of RLS we found in HMD with studies adequately powered to target various age-gender groups and potential risk factors in a much larger sample population.
Acculturation and Prevalence of RLS
We found that HMD with high acculturation had significantly higher RLS prevalence than those with low acculturation; similar to the relationship we observed between HMD and NHW, this difference appeared to be driven primarily by a low RLS prevalence in the low acculturation younger men group (Figure 2). Also, the RLS prevalence of the high acculturation group was of similar magnitude to that of the NHW (Figure 1). Acculturation to the US has long been associated with changes in the health status of Hispanic immigrants, including increased rates of obesity,32,33 diabetes,32,34 cardiovascular disease,35,36 psychiatric disorders,37,38 and abnormal sleeping habits.39,40 These acculturation related health changes have been attributed to changes in diet,41 increases in alcohol and tobacco use,42– limited access to health services,46 low socioeconomic status,47 and the stress associated with sociocultural change and change in social status.37,38,48
It is possible that the higher prevalence of RLS in highly acculturated HMD we observed was the result of the stress associated with sociocultural change and change in social status often experienced by Hispanic immigrants.37,38,48 Restless legs syndrome has been associated with increased stress. Cancer patients afflicted by RLS had significantly higher levels of anxiety and depression, and poorer quality of life.49 In Koreans, having RLS was associated with depression and anxiety disorders50; in uremic patients, increased anxiety levels was an independent predictor of RLS.51 We are unable to explain from our data why only men, primarily younger men, had lower RLS prevalence than younger women, as would be suggested by previously reported higher prevalence of RLS in women.5,8,28 Further investigation is needed.
Ethnic Differences in RLS Risk Factors
In our sample population, predictors of RLS differed between HMD and NHW. In both groups the strongest independent risk factors for a diagnosis of RLS was difficulty falling asleep two nights or more per month (Tables 3 and 4). Excessive daytime sleepiness was a weaker predictor in both groups. These findings most likely represent markers of RLS, since RLS is commonly clinically associated with difficulty falling asleep due to the urge to move the legs, especially in the evening while in repose,2,3 and complaints of reduced daytime functioning, increased sleepiness, and reduced quality of life.52–55 In a report by Allen et al., difficulty falling asleep was the second most frequent complaint of patients with RLS.5
However, for HMD, female gender and smoking were independent risk factors for RLS (Table 3) while for NHW only older age was an independent risk factor (Table 4), suggesting a difference in ethnic susceptibility for RLS. Our findings are consistent with prior studies showing that gender is a predictor of RLS that varies depending on the population studied. Phillips et al. reported that gender was not a predictor of RLS in a sample of whites from Kentucky,8 similar to our findings with NHW in San Diego County. However, others have shown that being female is a risk factor for RLS,56,57 similar to our findings for HMD.
Older age has been a predictor of RLS in many studies.2,8,28 However, in our study, older age was an independent predictor of RLS only for NHW. Older age has been associated with higher prevalence of RLS; as suggested by Phillips et al., RLS may follow a model of chronic disease with a variable age of onset.8 This may explain why age was not a predictor in our HMD population, which was on average almost 15 years younger than NHW.
A potentially important finding was the association of smoking with a diagnosis of RLS only in HMD, suggesting that HMD may be more sensitive to the effects of tobacco (Table 3). It is unlikely that smoking had a protective effect for RLS in NHW since smoking has been shown to be an independent predictor of RLS in several studies of white populations.8,55 A limitation of the current study was our determination of smoking status by a single dichotomous question, which did not allow us to evaluate the effect of never smoking versus ex and current smoking, and light and heavy smoking on the prevalence of RLS.
Finally, acculturation to the US life style was an independent predictor for a diagnosis of RLS (Table 3). Acculturation of Hispanics to the US lifestyle has been well documented to increase the rates of metabolic disorders, cardiovascular disease, psychiatric disorders and stress, and poor health habits that could increase the risk of RLS.32–48 Further research is warranted to determine why acculturation is an independent risk factor for RLS in HMD that would include stress and anxiety levels, nutritional factors such as iron deficiency and ferritin levels, and the degree of smoking as potential risk factors.
Study Limitations
The current study is somewhat limited by the methodology which is intrinsic to a large epidemiological telephone survey with limited time for ample questioning. We took a careful systematic approach when administering the 4 essential diagnostic criteria of RLS. However, methodology to exclude RLS mimics29,30 was not available during data collection for this study. Therefore, our study most likely included cases of secondary RLS and RLS mimics, which could potentially affect the prevalence of RLS noted in both HMD and NHW. We did not collect supportive criteria or associated features of RLS to bolster the strength of the RLS diagnosis, which also constitutes a major limitation of this study. Also, we were not able to determine if there was an ethnic propensity to false positive RLS mimics. The study population was limited to HMD and NHW making the findings difficult to generalize to other race/ethnic groups or potentially even other Hispanic populations living in the US.
CONCLUSION
In conclusion, the prevalence of RLS was significantly lower in HMD than in NHW and significantly greater in high acculturation HMD. Our data suggest that risk factors for RLS vary by race/ethnicity and acculturation to the US lifestyle is an independent risk factor for RLS in HMD. Further investigation is warranted to determine how acculturation affects RLS prevalence in HMD.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Work for this study was performed at the University of California, San Diego School of Medicine. This work was supported by the following grants: NIH R01 HL075630, UL1RR031980 (CTRI), NIH M01 RR00827.
REFERENCES
- 1.Hening WA. Restless legs syndrome: a sensorimotor disorder of sleep/wake motor regulation. Curr Neurol Neurosci Rep. 2002;2:186–96. doi: 10.1007/s11910-002-0029-y. [DOI] [PubMed] [Google Scholar]
- 2.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology: a report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 3.Walters AS International Restless Legs Syndrome Study Group. Toward a better definition of the restless legs syndrome. Mov Disord . 1995;10:634–42. doi: 10.1002/mds.870100517. [DOI] [PubMed] [Google Scholar]
- 4.Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini-Strambi L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med . 2004;5:237–46. doi: 10.1016/j.sleep.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–92. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 6.Trotti LM, Bhadriraju S, Rye DB. An update on the pathophysiology and genetics of restless legs syndrome. Curr Neurol Neurosci Rep . 2008;8:281–7. doi: 10.1007/s11910-008-0044-8. [DOI] [PubMed] [Google Scholar]
- 7.Earley CJ, Hyland K, Allen RP. Circadian changes in CSF dopaminergic measures in restless legs syndrome. Sleep Med. 2006;7:263–8. doi: 10.1016/j.sleep.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160:2137–41. doi: 10.1001/archinte.160.14.2137. [DOI] [PubMed] [Google Scholar]
- 9.Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77–83. doi: 10.1097/AOG.0b013e3181c4f8ec. [DOI] [PubMed] [Google Scholar]
- 10.O’Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age Ageing. 1994;23:200–3. doi: 10.1093/ageing/23.3.200. [DOI] [PubMed] [Google Scholar]
- 11.Zucconi M, Ferini-Strambi L. Epidemiology and clinical findings of restless legs syndrome. Sleep Med. 2004;5:293–9. doi: 10.1016/j.sleep.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Memory and Morbidity in Augsburg Elderly. Neurology. 2000;54:1064–8. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 13.Merlino G, Piani A, Dolso P, et al. Sleep disorders in patients with end-stage renal disease undergoing dialysis therapy. Nephrol Dial Transplant. 2006;21:184–90. doi: 10.1093/ndt/gfi144. [DOI] [PubMed] [Google Scholar]
- 14.Rottach KG, Schaner BM, Kirch MH, et al. Restless legs syndrome as side effect of second generation antidepressants. J Psychiatr Res. 2008;43:70–5. doi: 10.1016/j.jpsychires.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Chen NH, Chuang LP, Yang CT, et al. The prevalence of restless legs syndrome in Taiwanese adults. Psychiatry Clin Neurosci. 2010;64:170–8. doi: 10.1111/j.1440-1819.2010.02067.x. [DOI] [PubMed] [Google Scholar]
- 16.Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disordered and sleep habits in the United States. Sleep Breath. 2010;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 17.Johns M. A new method of measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 18.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 19.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a Short Acculturation Scale for Hispanics. Hisp J Behav Sci. 1987;9:183–205. [Google Scholar]
- 20.Castillo PR, Kaplan J, Lin SC, Fredrickson PA, Mahowald MW. Prevalence of restless legs syndrome among native South Americans residing in coastal and mountainous areas. Mayo Clin Proc. 2006;81:1345–7. doi: 10.4065/81.10.1345. [DOI] [PubMed] [Google Scholar]
- 21.García-Borreguero D, Lahuerta-Dal Ré J, Albares J, Zaragoza S, de Gracia M. Validated translation to Spanish of the evaluation questionnaire of patients with restless legs syndrome. Neurologia. 2009;24:823–34. [PubMed] [Google Scholar]
- 22.Chiner E, Arriero JM, Signes-Costa J, Marco J, Fuentes I. Validación de la versión Española del test de somnolencia Epworth en pacientes con síndrome de apnea de sueño. Arch Bronconeumol. 1999;35:422–7. doi: 10.1016/s0300-2896(15)30037-5. [DOI] [PubMed] [Google Scholar]
- 23.Ferrer M, Vilagut G, Monasterio C, Montserrat JM, Mayos M, Alonso J. Measurement of the perceived impact of sleep problems: the Spanish version of the functional outcomes sleep questionnaire and the Epworth sleepiness scale. Med Clin (Barc) 1999;113:250–5. [PubMed] [Google Scholar]
- 24.O’Connor G, Lind B, Lee E, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;1:74–9. [PubMed] [Google Scholar]
- 25.Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res. 2002;53:547–54. doi: 10.1016/s0022-3999(02)00443-9. [DOI] [PubMed] [Google Scholar]
- 26.Al-Jahdali HH, Al-Qadhi WA, Khogeer HA, Al-Hejaili FF, Al-Ghamdi SM, Al Sayyari AA. Restless legs syndrome in patients on dialysis. Saudi J Kidney Dis Transpl. 2009;20:378–85. [PubMed] [Google Scholar]
- 27.Aldrich MS, Shipley JE. Alcohol use and periodic limb movements of sleep. Alcohol Clin Exp Res. 1993;17:192–6. doi: 10.1111/j.1530-0277.1993.tb00747.x. [DOI] [PubMed] [Google Scholar]
- 28.Nichols DA, Allen RP, Grauke JH, et al. Restless legs syndrome symptoms in primary care: a prevalence study. Arch Intern Med. 2003;163:2323–9. doi: 10.1001/archinte.163.19.2323. [DOI] [PubMed] [Google Scholar]
- 29.Benes H, Walters AS, Allen RP, Hening WA, Kohnen R. Definition of restless legs syndrome, how to diagnose it, and how to differentiate it from RLS mimics. Mov Disord. 2007;22(Suppl 18):S401–8. doi: 10.1002/mds.21604. [DOI] [PubMed] [Google Scholar]
- 30.Hening WA, Allen RP, Washburn M, Lesage SR, Earley CJ. The four diagnostic criteria for Restless Legs Syndrome are unable to exclude confounding conditions (mimics) Sleep Med . 2009;10:976–81. doi: 10.1016/j.sleep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Persi GG, Etcheverry JL, Vecchi C, Parisi VL, Ayarza AC, Gatto EM. Prevalence of restless legs syndrome: a community-based study from Argentina. Parkinsonism Relat Disord. 2009;15:461–5. doi: 10.1016/j.parkreldis.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 32.Hazuda HP, Haffner SM, Stern MP, Eifler CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol. 1988;128:1289–301. doi: 10.1093/oxfordjournals.aje.a115082. [DOI] [PubMed] [Google Scholar]
- 33.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29:470–7. [PubMed] [Google Scholar]
- 34.Stern MP, Knapp JA, Hazuda HP, Haffner SM, Patterson JK, Mitchell BD. Genetic and environmental determinants of type II diabetes in Mexican AmericansIs there a descending limb to the modernization/diabetes relationship? Diabetes Care. 1991;14:649–54. doi: 10.2337/diacare.14.7.649. [DOI] [PubMed] [Google Scholar]
- 35.Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988-1994. Am J Public Health. 1999;89:723–30. doi: 10.2105/ajph.89.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crespo CJ, Loria CM, Burt VL. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996;111(Suppl 2):7–10. [PMC free article] [PubMed] [Google Scholar]
- 37.Burnam MA, Hough RL, Karno M, Escobar JI, Telles CA. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. J Health Soc Behav. 1987;28:89–102. [PubMed] [Google Scholar]
- 38.Alderete E, Vega WA, Kolody B, Aguilar-Gaxiola S. Lifetime prevalence of and risk factors for psychiatric disorders among Mexican migrant farmworkers in California. Am J Public Health. 2000;90:608–14. doi: 10.2105/ajph.90.4.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cantero PJ, Richardson JL, Baezconde-Garbanati L, Marks G. The association between acculturation and health practices among middle-aged and elderly Latinas. Ethn Dis. 1999;9:166–80. [PubMed] [Google Scholar]
- 40.Ebin VJ, Sneed CD, Morisky DE, Rotheram-Borus MJ, Magnusson AM, Malotte CK. Acculturation and interrelationships between problem and health-promoting behaviors among Latino adolescents. J Adolesc Health. 2001;28:62–72. doi: 10.1016/s1054-139x(00)00162-2. [DOI] [PubMed] [Google Scholar]
- 41.Bermudez OI, Falcon LM, Tucker KL. Intake and food sources of macronutrients among older Hispanic adults: association with ethnicity, acculturation, and length of residence in the United States. J Am Diet Assoc. 2000;100:665–73. doi: 10.1016/s0002-8223(00)00195-4. [DOI] [PubMed] [Google Scholar]
- 42.Caetano R, Mora ME. Acculturation and drinking among people of Mexican descent in Mexico and the United States. J Stud Alcohol . 1988;49:462–71. doi: 10.15288/jsa.1988.49.462. [DOI] [PubMed] [Google Scholar]
- 43.Markides KS, Krause N, Mendes de Leon CF. Acculturation and alcohol consumption among Mexican Americans: a three-generation study. Am J Public Health. 1988;78:1178–81. doi: 10.2105/ajph.78.9.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marin G, Perez-Stable EJ, Marin BV. Cigarette smoking among San Francisco Hispanics: the role of acculturation and gender. Am J Public Health. 1989;79:196–8. doi: 10.2105/ajph.79.2.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palinkas LA, Pierce J, Rosbrook BP, et al. Cigarette smoking behavior and beliefs of Hispanics in California. Am J Prev Med. 1993;9:331–7. [PubMed] [Google Scholar]
- 46.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982-84. Am J Public Health. 1990;80(Suppl):11–19. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Winkleby MA, Fortmann SP, Rockhill B. Health-related risk factors in a sample of Hispanics and whites matched on sociodemographic characteristics. The Stanford Five-City Project. Am J Epidemiol. 1993;137:1365–75. doi: 10.1093/oxfordjournals.aje.a116646. [DOI] [PubMed] [Google Scholar]
- 48.Espino DV, Maldonado D. Hypertension and acculturation in elderly Mexican Americans: results from 1982-84 Hispanic HANES. J Gerontol. 1990;45:M209–13. doi: 10.1093/geronj/45.6.m209. [DOI] [PubMed] [Google Scholar]
- 49.Ostacoli L, Saini A, Ferini-Strambi L, et al. Restless legs syndrome and its relationship with anxiety, depression, and quality of life in cancer patients undergoing chemotherapy. Qual Life Res. 2010;19:531–7. doi: 10.1007/s11136-010-9614-8. [DOI] [PubMed] [Google Scholar]
- 50.Cho SJ, Hong JP, Hahm BJ, et al. Restless legs syndrome in a community sample of Korean adults: prevalence, impact on quality of life, and association with DSM-IV psychiatric disorders. Sleep. 2009;32:1069–76. [PMC free article] [PubMed] [Google Scholar]
- 51.Takaki J, Nishi T, Nangaku M, et al. Clinical and psychological aspects of restless legs syndrome in uremic patients on hemodialysis. Am J Kidney Dis . 2003;41:833–9. doi: 10.1016/s0272-6386(03)00031-3. [DOI] [PubMed] [Google Scholar]
- 52.Allen RP, Abetz L, Washburn T, Earley CJ. The impact of restless legs syndrome (RLS) on sleep and cognitive function. Eur J Neurol. 2002;9(Suppl 2):50. [Google Scholar]
- 53.Abetz L, Allen R, Follet A, et al. Evaluating the quality of life of patients with restless legs syndrome. Clin Ther. 2004;26:925–35. doi: 10.1016/s0149-2918(04)90136-1. [DOI] [PubMed] [Google Scholar]
- 54.Allen RP, Bharmal M, Calloway M. Prevalence and disease burden of primary restless legs syndrome: results of a general population survey in the United States. Mov Disord. 2011;26:114–20. doi: 10.1002/mds.23430. [DOI] [PubMed] [Google Scholar]
- 55.Benediktsdottir B, Janson C, Lindberg E, et al. Prevalence of restless legs syndrome among adults in Iceland and Sweden: Lung function, comorbidity, ferritin, biomarkers and quality of life. Sleep Med. 2010;11:1043–8. doi: 10.1016/j.sleep.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 56.Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70:35–42. doi: 10.1212/01.wnl.0000287072.93277.c9. [DOI] [PubMed] [Google Scholar]
- 57.Thomas K, Watson CB. Restless legs syndrome in women: a review. J Womens Health (Larchmt) 2008;17:859–68. doi: 10.1089/jwh.2007.0515. [DOI] [PubMed] [Google Scholar]


