Abstract
Study Objectives:
The current study investigated the factor structure of the Pittsburgh Sleep Quality Index (PSQI) among English speaking non-Hispanic whites (NHW) and English and Spanish speaking Hispanics of Mexican descent (HMD).
Design:
The PSQI was administered during a telephone interview. In order to test the factor structure of the PSQI structure across ethnic/language groups, multiple group confirmatory analysis with covariates (MIMIC) was employed. The 1- and 3-factor versions of the PSQI previously reported in the literature were examined.
Setting:
San Diego County.
Participants:
Community-dwelling English speaking, NHW (n = 1,698) and English (n = 654) and Spanish (n = 792) speaking HMD.
Measurement and Results:
A single-factor scoring model fit across language/ethnic groups; however, a 3-factor model provided a better than the 1-factor model in all language/ethnic groups. The subscale sleep medications loaded poorly and was removed from all models.
Conclusion:
Across groups, a 3-factor model of the PSQI more reliably assessed sleep quality than a single-factor global score. Results indicate that the 3-factor structure of the PSQI was uniform across English speaking NHW and English and Spanish speaking HMD.
Citation:
Tomfohr LM; Schweizer CA; Dimsdale JE; Loredo JS. Psychometric characteristics of the Pittsburgh Sleep Quality Index in English speaking non-Hispanic whites and English and Spanish speaking Hispanics of Mexican descent. J Clin Sleep Med 2013;9(1):61-66.
Keywords: Hispanics of Mexican descent, multiple group confirmatory factor analysis with covariates (MIMIC), Pittsburgh Sleep Quality Index, reliability, non-Hispanic whites
Poor sleep quality is associated with the development of numerous physical and psychological health outcomes.1–5 It is important to understand factors that promote and detract from sleep quality in the general population. To date, the extant literature has primary explored the sleep of non-Hispanic whites and to a smaller degree, African Americans, leaving the sleep of other ethnic groups within the United States (US) relatively underexplored.6
The Hispanic population is the fastest growing minority group in the US, with two-thirds being of Mexican descent.7,8 The few sleep studies conducted in Hispanic American populations suggest that some groups may be at an increased risk for sleep complaints and insomnia.9–11 However, investigations in this area have been limited by the lack of ethnically validated measurement tools. Before self-report measures can be compared across ethnic groups, it must be established that the same underlying variable (e.g., sleep quality) is being assessed across the groups. Cross-group measurement equivalence can be established by demonstrating that questions thought to assess the latent variable under study show similar loading patterns onto the factor.12 If an assessment tool is differentially influenced by within group factors other than sleep quality (e.g., response styles), then comparing scores across groups is inappropriate.
BRIEF SUMMARY
Current Knowledge/Study Rationale: The factor analytic solution of the Pittsburgh Sleep Quality Index (PSQI) has been under explored in Spanish and English speaking Hispanics of Mexican descent (HMD), making it difficult to compare PSQI scores between HMD and non-Hispanic Whites (NHW).
Study Impact: Results from this paper suggest that a three-factor solution of the PSQI fit well in Spanish and English speaking HMD and NHW; however the subscale sleep medications fit poorly across groups. Our findings suggest that a truncated version of the PSQI assessed the same three latent variables across language/ethnic groups.
The Pittsburgh Sleep Quality Index (PSQI) is a widely used assessment of sleep quality.13–16 The PSQI inquires about seven domains of sleep difficulties; traditionally, these have been summed into a total score indicating a single factor thought to measure global sleep quality. Since its creation the PSQI has been used to assess sleep quality in a variety of populations and has been translated into multiple languages.17–22 However, the seven component scores that compose the PSQI total have not consistently fit the same factor analytic solution.21–26 Additionally, the reliability of the PSQI has not been examined in the Mexican American population, and to date, there has not been published psychometric data on the use of the PSQI in Spanish and English speaking Hispanics of Mexican descent. We sought to extend the literature in this area, using a confirmatory factor analytic strategy to investigate and compare the factor structure of the PSQI in English speaking, non-Hispanic whites (NHW) and Spanish and English speaking Hispanics of Mexican descent (HMD).
METHODS
Population and Procedure
The Sleep Health and Knowledge in US Hispanics Project, is a population-based survey conducted in San Diego County from January 2007 to September 2009. Adult (age ≥ 18 years) HMD and NHW men and women capable of completing a telephone interview in English or Spanish participated. Recruitment occurred by random digit dialing by trained, bilingual, culturally competent telephone interviewers from the California Survey Research Services, Inc. (CSRS) in Van Nuys, CA, utilizing a computer assisted telephone interview system. In order to adjust for the racial/ethnic distribution of the San Diego County population, zip codes with higher concentrations of HMD were oversampled. Once a qualifying household was identified, a randomization procedure was utilized to recruit only one adult participant per household. After informed consent was obtained over the telephone, participants were asked to complete an extensive questionnaire, which included information about sleep health knowledge, depression, sleepiness, health practices (information to be reported elsewhere), background demographic and sleep habits, and the Pittsburgh Sleep Quality Index (PSQI). Interviews took on average 45 min to complete in English and 52 min in Spanish, and participants received a $25 incentive for their participation in the study. The protocol was approved by the University of California, San Diego Human Research Protection Program.
Participants
A total of 149,552 phone numbers were randomly dialed from which 14,162 (9.5%) households showed interest in participating in the telephone survey. The other randomly dialed numbers were non-households, disconnected, no answer, or no interest in participating. Of the households showing interest in participating, 10,495 (74%) were not qualified to participate because no one in the household was HMD or NHW or over quota for NHW in 59 cases. The rest—3,667 adult subjects (≥ 18 years of age)—completed the telephone survey. We excluded data from subjects who reported logically inconsistent sleep information (e.g., habitual sleep durations > 100% of calculated sleep efficiency or sleeping > 12 h per night). In total, 523 participants were removed from the analysis, including the removal of 10.5% of the NHW group, 17.2% of the English-speaking HMD group, and 17.7% of the Spanish-speaking HMD group. The final sample (N = 3,144) was grouped by ethnicity and language, yielding 3 groups: (1) NHW, English language survey (n = 1,698), mean age of 55.36 years (SD 17.3), 49.4% female; (2) HMD, English language survey (n = 654) mean age 38.8 years (SD 15.3), 53.2% female; and (3) HMD, Spanish language survey (n = 792), mean age 43.9 years (SD 15.9), 61.1% female. The entire sample ranged in age from 18 to 94 years.
Measures
Pittsburgh Sleep Quality Index (PSQI)
Subjective sleep quality over the past month was assessed with the Pittsburgh Sleep Quality Index (PSQI). The PSQI is a 19-item self-report questionnaire composed of 7 subscales: Subjective Sleep Quality, Sleep Latency, Sleep Duration, Habitual Sleep Efficiency, Sleep Disturbances, Use of Sleep Medication, and Daytime Drowsiness.14 Both the English and Spanish versions of the PSQI were available for administration. The PSQI has been translated into Spanish by various authors and validated in Spanish speaking populations in Spain,27 Colombia,28 and Mexico.29 Each translation varies slightly. We chose to use the version by Royuela and Macias,27 and made minor changes to some of the expressions to adapt the instrument to a telephone interview format and to the HMD population in San Diego. Two Spanish-English bilingual Mexican American culturally competent medical personnel who had lived in San Diego for more than 20 years collaborated with culturally competent telephone interviewer specialists from CSRS to make the minor changes to the PSQI. For example, in question 5c we used baño instead of servicio to denote the bathroom.
Demographic and Health Practices
Information about ethnicity, gender, and age was obtained via self-report. Only subjects identifying themselves as white or Hispanics of Mexican descent were included.
Analytic Plan
To determine the reliability of the PSQI factor structure across groups, multiple group confirmatory factor analysis with covariates (MIMIC), which uses maximum likelihood estimation, was applied to the data using MPlus statistical software Version 5.21.30 First, the factor structure of the English version of the PSQI was compared between English speaking NHW and English speaking HMD. Second, the best fitting model from the English-language ethnic group analysis was applied to the Spanish language survey data to determine the reliability of a Spanish language version of the PSQI. Previous research supports both 1-factor and 3-factor structures of the PSQI; using the steps below, we tested the reliability of both structures across groups. Gender and age were included as covariates in all models.
Each group comparison proceeded in steps. In the first step of each analysis, factor structures were compared between groups to determine configural invariance while factor loadings were allowed to differ. Size of factor loadings were examined to established the best baseline model for each group (> 0.450 was used as a cutoff). The next step tested the metric invariance across groups by constraining factor loadings to equivalence between groups. The fit for each model was determined by consulting the χ2 test, the comparative fit index (CFI; values ≥ 0.90 indicate good fit, although improvement in fit is also considered when comparing models with values < 0.90),31 and the standardized root mean square residual (SRMR values ≤ 0.05 indicate good fit).32 To empirically determine improvements in model fit, χ2 difference tests were conducted. Alpha level was set at a more conservative p ≤ 0.01 for evaluating significant differences with parameter changes.33
RESULTS
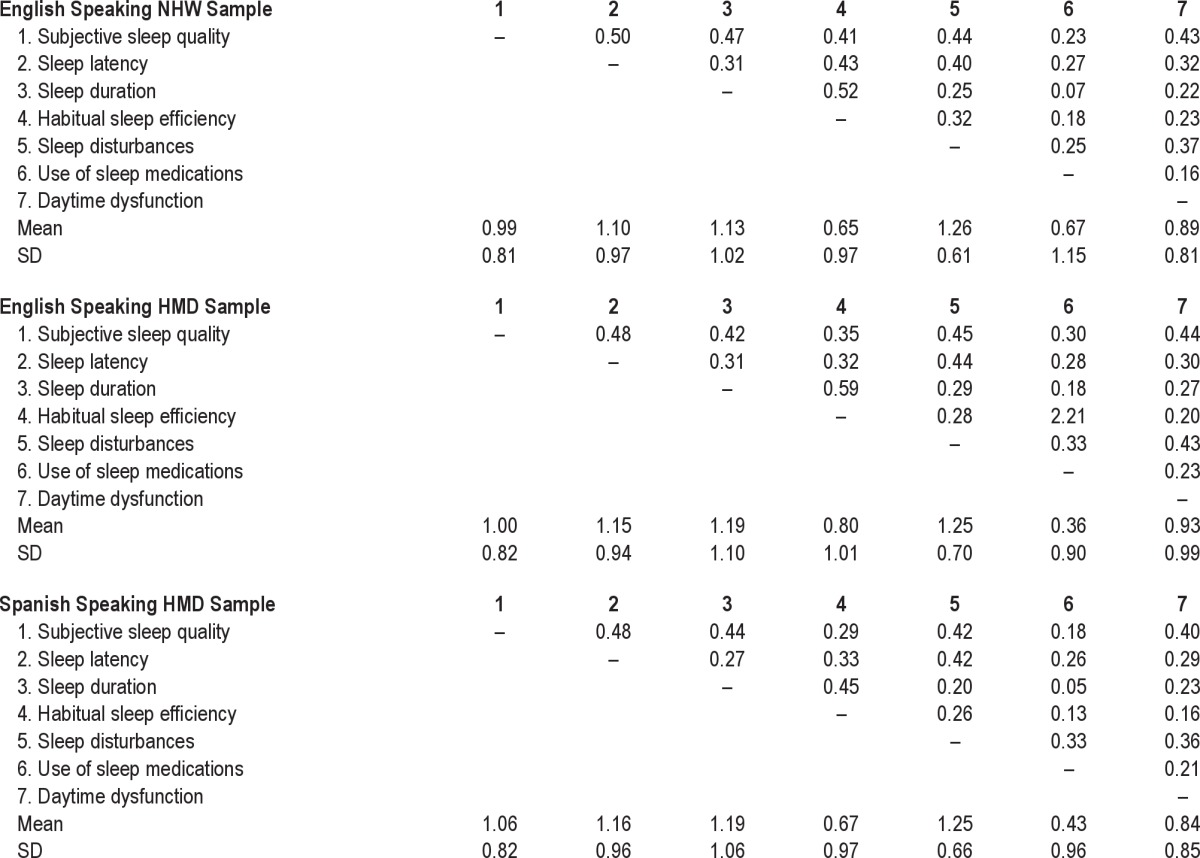
PSQI component descriptive statistics are in Table 1 for each ethnic group.
Table 1.
Pittsburgh Sleep Quality Index component correlations and descriptive statistics
One-Factor Structure
Ethnic Group Comparisons
Confirmatory factor analysis was used to examine the fit of a 1-factor structure of the English language version of the PSQI in both ethnic groups. The initial model included all 7 subscales of the PSQI. For NHW, the initial model did not fit the data well statistically (χ2 (26) = 424.825, p < 0.0001; CFI = 0.861), but fit well descriptively (SRMR = 0.049). The factor loading for Sleep Medication was low (0.314) and was removed from the model. The re-estimated model showed slightly improved fit statistically (χ2 (19) = 333.812, p < 0.0001; CFI = 0.881) and descriptively (SRMR = 0.045). Likewise, among English-speaking HMD, the one factor model with 7 subscales did not fit the data well statistically (χ2 (26) = 202.021, p < 0.0001; CFI = 0.818) but fit reasonably well descriptively (SRMR = 0.057). Again, the factor loading for Sleep Medication was low (0.330) and was removed from the model. The reduced model also showed slightly improved fit among the English-speaking HMD, both statistically (χ2 (19) = 155.894, p < 0.0001; CFI = 0.843) and descriptively (SRMR = 0.053). The retained baseline models in both groups included 6 subscales loaded on a single factor, with large factor loadings for all indicators (0.470-0.768) suggesting configural invariance across groups.
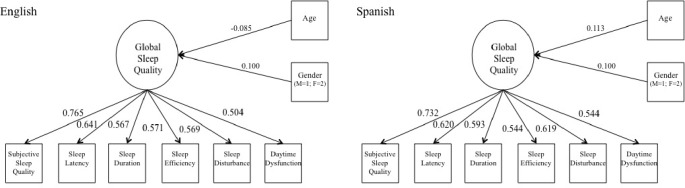
Next, to empirically determine whether the factor loadings differed between groups, all factor loadings (parameters) were constrained to equivalence. The metric invariance model also did not have good fit statistically (χ2 (48) = 510.040, p < 0.0001; CFI = 0.869), but did fit well descriptively (SRMR = 0.050) with some indicators suggesting improved fit over the configural invariance model. A χ2 difference test revealed the metric invariance model was not significantly different from the configural invariance model (Δχ2 (12) = 20.334, p > 0.01) so the structural invariance model was considered the more parsimonious and better fitting model. See Figure 1.
Figure 1. The retained one-factor model of Global Sleep Quality with overall model fit and factor loadings for both language groups.
Language Group Comparisons
A second multiple group confirmatory factor analysis with covariates was conducted to examine the fit of the model determined above to the Spanish language survey data and to establish structural invariance across languages (those who took the survey in English, NHW, and English-speaking HMD, were combined to form the English language group). The baseline model, which included the 6 subscales retained from the ethnic group analyses (subjective sleep quality, sleep duration, sleep disturbance, sleep efficiency daytime dysfunction, and sleep latency) to indicate a single factor fit the data adequately statistically (χ2 (19) = 224.088, p = 0.0001; CFI = 0.835) and descriptively (SRMR = 0.046), with large factor loadings (0.544-0.732) among Spanish-speaking MHD and fit well to the data from the combined NHW/HMD English-speaking group (χ2 (19) = 463.095, p = 0.0001; CFI = 0.873) and descriptively (SRMR = 0.054). Next, the metric invariance model, which constrained factor loadings to equivalence between English and Spanish language groups was estimated and fit the data reasonably well statistically (χ2 (48) = 726.001, p ≤ 0.0001; CFI = 0.857) and descriptively (SRMR = 0.052). Modification indices indicated loadings for Sleep Efficiency and Subjective Sleep Quality differed across groups. The constraints for these 2 subscale scores were removed and the model was re-estimated. The revised model showed marginally improved fit statistically (χ2 (46) = 718.835, p ≤ 0.0001; CFI = 0.858) and descriptively (SRMR = 0.051). The partial metric invariance model was then compared to the baseline model. The χ2 difference test (Δχ2 (10) = 31.652, p < 0.01) indicated the baseline model, wherein all factor loadings are estimatedly separately for each group, should be retained. Therefore, the configural invariance model, in which the factor structure did not vary between English and Spanish speaking groups, but factor loadings were estimated separately, was the best solution.
Internal Consistency of the 1-factor, 6-subscale PSQI
Cronbach α values were calculated and compared across groups to establish internal consistency of the retained 1-factor solution. In each group, Cronbach α values were indicative of adequate internal consistency (NHW Cronbach α = 0.775; English-speaking HMD Cronbach α = 0.741; HMD Cronbach α = 0.770).
Three-Factor Structure
Ethnic Group Comparisons
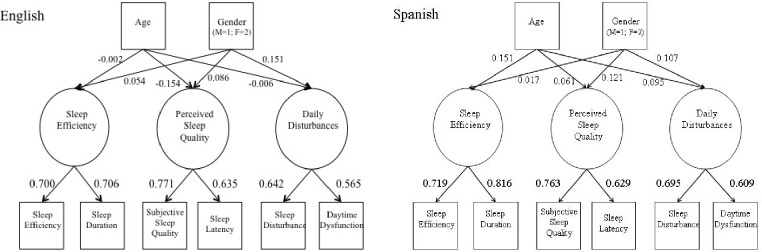
Next, reliability across groups of a 3-factor PSQI structure was tested, using the factor structure found by Cole and colleagues.23 The 3 latent factors tested were Sleep Efficiency (indicated by observed variables Sleep Duration and Sleep Efficiency), Perceived Sleep Quality (indicated by observed variables Subjective Sleep Quality, Sleep Latency, and Sleep Medication), and Daily Disturbances (Sleep Disturbances and Daytime Dysfunctions). Within both groups, the baseline 3-factor model had good fit to the data (NHW: χ2 (19) = 213.295, p < 0.0001; CFI = 0.932; SRMR = 0.037; English-speaking HMD: χ2 (19) = 104.149, p < 0.0001; CFI = 0.912; SRMR = 0.041). As with the 1-factor model, the factor loadings for Sleep Medication were < 0.450, Sleep Medication was removed, and the model was re-estimated. The revised models showed improved fit in both groups NHW: χ2 (12) = 118.289, p < 0.0001; CFI = 0.960; SRMR = 0.026; English-speaking HMD: χ2 (12) = 53.504, p < 0.0001; CFI = 0.952; SRMR = 0.028. All remaining factor loadings were large (0.547-0.773). Next, the metric invariance model was estimated, constraining the loadings for all 3 factors to equivalence across English-speaking groups. The metric invariance model also had good fit to the data χ2 (30) = 185.455, p < 0.0001; CFI = 0.956; SRMR = 0.028. A χ2 difference test indicated the metric invariance model was not significantly different from the configural invariance model (Δχ2 (6) = 13.662, p > 0.01) so the structural invariance model was considered the more parsimonious and better fitting model. See Figure 2.
Figure 2. The retained 3-factor model of Global Sleep Quality with overall model fit and factor loadings for both language groups.
Language Group Comparisons
The fit of the 3-factor model determined above was then fit to the Spanish language survey data to establish structural invariance across languages (as above, those who took the survey in English, NHW and English-speaking HMD, were combined to form the English language group). The baseline model, which included the 6 subscales indicating 3 factors fit the data well in both groups (Spanish-speaking HMD: χ2 (12) = 32.133, p < 0.0001; CFI = 0.984; SRMR = 0.018; English-speaking NHW/HMD: χ2 (12) = 154.142, p < 0.0001; CFI = 0.959; SRMR = 0.024). Next, the metric invariance model, which constrained factor loadings to equivalence between English and Spanish language groups was estimated and fit the data reasonably well statistically (χ2 (30) = 201.262, p < 0.0001; CFI = 0.964) and descriptively (SRMR = 0.025). The metric invariance model was then compared to the baseline model. The χ2 difference test (Δχ2 (6) = 14.987, p > 0.01) indicated the metric invariance model should be retained, see Figure 2,
Internal Consistency of the 3-Factor, 6-Subscale PSQI
Cronbach α values were calculated and compared across groups to establish internal consistency of the retained 3-factor solution. In each group, Cronbach α values were low for the English-speaking groups (NHW Cronbach α = 0.680; English-speaking HMD Cronbach α = 0.614) and adequate for the Spanish-speaking HMD (Cronbach α = 0.738). Internal consistency was low for the Perceived Sleep Quality scale in all groups (NHW Cronbach α = 0.655; English-speaking HMD Cronbach α = 0.640; HMD Cronbach α = 0.644) and low for the Sleep Disturbances scale in all groups (NHW Cronbach α = 0.519; English-speaking HMD Cronbach α = 0.515; HMD Cronbach α = 0.573).
DISCUSSION
The PSQI is a widely used measure, which taps the important dimension of sleep quality. There are several accepted translations of the PSQI, and it has been used in numerous populations and language groups. In this investigation, we examined the reliability of the PSQI for assessment of sleep quality in community-dwelling, adult, English-speaking NHW and HMD, and Spanish speaking HMD. Our data suggest that the English version PSQI global score composed of seven subscales did not fit well into a one-factor model for either HMD or NHW. Six of the seven PSQI subscales (Subjective Sleep Quality, Sleep Duration, Sleep Disturbance, Sleep Efficiency, Daytime Dysfunction, and Sleep Latency) fit into a single factor global model with equivalent factor loadings for English speaking NHW and HMD (e.g., the subscales accounted for similar amounts of variance in the global scores of these two populations). The truncated single factor global model also fit well the Spanish speaking HMD group, but factor loadings differed slightly.
Different factor structures for the PSQI have been reported. In our sample population, a three-factor PSQI model reported by Cole and colleagues23 fit well, and provided a better fit than the one-factor model in all subject groups. The truncated three-factor model also fit well in the Spanish speaking HMD group and factor loadings were equivalent across ethnic/language groups. Together, these results suggest that across ethnic/language groups, the six individual subscales (the subscale Sleep Medications again fit poorly) of the PSQI assessed the same three latent variables and that the contribution of individual subscales to each latent variable did not vary across language/ethnic group.
An increasing body of literature suggests that a multiple factor structure of the PSQI may more reliably assess sleep problems than the original single-factor model. In populations of Nigerian university students, Australian adults, renal transplant recipients, and adults with chronic fatigue syndrome, a three-factor scoring method of the PSQI better fit the data than the original single factor model.21,22,34,35 A similar finding emerged in our data; importantly, we also demonstrated that the factor loadings of the three-factor scoring method were equivalent across English speaking NHW and Spanish and English speaking HMD. Consistent with other reports, we also found that use of sleeping medications did not load well into the construct of sleep quality.20,23,25,26,36–39
The results of this study should be interpreted in light of a number of limitations. Participants were interviewed using a telephone survey, a methodology that has been criticized for being biased against those without telephones, especially in ethnic minority samples. Additionally, despite the goal of equivalence with regards to demographic characteristics, the composition of groups differed markedly in terms of age and gender. NHW were significantly older than HMD, and it is well known that objective poor sleep quality increases with age and women report more subjective poor sleep quality with aging.40 Additionally, a significant proportion of subjects had to be excluded primarily due to discordant reported habitual total sleep duration and sleep schedule. Notably, missing data was associated with ethnicity, such that significantly higher numbers of HMD were removed from the analysis. Excluding a larger number of subjects from the HMD groups may have obscured potential differences in factor analytic structure across groups. It is striking that the telephone interview asked straightforward questions about sleep quality and our data shows clearly that many participants answered these questions in ways that demonstrated they did not understand them. As a result, we were forced to eliminate approximately 14% of our total sample: this is not an unusually high amount of missing data in epidemiological research, but it serves as a cautionary tale. Our experience suggests that when the PSQI is administered using computer assisted telephone interviewing (CATI), an electronic trigger should be constructed to immediately alert the interviewer to discrepancies in reported sleep efficiency. Then further clarifications can be made.
Based on our findings, more investigation is needed on the reliability of the PSQI and other measures of sleep quality across ethnic/language groups. Specifically our investigation needs to be replicated in populations seeking help for sleep problems and among the various Hispanic groups. In conclusion, our results suggest that the seven-subscale PSQI global score is not reliable in HMD regardless of being English or Spanish speakers. Our data suggest that for English and Spanish speaking HMD, a three-factor version of the PSQI composed of six of the original subscales (Subjective Sleep Quality, Sleep Duration, Sleep Disturbance, Daytime Dysfunction, Sleep Efficiency and Sleep Latency) may more reliably assess sleep quality
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This work was supported by NIH grant R01 HL075630 (to Dr. Loredo) and by the Canadian Institute of Health Research (to Dr. Tomfohr)
REFERENCES
- 1.Leineweber C, Kecklund G, Janszky I, Åkerstedt T, Orth-Gomér K. Poor sleep increases the prospective risk for recurrent events in middle-aged women with coronary disease: The Stockholm Female Coronary Risk Study. J Psychosom Res. 2003;54:121–7. doi: 10.1016/s0022-3999(02)00475-0. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz SW, Cornoni-Huntley J, Cole SR, Hays JC, Blazer DG, Schocken DD. Are sleep complaints an independent risk factor for myocardial infarction? Ann Epidemiol. 1998;8:384–92. doi: 10.1016/s1047-2797(97)00238-x. [DOI] [PubMed] [Google Scholar]
- 3.Ayas NT, White DP, Manson JAE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 4.Jennings JR, Muldoon MF, Hall M, Buysse DJ, Manuck SB. Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007;30:219–23. doi: 10.1093/sleep/30.2.219. [DOI] [PubMed] [Google Scholar]
- 5.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33:962–7. doi: 10.1093/sleep/33.7.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Humes KR, Jones NA, Ramirez RR. Overview of Race and Hispanic Origin: 2010 Census Briefs. 2011;2011:23. [Google Scholar]
- 8.Guzmán B. Washington, DC: U.S. Census Bureau; 2001. Census 2000 Brief. The Hispanic Population. [Google Scholar]
- 9.Roberts RE, Roberts CR, Chen IG. Ethnocultural differences in sleep complaints among adolescents. J Nerv Ment Dis. 2000;188:222–9. doi: 10.1097/00005053-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. Sleep. 2006;29:359–65. doi: 10.1093/sleep/29.3.359. [DOI] [PubMed] [Google Scholar]
- 11.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson B. Washington, DC: American Psychological Association; 2004. Exploratory and confirmatory factor analysis: Understanding concepts and applications. [Google Scholar]
- 13.Buysse DJ, Reynolds CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh sleep quality index (PSQI) Sleep. 1991;14:331–8. [PubMed] [Google Scholar]
- 14.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res . 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 16.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 17.Doi Y, Minowa M, Uchiyama M, et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–72. doi: 10.1016/s0165-1781(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 18.Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14:1943–52. doi: 10.1007/s11136-005-4346-x. [DOI] [PubMed] [Google Scholar]
- 19.Shochat T, Tzischinsky O, Oksenberg A, Peled R. Validation of the Pittsburgh Sleep Quality Index Hebrew translation (PSQI-H) in a sleep clinic sample. Isr Med Assoc J. 2007;9:853–6. [PubMed] [Google Scholar]
- 20.Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manage. 2004;27:140–8. doi: 10.1016/j.jpainsymman.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh Sleep Quality Index (PSQI) among Nigerian university students. Sleep Med. 2007;8:266–70. doi: 10.1016/j.sleep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Burkhalter H, Sereika SM, Engberg S, Wirz-Justice A, Steiger J, De Geest S. Structure validity of the Pittsburgh Sleep Quality Index in renal transplant recipients: a confirmatory factor analysis. Sleep Biol Rhythms. 2010;8:274–81. [Google Scholar]
- 23.Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep. 2006;29:112–6. doi: 10.1093/sleep/29.1.112. [DOI] [PubMed] [Google Scholar]
- 24.Kotronoulas GC, Papadopoulou CN, Papapetrou A, Patiraki E. Psychometric evaluation and feasibility of the Greek Pittsburgh Sleep Quality Index (GR-PSQI) in patients with cancer receiving chemotherapy. Supportive Care Cancer. 2010:1–10. doi: 10.1007/s00520-010-1025-4. [DOI] [PubMed] [Google Scholar]
- 25.Skouteris H, Wertheim EH, Germano C, Paxton SJ, Milgrom J. Assessing sleep during pregnancy: a study across two time points examining the Pittsburgh Sleep Quality Index and associations with depressive symptoms. Womens Health Issues. 2009;19:45–51. doi: 10.1016/j.whi.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Jomeen J, Martin CR. Assessment and relationship of sleep quality to depression in early pregnancy. J Reprod Infant Psychol. 2007;25:87–99. [Google Scholar]
- 27.Royuela A, Macias JA. Propiedades clinimetricas de la versión castellana del cuestionario de Pittsburgh. Vigilia-Sueño. 1997;9:81–94. [Google Scholar]
- 28.Escobar-Cordoba F, Eslava-Schmalbach J. Validación colombiana del índice de calidad de sueño de Pittsburgh. Rev Neurol. 2005;4:150–5. [PubMed] [Google Scholar]
- 29.Jiménez-Genchi A, Monteverde-Maldonado E, Nenclares-Portocarrero A, Esquivel-Adame G, de la Vega-Pacheco A. Reliability and factorial analysis of the Spanish version of the Pittsburgh Sleep Quality Index among psychiatric patients. Gac Med Mex. 2008;144:491–6. [PubMed] [Google Scholar]
- 30.Muthén LK, Muthén BO. Los Angeles, CA: Muthén & Muthén; 2007. Mplus: Statistical analysis with latent variables: user's guide. [Google Scholar]
- 31.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–46. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 32.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 33.Ullman JB. Reviewing the basics and moving forward. J Pers Assess. 2006;87:35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- 34.Magee CA, Caputi P, Iverson DC, Huang XF. An investigation of the dimensionality of the Pittsburgh Sleep Quality Index in Australian adults. Sleep Biol Rhythms. 2008;6:222–7. [Google Scholar]
- 35.Mariman A, Vogelaers D, Hanoulle I, Delesie L, Tobback E, Pevernagie D. Validation of the three-factor model of the PSQI in a large sample of chronic fatigue syndrome (CFS) patients. J Psychosom Res. 2012;72:111–3. doi: 10.1016/j.jpsychores.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 36.Koffel E, Watson D. The two-factor structure of sleep complaints and its relation to depression and anxiety. J Abnorm Psychol. 2009;118:183–94. doi: 10.1037/a0013945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–71. [PMC free article] [PubMed] [Google Scholar]
- 38.Spira AP, Beaudreau SA, Stone KL, et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. 2012;67:433–9. doi: 10.1093/gerona/glr172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beaudreau SA, Spira AP, Stewart A, et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med. 2012;13:36–42. doi: 10.1016/j.sleep.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Unruh ML, Redline S, An MW, et al. Subjective and objective sleep quality and aging in the Sleep Heart Health Study. J Am Geriatr Soc. 2008;56:1218. doi: 10.1111/j.1532-5415.2008.01755.x. [DOI] [PubMed] [Google Scholar]