Abstract
Background:
There is a gap in the literature regarding the extent of possible co-occurrence of attention deficit hyperactivity disorder (ADHD) and pervasive developmental disorders (PDD). This study aimed to investigate co-occurring of ADHD in children with PDD.
Methods:
A clinical sample of 68 children with PDD was assessed according to DSM-IV criteria to make ADHD and/ or PDD diagnoses. All the different types of PDD were included. DSM-IV derived criteria for ADHD and PDD were analyzed. An exploratory factor analysis was conducted.
Results:
the rate of autism, Asperger syndrome, Rett's disorder, childhood disintegrative disorder and PDD-NOS (not otherwise specified) was 55.4%, 16.9%, 3.1%, 3.1%, 21.5%, respectively. 53.8% of the sample was with ADHD co-morbidity. The rate of ADHD subtypes was 37.1%, 22.9%, and 40.0% for inattentive type, hyperactivity/impulsivity type and combined type, respectively.
Conclusion:
ADHD and its symptoms highly co-occur with PDD. Meanwhile, the result of factor analysis supports the independence of ADHD and PDD diagnostic criteria.
Keywords: Prevalence, autism, co-morbidity, factor analysis
INTRODUCTION
Pervasive developmental disorder (PDD) is an exclusive criterion for attention deficit hyperactivity disorder (ADHD) diagnosis according to the DSM-IV diagnostic criteria.[1] In the same way, according to the international classification of mental and behavioral disorders (ICD-10), hyperkinetic disorder that is the ICD equivalent of ADHD cannot be diagnosed in the presence of PDD.[2] In other words, it is impossible to make ADHD and PDD diagnoses in the same time. Maybe, this is one of the reasons that why the co-morbidity and overlap of these two disorders, comparing to large body of the literature about ADHD or PDD, have not been well studied in the literature.[3] Probably, the co-occurring of PDD and ADHD enhances impairment in daily activities.[4] Studies about ADHD in children with PDD are needed to have a better understanding from similarities and differences of the disorders.
In recent years, there are some reports about the co-morbidity of ADHD and PDD.[5] The rate of high hyperactivity in children with PDD is more than those without PDD.[6,7] Lecavalier (2006) surveyed symptoms of inattention and hyperactivity in children with autism spectrum disorder using a questionnaire. It is reported that higher than half of the sample had moderate to severe symptoms of inattention and hyperactivity.[8] A retrospective chart review study on 57 children with autism or PDD-Not Otherwise Specified (PDD-NOS), or ADHD indicated that 26% of the subjects met DSM- IV criteria for the combined type of ADHD. The rate of the inattentive type of ADHD was 33%. Meanwhile, 41% did not fulfill criteria for diagnosis of ADHD.[9] A population-derived study reported that the rate of 29.2% for ADHD in autism spectrum disorders.[10] In a newly published article, Ponde et al. reported that 53.1% of the autism spectrum disorders (ASD) children selected from a specialized school had ADHD. The rate of inattentive subtype, hyperactive-impulsive, and combined subtype was 5.8%, 31.2%, 18.7%, respectively.[11] Shared genetic correlation between ADHD and autism is suggested.[12]
Some of the limitations of the previous studies are (i) lack of including different types of PDD,[9,11] (ii) the gathering of information via questionnaires rather than face to face interview[6,8,13,14] or retrospective chart review,[9] (iii) lack of using a formal diagnostic criteria like DSM-IV diagnostic criteria,[6,8] (iv) reporting of hyperactivity and inattention symptoms rather than ADHD as a disorder.[6,8,14] In addition, both ADHD and autism can be impactful due to pharmacotherapy while some participants were undertaking medications.[11] These limitations indicate that there is a gap in the literature regarding the co-occurrence of ADHD and autism. The first aim of the current study is to overcome to all of these limitations.
Moreover, a review article reported that there is no study on the factor analysis of DSM-IV-derived items for ADHD and PDD to examine the extent of their possible diagnostic criteria overlapping.[15] So, the second aim of this study is to find an answer for another gap in the literature concerning the factor analysis of autism and ADHD diagnostic criteria.
METHODS
The participants of this prospective cross-sectional study were a convenient clinical sample of 68 children and adolescents with autism spectrum disorder. The sample was new referrals to the Child and Adolescent Psychiatry outpatient clinic affiliated with Shiraz University of Medical Sciences, Shiraz, Iran. The information about three children was not enough, so, 65 children were included.
Whenever applicable, children and at least one of the parents of the children were interviewed face to face by the child and adolescent psychiatrist. The children were also observed.
ADHD diagnosis was made according to Diagnostic and Statistical Manual of Mental Disorders (DSM IV-TR).[1] The schedule for affective disorders and schizophrenia (K-SADS), farsi version, was administered.[16] KSADS is a diagnostic semistructured psychiatric interview. Its consensual validity for ADHD (Kappa) is 0.90. Its test-retest reliability is 0.81.[16]
PDD was diagnosed according to the autism diagnostic interview-revised (ADI-R) using DSM IV-TR criteria.[1,17] All the interviews were administered by an experienced child psychiatrist.
There are several inclusion criteria. All the different types of autism spectrum disorders (ASD) including autism, Asperger syndrome, Rett's disorder, Childhood disintegrative disorder, and pervasive developmental disorder-not otherwise specified (NOS) were included in this study. The parents gave informed consent for voluntary participation in this study. All of them agreed to participate.
The intelligence level was not as an exclusive criterion. They were not excluded on the basis of socioeconomic status and level of functioning.
Analysis
SPSS for Windows was used for conducting statistical analysis. Frequencies were calculated for the different types of ASD, ADHD symptoms, and the demographic categorical data. The variable of age was reported as mean and standard deviation (SD). An exploratory factor analysis with two fixed number factors was conducted to examine loading of items of ADHD and PDD criteria. There were 30 items including 12 items for autism and 18 items for ADHD according to DSM-IV-TR diagnostic criteria.[1] The Farsi version of the items was provided by a study[18] and it is used in many similar studies in Iran.[19,20]
Kaiser–Meyer–Olkin measure of sampling was calculated to investigate sampling adequacy for conducting of factor analysis. Bartlett's test of sphericity was also conducted.
RESULTS
Forty-nine (75.4%) of the sample were boys. The mean age and standard deviation of age was 7.3 and 2.4 years, respectively. According to clinical interview, 55.4% of them were with autism. The rate of Asperger syndrome, Rett's syndrome, childhood disintegrative disorder, and PDD- NOS was 16.9%, 3.1%, 3.1%, 21.5%, respectively [Figure 1].
Figure 1.
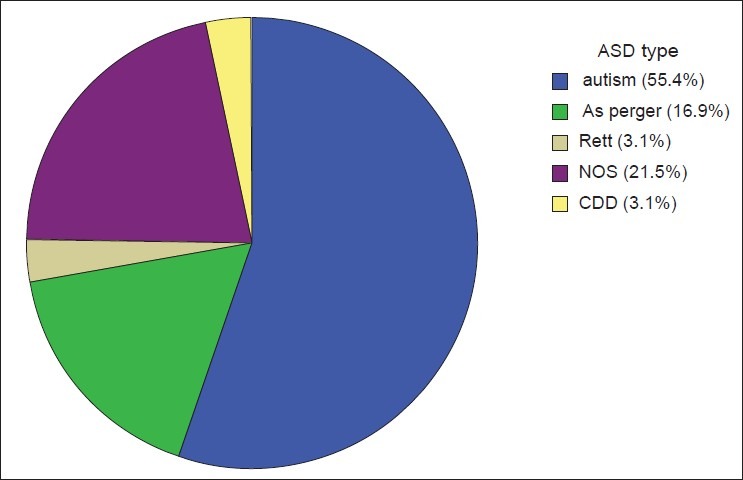
The prevalence of different autism spectrum disorders
Kaiser–Meyer–Olkin measure of sampling adequacy was 0.594. Bartlett's test of sphericity was significant (Chi-Square=830.7, P<0.001). This results support the suitability of data for factor analysis. Factor analysis with the two factors explained 37.4% of the total variance. The eigenvalues for the factors were 4.1 and 7.04. Factor structure and items loading of ADHD and PDD are indicated in [Table 1]. Factor analysis showed that all the items related to PDD were loaded on the Factor I and all the items related to ADHD were loaded on Factor II.
Table 1.
Factor structure and items loading of attention deficit hyperactivity disorder (ADHD) and pervasive developmental disorders (PDD)
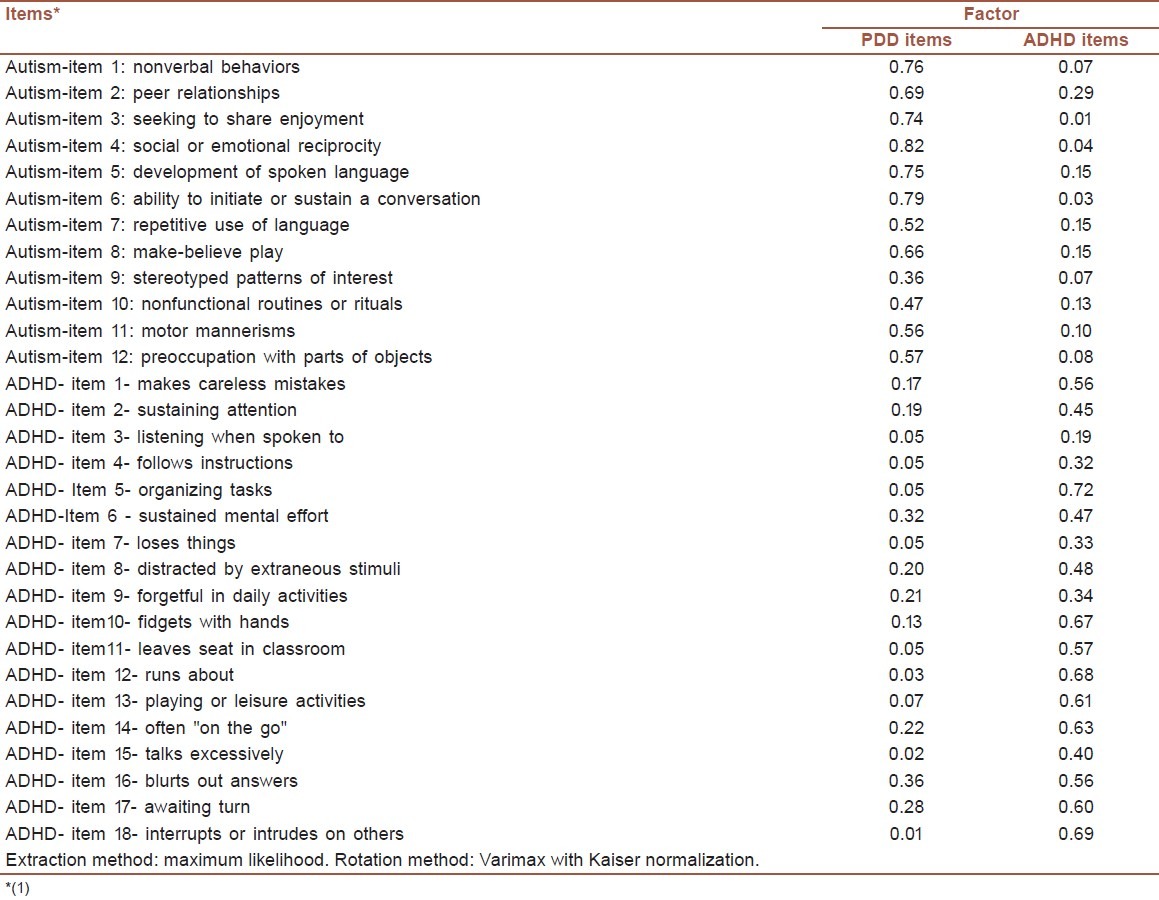
Table 2 indicates that 46.2% of the sample did not fulfill diagnostic criteria for ADHD while 53.8% of the sample was with ADHD co-morbidity. Psychiatric interviews also showed that the percent of different subtypes of ADHD in children with ASD co-morbid with ADHD was 37.1%, 22.9%, and 40.0% for the inattentive type, hyperactivity/ impulsivity type and combined type, respectively [Figure 2].
Table 2.
The frequency of different types of attention deficit hyperactivity disorder
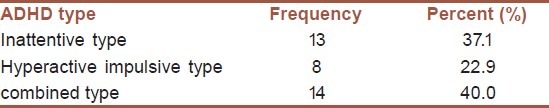
Figure 2.
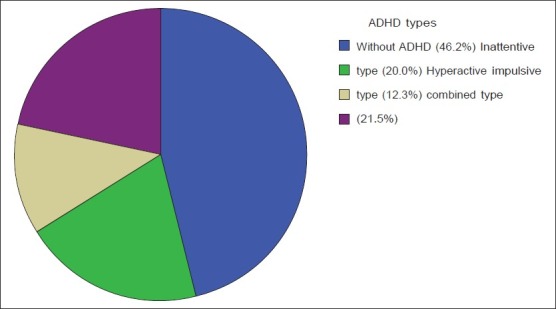
The frequency of attention deficit hyperactivity disorder (ADHD) and its subtypes in the children and adolescents with autism spectrum disorders
The frequency of ADHD symptoms are displayed in [Table 3]. The prevalence of 9 out of the 18 symptoms related to ADHD was more than 50% in children with PDD.
Table 3.
The frequency of attention deficit hyperactivity disorder (ADHD) symptoms in children and adolescents with autism spectrum disorders
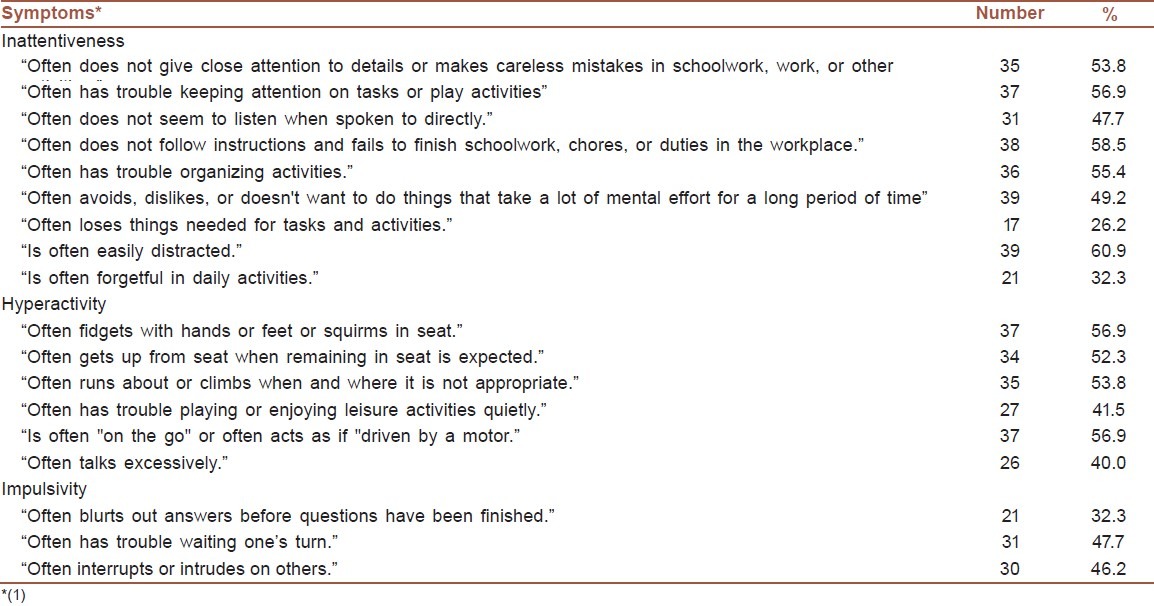
Except two symptoms, the prevalence of seven symptoms related to inattentiveness were more than 47%. The prevalence of all of six symptoms related to hyperactivity was more than 40%. The rate of two from the three symptoms related to impulsivity was more than 46%. Overall, only one symptom from the 18 symptoms of ADHD was less than 26%.
DISCUSSION
The most striking finding of this study is a high rate of ADHD in the clinical sample of children with PDD. More than half of the children have ADHD. This confirms the high rate of ADHD in PDD.[11] However, lack of correlation between ADHD and PDD symptoms in factor analysis would further indicate the independence of the two disorders diagnostic criteria. This finding is in a similar with the result of a study included general population of children and adolescents.[21]
The rate of ADHD subtypes was 37.1%, 22.9%, and 40.0% for the inattentive type, hyperactivity/impulsivity type, and combined type, respectively. The total rate of ADHD was very similar to a previous study.[11] While, in a previous study on the children of a specialized school, the rate of inattentive subtype, hyperactive-impulsive, and combined subtype was 5.8%, 31.2%, 18.7%, respectively.[11] One explanation for this difference may be related to methodological issues. The current study was from a clinic while the previous study was from a specialized school.[11] However, both of these studies report the high rate of ADHD in PDD.
A clinical implication for the current results is that clinicians should be noticed that ADHD and its symptoms should be evaluated in all of children with PDD despite that PDD is an exclusionary criterion in ADHD according to DSM-IV diagnostic criteria. In addition, it has an important clinical implication for the management of children with PDD. Since, the parents of children with ADHD need parent management education; clinicians should educate the parents of children with PDD to have a better understanding from these two disorders and their managing. It is not clear if failure to manage one of these two disorders may compromise the benefits of managing the other one or outcome of the disorder. Maybe, appropriate specific interventional treatments should be designed. A larger and more homogenous sample of children with PDD may help to delineate possible endophenotypes and common etiological factor for PDD and ADHD.
This study reports the co-morbidity of ADHD and ASD from a small and clinical sample. So, the generalization of the results to other settings or community samples is not guaranteed because of the possible sampling bias.[22] Further studies should include samples of children drawn from general population. There are some other methodological points needed for further considerations. As many of previous studies, the intelligence level was not assessed.[11] Future studies required to include intelligence assessment since its level may affect on manifestation of psychopathology and cognitive function.[23] For example, some of them are not able to express their emotional problems due to their low intellectual abilities. The source of information was only parents. The sample is relatively small. However, KMO and Bartlett's test of sphericity shows that the sample is suitable for factor analysis. The low total variance can be related to this low sample size.
Gathering information from different informants and larger sample size would be helpful. In addition, the sample consists only of children referred to PDD. Therefore, the results tell us about the presence of ADHD symptoms in children with PDD. Furthermore, the rates of PDD in an ADHD population should be investigated in future studies. One of the research implications of these high rates of co- morbidity is that future studies should try to have a better understanding and defining from the interactions of these two disorders. It needs to be answered whether ADHD in PDD is truly ADHD rather than a phenocopy.[13] There is a speculation that PDD can be evolved into ADHD.[24] Further longitudinal studies will show whether the children with PDD and ADHD are evolving from PDD to ADHD.
Clinicians should be reminded that ADHD and its symptoms in children suffering from any types of PDD are very high and it should be as a major treatment goal. In other words, ADHD and PDD are two separate disorders but ADHD frequently occur in PDD.
Despite limitations, this study used DSM-IV diagnostic criteria and diagnoses were made using face to face interview with the parent and observation of the children. This is very important because the symptoms of ADHD can or cannot be associated with other behavioral and/or emotional problems. This differentiation is more reliable using face to face interview rather than using questionnaires.
ACKNOWLEDGMENT
This is part of a broader ongoing study about ADHD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Association AP. Washington: American Psychiatric Press; 2000. American Psychiatric Association, Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 2.The ICD-10 classification of mental and behavioural disorders. Geneva: 1993. World Health Organization. [Google Scholar]
- 3.Gillberg C, Billstedt E. Autism and Asperger syndrome:Coexistence with other clinical disorders. Acta Psychiatr Scand. 2000;102:321–30. doi: 10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]
- 4.Frazier JA, Biederman J, Bellordre CA, Garfield SB, Geller DA, Coffey BJ, et al. Should the diagnosis of attention deficit/hyperactivity disorder be consider in children with pervasive developmental disorder? J Atten Disord. 2001;4:203–11. [Google Scholar]
- 5.Reiersen AM, Constantino JN, Todd RD. Co-occurrence of motor problems and autistic symptoms in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2008;47:662–72. doi: 10.1097/CHI.0b013e31816bff88. [DOI] [PubMed] [Google Scholar]
- 6.Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R. Prevalence of pervasive developmental disorders in the British nationwide survey of child mental health. J Am Acad Child Adolesc Psychiatry. 2001;40:820–7. doi: 10.1097/00004583-200107000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Yoshida Y, Uchiyama T. The clinical necessity for assessing Attention Deficit/Hyperactivity Disorder (AD/HD) symptoms in diabetic patients. Int J Food Sci Nutr. 2001;62:289–94. [Google Scholar]
- 8.Lecavalier L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. J Autism Dev Disord. 2006;36:1101–14. doi: 10.1007/s10803-006-0147-5. [DOI] [PubMed] [Google Scholar]
- 9.Goldstein S, Schwebach AJ. The comorbidity of Pervasive Developmental Disorder and Attention Deficit Hyperactivity Disorder: Results of a retrospective chart review. J Autism Dev Disord. 2004;34:329–39. doi: 10.1023/b:jadd.0000029554.46570.68. [DOI] [PubMed] [Google Scholar]
- 10.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47:921–9. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 11.Ponde MP, Novaes CM, Losapio MF. Frequency of symptoms of attention deficit and hyperactivity disorder in autistic children. Arq Neuropsiquiatr. 2010;68:103–6. doi: 10.1590/s0004-282x2010000100022. [DOI] [PubMed] [Google Scholar]
- 12.Ronald A, Edelson LR, Asherson P, Saudino KJ. Exploring the relationship between autistic-like traits and ADHD behaviors in early childhood: Findings from a community twin study of 2-year-olds. J Abnorm Child Psychol. 2010;38:185–96. doi: 10.1007/s10802-009-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gadow KD, DeVincent CJ, Pomeroy J, Azizian A. Psychiatric symptoms in preschool children with PDD and clinic and comparison samples. J Autism Dev Disord. 2004;34:379–93. doi: 10.1023/b:jadd.0000037415.21458.93. [DOI] [PubMed] [Google Scholar]
- 14.Clark T, Feehan C, Tinline C, Vostanis P. Autistic symptoms in children with attention deficit-hyperactivity disorder. Eur Child Adolesc Psychiatry. 1999;8:50–5. doi: 10.1007/s007870050083. [DOI] [PubMed] [Google Scholar]
- 15.Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK. Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. Eur Child Adolesc Psychiatry. 2010;19:281–95. doi: 10.1007/s00787-010-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghanizadeh A, Mohammadi MR, Yazdanshenas A. Psychometric properties of the Farsi translation of the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version. BMC Psychiatry. 2006;6:10. doi: 10.1186/1471-244X-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24:659–85. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 18.Alipour A, Esmaile EM. Studying of Validity, Reliability, and Cutoff points of CSI-14 in the School Children Aged 6 to 14 in Tehran. Tehran: Exceptional students’ Research Center; 2004. [Google Scholar]
- 19.Ghanizadeh A, Jafari P. Cultural structures of the Persian parents’ ratings of ADHD. J Atten Disord. 2010;13:369–73. doi: 10.1177/1087054709332421. [DOI] [PubMed] [Google Scholar]
- 20.Ghanizadeh A. Overlap of ADHD and Oppositional Defiant Disorder DSM-IV Derived Criteria. Arch Iran Med. 2011;14:179–82. [PubMed] [Google Scholar]
- 21.Ghanizadeh A. Factor analysis on ADHD and autism spectrum disorder DSM-IV-derived items shows lack of overlap. Eur Child Adolesc Psychiatry. 2010;19:797–8. doi: 10.1007/s00787-010-0127-3. [DOI] [PubMed] [Google Scholar]
- 22.Ghanizadeh A, Mohammadi MR, Sadeghiyeh T, Shooshtari AA, Akhondzadeh S. Symptoms of children with autism spectrum disorder, a clinical sample. Iran J Psychiatry. 2009;4:44–8. [Google Scholar]
- 23.Tager-Flusberg H, Sullivan K. Predicting and explaining behavior: A comparison of autistic, mentally retarded and normal children. J Child Psychol Psychiatry. 1994;35:1059–75. doi: 10.1111/j.1469-7610.1994.tb01809.x. [DOI] [PubMed] [Google Scholar]
- 24.Fein D, Dixon P, Paul J, Levin H. Brief report: Pervasive developmental disorder can evolve into ADHD: Case illustrations. J Autism Dev Disord. 2005;35:525–34. doi: 10.1007/s10803-005-5066-3. [DOI] [PubMed] [Google Scholar]


