Abstract
Background
Cigarette smoking causes cardiovascular disease and activates markers of endothelial dysfunction or injury. We investigated the nailfold capillary blood velocity (NCV) in cigarette smokers compared to non-smokers.
Methods
Forty-eight men (eighteen non-smokers and thirty smokers) were recruited. We measured NCV using nailfold capillary microscopy and exhaled carbon monoxide (ECO) concentration three times (before smoking; NCV0min and ECO0min, and after smoking; NCV5min, ECO5min, NCV30min, and ECO30min), in a condition of fasting in the case of smokers. In non-smokers, the same measurements were taken without smoking. Additionally, personal cigarette smoking and alcohol drinking history were acquired by a self-administrated questionnaire.
Results
Mean age, waist circumference, ECO0min, ECO5min, and ECO30min was higher and NCV5min and NCV30min were significantly lower in smokers compared to non-smokers. Total smoking years were negatively correlated with NCV5min. Average pack of the daily smoking, total pack-years, as well as total smoking years were also negatively correlated with NCV30min by regression analysis. After adjustment of significantly different variables, NCV30min was significantly lower in smokers. In the subgroup analysis, the interleukin-6 level was significantly increased in subjects with a long period of cigarette smoking compared with non-smokers.
Conclusion
Reduction of NCV in smokers is associated with personal smoking history, not with body composition or certain oxidative stress markers.
Keywords: Nailfold Capillary Blood Velocity, Smoking, Qxidative Stress
INTRODUCTION
Cigarette smoking is a serious health threat worldwide and is also the most important modifiable health risk factor. Cigarette smoking has been definitively linked to many cancers, cardiovascular diseases, lung diseases and some reproductive diseases.1) According to 2007 data of the Korean Ministry of Health and Welfare, the rate of cigarette smoking in Koreans over the age of 20 twenties was 22.8% and that of men was 42.5%.2) This could prelude a great increase in cardiovascular disease in the coming decades, since cigarette smoking causes more deaths from cardiovascular disease than any other disease.3) In some proposed pathways, smoking impairs endothelium-dependent vasodilation in arteries and activates markers of endothelial dysfunction or injury.4) Inflammation plays a central role in the progression of atheroscleorsis,5) and several reports have suggested that smoking may trigger the inflammatory arm of atherogenesis.6) As the number of cardiovascular risk factors increases, so does the severity of asymptomatic coronary and aortic atherosclerosis. This is true even in young people, and the major cause of which is cigarette smoking.7)
During the beginning of the 20th century, LeRoy et al.8) used capillaroscopic analysis to show in detail the abnormalities that characterize the involvement of microvasculature during Raynaud's phenomenon (RP) in systemic sclerosis. Three defined major nailfold videocapillaroscopy patterns are considered useful in assessing the appearance and progression of the sclerodermic microangiopathy.9) Early in the disease, the peripheral microangiopathy may be well recognized and studied by nailfold capillaroscopy or, even better, with videocapillaroscopy, a noninvasive and safe technique, which has both diagnostic and prognostic value in the presence of RP.10) Nailfold capillary red blood cell velocity at rest and after circulatory arrest is slightly reduced in patients with peripheral arterial disease, but not to a significant degree.11) However, nailfold capillary blood velocity (NCV) in cigarette smokers before and after cigarette smoking has not been reported. Therefore, we investigated NCV in cigarette smokers compared to non-smokers.
METHODS
1. Study Design
A cross-sectional study was conducted to evaluate NCV before and after cigarette smoking in smokers compared to non-smokers in the Department of Family Practice and Community Health, Ajou University Hospital, Suwon, Gyeonggi-do, Korea. Forty eight men comprising 18 non-smokers and 30 smokers (defined as smoking for ≥1 year) were recruited voluntarily after providing informed consent. Smoking history was defined in terms of average pack of daily smoking, total smoking years, and total pack-years, which was calculated by (total pack-years = pack of daily smoking × total smoking years) from information solicited using a self-administered questionnaire. NCV and exhaled carbon monoxide (ECO) concentration were measured three times after fasting in all subjects and the results were compared. Additional information on personal history including smoking history and alcohol consumption was also collected using a self-administrated questionnaire on the day of testing.
2. Measurement of Nailfold Capillary Blood Velocity and Exhaled Carbon Monoxide Concentration
The same trained research nurse measured the NCV using the Nailfold Capillary Microscopy, Raynaud Sanner XWL (YP 0901; Yejin Medical, Gwangmyeong, Korea). NCV was determined in the arterial limb of all visible capillaries (on average between three and four capillaries per subject) using frame-by-frame analysis. The videotape was advanced frame by frame at a rate of 20 ms per frame, and the displacement of plasma gaps was measured on the monitor. The velocity was calculated from these measurements using the calibration factor. For each of the 3 minutes of resting blood flow, NCV was measured for the final 20 seconds and the average NCV was calculated. The overall mean of these three values was defined as resting NCV. During and after cooling, NCV was measured for the final 10 seconds of each minute and the initial 10 seconds of the subsequent minute. NCV was measured three times in all subjects. The first measurement was conducted before smoking (NCV0min) in all study subjects. Then, in the case of smokers, subjects moved to a smoking area to smoke a cigarette and returned to measure NCV after 5 minutes (NCV5min) and 30 minutes (NCV30min). Non-smokers also moved to the smoking area but did not smoke, and also returned for measurements of NCV5min and NCV30min. Smokers were instructed to smoke in their usual fashion.
ECO measurement was conducted just after each NCV determination (i.e., ECO0min, ECO5min, and ECO30min) in expired breath using a Micro Smokerlyzer (Bedfont Scientific Ltd., Harrietsham, UK). Measurement was conducted by one experienced research nurse. All subjects were instructed to inhale as deeply as possible and hold their breath throughout the countdown, which was set for five seconds. They were educated to exhale slowly but gently into the mouthpiece until their lungs felt empty. There was no adverse event in this measurement procedure.
3. Measurement of Anthropometry and Oxidative Stress Markers
Routine health examination was done after overnight fasting (at least eight hours). The height and body weight of the participants were measured while they wore light clothing without shoes. Weight was measured to the nearest 0.1 kg, and height was measured to the nearest centimeter. Body mass index was calculated as the weight divided by height squared (kg/m2). Trained nurses in the Department of Family Practice and Community Health, Ajou University Hospital, measured the waist circumference (WC) between the lower rib and the iliac crest and electrically measured blood pressure (BP) after the participants had been at rest for at least 15 minutes. BP measurements were taken using a model TM-2655P apparatus (PMS Instruments, Tokyo, Japan). The body composition of each participant was analyzed using the body impedance analysis (In body 7.0; Biospace, Seoul, Korea). Additionally, every subject underwent blood testing for oxidative stress markers, oxidized low density lipoprotein (oxLDL), intracellular adhesion molecule-1 (ICAM-1), and interleukin-6 (IL-6). Plasma levels of soluble ICAM-1 and IL-6 were measured using a commercial enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, MN, USA) according to the manufacturer's instructions. The resultant color reaction was read using a Victor reader at 450 nm with wavelength correction set to 540 nm (Perkin Elmer Life Sciences, Turku, Finland). Plasma ox-LDL was measured using an enzyme immunoassay (Mercodia, Uppsala, Sweden). The resulting color reaction was read at 450 nm with a Wallac Victor multilabel counter (Perkin Elmer Life Sciences).
4. Statistical Analyses
All values, except IL-6, showed normal distribution. In the case of IL-6, a log-transformation was made to get the normal distribution. Baseline characteristics were simply compared by a descriptive method. An independent t-test was used to compare all values between smokers and non-smokers. An analysis of covariance (ANCOVA) test was performed to evaluate the NCV difference after adjustment of significant values between the two groups. The Pearson correlation method was used to evaluate the relationship between the NCV and other values. In case of significantly different NCV in the two groups, linear regression analysis was performed to find which factors were closely related to NCV. Subgroup analysis was performed using three subgroups: non-smoking group (group 1, n = 18), <10 years of total pack-years + fewer than one pack of daily smoking in addition to >10 years of total pack-years + fewer than one pack of daily smoking (group 2, n = 13) and >10 years of total pack-years + more than one pack of daily smoking (group 3, n = 17). The subgroup analysis to discern any differences utilized the analysis of variance (ANOVA) test with post hoc analysis. In case of significantly different values among NCV, the ANCOVA test was also performed to ascertain which NCV has an important relationship. All significant P-values were <0.05 and SPSS ver. 11.5 (SPSS Inc., Chicago, IL, USA) was used.
5. Ethics Statement
The institutional review board of Ajou University Hospital approved this study (AJIRB-MED-OBS-10-016).
RESULTS
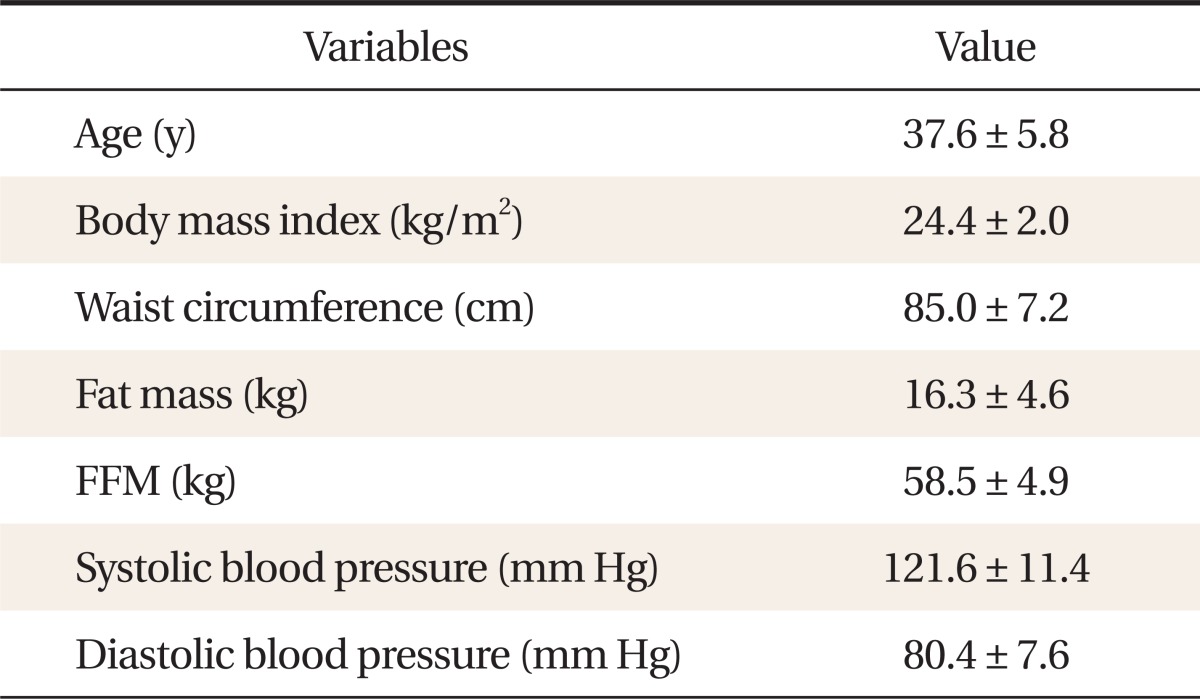
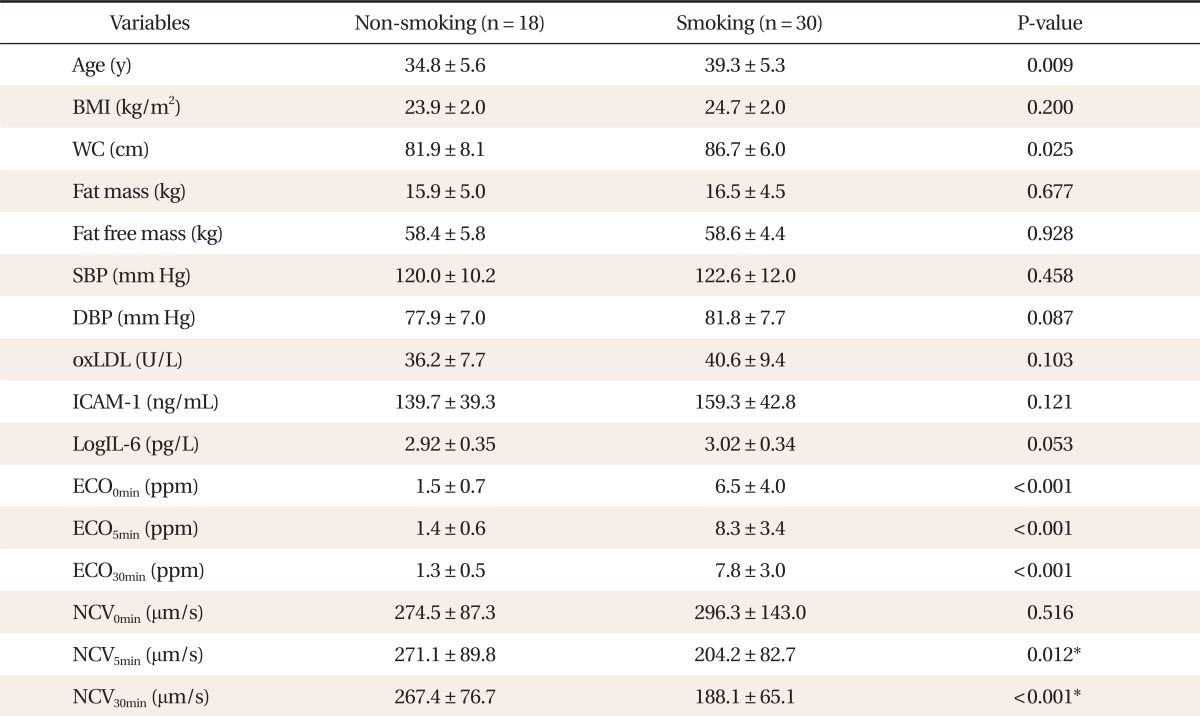
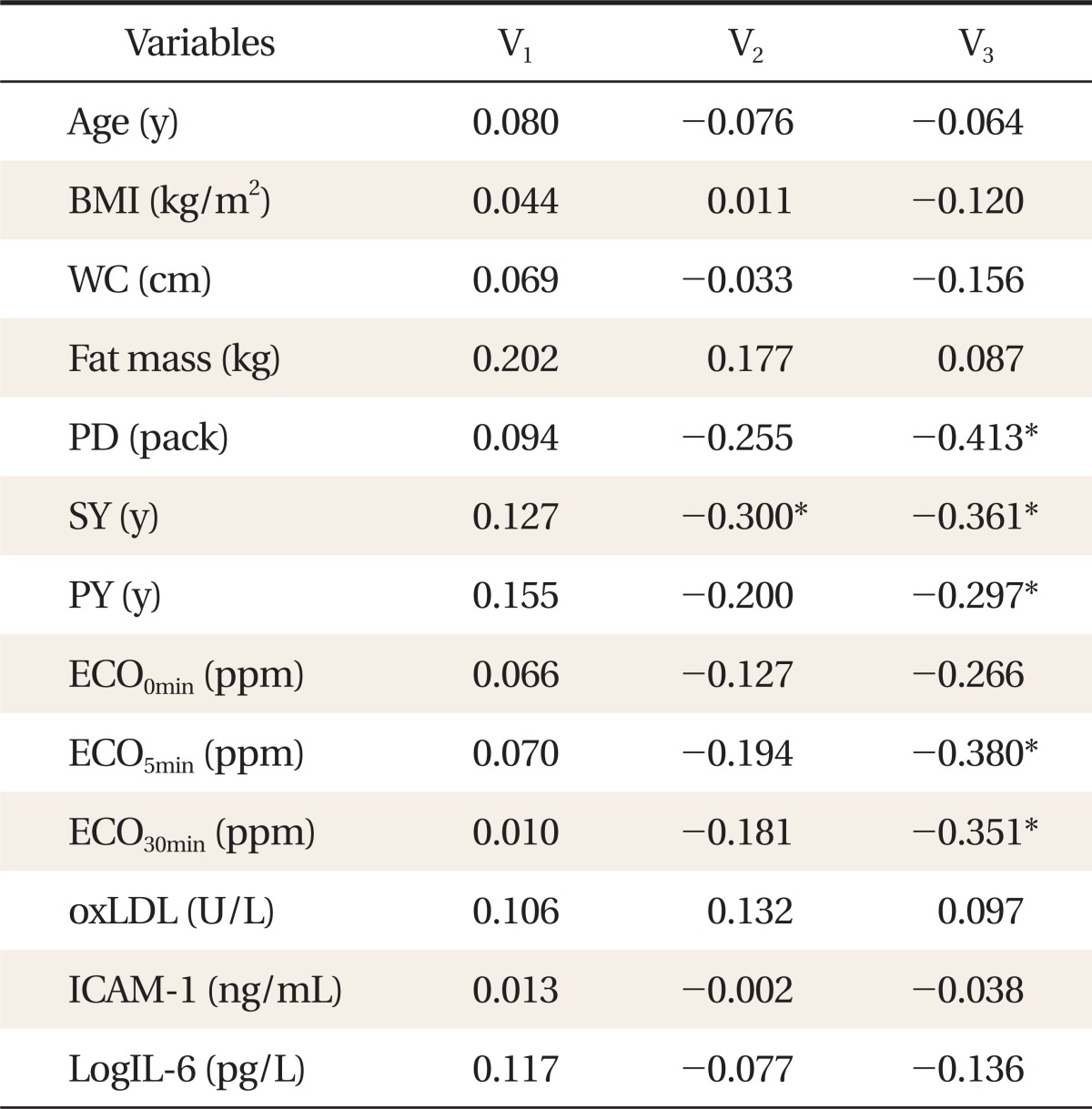
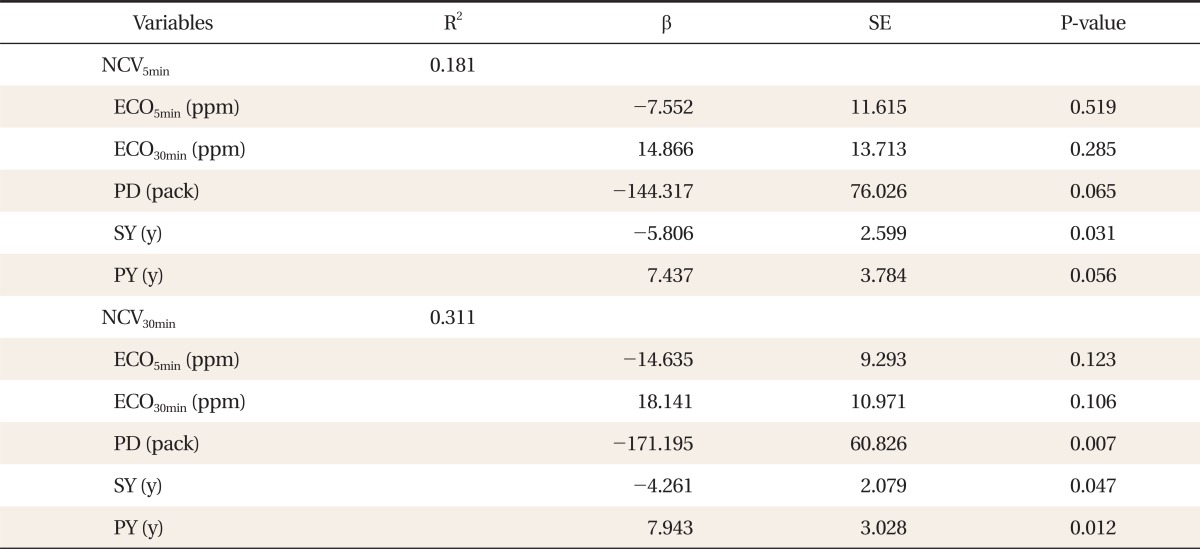
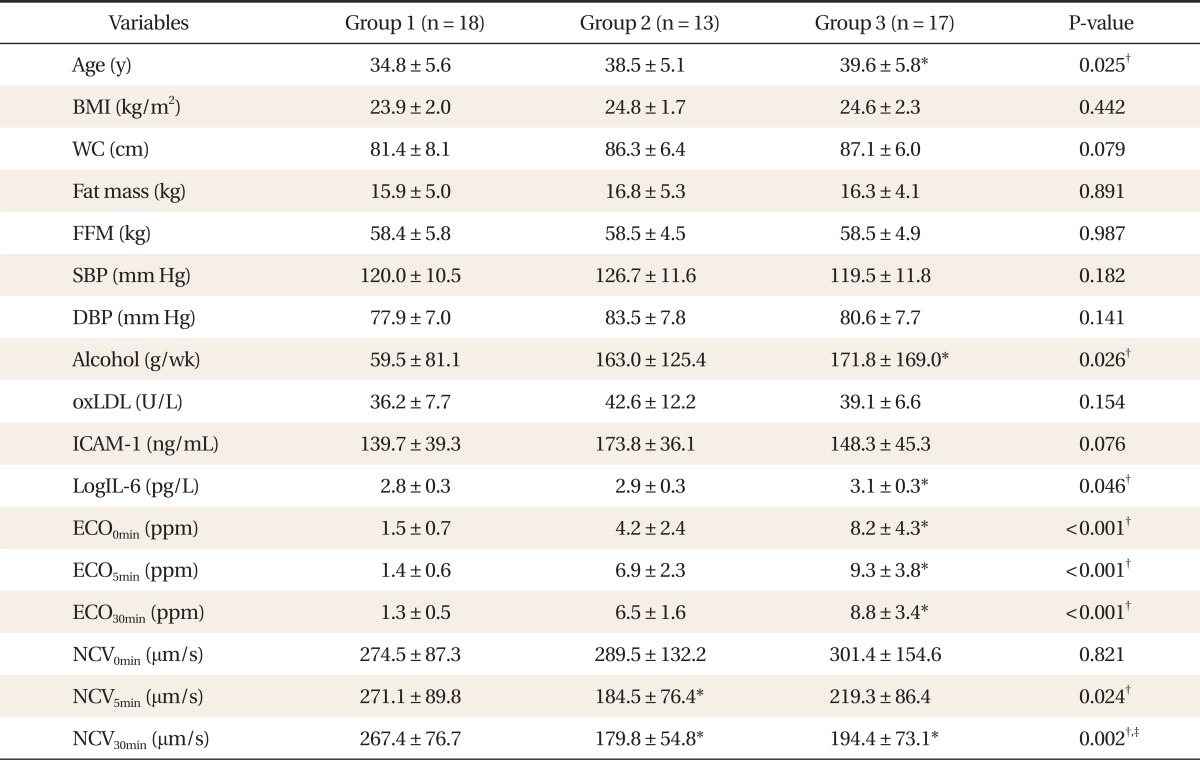
Forty eight subjects were voluntarily recruited and their characteristics are summarized in Table 1. The mean age was 37.6 years and, overall, the subjects were overweight. Mean WC was 85.0 cm and BP was within normal range. In the comparison of smokers and non-smokers, mean age, WC, concentration of ECO0min, ECO5min, ECO30min, and NCV5min, NCV30min were significantly different. By ANCOVA testing after adjustment for age and WC, all ECO concentrations, NCV5min and NCV30min were significantly reduced in smokers (Table 2). Total smoking years were negatively correlated with NCV5min. Average pack of daily smoking, total pack-years and total smoking years were also negatively correlated with NCV30min. ECO5min and ECO30min concentration were negatively correlated with NCV30min (Table 3). Factors closely associated with NCV were revealed by linear regression analysis. Smoking years was negatively associated with NCV5min. Average pack of daily smoking and smoking years also showed negative correlation with the NCV30min, but total pack-years unexpectedly showed a positive association with NCV30min (Table 4). Subgroup analysis was carried out using smoking history. In this subgroup analysis, age, alcohol consumption, LogIL-6, ECO0min, ECO5min, ECO30min, NCV5min, and NCV30min were significantly different by ANOVA testing with post hoc analysis. ANCOVA testing showed only NCV30min was significantly different after adjustment for age, alcohol, and LogIL-6. Interestingly, the LogIL-6 level in group 3 was significantly increased compared with non-smokers (Table 5).
Table 1.
Baseline characteristics of study subjects (n = 48).
Values are presented as mean ± SD. Fat mass was analyzed by bio-impedance analysis.
FFM: fat free mass by bio-impedance analysis.
Table 2.
Comparison of variables between non-smoking group and smoking group.
Values are presented as mean ± SD. P-values were from independent t-test. BMI was calculated from body weight (kg)/height (m2). Fat mass was analyzed by bio-impedance analysis. Alcohol: average alcohol consumption in a week.
BMI: body mass index, WC: waist circumference, SBP: systolic blood pressure, DBP: diastolic blood pressure, oxLDL: oxidized low density lipoprotein, ICAM-1: inter-cellular adhesion molecule-1, IL-6: interleukin-6, ECO0min: concentration of expiratory CO before cigarette smoking detected by micro smokerlyzer, ECO5min: concentration of expiratory CO after 5 minutes of cigarette smoking detected by micro smokerlyzer, ECO30min: concentration of expiratory CO after 30 minutes cigarette smoking detected by micro smokerlyzer, NCV0min: nailfold capillary blood velocity before smoking, NCV5min: nailfold capillary blood velocity after 5 minutes of cigarette smoking, NCV30min: nailfold capillary blood velocity after 30 minutes of cigarette smoking.
*Marked on the P-values with significance after age, WC, ExpCO-1, ExpCO-2, and ExpCO-3 adjustment by analysis of covariance test.
Table 3.
Correlation of the sequential nailfold blood velocity with other variables (n = 48).
All values are Pearson correlation coefficients. Fat mass was analyzed by bio-impedance analysis. BMI was calculated from body weight (kg)/height (m2).
V1: nailfold capillary blood velocity before cigarette smoking, V2: nailfold capillary blood velocity after 5 minutes of cigarette smoking, V3: nailfold capillary blood velocity after 30 minutes of cigarette smoking, BMI: body mass index, WC: waist circumference, PD: average pack of the daily smoking, SY: total smoking years, PY: total pack-years calculated by PD × SY, ECO0min: concentration of expiratory CO before cigarette smoking detected by micro smokerlyzer, ECO5min: concentration of expiratory CO after 5 minutes of cigarette smoking detected by micro smokerlyzer, ECO30min: concentration of expiratory CO after 30 minutes cigarette smoking detected by micro smokerlyzer, oxLDL: oxidized low density lipoprotein, ICAM-1: inter-cellular adhesion molecule-1, IL-6: interleukin-6.
*Marked on the P-value < 0.05.
Table 4.
Factors associated with NCV by linear regression analysis.
β unstandardized coefficients, SE: standard error, NCV: nailfold capillary blood velocity, NCV5min: nailfold capillary blood velocity after 5 minutes of cigarette smoking, NCV30min: nailfold capillary blood velocity after 30 minutes of cigarette smoking, ECO5min: concentration of expiratory CO after 5 minutes of cigarette smoking detected by micro smokerlyzer, ECO30min: concentration of expiratory CO after 30 minutes cigarette smoking detected by micro smokerlyzer, PD: average pack of the daily smoking, SY: total smoking years, PY: total pack-year calculated by PD × SY.
Table 5.
Comparison of variables in the groups divided by smoking status.
Values are presented as mean ± SD. P-values were from analysis of variance test. G1: non-smoking group, G2: less than 10 years of total pack-years + less than one pack of daily smoking and more than 10 years of total pack-years + less than one pack of daily smoking, G3: more than 10 years of total pack-years + more than one pack of daily smoking. BMI was calculated from body weight (kg)/height (m2). Fat mass was analyzed by bio-impedance analysis. Alcohol: average alcohol consumption in a week.
BMI: body mass index, WC: waist circumference, FFM: fat free mass by bio-impedance analysis, SBP: systolic blood pressure, DBP: diastolic blood pressure, oxLDL: oxidized low density lipoprotein, ICAM-1: inter-cellular adhesion molecule-1, IL-6: interleukin-6, ECO0min: concentration of expiratory CO before cigarette smoking detected by micro smokerlyzer, ECO5min: concentration of expiratory CO after 5 minutes of cigarette smoking detected by micro smokerlyzer, ECO30min: concentration of expiratory CO after 30 minutes cigarette smoking detected by micro smokerlyzer, NCV0min: nailfold blood velocity before smoking, NCV5min: nailfold blood velocity after 5 minutes of cigarette smoking, NCV30min: nailfold blood velocity after 30 minutes of cigarette smoking.
*Marked on the value with significance by the comparison with non-smoker in post hoc analysis. †Marked on the P-values with significance by post hoc analysis. ‡Marked on the P-value with significance after age, alcohol consumption, and LogIL-6 adjustment by analysis of covariance test between NCV5min and NCV30min.
DISCUSSION
In this study, NCV measured at 5 minutes and 30 minutes after cigarette smoking was lower in current smokers compared to non-smokers, furthermore, NCV30min was lower in long-period smokers compared with non-smokers after adjustment for age, alcohol consumption, and LogIL-6 concentration. In addition, the reduction of NCV5min was related with total smoking years in smokers and that of NCV30min was related with average pack of daily smoking, total pack-years as well as total cigarette smoking years.
Some studies have shown acute deleterious effects of smoking on blood clotting, coronary vasomotor tone, and coronary endothelial function.12,13) Cigarette smoking especially causes endothelial dysfunction. The endothelium plays a key role in the maintenance of normal homeostasis of the cardiovascular system. Normal endothelium has anti-inflammatory, anti-aggregant, anti-oxidant, and vasodilatory properties that are lost in several pathologies associated with cardiovascular risk (cigarette smoking, diabetes, hypertension, and dyslipidemia and atherogenesis.14,15) Acute smoking is associated with impaired capillary recruitment during peak reactive hyperemia and impaired microvascular endothelium-dependent vasodilatation.16) In addition, cigarette smoking acutely increases aortic stiffness and BP in male smokers with hypertension, and the effects persist longer than in male smokers without hypertension.17) Some reports showed passive smoking specifically increases aortic wave reflection through a nicotine-dependent pathway and impairs microvascular function, even after the end of the exposure,18) with even 30 minutes of passive smoking rapidly impairing vascular endothelial function, which was associated with oxidative stress.19) Therefore, smoking cessation improves arterial stiffness as assessed by the augmentation index, owing mainly to an increase in small artery compliance, which is an early index of endothelial damage20) and coronary endothelial dysfunction may be reversible within 1 month after smoking cessation in healthy young smokers.21)
Many studies have evaluated vascular health status using nailfold capillary microscopy. Cutolo et al.22) reported that effectively and early in the disease, peripheral microangiopathy might be recognized and studied by nailfold capillaroscopy, or even better, with nailfold video capillaroscopy. A study of functional capillary rarefaction in mild BP elevation using capillaroscopy showed functional capillary rarefaction was detectable and associated with endothelial dysfunction measured by plethysmography of flow-mediated vasodilatation.23)
The present study more specifically revealed the reduction in NCV after smoking in all smokers. Especially, NCV30min was closely associated with personal smoking history such as total smoking years, average pack of the daily smoking and total pack-years, which may be related to smoking intensity. In regression analysis, total pack-years showed a positive relation with NCV30min, contrary to other smoking history, although total pack-years and NCV30min showed significant negative correlation. We do not have a firm explanation for this finding, but smaller numbers of smoking subjects may be a factor. Although we did not measure any other endothelial dysfunction markers or structural damage, we could simply assume that smoking is associated with vascular deterioration in smokers by reduced NCV. Therefore, reduced NCV can be a factor that affects vascular injury in smokers. In subgroup analysis, oxLDL concentration was elevated in recent smokers, but not in long-standing smokers. This might implicate oxLDL as a marker of acute vascular damage in smokers. Some previous intervention studies showed inconstancy in the changes of oxLDL and ICAM-1 in smokers,24,25) while more recently smoking intensity was reported to be associated with increased white blood cell count, but not C-reactive protein (CRP) levels, and smoking cessation did not reduce CRP. The relationship between CRP and smoking intensity might be masked by CRP's stronger relationship with adiposity.26)
This study has several limitations. The first is its crosssectional observational nature. Causality could not be drawn from this study. Our study subjects represented one ethnic group and were a small number of people from one region, making generalization of the results impossible. We could not adjust for many possible confounding factors such as regular exercise time and frequency, and other metabolic parameters such as cholesterol level and fasting glucose levels. Despite these limitations, this study is noteworthy as it is the first study to evaluate NCV before and after smoking in a sequential manner in Korean smokers. The intriguing findings warrant further studies using more specific parameters related to endothelial dysfunction.
In conclusion, reduction of NCV in smokers is associated with personal smoking history such as total smoking years, average pack of daily smoking, and total pack-years, not with body composition or some oxidative stress markers.
ACKNOWLEDGMENTS
We thank the Esai, Japan, for research support.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Vickerie JL, Barnes PM US Department of Health and Human Services, Office of the Surgeon General. The health consequences of smoking: a report of the surgeon general. Rockville: US Department of Health and Human Services, Office of the Surgeon General; 2004. [Google Scholar]
- 2.Ministry of Health and Welfare. Gallup: 2007 research on the actual condition of smoking status. Seoul: Ministry of Health and Welfare; 2007. [Google Scholar]
- 3.Howard G, Wagenknecht LE, Burke GL, Diez-Roux A, Evans GW, McGovern P, et al. Cigarette smoking and progression of atherosclerosis: The Atherosclerosis Risk in Communities (ARIC) Study. JAMA. 1998;279:119–124. doi: 10.1001/jama.279.2.119. [DOI] [PubMed] [Google Scholar]
- 4.Bazzano LA, He J, Muntner P, Vupputuri S, Whelton PK. Relationship between cigarette smoking and novel risk factors for cardiovascular disease in the United States. Ann Intern Med. 2003;138:891–897. doi: 10.7326/0003-4819-138-11-200306030-00010. [DOI] [PubMed] [Google Scholar]
- 5.Glass CK, Witztum JL. Atherosclerosis: the road ahead. Cell. 2001;104:503–516. doi: 10.1016/s0092-8674(01)00238-0. [DOI] [PubMed] [Google Scholar]
- 6.Bermudez EA, Rifai N, Buring JE, Manson JE, Ridker PM. Relation between markers of systemic vascular inflammation and smoking in women. Am J Cardiol. 2002;89:1117–1119. doi: 10.1016/s0002-9149(02)02284-1. [DOI] [PubMed] [Google Scholar]
- 7.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 8.LeRoy EC, Downey JA, Cannon PJ. Skin capillary blood flow in scleroderma. J Clin Invest. 1971;50:930–939. doi: 10.1172/JCI106565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutolo M, Sulli A, Pizzorni C, Accardo S. Nailfold video-capillaroscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol. 2000;27:155–160. [PubMed] [Google Scholar]
- 10.Blockmans D, Beyens G, Verhaeghe R. Predictive value of nailfold capillaroscopy in the diagnosis of connective tissue diseases. Clin Rheumatol. 1996;15:148–153. doi: 10.1007/BF02230332. [DOI] [PubMed] [Google Scholar]
- 11.Ostergren J, Fagrell B. Skin capillary blood cell velocity in patients with arterial obliterative disease and polycythaemia: a disturbed reactive hyperaemia response. Clin Physiol. 1985;5:35–43. doi: 10.1111/j.1475-097x.1985.tb00744.x. [DOI] [PubMed] [Google Scholar]
- 12.Newby DE, Wright RA, Labinjoh C, Ludlam CA, Fox KA, Boon NA, et al. Endothelial dysfunction, impaired endogenous fibrinolysis, and cigarette smoking: a mechanism for arterial thrombosis and myocardial infarction. Circulation. 1999;99:1411–1415. doi: 10.1161/01.cir.99.11.1411. [DOI] [PubMed] [Google Scholar]
- 13.Smith CJ, Fischer TH. Particulate and vapor phase constituents of cigarette mainstream smoke and risk of myocardial infarction. Atherosclerosis. 2001;158:257–267. doi: 10.1016/s0021-9150(01)00570-6. [DOI] [PubMed] [Google Scholar]
- 14.Kubes P, Suzuki M, Granger DN. Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci U S A. 1991;88:4651–4655. doi: 10.1073/pnas.88.11.4651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radomski MW, Palmer RM, Moncada S. An l-arginine/nitric oxide pathway present in human platelets regulates aggregation. Proc Natl Acad Sci U S A. 1990;87:5193–5197. doi: 10.1073/pnas.87.13.5193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ijzerman RG, Serne EH, van Weissenbruch MM, de Jongh RT, Stehouwer CD. Cigarette smoking is associated with an acute impairment of microvascular function in humans. Clin Sci (Lond) 2003;104:247–252. doi: 10.1042/CS20020318. [DOI] [PubMed] [Google Scholar]
- 17.Rhee MY, Na SH, Kim YK, Lee MM, Kim HY. Acute effects of cigarette smoking on arterial stiffness and blood pressure in male smokers with hypertension. Am J Hypertens. 2007;20:637–641. doi: 10.1016/j.amjhyper.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Argacha JF, Adamopoulos D, Gujic M, Fontaine D, Amyai N, Berkenboom G, et al. Acute effects of passive smoking on peripheral vascular function. Hypertension. 2008;51:1506–1511. doi: 10.1161/HYPERTENSIONAHA.107.104059. [DOI] [PubMed] [Google Scholar]
- 19.Kato T, Inoue T, Morooka T, Yoshimoto N, Node K. Short-term passive smoking causes endothelial dysfunction via oxidative stress in non-smokers. Can J Physiol Pharmacol. 2006;84:523–529. doi: 10.1139/y06-030. [DOI] [PubMed] [Google Scholar]
- 20.Oren S, Isakov I, Golzman B, Kogan J, Turkot S, Peled R, et al. The influence of smoking cessation on hemodynamics and arterial compliance. Angiology. 2006;57:564–568. doi: 10.1177/0003319706293119. [DOI] [PubMed] [Google Scholar]
- 21.Morita K, Tsukamoto T, Naya M, Noriyasu K, Inubushi M, Shiga T, et al. Smoking cessation normalizes coronary endothelial vasomotor response assessed with 15O-water and PET in healthy young smokers. J Nucl Med. 2006;47:1914–1920. [PubMed] [Google Scholar]
- 22.Cutolo M, Sulli A, Secchi ME, Paolino S, Pizzorni C. Nailfold capillaroscopy is useful for the diagnosis and follow-up of autoimmune rheumatic diseases. A future tool for the analysis of microvascular heart involvement? Rheumatology (Oxford) 2006;45(Suppl 4):iv43–iv46. doi: 10.1093/rheumatology/kel310. [DOI] [PubMed] [Google Scholar]
- 23.Cheng C, Diamond JJ, Falkner B. Functional capillary rarefaction in mild blood pressure elevation. Clin Transl Sci. 2008;1:75–79. doi: 10.1111/j.1752-8062.2008.00016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Hoydonck PG, Schouten EG, Manuel-Y-Keenoy B, van Campenhout A, Hoppenbrouwers KP, Temme EH. Does vitamin C supplementation influence the levels of circulating oxidized LDL, sICAM-1, sVCAM-1 and vWF-antigen in healthy male smokers? Eur J Clin Nutr. 2004;58:1587–1593. doi: 10.1038/sj.ejcn.1601990. [DOI] [PubMed] [Google Scholar]
- 25.Seppo L, Lahteenmaki T, Tikkanen MJ, Vanhanen H, Korpela R, Vapaatalo H. Effects of vitamin E on the toxicity of oxidized LDL on endothelial cells in vitro in smokers vs non-smokers on diets rich in fish. Eur J Clin Nutr. 2005;59:1282–1290. doi: 10.1038/sj.ejcn.1602241. [DOI] [PubMed] [Google Scholar]
- 26.Asthana A, Johnson HM, Piper ME, Fiore MC, Baker TB, Stein JH. Effects of smoking intensity and cessation on inflammatory markers in a large cohort of active smokers. Am Heart J. 2010;160:458–463. doi: 10.1016/j.ahj.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]