Abstract
Individuals with low socioeconomic position have high rates of depression; however, it is not clear whether this reflects higher incidence or longer persistence of disorder. Past research focused on high-risk samples, and risk factors of long-term depression in the population are less well known. Our aim was to test the hypothesis that socioeconomic position predicts depression trajectory over 13 years of follow-up in a community sample. We studied 12 650 individuals participating in the French GAZEL study. Depression was assessed by the Center for Epidemiological Studies-Depression scale in 1996, 1999, 2002, 2005 and 2008. These five assessments served to estimate longitudinal depression trajectories (no depression, decreasing depression, intermediate/increasing depression, persistent depression). Socioeconomic position was measured by occupational grade. Covariates included year of birth, marital status, tobacco smoking, alcohol consumption, body mass index, negative life events and preexisting psychological and non-psychological health problems. Data were analyzed using multinomial regression, separately in men and women. Overall, participants in intermediate and low occupational grades were significantly more likely than those in high grades to have an unfavorable depression trajectory and to experience persistent depression (age-adjusted ORs: respectively 1.40, 95% confidence interval (CI) 1.16–1.70 and 2.65, 95% CI 2.04–3.45 in men, 2.48, 95% CI 1.36–4.54 and 4.53, 95% CI 2.38–8.63 in women). In multivariate models, the socioeconomic gradient in long-term depression decreased by 21–59% in men and women. Long-term depression trajectories appear to follow a socioeconomic gradient; therefore, efforts aiming to reduce the burden of depression should address the needs of the whole population rather than exclusively focus on high-risk groups.
Keywords: depression, longitudinal cohort study, occupational grade, socioeconomic gradient, socioeconomic position
Introduction
Each year, 3–7% of individuals living in industrialized countries suffer from depression; 10–15% are affected over the course of their lifetime.1, 2 Among people who have depression at a particular point in time, an estimated 35–50% will experience symptoms that are recurrent or persistent3, 4 and another 20% may have residual symptoms that impair daily activities and increase the long-term risk of physical health, social and economic difficulties.5 Identifying factors that predict depression trajectories over time is important from both a clinical and a public health perspective.
Previous research suggests that depression is especially likely to occur among individuals who have low socioeconomic position, as measured by educational level, occupational grade or income.6 However, it is not clear whether socioeconomic position predicts depression trajectories over time. First, with few exceptions,7, 8, 9, 10, 11 previous studies reporting socioeconomic inequalities with regard to depression persistence have been based on high-risk or clinical samples,12, 13, 14, 15 which may not be sufficiently varied to contrast groups with different levels of resources.6, 16 Second, prior investigations based on community samples were characterized by limited follow-up (up to 3 years),7, 8, 10 high attrition (13% per year over a 7-year follow-up)9 or followed individuals who were depressed at baseline.11 Growing evidence suggests that in the population, most health outcomes follow a socioeconomic gradient,17 and there is need for additional data on determinants of depression trajectories in broad samples. Third, although depression rates and the role of socioeconomic factors may vary with sex,18, 19 until now, prior studies did not consider women and men separately.
Using data from the French GAZEL cohort study, we examined the association between socioeconomic position, as assessed by occupational grade, and depression trajectories over 13 years of follow-up. Specifically, we studied the association between socioeconomic characteristics and depression trajectories net of the effect of factors that may be simultaneously associated with socioeconomic position and depression trajectory such as age, sex, marital status, negative life events, tobacco and alcohol use,20 body weight index,21 and preexisting psychological and physical health problems.20, 22
Materials and methods
Study population
The GAZEL cohort is an ongoing epidemiological study set up in 1989 among employees of France's national gas and electricity company (n=20 624).23 The study uses an annual questionnaire to collect data on health, lifestyle, individual, familial, social and occupational factors. Additional data are available through various sources, including EDF-GDF administrative records. Since inception of the study in 1989, <1% of participants left the company (n=99) or requested to leave the study (n=264), 6% died (n=1314) and ∼75% completed the yearly study questionnaire. Attrition during follow-up was shown to be related to concomitant health problems, as well as, to a lesser extent, socioeconomic position.24 However, as all participants are sent the yearly study questionnaire (up to date coordinates of all study participants recruited at baseline are available through EDF-GDF administrative records), even those who are not able to participate in a particular year are able to come back into the study during a subsequent wave of data collection. The GAZEL study received approval from the national commission overseeing the ethical data collection in France (Commission Nationale Informatique et Liberté) and from the INSERM's Institutional Review Board.
Measures
Depressive symptoms were measured in 1996, 1999, 2002, 2005 and 2008 using the Center for Epidemiological Studies-Depression (CES-D) scale.25 This scale includes 20 items, which describe symptoms and behaviors characteristic of depressive disorder. On the basis of a previous validation against clinical diagnosis conducted in France, we used cutoff scores of ⩾17 in men and ⩾23 in women to determine the presence of clinically significant depressive symptoms, referred to as depression from here on.26, 27
Occupational grade at the beginning of follow-up and employment status (retired vs actively working) were obtained from EDF-GDF administrative records. Occupational grade was coded according to France's national job classification:28 low (manual worker/clerk), intermediate (administrative associate professional/technician) or high (manager). Study participants were middle-aged and worked for a large national company, therefore, occupational grade was stable throughout the follow-up period.
Covariates
All covariates were measured up to the baseline measure of depression, as our aim was to identify predictors of depression trajectories (i.e., covariates were not dependent on time). Participants' sociodemographic characteristics and health behaviors were assessed in the 1996 GAZEL cohort survey: year of birth (1939–1943, 1944–1949, 1950–1954), marital status (divorced/separated/widowed or married/living with a partner), tobacco smoking status (non-smoker or smoker), alcohol consumption (none, moderate: women: 1–20 units of alcohol per week, men: 1–27 units of alcohol per week, or heavy: women: 21 or more units of alcohol per week, men: 28 or more units of alcohol per week), body mass index (<25 kg m−2, 25–29 kg m−2, ⩾30 kg m−2). Negative life events (divorce/marital breakup, spouse's death, spouse's job loss, hospitalization, spouse's hospitalization) were measured yearly between 1990 and 1996. Preexisting health problems were measured yearly between 1989 and 1996 via a self-completed checklist: psychological problems (depression, treated depression or treated sleep problems29), chronic physical illness (respiratory disorders, cardiovascular disorder, arthritis and diabetes) and cancer.
Statistical analysis
To test the association between occupational grade and depression trajectory, we restricted the study sample to GAZEL study participants with complete data on at least three out of the five possible depression measures (n=12 789). Participants excluded from the analysis were more likely to be female, to work in low occupational grades and to be depressed in 1996. Depression trajectories were determined using a semi-parametric mixture model30 implemented with the PROC TRAJ procedure available in SAS (Cary, NC, USA). For each depression group, the model defines the shape of the trajectory and the proportion of participants in each group. In order to define the optimal number of trajectories, several models were fitted, from a 1-group trajectory model to a 6-group trajectory model. Using the Bayesian Information Criterion,31 a fit index, in which lower values indicate a more parsimonious model, we determined that a 4-group solution was the best fit for our data.
After defining the depression trajectories, we estimated the association between socioeconomic position and the probability of belonging to each of the depression groups using multinomial logistic regression models in which the ‘no depression' trajectory group served as the reference category.
Our analytical strategy was as follows: first, we tested associations between occupational grade and depression trajectories adjusting for year of birth; next, we successively controlled for each block of covariates (1. marital status, 2. negative life events, 3. health behaviors, 4. preexisting health problems). Finally, we tested the association between occupational grade and depression trajectory adjusting for all covariates. To calculate the contribution of each block of explanatory variables to the occupational gradient in depression we repeated the analysis testing the relationship between a single 3-level occupational grade variable and compared adjusted vs non-adjusted odds ratios (ORs) with the following formula: (ORadjusted for year of birth−ORadjusted for year of birth+variable of interest/ORadjusted for year of birth−1) × 100. All analyses were conducted separately in men and women, using the SAS statistical software package.
Results
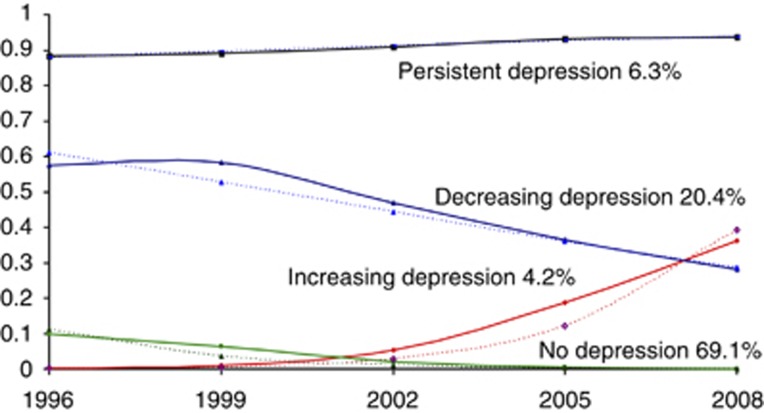
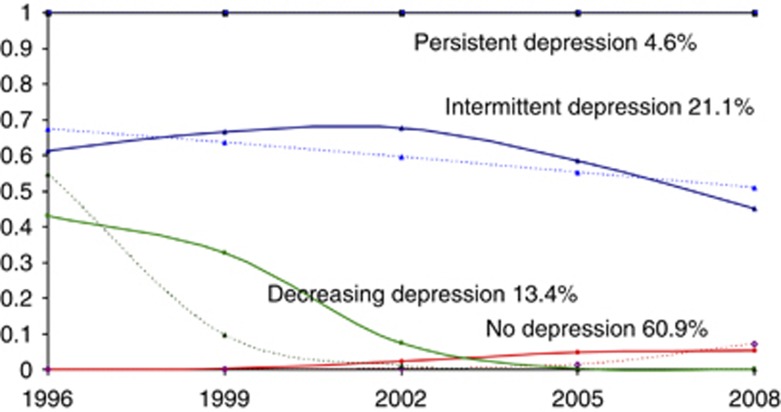
The four depression trajectory groups identified in our study were as follows: men: no depression (72.0%, n=6787), increasing depression (4.2%, n=385), decreasing depression (17.8%, n=1683), persistent depression (6.0%, n=569); women: no depression (58.1%, 1873), decreasing depression (14.0%, n=452), intermittent depression (21.8%, n=702), persistent depression (6.1%, n=199) (Figures 1 and 2).
Figure 1.
Depression trajectories among men of the GAZEL cohort (1996–2008).
Figure 2.
Depression trajectories among women of the GAZEL cohort (1996–2008).
In additional analyses we verified that participants in the ‘no depression' group were depressed an average of 0.13 times during the follow-up (s.d.=0.33), as compared with 1.79 times in participants in the ‘decreasing depression' group (s.d.=0.61), 1.09 times in participants in the ‘increasing depression' group (s.d.=0.28), 2.48 times in participants in the ‘intermittent depression' group (s.d.=0.93) and 4.26 times in participants in the ‘persistent depression' group (s.d.=0.84).
Tables 1 and 2 show characteristics of male and female study participants in relation to depression trajectory. As expected, we found an association between occupational grade and depression trajectory group (P<0.0001). In addition, the pattern of depression over time was significantly associated with participants' year of birth, marital status, divorce or partner separation, hospitalization, spouse's hospitalization, tobacco smoking (men only), alcohol use, body mass index (men only), past psychological problems, chronic physical illness and cancer (women only).
Table 1. Characteristics of men of the GAZEL cohort in relation to depression trajectories (1996–2008), n=9424 (%, P-value).
| No depression (n=6787) | Increasing depression (n=385) | Decreasing depression (n=1683) | Persistent depression (n=569) | P-value | |
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Occupational grade: | |||||
| High | 42.3 | 39.2 | 36.9 | 31.6 | |
| Intermediate | 49.0 | 53.8 | 52.1 | 51.3 | |
| Low | 8.6 | 7.0 | 11.0 | 17.1 | <0.0001 |
| Year of birth: | |||||
| 1939–1943 | 43.2 | 50.1 | 39.5 | 41.5 | |
| 1944–1949 | 56.8 | 49.9 | 60.5 | 58.5 | 0.0007 |
| Marital status: | |||||
| Married/living with partner | 93.6 | 93.8 | 89.8 | 84.0 | |
| Single/widowed/divorced | 6.4 | 6.2 | 10.2 | 16.0 | <0.0001 |
| Negative life events | |||||
| Divorce/separation | 4.1 | 3.1 | 6.1 | 9.3 | <0.0001 |
| Spouse's death | 1.4 | 1.3 | 2.0 | 1.9 | 0.26 |
| Spouse's unemployment | 5.8 | 7.5 | 7.4 | 7.0 | 0.06 |
| Hospitalization | 22.8 | 26.8 | 29.1 | 33.0 | <0.0001 |
| Spouse's hospitalization | 19.4 | 22.6 | 22.2 | 20.6 | 0.041 |
| Health behaviors | |||||
| Tobacco smoking: | |||||
| Non-smoker | 82.7 | 83.1 | 80.4 | 77.2 | |
| Current smoker | 17.3 | 16.9 | 19.6 | 22.8 | 0.0021 |
| Alcohol use: | |||||
| Moderate | 77.6 | 78.4 | 75.4 | 74.2 | |
| High | 14.7 | 14.8 | 15.9 | 14.1 | |
| None | 7.7 | 6.8 | 8.8 | 11.8 | 0.018 |
| BMI (kg m−2) | |||||
| ⩽25 | 41.0 | 42.9 | 38.1 | 39.4 | |
| >25–29 | 50.6 | 48.8 | 52.1 | 47.8 | |
| ⩾30 | 8.4 | 8.3 | 9.8 | 12.8 | 0.0043 |
| Preexisting health problems | |||||
| Psychological problems | 12.5 | 20.5 | 38.1 | 58.6 | <0.0001 |
| Chronic physical illnessa | 51.6 | 61.0 | 62.8 | 69.4 | <0.0001 |
| Cancer | 1.3 | 1.3 | 1.7 | 2.1 | 0.33 |
Abbreviation: BMI, body mass index.
Chronic physical illnesses considered include: respiratory disorders, cardiovascular disorder, arthrosis and diabetes.
Table 2. Characteristics of women of the GAZEL cohort in relation to depression trajectories (1996–2008), n=3226 (%, P-value).
| No depression (n=1873) | Decreasing depression (n=452) | Intermittent depression (n=702) | Persistent depression (n=199) | P-value | |
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Occupational grade: | |||||
| High | 15.5 | 11.3 | 9.8 | 6.0 | |
| Intermediate | 68.5 | 69.9 | 69.0 | 65.8 | |
| Low | 16.0 | 18.8 | 21.2 | 28.2 | <0.0001 |
| Year of birth: | |||||
| 1939–1943 | 28.7 | 23.0 | 19.4 | 28.1 | |
| 1944–1949 | 35.8 | 40.7 | 36.0 | 33.7 | |
| 1950–1954 | 35.5 | 36.3 | 44.6 | 39.2 | <0.0001 |
| Marital status: | |||||
| Married/living with partner | 79.4 | 73.5 | 74.1 | 64.3 | |
| Single/widowed/divorced | 20.6 | 26.5 | 25.9 | 35.7 | <0.0001 |
| Negative life events | |||||
| Divorce/separation | 6.3 | 9.3 | 8.4 | 16.1 | <0.0001 |
| Spouse's death | 2.2 | 3.3 | 2.0 | 3.0 | 0.42 |
| Spouse's unemployment | 7.3 | 7.7 | 9.7 | 5.0 | 0.094 |
| Hospitalization | 27.1 | 33.2 | 37.9 | 41.7 | <0.0001 |
| Spouse's hospitalization | 13.4 | 12.8 | 17.7 | 15.6 | 0.033 |
| Health behaviors | |||||
| Tobacco smoking: | |||||
| Non-smoker | 87.3 | 85.0 | 84.8 | 83.4 | |
| Current smoker | 12.7 | 15.0 | 15.2 | 16.6 | 0.17 |
| Alcohol use: | |||||
| Moderate | 75.5 | 74.8 | 70.8 | 66.3 | |
| High | 4.5 | 3.1 | 4.1 | 4.0 | |
| None | 20.0 | 22.1 | 25.1 | 29.7 | 0.011 |
| BMI (kg m−2) | |||||
| ⩽25 | 73.6 | 73.0 | 75.1 | 69.4 | |
| >25–29 | 20.2 | 21.9 | 17.9 | 20.6 | |
| ⩾30 | 6.1 | 5.1 | 7.0 | 10.0 | 0.17 |
| Preexisting health problems | |||||
| Psychological problems | 29.4 | 64.4 | 68.2 | 85.4 | <0.0001 |
| Chronic physical illnessa | 52.8 | 64.4 | 63.7 | 80.4 | <0.0001 |
| Cancer | 3.1 | 3.3 | 3.1 | 6.5 | 0.082 |
Abbreviation: BMI, body mass index.
Chronic physical illnesses include: respiratory disorders, cardiovascular disorder, arthrosis and diabetes.
In men (Table 3), multinomial regression models adjusted for year of birth revealed no association between occupational grade and increasing depression symptoms over time; however, the probability of decreasing or persistent levels of depression followed an occupational gradient. Compared with participants with high occupational grade and no depression during follow-up, in participants with intermediate occupational grade, the odds of belonging to the group with decreasing levels of depression or to the group with persistent depression were, respectively, 1.22 (95% confidence interval (CI) 1.09–1.36) and 1.40 (95% CI 1.16–1.70) times higher. In participants with low occupational grade, the corresponding ORs were 1.45 (95% CI 1.21–1.75) for decreasing levels of depression and 2.65 (95% CI 2.04–3.45) for persistent depression. The likelihood of persistent depression associated with occupational grade was significantly higher than the likelihood of decreasing or increasing depression (P-values, respectively: <0.0001 and 0.0003). These occupational gradients somewhat decreased after adjusting for marital status (decreasing depression: 3%, persistent depression: 3%), negative life events (decreasing depression: 3%, persistent depression: 1%), health behaviors (decreasing depression: 6%, persistent depression: 5%) and preexisting health problems (decreasing depression: 14%, persistent depression: 9%). In fully adjusted models, the ORs associated with occupational grade decreased by 21% with regard to decreasing depression and by 16% with regard to persistent depression, but remained elevated and statistically significant.
Table 3. Socioeconomic position and depression trajectory (1996–2008); multinomial logistic regression analyses among men of the GAZEL cohort (n=9424).
| Increasing vs no depression OR1 (95% CI) | Decreasing vs no depression OR2 (95% CI) | Persistent vs no depression OR3 (95% CI) | P-value 1 OR1, OR2, OR3 ≠ 1 | |
|---|---|---|---|---|
| Adjusted for year of birth | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | <0.0001 |
| Intermediate | 1.20 (0.97–1.49) | 1.22 (1.09–1.36) | 1.40 (1.16–1.70) | |
| Low | 0.90 (0.59–1.37) | 1.45 (1.21–1.75) | 2.65 (2.04–3.45) | |
| Adjusted for year of birth and marital status | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.20 (0.97–1.49) | 1.21 (1.08–1.35) | 1.38 (1.13–1.67) | |
| Low | 0.90 (0.59–1.37) | 1.44 (1.19–1.74) | 2.59 (1.99–3.37) | <0.0001 |
| Adjusted for year of birth and negative life eventsa | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.20 (0.96–1.49) | 1.21 (1.08–1.35) | 1.39 (1.14–1.68) | |
| Low | 0.89 (0.59–1.36) | 1.44 (1.19–1.74) | 2.63 (2.02–3.42) | <0.0001 |
| Adjusted for year of birth and health behaviorsb | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.21 (0.98–1.50) | 1.20 (1.07–1.35) | 1.37 (1.13–1.67) | |
| Low | 0.91 (0.60–1.39) | 1.42 (1.18–1.72) | 2.54 (1.95–3.30) | <0.0001 |
| Adjusted for year of birth and preexisting health problemsc | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.18 (0.95–1.46) | 1.18 (1.05–1.33) | 1.35 (1.10–1.65) | |
| Low | 0.85 (0.56–1.30) | 1.37 (1.13–1.66) | 2.42 (1.83–3.20) | <0.0001 |
| Full modeld | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.18 (0.95–1.47) | 1.17 (1.04–1.32) | 1.30 (1.06–1.59) | |
| Low | 0.86 (0.56–1.31) | 1.34 (1.10–1.63) | 2.28 (1.72–3.02) | <0.0001 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Adjusted for divorce/marital breakup, spouse's job loss, hospitalization and spouse's hospitalization.
Adjusted for tobacco smoking, alcohol use and body mass index.
Adjusted for past psychological problems, chronic physical illness (respiratory disorders, cardiovascular disorder, arthrosis and diabetes) and cancer.
Adjusted for year of birth, marital status, divorce/marital breakup, spouse's job loss, hospitalization, spouse's hospitalization, tobacco smoking, alcohol use, body mass index, past psychological problems, chronic physical illness (respiratory disorders, cardiovascular disorder, arthrosis and diabetes) and cancer.
Similarly, in women (Table 4) we observed an occupational gradient in the probability of decreasing, intermittent or persistent levels of depression: compared with participants with high occupational grade who were not depressed during follow-up, participants with intermediate occupational grade had odds of decreasing levels of depression, intermittent depression or persistent depression, respectively, 1.39 (95% CI 1.00–1.91), 1.59 (95% CI 1.20–2.11) and 2.48 (95% CI 1.36–4.54) times higher. In participants with low occupational grade, the corresponding ORs were 1.61 (95% CI 1.10–2.36) for decreasing depression, 2.09 (95% CI 1.51–2.91) for intermittent depression and 4.53 (95% CI 2.38–8.63) for persistent depression. The likelihood of persistent depression associated with occupational grade was significantly higher than the likelihood of decreasing or intermittent depression (P-values, respectively: 0.002 and 0.02). These occupational gradients somewhat decreased after adjusting for negative life events (decreasing depression: 6%, intermittent depression: 8%, persistent depression trajectory: 9%), health behaviors (decreasing depression: 2%, intermittent depression: 2%, persistent depression trajectory: 6%) and preexisting health problems (decreasing depression: 44%, intermittent depression: 33%, persistent depression trajectory: 26%). In fully adjusted models, the ORs associated with occupational grade decreased by 40% with regard to decreasing levels of depression, by 33% with regard to intermittent depression and by 59% with regard to persistent depression; they remained elevated and statistically significant for intermittent and persistent depression. The ORs associated with further analyses revealed that approximately half of the contribution of health characteristics to the occupational gradient in depression in women reflected the role of preexisting psychological problems.
Table 4. Socioeconomic position and depression trajectory (1996–2008): multinomial logistic regression analyses among women of the GAZEL cohort (n=3226).
| Decreasing vs no depression OR1 (95% CI) | Intermittent vs no depression OR2 (95% CI) | Persistent vs no depression OR3 (95% CI) | P-value 1 OR1, OR2, OR3 ≠ 1 | |
|---|---|---|---|---|
| Adjusted for year of birth | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.39 (1.00–1.91) | 1.59 (1.20–2.11) | 2.48 (1.36–4.54) | |
| Low | 1.61 (1.10–2.36) | 2.09 (1.51–2.91) | 4.53 (2.38–8.63) | <0.0001 |
| Adjusted for year of birth and marital status | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.42 (1.03–1.97) | 1.63 (1.23–2.17) | 2.65 (1.45–4.87) | |
| Low | 1.65 (1.12–2.42) | 2.14 (1.54–2.98) | 4.80 (2.52–9.17) | <0.0001 |
| Adjusted for year of birth and negative life eventsa | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.37 (0.99–1.89) | 1.54 (1.16–2.06) | 2.36 (1.29–4.33) | |
| Low | 1.57 (1.07–2.31) | 1.99 (1.43–2.77) | 4.12 (2.16–7.87) | <0.0001 |
| Adjusted for year of birth and health behaviorsb | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.39 (1.00–1.92) | 1.58 (1.19–2.10) | 2.42 (1.32–4.44) | |
| Low | 1.60 (1.09–2.35) | 2.06 (1.48–2.87) | 4.57 (2.24–8.16) | <0.0001 |
| Adjusted for year of birth and preexisting health problemsc | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.24 (0.88–1.72) | 1.39 (1.03–1.87) | 2.09 (1.12–3.90) | |
| Low | 1.33 (0.89–1.98) | 1.69 (1.19–2.39) | 3.34 (1.71–6.53) | 0.0035 |
| Full modeld | ||||
| Occupational grade: | ||||
| High | 1 | 1 | 1 | |
| Intermediate | 1.26 (0.90–1.77) | 1.41 (1.04–1.91) | 2.07 (1.10–3.88) | |
| Low | 1.36 (0.91–2.03) | 1.69 (1.18–2.40) | 3.13 (1.59–6.17) | 0.0081 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Adjusted for divorce/marital breakup, spouse's job loss, hospitalization and spouse's hospitalization.
Adjusted for tobacco smoking, alcohol use, and body mass index.
Adjusted for past psychological problems, chronic physical illness (respiratory disorders, cardiovascular disorder, arthrosis and diabetes) and cancer.
Adjusted for year of birth, marital status, divorce/marital breakup, spouse's job loss, hospitalization, spouse's hospitalization, tobacco smoking, alcohol use, body mass index, past psychological problems, chronic physical illness (respiratory disorders, cardiovascular disorder, arthrosis and diabetes) and cancer.
In secondary analyses, we found that participants who retired during follow-up had a lower probability of depression than those who remained employed (OR: 0.55), but adjustment for retirement status did not modify the association between occupational grade and depression trajectory (data available upon request). In addition, in order to test the possibility that the restriction of the study sample to participants with complete data induced bias, we repeated the analyses on the whole sample, using the default option for the management of missing data available in PROC TRAJ. We also conducted sensitivity analyses imputing missing data using the MICE procedure in STATA. The results obtained using these methods were not systematically different from those of the main analysis (not shown).
Discussion
In this study of 12 789 individuals followed for 13 years, we found evidence of four longitudinal depression trajectories: no depression, decreasing levels of depression, increasing (men) or intermittent (women) levels of depression and persistent depression. The probability of belonging to a group with depression over the course of follow-up was inversely related to occupational grade. This association was especially strong for persistent depression. Observed depression trajectories and possible explanations of the occupational gradient in depression varied in men and women. Adding to past research, which reported socioeconomic inequalities with regard to depression persistence in high-risk samples, our study suggests that socioeconomic position predicts the long-term occurrence of depressive disorder in a large community-based sample. Importantly, the risk of depression is not concentrated exclusively in the most disadvantaged groups of the population, but distributed across the whole socioeconomic range.
Limitations and strengths
Our results need to be interpreted in light of several limitations. First, the GAZEL cohort includes individuals who, at the time they were recruited into the cohort, held a stable job. Moreover, participants excluded from this analysis were more likely to belong to a low occupational grade and to be depressed. Past research based on GAZEL study data has shown associations between socioeconomic position and physical and mental health,32, 33, 34 implying that this sample is well suited to study social health inequalities and that the results will apply in other settings. Nevertheless, socioeconomic gradients with regard to long-term risk of depression in the general population are probably steeper than we report. Second, we did not account for several factors shown to predict the long-term risk of depressive symptomatology such as a family history of depression,35 the age of onset of depressive disorder36 and personality.37 However, by accounting for preexisting psychological problems we most likely captured disorder variability associated with these predictors.4 Third, depression in our study was assessed using the CES-D scale, which is less specific than a clinician's diagnosis and bears the risk of false positives.38 Still, it is a well-established screening instrument, shown to be reliable and valid across different cultural and sociodemographic settings. The cutoffs validated in France and used in this study (⩾17 in men and ⩾23 in women) are higher than those used in other populations (⩾16 in men and women), which probably decreases the likelihood of misclassification. Evidence of psychosocial impairment in individuals who have mild and moderate depression39 suggests that measures of depressive symptomatology such as the CES-D can help identify individuals who require medical attention. Fourth, depression measures were obtained every 3 years, raising the possibility that we underestimated depression trajectories. Reassuringly, case undercounting appears rare (6% of participants self-reported psychological problems but were not identified as CES-D cases). Moreover, misclassification bias because of unaccounted cases is more likely to be a problem when studying the recurrence of depression at a specific point in time than when examining long-term trajectories of depression over multiple measurements, as is the case in the present study. Overall, the most likely consequence of case undercounting is the attenuation of the association between occupational grade and depression.
Our study also has several strengths: (1) the study sample was selected independently of mental health treatment status and is socioeconomically more varied than clinical samples; (2) the occurrence of depression was ascertained prospectively over a 13-year period, limiting information bias; (3) the analysis accounted for several factors associated with depression course measured longitudinally.
Socioeconomic gradient in depression course
Our main finding is that the long-term likelihood of depression appears to follow a socioeconomic gradient, that is individuals in the highest occupational groups are least likely to be depressed, followed by those in an intermediate position; individuals in lowest occupational groups are most likely to be depressed and to have depression that persists over time. Although the association between socioeconomic position and depression persistence has previously been reported,7, 8, 10, 11, 34 we are not aware of research quantifying socioeconomic inequalities in long-term depression patterns.
The association between socioeconomic position and depression may reflect two mechanisms: (1) health selection, whereby psychological symptoms cause individuals to drift down the social hierarchy and (2) social causation, whereby disadvantaged living conditions directly affect mental health.40 Moreover, differential use of mental healthcare services may additionally contribute to worse depression outcomes in lower socioeconomic groups.41 This study, based on a sample of middle-aged, working, men and women was not designed to test the role of selection vs causation mechanisms. However, our results are consistent with both explanations. Although study participants held a stable job, which they were unlikely to lose in case of psychological problems, depression may have affected their chances of being promoted. Prior data from the GAZEL cohort show that social mobility over time is associated with cancer incidence and premature mortality, as well as risky health behaviors.32, 42, 43 By definition, study participants from the lowest occupational groups were not promoted during the course of their career, and it may be that in some cases this was due to their psychological problems. However, if health selection were the primary explanation, one would expect the probability of depression to be solely elevated among individuals in low occupational grades. The observation of a socioeconomic gradient suggests that position on the occupational ladder contributes to depression risk. Factors associated with depression in our study (absence of a partner, the experience of negative life events, tobacco smoking, high alcohol use, high body mass index, prior health problems) followed an occupational gradient and statistically explained up to 21% of the association between occupational grade and depression in men and up to 59% in women, implying that depression risk is partly shaped by socioeconomic circumstances.
Differences between men and women
In our study, men and women had different depression trajectories: women were less likely to have persistent depression than men (4.6% as compared with 6.3%), yet their overall levels of depression were higher (60.9% had no depression during follow-up as compared with 69.1% of men). It is important to highlight that the cutoffs used to define clinically significant depression were sex-specific and higher for women. Thus, sex differences are probably larger when the same criteria are applied to men and women. Although research has consistently reported that women have higher rates of depression at any given point in time, there has been some debate as to whether women also experience worse course of depression.18, 19, 44 Our data are consistent with the hypothesis that long-term patterns of depression are less favorable in women, possibly due to multiple affective, biological and cognitive mechanisms, which operate in interaction with exposure to stress.45 We also found evidence of steeper socioeconomic gradients in women than in men, even in fully adjusted models. Among factors we controlled for, preexisting health problems had an especially important role in statistically explaining the socioeconomic gradient in depression in women, drawing attention to the interrelationship between mental and physical health. Overall, this study confirms that the prevalence as well as risk factors of depression differ in men and women, suggesting that investigations examining long-term patterns of depression should test for sex differences.
Conclusion
Adding to prior research, which showed that individuals who belong to disadvantaged socioeconomic groups have elevated rates of depression, our study suggests that the risk of depression follows a socioeconomic gradient, particularly when the disorder is chronic. In terms of theory, this finding argues in favor of a social causation explanation of persistent depression. In terms of practice, the main implication is that efforts aimed to reduce the burden of depression and decrease socioeconomic inequalities should address the mental health needs of the population.
Acknowledgments
We express thanks to EDF-GDF, especially to the Service des Etudes Médicales and the Service Général de Médecine de Contrôle and the ‘Caisse centrale d'action sociale du personnel des industries électrique et gazière'. We also wish to acknowledge the GAZEL cohort study team responsible for data management. This research was supported by EDF-GDF; INSERM; the Association de la Recherche sur le Cancer; the Fondation de France; and the French Ministry of Health-IReSP (TGIR Cohortes) (GAZEL cohort). Maria Melchior is the recipient of a Young Researcher Award from the French National Research Agency (ANR). Funding bodies had no role in influencing data collection, managements, analysis or interpretation.
The authors declare no conflict of interest.
References
- World Health Organization World Health Report 2001-Mental Health: New Understanding, New Hope[Available from http://www.who.int/whr/2001/en/]. [DOI] [PubMed]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders(4th ed.).American Psychological Association: Washington, DC; 1994 [Google Scholar]
- Hardeveld F, Spijker J, de Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122:184–191. doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- Scott J. Depression should be managed like a chronic disease - clinicians need to move beyond ad hoc approaches to isolated acute episodes. BMJ. 2006;332:985–986. doi: 10.1136/bmj.332.7548.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Spijker J, de GR, Bijl RV, Beekman AT, Ormel J, Nolen WA. Determinants of persistence of major depressive episodes in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) J Affect Disord. 2004;81:231–240. doi: 10.1016/j.jad.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Skapinakis P, Weich S, Lewis G, Singleton N, Araya R. Socio-economic position and common mental disorders. Longitudinal study in the general population in the UK. Br J Psychiatry. 2006;189:109–117. doi: 10.1192/bjp.bp.105.014449. [DOI] [PubMed] [Google Scholar]
- Lorant V, Croux C, Weich S, Deliege D, Mackenbach J, Ansseau M. Depression and socio-economic risk factors: 7-year longitudinal population study. Br J Psychiatry. 2007;190:293–298. doi: 10.1192/bjp.bp.105.020040. [DOI] [PubMed] [Google Scholar]
- Beard JR, Tracy M, Vlahov D, Galea S. Trajectory and socioeconomic predictors of depression in a prospective study of residents of New York City. Ann Epidemiol. 2008;18:235–243. doi: 10.1016/j.annepidem.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65:513–520. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka L. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychol Med. 2003;33:1341–1355. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychol Med. 2004;34:623–634. doi: 10.1017/S0033291703001764. [DOI] [PubMed] [Google Scholar]
- Miech RA, Eaton WW, Brennan K.Mental health disparities across education and sex: a prospective analysis examining how they persist over the life course J Gerontol B Psychol Sci Soc Sci 200560Spec No 2: 93–98. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Shelton RC, Wisniewski S, Warden D, Biggs MM, Friedman ES, et al. Presenting characteristics of depressed outpatients as a function of recurrence: preliminary findings from the STAR*D clinical trial. J Psychiatr Res. 2006;40:59–69. doi: 10.1016/j.jpsychires.2005.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot MG. Inequalities in health. N Engl J Med. 2001;345:134–144. doi: 10.1056/NEJM200107123450210. [DOI] [PubMed] [Google Scholar]
- Bracke P. Sex differences in the course of depression: evidence from a longitudinal study of a representative sample of the Belgian population. Soc Psychiatry Psychiatr Epidemiol. 1998;33:420–429. doi: 10.1007/s001270050075. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–713. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Head J, Fuhrer R, Wardle J, Cattell V. Social inequalities in depressive symptoms and physical functioning in the Whitehall II study: exploring a common cause explanation. J Epidemiol Community Health. 2003;57:361–367. doi: 10.1136/jech.57.5.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Clark C, Rodgers B, Caldwell T, Power C. Repeated exposure to socioeconomic disadvantage and health selection as life course pathways to mid-life depressive and anxiety disorders. Soc Psychiatry Psychiatr Epidemiol. 46:549–558. doi: 10.1007/s00127-010-0221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg M, Leclerc A, Bonenfant S, Chastang JF, Schmaus A, Kaniewski N, et al. Cohort profile: the GAZEL Cohort Study. Int J Epidemiol. 2007;36:32–39. doi: 10.1093/ije/dyl247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg M, Chastang JF, Zins M, Niedhammer I, Leclerc A. Health problems were the strongest predictors of attrition during follow-up of the GAZEL cohort. J Clin Epidemiol. 2006;59:1213–1221. doi: 10.1016/j.jclinepi.2006.02.020. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: a self report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- Fuhrer R, Rouillon F. La version française de l'échelle CES-D (center for Epidemiologic Studies-Depression scale). Description et traduction de l'échelle d'auto-évaluation. Psychiat Psychobiol. 1989;4:163–166. [Google Scholar]
- Melchior M, Ferrie JE, Alexanderson K, Goldberg M, Kivimaki M, Singh-Manoux A, et al. Predicting future depression in a working population—the use of sickness absence records. Prospective findings from the GAZEL cohort. Am J Public Health. 2009;99:1417–1422. doi: 10.2105/AJPH.2008.142273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- France's National Institute of Economic Studies and Statistics (INSEE) Occupations and social categories [Nomenclature des Professions et Catégories Sociales (PCS 2003)][Available from: http://www.inseefr/fr/methodes/defaultasp?page=nomenclatures/pcs2003/pcs2003htm , 2010].
- Galéra C, Melchior M, Chastang JF, Bouvard MP, Fombonne E. Childhood and adolescent hyperactivity-inattention symptoms and academic achievement 8 years later: the GAZEL Youth study. Psychol Med. 2009;9:1895–1906. doi: 10.1017/S0033291709005510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–393. [Google Scholar]
- Nagin DS. Group-Based Modeling of Development. Harvard University Press: Cambridge, MA; 2005. [Google Scholar]
- Melchior M, Berkman LF, Kawachi I, Krieger N, Zins M, Bonenfant S, et al. Lifelong socioeconomic trajectory and premature mortality (35–65 years) in France: findings from the GAZEL Cohort Study. J Epidemiol Community Health. 2006;60:937–944. doi: 10.1136/jech.2005.042440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M, Berkman LF, Niedhammer I, Zins M, Goldberg M. Multiple work and family demands and mental health: a prospective study of psychiatric sickness absence in the French GAZEL study. Soc Psychiatry Psychiatr Epidemiol. 2007;42:573–582. doi: 10.1007/s00127-007-0203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M, Chastang J-F, Leclerc A, Ribet C, Rouillon F. Low socioeconomic position and depression persistence: longitudinal results from the GAZEL cohort study. Psychiatry Res. 2010;177:92–96. doi: 10.1016/j.psychres.2009.08.002. [DOI] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, et al. The validity of the family history screen for assessing family history of mental disorders. Am J Med Gen Part B Neuropsychiatr Gen. 2008;150B:41–49. doi: 10.1002/ajmg.b.30764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, et al. Effect of age at onset on the course of major depressive disorder. Am J Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode: a 3-wave population-based study. Arch Gen Psychiatry. 2004;61:990–996. doi: 10.1001/archpsyc.61.10.990. [DOI] [PubMed] [Google Scholar]
- McDowell I.Depression. Measuring Health. A Guide to Rating Scales and QuestionnairesThird ed.Oxford University Press: New York, NY; 2006330–393. [Google Scholar]
- Judd LL, Akiskal HS, Zeller PJ, Paulus M, Leon AC, Maser JD, et al. Psychosocial disability during the long-term course of unipolar major depressive disorder. Arch Gen Psychiatry. 2000;57:375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- ten Have M, de GR, Ormel J, Vilagut G, Kovess V, Alonso J. Are attitudes towards mental health help-seeking associated with service use? Results from the European Study of Epidemiology of mental disorders. Soc Psychiatry Psychiatr Epidemiol. 45:153–163. doi: 10.1007/s00127-009-0050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclerc A, Zins M, Bugel I, Chastang J-F, David S, Morcet J-F, et al. Consommation de boissons alcoolisées et situation professionnelle dans la cohorte GAZEL (EDF-GDF) Arch Malad Prof. 1994;55:509–517. [Google Scholar]
- Melchior M, Goldberg M, Krieger N, Kawachi I, Menvielle G, Zins M, et al. Occupational class, occupational mobility and cancer incidence among middle-aged men and women: a prospective study of the French GAZEL cohort. Cancer Causes Control. 2005;16:515–524. doi: 10.1007/s10552-004-7116-0. [DOI] [PubMed] [Google Scholar]
- Essau CA, Lewinsohn PM, Seeley JR, Sasagawa S. Gender differences in the developmental course of depression. J Affect Disord. 2010;127:185–190. doi: 10.1016/j.jad.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]