Abstract
Patellofemoral arthritis is a fairly common disease, and it has been gaining interest with increasing number of studies due to its diverse treatment methods. Patellofemoral arthritis has a broad range of management options according to the characteristics of individual diseases. Identifying whether patellofemoral arthritis is the primary cause of knee pain and is compartment arthritis is necessary for establishing an adequate treatment method. Through investigation of the literature, the issues of recent knowledge of femoropatella arthritis and the diagnosis and treatment of which were studied.
Keywords: Patellofemoral arthritis, Diagnosis, Treatment
Introduction
Unicompartmental arthritis of the knee generally refers to not only tibiofemoral arthritis but also to disorders of the patella and the cartilage. In particular, isolated patellofemoral arthritis is a relatively common disorder for which there has been increasing research regarding its treatment methods.
Patellofemoral arthritis occurs due to the loss of the cartilage of the patella and the trochlear groove in approximately half of the patients diagnosed with degenerative arthritis of the knee. Isolated patellofemoral arthritis is not rare and radiographic evidence of deformity can be observed in 17.1-34% of female patients and 18.5-19% of male patients in the age of ≥55 or ≥60 years old according to some studies1,2). Noble and Hamblen2) reported patellofemoral osteoarthritis in 79% of 100 cadavers aged ≥65 years. In spite of its prevalence, treatment of this painful disorder is challenging due to the diversity of causes of the disorder and the lack of knowledge on articular regeneration. It has been reported that valgus knee alignment accelerates lateral patellofemoral arthritis and dysplasia of the patella or trochlea, malrotation of the tibia. Direction or force of the quadriceps femoris can also influence the progression of this disease.
Patellofemoral arthritis, a common cause of anterior knee pain, has been known to be refractory to treatment. This can be attributed to the complexity of the patellofemoral joint structure and insufficient recognition of the biomechanics of the joint. In this article, I will discuss the diagnosis and treatment options of patellofemoral arthritis based on recent studies on the biomechanics of the patellofemoral joint and disorders associated with patellofemoral arthritis.
Pathophysiology
The patellofemoral joint is a unique and complex structure consisting of static elements (ligaments and bones) and dynamic elements (neuromuscular system). The primary soft tissue static stability of the joint is provided by the medial and lateral patellofemoral and patellotibial complexes3). The stability of the joint is also influenced by lower limb alignment including varus/valgus femorotibial alignment and rotational variances of the femur. In addition, the relation of the knee to the pelvic position and strength is another important stabilizer for the knee. Therefore, patellofemoral joint abnormality can be associated with one or combination of these factors4).
The articular cartilage of the patella is similar to that of other joints in that it contains a solid phase and a fluid phase that is mostly composed of collagen and glycosaminoglycans. The solid phase is somewhat permeable and when the articular surface is under load, the fluid gradually redistributes itself within the solid matrix5). Therefore, the pressure within the fluid is strongly associated with the cushioning effect of the articular cartilage and the low friction coefficient of articular surfaces. Any damage to the articular surfaces causes a loss of pressure within the fluid phase, which subsequently results in higher stresses on the collagen fibers and more vulnerability leading to possible breakdown6).
Patellofemoral arthritis results from the loss of articular cartilage of the patella and the trochlear groove and chondral wear is most prevalent in the lateral patellar facet4). This indicates that the lateral patellar facet is more often overloaded than the central or medial aspect of the patella. Considering that lateral facet arthritis can be caused by malalignment or tilt, arthritis can naturally be associated with malalignment or tilt. Furthermore, the patellofemoral joint is affected by the extensor mechanism of the knee including the quadriceps femoris, patellar bone, and ligaments. Malalignment of the extensor mechanism can result in anterior knee pain due to overload on the lateral aspect of the knee, patellar subluxation or tilt, abnormal Q-angle, or torsion of the distal femur, all of which are good indications for tibial tubercle osteotomy or patellofemoral joint replacement.
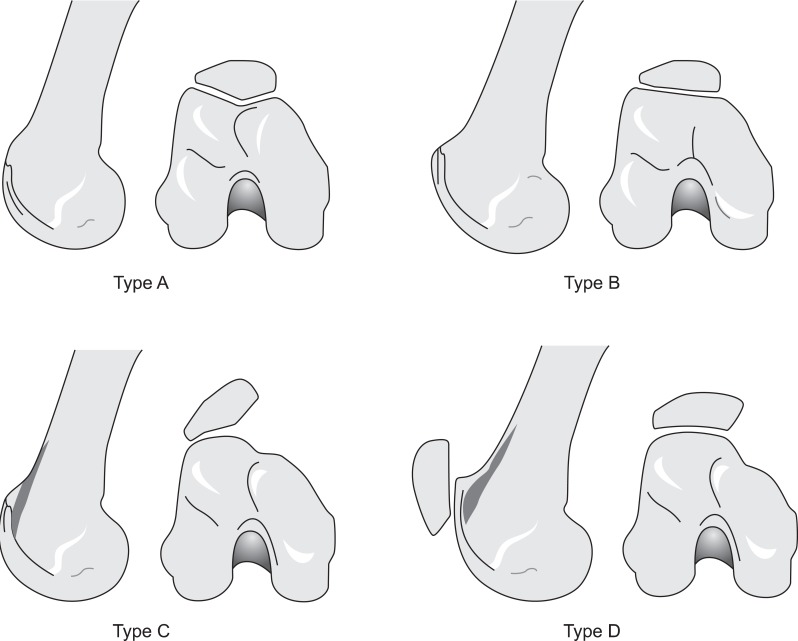
Other abnormal mechanisms related to patellofemoral joint pain include trochlear dysplasia which is observed in 78% of knees with isolated patellofemoral arthritis (Fig. 1)5,7,8). Degeneration of the patellofemoral joint can develop secondary to abnormal stress on the patella caused by patella alta, increased Q-angle combined with secondary soft tissue problems, a weakened or hypoplastic vastus medialis obliqus combined with contracture of the lateral retinaculum, or deficiency of the medial patellofemoral ligament. Articular fractures of the patella and trochlea caused by micro-trauma or macro-trauma is a risk factor for arthritis, which is indicated for isolated treatment of patellofemoral joint arthritis that progresses faster than other joint arthritides. Other causes include instability, osteoarthritis, inflammatory arthritis, obesity, and genetic quality of the cartilage9).
Fig. 1.
Dejour's classification of trochlear dysplasia. Type A: crossing sign (flat or convex trochlea), Type B: crossing sign and supratrochlear spur, Type C: crossing sign and double contour, Type D: crossing sign. Supratrochlear spur, double contour, and sharp step-off of the trochlea.
Clinical Manifestation
Patellofemoral arthritis has no characteristic symptoms although anterior knee pain is the most common complaint among patients. The pain is aggravated by stair ascending and descending, hill climbing, standing from a seated position, kneeling or squatting, which is related to friction or crackling crepitus. Some patients complain of stiffness of the knee or pseudolocking due to "kissing" lesions between the patella and the trochlea groove when friction occurs between the exposed bones.
Iwano et al.10) assessed the level of difficulty of 7 items of activities of daily living (ADL) in their patients. Each item was scored as 2 points if done without any problem, 1 point if done with some problem, and 0 point if done with great difficulty. The highest attainable score was 14 points. The ADL score of 4.1 was noted in the cases of patellofemoral osteoarthrosis combined with femorotibial osteoarthrosis whereas 9.4 noted in the cases of isolated patellofemoral osteoarthrosis. The score was 0 in the cases of isolated patellofemoral osteoarthrosis during squatting, running with short steps, or sitting with the knee in full flexion. None of the patients had difficulty in standing from a low seat. Patients had more difficulty in descending than ascending stairs. However, the ADL score was not correlated with the radiographic findings on the severity of the disorder. The ADL was defined as follows: 1) Pain on grinding the patella (the patella being moved both medio-laterally and infero-superiorly), 2) Crepitation on grinding the patella, 3) Crepitation during knee movement, 4) Peripatellar tenderness, 5) Pain on compression of the patella, 6) Limitation of patellar mobility, and 7) Clarke's test (positive when patients complained of pain during knee extension with patella compression).
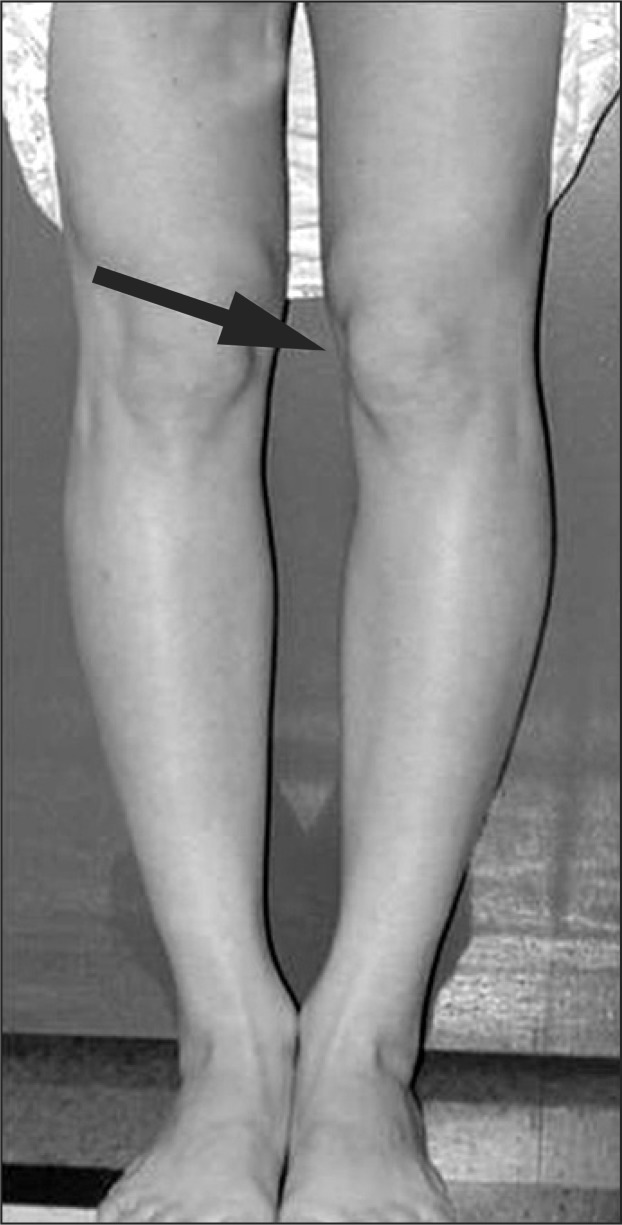
Physical examination is nonspecific but often reveals crepitus and effusion. Leslie and Bentley11) reported that quadriceps wasting over than 2 cm, effusion, and retropatellar crepitus are the most important clinical findings for the detection of chondromalacia patellae. Tenderness over the medial or lateral patellar facet is a major sign of patellofemoral arthritis12). The examiner places fingers under the lateral or medial border of the patella and applies pressure on the patellar facet to elicit clinically significant pain in the patellofemoral joint (the source of pain during this test has been controversial because 1) pain is felt in the early stage of the test when stress is placed on all soft tissues between the skin and the bone including the retinaculum and synovium, and 2) high flexion of the knee is required for the detection of proximal lesions). The site of articular lesion can be determined according to the degree of flexion where pain is most elicited when pressure is applied on the patellofemoral articular surface: the distal the lesion is located, the lower the degree of flexion where pain occurs. Furthermore, the patient's standing position and ambulation should be observed to identify the presence of squinting patella (Fig. 2) and pronated foot, positions that cause pain, and rotational alignment of the femur and tibia. Femoral abnormality should be examined with the patient sitting or lying since it can be the cause of anterior knee pain in some cases. A differential diagnosis should be made with L-34 lumbar disc herniation, neuroma, and tendinitis.
Fig. 2.
The points inward (arrow) are squinting patella. This finding is associated with femoral antevesion.
Radiographic Diagnosis
Patellofemoral arthritis can be assessed on the standing anteroposterior view, standing tunnel view at 45° (Rosenberg view), and lateral or skyline view (Merchant view). The Merchant view at 25°-30° allows the assessment of the proximal patellofemoral joint and the contact area between the patella and the trochlea.
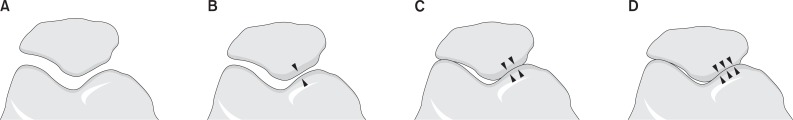
The severity of patellofemoral joint arthritis can be classified into 4 stages based on the 45° skyline view according to Merchant et al.13) (Fig. 3).
Fig. 3.
Merchant staged the severity of the disease based on the 45° skyline view. (A) Stage 1: mild with more than 3 mm of joint space. (B) Stage 2: moderate with less than 3 mm of joint space but no bony contact. (C) Stage 3: severe with bony surfaces in contact over less than one quarter of the joint surface. (D) Stage 4: very severe with bony contact throughout the entire joint surface.
The Rosenberg et al.14) view can be useful for evaluating arthritis that is localized to the medial or posterior femorotibial compartments because the space between the femur and tibia can be visualized without any superimposition.
Computed tomography (CT) is recommended when maltracking is suspected in the physical examination of patients with patellofemoral arthritis for identification of lateral patellar subluxation or femoral trochlear dysplasia. Magnetic resonance imaging (MRI) and diagnostic arthroscopy are useful for the diagnosis or identification of arthritis in other compartments. Patellofemoral arthritis can be a symptom of other inflammatory arthritides and thus serological tests for rheumatoid arthritis or Lyme disease should be performed.
Treatment
1. Conservative Treatment
Isolated patellofemoral arthritis is mostly asymptomatic. Conservative treatment is the preferred primary treatment option and surgical intervention is considered as a last resort in a small number of patients. Symptoms can be alleviated with quadriceps femoris strengthening exercises, stretching of the lateral patellar retinaculum, and range of motion (ROM) restriction. Weight loss can also be helpful in reducing the load on the anterior knee. Pain reduction can be expected by avoiding stair climbing, squatting, and jumping or by injection of nonsteroidal anti-inflammatory drugs (NSAIDS) or intra-articular injection of steroids or hyaluronic acid.
Nutrition therapy has not been recommended for osteoarthritis except for glucosamine which has been considered safe to use15). Some pilot studies have shown that viscosupplementation can potentially relieve arthritis16). Albeit not established, patella unload sleeves, braces, and taping can be useful for pain relief17). Surgical treatment should be considered as an option if 3 to 6 months of conservative treatment is not effective.
2. Operative Treatment
1) Soft-tissue realignment of the extensor mechanism
Soft-tissue realignment procedures for patellofemoral osteoarthritis include release of the lateral patellar retinaculum, reattachment or reconstruction of the medial patellofemoral ligament, and advancement of the vastus medialis obliqus. The results of soft-tissue realignment procedures for patellofemoral osteoarthritis in the absence of patellar instability have not yet been sufficiently investigated. The medial patellofemoral ligament has been known to be a crucial component in patellofemoral joint stability for the prevention of lateral patellofemoral dislocation3).
Release of the lateral patellar retinaculum, which has been widely performed for anterior knee pain, involves medial transfer of the patellofemoral contact surface. This procedure can be effective if patellar instability is not present, pathologic lateral tilt is the major lesion in radiography, and the medial articular cartilage is intact. However, the vector direction of the lateral patellar retinaculum is posterolateral, and Desio et al.18) reported that the lateral restraining force was reduced by only 10% after cutting of the lateral patellar retinaculum. Procedures using this technique can be performed when patellofemoral joint pain is present, the lateral retinaculum is the source of force causing malalignment, and contracture or tightness is present in the posterolateral aspect of the lateral patellar retinaculum.
Release of the lateral patellar retinaculum can be either open or arthroscopic. It should be performed for mild patellofemoral osteoarthritis with insignificant level of patellar tilt or subluxation. However, the procedure generally precedes a more complete treatment and its pain relieving effect is difficult to predict.
The procedure can be performed in combination with partial lateral facetectomy in the following conditions: 1) lateral patellofemoral arthritis is present on one or both sides of the joint, 2) radiographic evidence of tilt exists without subluxation, and 3) there is no clinical evidence of instability. When there is a large osteophyte, the combined procedure may contribute to clinical improvement.
2) Osteotomies of the tibial tubercle
Osteotomies of the tibial tubercle were designed to alleviate pressure in the arthritic portion of the patellofemoral joint to improve symptoms. Huberti and Hayes19) first introduced a procedure that transfers the tibial tuberosity anteriorly to reduce the load on the defective articular cartilage. Unfortunately, the procedure often resulted in an increased load on the medial joint of the knee due to excessive medialization, which eventually resulted in severe osteoarthritis19,20).
However, anterior transfer of the tibial tubercle is advantageous for the treatment of articular cartilage lesions in the distal portion of the patella. Tibial tubercle anteriorization has been considered remarkably effective for patellofemoral osteoarthritis in young patients and can be a permanent solution for arthritic pain and dysfunction related to malalignment, when properly indicated.
The following are the main principles of successful tibial tubercle transfer for the treatment of patellofemoral arthritis proposed by Saleh et al.4) in 2005.
Restoration or maintenance of the proper balance of the extensor mechanism.
Transfer of a painful and degenerated area to a less loaded articular surface and reduction of the load on the lateral aspect of the patella through medial transfer of the tibial tuberosity.
Relief of pain caused by the patellar retinaculum.
Tibial tubercle osteotomy for early joint motion and prompt healing.
In order to apply these principles, the surgeon should identify the area of pain in the patellofemoral joint based on the findings in the patient's medical history and physical, radiographic, and arthroscopic examinations and determine the direction of osteotomy in the tibial tubercle.
3) Autologous chondrocyte implantation
The etiology and cause of arthritis should be precisely analyzed prior to autologous chondrocyte implantation for cartilage defects. The diagnosis and correction of the underlying abnormalities are crucial to the success of the procedure. In 1994, Brittberg et al.21) reported that autologous chondrocyte implantation was successful only in 2 out of 7 cases. Thereafter, restoration of adequate patellar tracking through realignment of the extensor mechanism has been considered necessary. Peterson et al.22) obtained excellent results in 11 out of 17 patients after autologous chondrocyte implantation with patellar realignment. Thus, it is of utmost importance to address the fundamental cause before beginning treatment of cartilage defects.
As mentioned above, the site of patellar cartilage lesion is important for the success of tibial tubercle osteotomy. Patients with a lesion in the inferior pole or the lateral facet of the patella can obtain more satisfying results than those with a lesion in the proximal pole, medial facet or diffuse of the patella. A lesion at the center of the trochlea is related to an articular lesion in the medial aspect of the patella, which has been associated with poor outcomes.
The success of autologous chondrocyte implantation depends on the support, follow-up, joint stability, cartilage defect size, severity of cartilage defect, and concomitant arthritis. In patients with mechanical axis deviation over than 2° or a large cartilage defect, valgus or varus osteotomy should be performed prior to restoration of the cartilage of the weight-bearing area.
In a prospective cohort study by Minas and Bryant9), 45 patients were followed up for 7 years after autologous chondrocyte implantation for the treatment of isolated patellar cartilage defect, isolated trochlear cartilage defect, or both defects. The mean age of the patients at the time of surgery was 36.9 years (range, 15 to 54 years). The mean follow-up period was 47.5 months (range, 24 to 86 months). The patient survey showed that 71% of the patients were satisfied with the results, 16% had no complaints, and 13% were unsatisfied. Overall, the results were rated as good or excellent in 71% of the patients, fair in 22%, and poor in 7%. The most significant improvement in motor function was observed in patients with severe knee defects. The cost effectiveness of the procedure, long-term follow-up results, and comparison with other treatment methods should be addressed in future studies.
4) Patellectomy
The theoretical basis of patellectomy is that chronic pain related to severe defects of the patella and the cartilage can be resolved through removal of the patella, the source of the pain. Weaver et al.23) reported that 87% of the cases showed good results during the 3 to 12 years of follow-up period after longitudinal semipatellectomy, total patellectomy, and the modified Trillat procedure for the treatment of patellofemoral arthritis secondary to malalignment. On the other hand, side effects of the procedure have also been reported in a variety of studies. Lennox et al.24) reported that 54% of 83 cases with patellar arthritis including patellofemoral arthritis (25 cases) achieved pain relief following patellectomy and the muscle strength of the quadriceps femoris was 60% of the normal value. Furthermore, the procedure can result in chronic weakness in extension, extension lag, or trochlear wear due to the contact with a tendon over time.
In general, patellectomy can be considered as an option when 1) the alignment of the extensor mechanism is normal and the femoral trochlea is intact in spite of severe patellar arthritis, 2) anatomical reduction is impossible due to severe comminuted fracture of the patella, 3) patellar tracking is normal in the presence of severe chondromalacia patella, or 4) realignment procedure resulted in poor outcome (Fig. 4). However, patellectomy should be regarded as a salvage procedure.
Fig. 4.
(A) Simple radiographs of a patient diagnosed with patellofemoral arthritis after patellar fracture. (B) Intraoperative gross photos and postoperative radiographs after patellectomy.
5) Patellofemoral replacement
The first patellofemoral replacement procedure was performed using a screw-on Vitallium patellar shell by McKeever25) in 1955. This procedure was further developed later and Lubinus26) introduced a patellofemoral replacement prosthesis in 1979. In the early days of patellofemoral replacement, the results were unsatisfactory due to the problems related to patient selection, surgical technique, lack of understanding of the extensor mechanism, and durability. Tauro et al.27) reported a 50% failure rate at 8 years after patellofemoral replacement, which was attributed to prolonged malalignment, polyethylene wear, impingement, and progression of arthritis in the other initially unaffected compartments.
However, prosthesis design has evolved to produce improved outcomes thereafter28,29). The femoral flange is shallow and broad to promote stable fixation of the patella to the femoral trochlea. The medial side of the patellar component is uniquely concave to avoid impingement on the femoral component in flexion. This design improvement has contributed to the ruling out of the potential risk of early polyethylene wear and malalignment, which in turn caused a low complication rate and improved ROM (Fig. 5). Patellofemoral replacement is primarily indicated in patients who are young for total knee arthroplasty or have isolated patellofemoral arthritis. In general, patellectomy produces unsatisfactory results in these patients or poor results in 47% of patients. In addition, patellofemoral replacement is advantageous for maintaining the biomechanics of the knee joint while preserving the menisci and cruciate ligaments compared to total knee arthroplasty.
Fig. 5.
Postoperative simple radiographs after patellofemoral replacement in a patient diagnosed with patellar malunion.
6) Total knee arthroplasty
Total knee arthroplasty has been established as an effective treatment for isolated patellofemoral arthritis in elderly patients30,31). Laskin and van Steijn30) compared the results of total knee arthroplasty between 53 patients with isolated patellofemoral arthritis and those with tricompartment arthritis. At a mean of 7.4 years after surgery, 53 patients obtained significant improvement in symptoms although anterior knee pain remained in 7%. In addition, total knee arthroplasty resulted in better outcomes than patellectomy. Thus, total knee arthroplasty appears to be the most proven and predictable procedure for the treatment of patellofemoral arthritis in older patients. However, the disadvantages of the procedure should be taken into account including larger surgical area compared to the lesion size and extensive tissue loss.
Conclusions
A broad range of management options is available for patellofemoral arthritis depending on the patient's symptoms and conditions. In patients with anterior knee pain, determination of the cause of the disorder is essential. Whether the pain is primary or secondary and whether the arthritis is isolated or combined should be identified prior to treatment planning.
Ongoing improvement has been reported regarding patellofemoral arthritis treatment. However, sufficient treatment results have not been reported for comparison studies and there is no consensus among the authors of different studies. An agreement on the ultimate treatment method will require more quality clinical studies on the cause of patellofemoral arthritis and long-term treatment results. The controversy over the treatment methods for patellofemoral arthritis is not fully resolved and there are many exciting areas of progress.
Isolated patellofemoral arthritis is asymptomatic and does not require treatment in most cases. Sufficient strength of the quadriceps femoris appears crucial for achieving good treatment results. The incidence of total knee arthroplasty would gradually decrease with the improvement of patellofemoral replacement techniques. Finally, it should be noted that patellofemoral replacement is a viable treatment option for elderly patients.
References
- 1.Davies AP, Vince AS, Shepstone L, Donell ST, Glasgow MM. The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res. 2002;(402):206–212. doi: 10.1097/00003086-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Noble J, Hamblen DL. The pathology of the degenerate meniscus lesion. J Bone Joint Surg Br. 1975;57:180–186. [PubMed] [Google Scholar]
- 3.Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499–519. doi: 10.1016/s0278-5919(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 4.Saleh KJ, Arendt EA, Eldridge J, Fulkerson JP, Minas T, Mulhall KJ. Symposium Operative treatment of patellofemoral arthritis. J Bone Joint Surg Am. 2005;87:659–671. doi: 10.2106/JBJS.D.03035. [DOI] [PubMed] [Google Scholar]
- 5.Mow VC, Kuei SC, Lai WM, Armstrong CG. Biphasic creep and stress relaxation of articular cartilage in compression? Theory and experiments. J Biomech Eng. 1980;102:73–84. doi: 10.1115/1.3138202. [DOI] [PubMed] [Google Scholar]
- 6.Ateshian GA, Hung CT. Patellofemoral joint biomechanics and tissue engineering. Clin Orthop Relat Res. 2005;(436):81–90. doi: 10.1097/01.blo.0000171542.53342.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 8.Tecklenburg K, Dejour D, Hoser C, Fink C. Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:235–240. doi: 10.1007/s00167-005-0683-0. [DOI] [PubMed] [Google Scholar]
- 9.Minas T, Bryant T. The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res. 2005;(436):30–39. doi: 10.1097/01.blo.0000171916.40245.5d. [DOI] [PubMed] [Google Scholar]
- 10.Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990;(252):190–197. [PubMed] [Google Scholar]
- 11.Leslie IJ, Bentley G. Arthroscopy in the diagnosis of chondromalacia patellae. Ann Rheum Dis. 1978;37:540–547. doi: 10.1136/ard.37.6.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grelsamer RP. Patellar malalignment. J Bone Joint Surg Am. 2000;82:1639–1650. [PubMed] [Google Scholar]
- 13.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 14.Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479–1483. [PubMed] [Google Scholar]
- 15.Anderson JW, Nicolosi RJ, Borzelleca JF. Glucosamine effects in humans: a review of effects on glucose metabolism, side effects, safety considerations and efficacy. Food Chem Toxicol. 2005;43:187–201. doi: 10.1016/j.fct.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Clarke S, Lock V, Duddy J, Sharif M, Newman JH, Kirwan JR. Intra-articular hylan G-F 20 (Synvisc) in the management of patellofemoral osteoarthritis of the knee (POAK) Knee. 2005;12:57–62. doi: 10.1016/j.knee.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Fulkerson JP. Alternatives to patellofemoral arthroplasty. Clin Orthop Relat Res. 2005;(436):76–80. doi: 10.1097/01.blo.0000172305.20156.ba. [DOI] [PubMed] [Google Scholar]
- 18.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 19.Huberti HH, Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715–724. [PubMed] [Google Scholar]
- 20.Kuroda R, Kambic H, Valdevit A, Andrish JT. Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med. 2001;29:403–409. doi: 10.1177/03635465010290040301. [DOI] [PubMed] [Google Scholar]
- 21.Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331:889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 22.Peterson L, Minas T, Brittberg M, Nilsson A, Sjogren-Jansson E, Lindahl A. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res. 2000;(374):212–234. doi: 10.1097/00003086-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Weaver JK, Wieder D, Derkash RS. Patellofemoral arthritis resulting from malalignment. A long-term evaluation of treatment options. Orthop Rev. 1991;20:1075–1081. [PubMed] [Google Scholar]
- 24.Lennox IA, Cobb AG, Knowles J, Bentley G. Knee function after patellectomy A 12- to 48-year follow-up. J Bone Joint Surg Br. 1994;76:485–487. [PubMed] [Google Scholar]
- 25.McKeever DC. Patellar prosthesis. J Bone Joint Surg Am. 1955;37:1074–1084. [PubMed] [Google Scholar]
- 26.Lubinus HH. Patella glide bearing total replacement. Orthopedics. 1979;2:119–127. doi: 10.3928/0147-7447-19790301-03. [DOI] [PubMed] [Google Scholar]
- 27.Tauro B, Ackroyd CE, Newman JH, Shah NA. The Lubinus patellofemoral arthroplasty. A five- to ten-year prospective study. J Bone Joint Surg Br. 2001;83:696–701. doi: 10.1302/0301-620x.83b5.11577. [DOI] [PubMed] [Google Scholar]
- 28.Kooijman HJ, Driessen AP, van Horn JR. Long-term results of patellofemoral arthroplasty. A report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg Br. 2003;85:836–840. [PubMed] [Google Scholar]
- 29.Krajca-Radcliffe JB, Coker TP. Patellofemoral arthroplasty. A 2- to 18-year followup study. Clin Orthop Relat Res. 1996;(330):143–151. [PubMed] [Google Scholar]
- 30.Laskin RS, van Steijn M. Total knee replacement for patients with patellofemoral arthritis. Clin Orthop Relat Res. 1999;(367):89–95. [PubMed] [Google Scholar]
- 31.Mont MA, Haas S, Mullick T, Hungerford DS. Total knee arthroplasty for patellofemoral arthritis. J Bone Joint Surg Am. 2002;84:1977–1981. doi: 10.2106/00004623-200211000-00011. [DOI] [PubMed] [Google Scholar]