Summary
Objectives
The Intermittent and Constant Osteoarthritis Pain (ICOAP) questionnaire was developed to assess two forms of pain reported by people with osteoarthritis: intermittent and constant pain. Studies examining its measurement qualities have provided some support for its use as separate and total scales. However, it has not been previously evaluated using Rasch analysis. The current study examined the fit between data obtained from the ICOAP questionnaire and the Rasch model to determine whether it meets the requirements of interval-level measurement.
Design
ICOAP responses from 175 participants with knee osteoarthritis were collected in a cross-sectional questionnaire study. Participants were recruited from hospital clinics and a group who had taken part in previous research. The questionnaires were completed at home and returned by pre-paid envelope and the data were analysed using RUMM2020.
Results
Fit to the Rasch model was achieved for both the Constant and Intermittent subscales following removal of a small number of items. The Total scale initially resulted in substantial misfit to the model, but fit was improved by removing four items that misfit the model. However, several participants presented with high fit residuals, which is consistent with misfit.
Conclusions
The results support the use of Constant and Intermittent subscales as unidimensional measures of pain. The Total scale can be adapted to improve fit to the Rasch model, but there are concerns over participant misfit.
Keywords: Rasch analysis, Osteoarthritis, Pain, Outcome assessment
Introduction
The most important reported symptom of osteoarthritis (OA) is pain1,2. Pain is often treated as a single outcome in clinical trials, but the experience of pain in OA is complex and diverse3. Pain may vary according to its localisation, periodicity and descriptive quality, reflecting diverse pathophysiological mechanisms4. Pain questionnaires used in OA research aim to measure the overall severity of pain and/or the severity or nature of specific dimensions of pain. In general, clinical trials seek to evaluate overall pain experience, whereas mechanistic studies require a more detailed understanding of phenotype. Estimates of overall pain severity may be sought by combining responses to questionnaires that target specific pain dimensions. However, measurement scales should ideally demonstrate unidimensionality, and combining distinct dimensions into a single scale can sometimes threaten validity5.
The Intermittent and Constant Osteoarthritis Pain (ICOAP) questionnaire was developed to assess two kinds of OA pain6 on the basis of aspects of pain that were identified as distinct and important by focus groups of people with OA7. Constant pain was characterised as a continuous aching sensation, and intermittent pain, was described as being severe but transient. This questionnaire was the first to assess these different types of OA pain, and it has been proposed that a total score may be a useful measure of overall pain severity in OA6.
There are eleven items on the ICOAP forming two subscales considering both pain intensity and the effect of pain on quality of life6. Five items address constant pain and the remaining six items deal with intermittent pain. Items are responded to using a five-point scale. Ten items are phrased to assess the intensity of pain (e.g., How intense has your constant knee pain been?). The response options for these items are 0 (Not at all), 1 (Mildly), 2 (Moderately), 3 (Severely) or 4 (Extremely). In contrast, item 7 asks patients about the frequency of their pain (How frequently has this knee pain that comes and goes occurred?). The response options for this item are 0 (Never), 1 (Rarely), 2 (Sometimes), 3 (Often) or 4 (Very often). The questionnaire can be administered by interview or self-completed8.
The ICOAP questionnaire has shown good internal consistency, test–retest reliability and construct validity6 when compared to scores on other questionnaires such as the Western Ontario and McMasters Universities Osteoarthritis (WOMAC) Index pain subscale9. It has also been successfully applied with other cultures10–12 and is starting to be used as a measure of outcome in medical intervention studies11,13,14. The ICOAP is considered an important pain indexes by Osteoarthritis Research Society International (OARSI)15, has been recommended by OA experts16, and is included in several protocols for future trials17,18. However, there have been concerns raised over the dimensional structure of the questionnaire. Hawker et al.6 conducted a principal components analysis of the ICOAP using a varimax rotation and found factorial complexity. Three components were extracted that accounted for 81.7% of the variance, but several items loaded onto more than one factor. These findings were supported in a secondary analysis using a promax rotation. The authors of the questionnaire therefore suggested using the total score rather than the subscales, but further testing was recommended6.
The ICOAP hasn't been evaluated using Rasch analysis19. Rasch is a modern psychometric technique, appropriate for newly developed and existing questionnaires5,20, which allows an examination of many critical measurement issues. It is important to allow researchers to ensure that different subgroups of participants (e.g., males and females) respond in similar ways given equivalent levels of pain5 and to address concerns6 about whether the ICOAP questionnaire displays unidimensionality21. Given fit to the model, it permits a transformation of ordinal data to interval-level measurement assisting with the calculation of mathematic operations such as change scores22. The purpose of the current study was therefore to examine fit between data obtained from the ICOAP and the Rasch model.
Methods
Participants and setting
Participants were recruited who had OA of the knee, defined and scored radiographically using Kellgren–Lawrence criteria23, and reported accompanying pain on most days for at least the past month. Exclusion criteria were another rheumatic disease (e.g., Rheumatoid Arthritis, Gout and Psoriatic Arthritis), joint surgery within the 3 months prior to participation and an inability to speak or understand English.
Participants were identified from three sources: (1) a group that had taken part in a previous community-based study of knee OA24, (2) Rheumatology and Orthopaedic clinics from Nottingham University Hospitals NHS Trust and (3) pre-operative assessment clinics from Sherwood Forest Hospitals NHS Trust. Potential participants were sent an invitation to the study, which was signed by a healthcare professional responsible for their care (e.g., surgeon). Those who agreed to participate were asked to complete a questionnaire set including measures of pain, anxiety, depression, fatigue, self-efficacy, acceptance, coping, beliefs, helplessness and quality of life. Only data from the ICOAP questionnaire and the Bodily Pain subscale of the RAND SF-3625 are reported in the current article. The Bodily Pain subscale is composed of two items assessing pain over the past 4 weeks and the effect it has had on participants' ability to work. The items have a five and six point response format, respectively, and a total score is calculated from selected options whereby higher values indicate less pain. Rasch-transformed scores from the questionnaires were correlated using Pearson's coefficient to provide an indication of external construct validity of the ICOAP. As participants were provided with a lengthy set of questionnaires they were advised to complete as many as they felt able to and the order of presentation was randomised into four sequences to minimise order effects. The questionnaires were completed at home and returned to the researchers by pre-paid envelope. Non-respondents were sent one reminder letter after 3 weeks as long as they were still able to participate.
Informed consent was obtained from all participants and the research was approved by Nottingham Research Ethics Committee one.
Rasch analysis
Three separate analyses were carried out on the Constant subscale, Intermittent subscale, and the Total scale. RUMM202026 was used to conduct the analyses.
Rasch analysis assesses fit between data obtained on a scale and the predictions of the Rasch model22. This is undertaken because the model shows us what to expect if a scale meets the axioms underlying additive conjoint measurement5.
To help decide whether the rating scale27 or the partial credit formulation28 of the Rasch model was most appropriate, a likelihood ratio test was performed for each analysis. If the test was not significant (i.e., P > 0.05), then the rating scale version can be adopted; otherwise the partial credit version should be used. The tests were significant for all but the Intermittent subscale and so the partial credit formulation was used for consistency. However, both versions of the model resulted in similar conclusions. Individual items were inspected to see whether there was evidence of disordered response thresholds5,22,29. When this was observed, the item was rescored (i.e., collapsing appropriate adjacent response options).
Mean and standard deviation fit residuals were calculated for the items and the persons. These values were transformed to estimate a z-score representing standardised normal distribution and so, given good fit, the means should be close to 0 and the standard deviations about 122,29,30. RUMM2020 creates groups, called class intervals, on the basis of the level of examined trait. An item-trait interaction chi-squared was used to test whether the hierarchical arrangement of the items was invariant across the class intervals. A significant P-value at the 0.05 level, with a Bonferroni adjustment for the number of items, signified that the item orderings differed across trait22,30. The Person Separation Index (PSI) was examined for each analysis to provide an indication of internal consistency. A value of 0.7 and above indicated acceptable internal consistency29.
Each individual item and person was examined for misfit. For items, chi-squared and Analysis of Variance (ANOVA) fit statistics were calculated with a Bonferroni correction. Fit residuals were also examined for items and persons. Values above +2.5 or below −2.5 were considered to be misfitting the model22.
Differential Item Functioning (DIF) was explored for gender (males and females) and age (<64 years, 64–71 years and >71 years). When an item displays DIF it means that different subgroups produced significantly different responses despite having equivalent levels of trait5,22. ANOVA with a Bonferroni Correction was applied to explore DIF. Local independence of the items was examined in two ways. First, response dependencies between items were identified from the residual correlation matrix. A positive correlation of 0.3 or more was considered to be indicative of response dependency31. Second, each scale was tested for a breach of unidimensionality5,21,32. Principal components analysis was performed on the residuals and used to identify two subsets of items; those loading positively and negatively on the first component. Person estimates were then calculated for each subset and then a series of independent t-tests were carried out to see whether the subsets produced significantly different estimates. Assuming that both subsets were measuring the same unidimensional construct no more than 5% of these t-tests should be significant at a 0.05 level. A binomial confidence interval (CI) was applied for cases that were more than 5%29.
Results
Of the 474 people invited to take part, 175 provided data for analysis (37% response rate). Responses with three or more missing items were not included as recommended by the ICOAP user guide. The study sample had approximately 50% females and 50% males with a median age of 66 years (see Table I). About half of the participants came from the community group and half from hospital clinics. Gender and age information was available from 174 and 283, respectively, of the 299 people that were invited to take part but not included in the analysis. There were 89 females (51%) and the median age was 69 (inter-quartile range = 61–76). This suggests that the study sample was representative of the total group.
Table I.
Participant characteristics
| n | % | |
|---|---|---|
| Gender | ||
| Females | 91 | 52 |
| Duration of OA∗ | ||
| 0–5 years | 55 | 40 |
| 6–10 years | 43 | 31 |
| More than 10 years | 39 | 28 |
| Community group | 99 | 57 |
| Nottingham University Hospitals NHS Trust clinics | 58 | 33 |
| Sherwood Forest Hospitals NHS Foundation Trust clinics | 18 | 10 |
| Median | IQR† | |
| Age | 66 | 60–73 |
| Kellgren–Lawrence (tibiofemoral) | 3 | 2–3 |
| Kellgren–Lawrence (patellofemoral) | 2 | 2–3 |
| ICOAP constant | 45 | 30–65 |
| ICOAP intermittent | 50 | 38–67 |
| ICOAP total | 48 | 34–65 |
| RAND SF-36 Bodily Pain | 45 | 23–58 |
Length of OA was based on participant estimation. Some estimates were reported as uncertain and some participants did not provide a response. Percentages are based on the total responses available.
IQR = inter-quartile range, 25th and 75th percentiles provided.
Constant subscale
All items exhibited ordered response thresholds. The summary item–person interaction statistics suggested misfit between data and the model (see Table II). The standard deviation item fit residual (1.97) was high indicating that there was likely some misfit at an individual item level. Items 2 (How much has your constant knee pain affected your sleep? Fit Residual = 3.49; χ2 = 8.49, df = 2, P = 0.01; F = 3.85, df = 2, P = 0.02) and 3 (How much has your constant knee pain affected your overall quality of life? Fit Residual = −1.26; χ2 = 10.12, df = 2, P = 0.006; F = 8.37, df = 2, P = 0.0003) exhibited misfit; item 2 had a high positive fit residual indicating under discrimination. There was no evidence of DIF or response dependency. Principal components analysis of the residuals identified items that positively (items 1 and 2) and negatively (items 3, 4 and 5) loaded on the first component. Twenty-two out of 167 t-tests were significant, which represented 13.17% (Binomial CI: 9.90–16.50%) of the total tests.
Table II.
Summary fit statistics for the Constant subscale, Intermittent subscale and Total scale
| Rasch Analysis | Number of items | Item fit residual (Mean) | Item fit residual (SD) | Person fit residual (Mean) | Person fit residual (SD) | χ2 (df) | P-value | PSI | Percentage of significant t-tests (CI) |
|---|---|---|---|---|---|---|---|---|---|
| Constant (initial) | 5 | 0.03 | 1.97 | −0.44 | 1.13 | 20.82 (10) | P = 0.02 | 0.92 | 13.17% (9.90–16.50%) |
| Constant (remove 2) | 4 | −0.08 | 1.23 | −0.43 | 0.89 | 7.44 (8) | P = 0.49 | 0.92 | 5.42% (2.10–8.70%) |
| Intermittent (initial) | 6 | 0.06 | 2.13 | −0.47 | 1.26 | 22.25 (12) | P = 0.03 | 0.90 | 8.82% (5.50–12.10%) |
| Intermittent (remove 9) | 5 | 0.23 | 1.47 | −0.42 | 1.13 | 11.88 (10) | P = 0.29 | 0.87 | 7.06% (3.80–10.30%) |
| Intermittent (remove 8) | 4 | 0.17 | 1.59 | −0.47 | 1.01 | 5.64 (8) | P = 0.69 | 0.85 | 7.14% (3.80–10.40%) |
| Total scale (initial) | 11 | 0.08 | 1.89 | −0.72 | 1.84 | 37.47 (22) | P = 0.02 | 0.94 | 9.25% (6.00–12.50%) |
| Total scale (rescore 7) | 11 | 0.09 | 1.88 | −0.71 | 1.84 | 35.05 (22) | P = 0.04 | 0.94 | 9.25% (6.00–12.50%) |
| Total scale (remove 7 & 6) | 9 | −0.01 | 1.51 | −0.79 | 1.78 | 27.72 (18) | P = 0.07 | 0.93 | 15.61% (12.40–18.90%) |
| Total scale (remove 8 & 2) | 7 | −0.18 | 1.26 | −0.83 | 1.51 | 21.42 (14) | P = 0.09 | 0.93 | 6.36% (3.10–9.60%) |
| Ideal value | 0.00 | 1.00 | 0.00 | 1.00 | >0.05 | >0.70 | <5% |
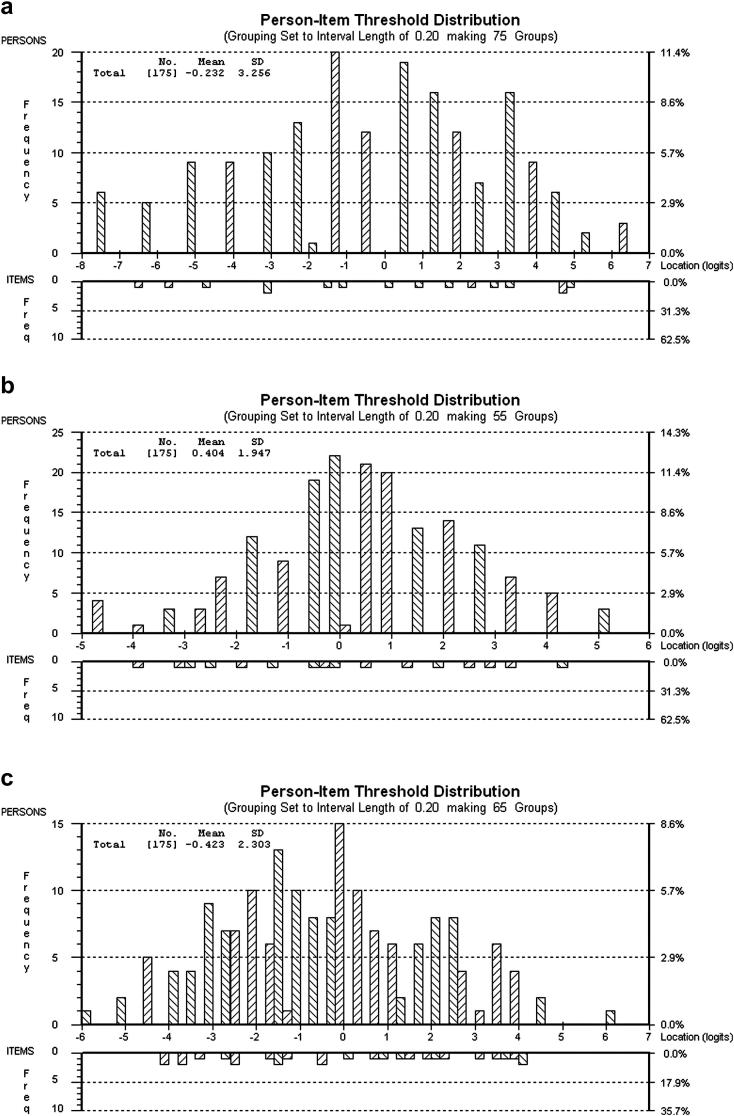
To improve fit to the model item 2 was removed. This item was chosen for two reasons. First, like item 3, it exhibited misfit to the model. Second, Hawker et al.6 found that item 2 (and item 8 – the Intermittent equivalent) loaded onto a separate factor indicating that it might be measuring sleep disorders in general as well as the effect of pain on sleep. Following removal of item 2 satisfactory fit to the model was achieved (see Table II). There were no misfitting items or persons, no evidence of response dependency or DIF, and the subscale passed the test of unidimensionality (5.42%; Binomial CI: 2.10–8.70%). Figure 1(a) shows the person–item threshold distribution and confirms that the subscale was well targeted. Only 5% of participants produced floor or ceiling effects.
Fig. 1.
Person–item threshold distributions for the Constant subscale (a), Intermittent subscale (b) and Total scale (c). The top part of the graphs show the distribution of persons along the Rasch-transformed scale of constant, intermittent and total pain, respectively. The bottom part shows the distribution of items. Ideally, given good targeting, the two distributions should mirror one another such that the full range of trait expressed by participants is captured by the items on a scale.
Intermittent subscale
All item thresholds were ordered, but the summary fit statistics indicated some misfit between data and the model (see Table II). Item 9 (How much has your knee pain that comes and goes affected your overall quality of life?) had a significant F-statistic (Fit Residual = −2.20; χ2 = 5.81, df = 2, P = 0.05; F = 5.19, df = 2, P = 0.007). Several participants also presented with high fit residuals. There was no evidence of response dependency, but item 8 (How much has your knee pain that comes and goes affected your sleep?) had uniform DIF for age. Specifically, participants aged 72 years and above produced lower expected values than the remaining participants across all three class intervals. Principal components analysis of the residuals identified items that loaded positively (items 9, 10 and 11) and negatively (items 6, 7 and 8) onto the first component. The Intermittent subscale marginally failed the test of unidimensionality (8.82%; Binomial CI: 5.50–12.10%).
The fit statistics may have been adversely affected by a small group of participants who responded in an unexpected way22. In total, 7% of participants produced fit residuals outside of the acceptable range. There was no obvious bias in this group towards sex (54% female), nor towards a particular age group (<64 years = 31%; 64–71 years = 38%; >71 years = 31%). The majority of participants had high negative fit residuals (85%), which indicates that their responses were too deterministic (i.e., too similar to a Guttman pattern) for the Rasch model. However, the summary fit statistics displayed in Table II suggest that the overall fit for persons was relatively good (e.g., SD < 1.4). It is possible that floor or ceiling effects increased the chance of obtaining a negative fit residual, but only 3% of participants produced them. Therefore, a technique proposed by Linacre33 was used to examine whether it was necessary to remove the misfitting participants. Persons estimates before and after removal of the misfitting participants were plotted against each other. Inspection of the plot confirmed that the effect of removing the participants was minimal and so they were retained.
Item 9 had a significant ANOVA test and so was considered for deletion. Removal of this item resulted in improved fit as shown in Table II. Item 8 continued to exhibit DIF for age. As the DIF was uniform, an attempt was made to ‘split the DIF’. This is where the item is split according to the subgroups that produced different scores – in this case 71 years and below and 72 years and above. However, this resulted in an increase in the item–trait interaction χ2 (11.88–18.83), which suggests reduced fit. To examine whether this item was having a negative effect on the fit statistics it was removed, which improved the overall fit (see Table II). The revised 4-item Intermittent subscale had no misfitting items or persons, no response dependency or DIF and was unidimensional (7.14%; Binomial CI: 3.80–10.40%). Following these changes item 7 exhibited marginally disordered thresholds but rescoring didn't improve the fit statistics and so the original scoring was retained. The person–item threshold distribution showed reasonable targeting [see Fig. 1(b)]. Four percent of participants were at floor or ceiling levels.
Total scale
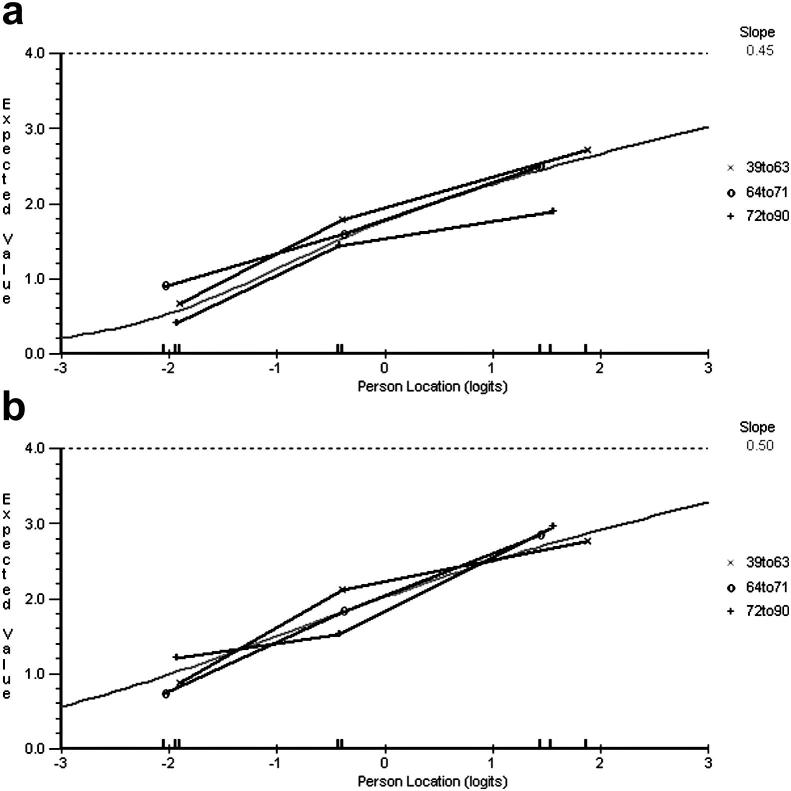
Item 7 (How frequently has this knee pain that comes and goes occurred?) had disordered thresholds and so was rescored by collapsing response options 0 and 1. The summary fit statistics suggested significant misfit for both items and persons (see Table II). Item 7 misfits the model (Fit Residual = 3.67; χ2 = 8.63, df = 2, P = 0.01; F = 3.85, df = 2, P = 0.02) and 18% of participants presented with high fit residuals. There was evidence of response dependency: items 2 and 8 (0.62), items 4 and 5 (0.40), items 9 and 10 (0.33) and items 10 and 11 (0.34). Notice that with the exception of items 2 and 8 the response dependency was limited to items within the same subscales. Items 8 [see Fig. 2(a)] and 9 [see Fig. 2(b)] exhibited uniform and non-uniform DIF for age, respectively. The Total scale failed the test of unidimensionality with 16 out of 173 t-tests significant (9.25%; Binomial CI: 6.60–12.50%). The subsets of items formed from the principal components analysis of the residuals were potentially revealing of the underlying cause of the multidimensionality. Specifically, items 1, 2, 3, 4, 5 and 8 (with the exception of 8, all Constant items) positively loaded onto the first component and items 6, 7, 9, 10 and 11 (all Intermittent items) negatively loaded.
Fig. 2.
DIF across age groups for items 8 (a) and 9 (b) of the Total scale.
To improve fit to the model, items 7, 6 (How intense has your most severe knee pain that comes and goes been? Fit Residual = 2.96; χ2 = 11.78, df = 2, P = 0.003; F = 4.60, df = 2, P = 0.01), 8 (Fit Residual = 2.65; χ2 = 5.79, df = 2, P = 0.06; F = 2.45, df = 2, P = 0.09) and 2 (Fit Residual = 3.93; χ2 = 7.68, df = 2, P = 0.02; F = 3.21, df = 2, P = 0.04) were removed one-by-one due to misfit (misfit for items 6, 8 and 2 became apparent after removing the preceding item). As Table II shows, this improved the fit statistics. There were no more misfitting items, no response dependency or DIF and the scale was unidimensional (6.36%; Binomial CI: 3.10–9.60%). The remaining Constant (1, 3, 4 and 5) and Intermittent (9, 10 and 11) items continued to load in opposite directions on the first component. The revised 7-item Total scale was relatively well targeted [see Fig. 1(c)], but unlike the analysis of the Intermittent subscale, the number of participants misfitting the model was still high (11%) following the changes. This was particularly reflected in the mean person fit residual (see Table II). This wasn't attributable to floor or ceiling effects, which were low (1%). Alternative analysis plans were carried out (i.e., removing misfitting persons before altering the scale, subtesting for response dependency and removing items 2 and 8 first), but they resulted in similar conclusions.
Correlation analysis
Data from the Bodily Pain subscale of the RAND SF-36 were Rasch analysed and suitable fit was achieved after minimal changes (rescoring one item). Pearson correlation coefficients were used to examine the relationships between the interval scores produced from the questionnaires. The Constant (r = −0.69, P < 0.0001) and Intermittent (r = −0.65, P < 0.0001) subscales significantly and negatively correlated with the Bodily Pain subscale suggesting that both measure pain.
Discussion
The current study explored the fit between data obtained from the ICOAP questionnaire and the Rasch model. The Constant subscale, Intermittent subscale and Total scale were analysed separately. Item 2 was removed from the Constant subscale due to misfit and multidimensionality. This resulted in adequate fit to the model. Items 8 and 9 were deleted from the Intermittent subscale because of DIF and misfit, respectively, which improved the fit statistics. The Total scale exhibited evidence of response dependency and multidimensionality, which violates the assumption of local independence5,22,34,35. There was also evidence of item and person misfit and DIF. Four items were removed from the analysis (items 2, 6, 7, and 8), which resolved the response dependency and multidimensionality and improved the fit. However, a number of participants continued to exhibit misfit after the scale was altered.
Hawker et al.6 observed factorial complexity when exploring the ICOAP with principal components analysis. The current study showed that the Constant and Intermittent subscales meet the requirements of the Rasch model once a few items have been removed. Principal components analysis of the residuals for the Total scale showed multidimensionality with items from the Constant and Intermittent subscales mostly loading in opposite directions. This suggests that the ICOAP is measuring both types of pain separately. Although removal of a few misfitting items from the Total scale resulted in an unidimensional measure supporting the findings of Hawker et al., the Constant and Intermittent items continued to load in opposite directions even after changes were made. Considering these findings it is suggested that the ICOAP is used as a measure of two different types of pain, as originally designed, rather than a general measure of pain.
Response dependency was observed between several items in the Total scale, but with the exception of items 2 and 8 it only occurred between items within the same subscales. This is important because the items ask participants about constant and intermittent pain in the same way (e.g., Items 3/9 – how much has your constant knee pain/knee pain that comes and goes affected your overall quality of life), which means that the participants were able to separate their sensations of constant and intermittent pain. If they were not able to do this, then their responses to items on the Constant subscale would have an impact on their responses to items on the Intermittent subscale creating response dependency.
These findings highlight the multidimensional nature of pain experience. It is well recognised that numerous factors need to be considered when assessing the mechanisms of pain such as physical (e.g., function), emotional (e.g., depression), social (e.g., family support) and cognitive (e.g., coping strategies)36. This study has shown that pain can be subdivided according to the periodicity of symptoms, which is well-captured by the ICOAP questionnaire.
The study has some limitations that need to be considered. The Intermittent subscale initially had misfitting participants. However, this was resolved by alterations to the scale. In contrast, a few participants misfit the Total scale even after changes were made. This raises concerns over the external validity of the scale22. Most of the misfitting participants (79%) had high negative fit residuals, which means that their responses were too deterministic37. These participants tended to select mostly the same response option for each item leading to less variation in their answers. This may have been due to them being given more than one questionnaire to complete leading to fatigue and less thought about each item38.
The sample size of the current study was slightly small. However, it was sufficient to have 99% confidence that the item calibrations were within ±0.5 logits39. It is useful to have more data, but it is not always feasible. Sample size requirements in Rasch analysis are in part governed by targeting. The results of this study have shown that the ICOAP is relatively well targeted with knee OA participants. The response rate was a little low in the study, which raises concerns over the generalisability of the findings. However, comparable response rates have been reported in similar studies30 and the available demographic information from those who did not respond suggests that they were similar in terms of gender and age. Nevertheless it is recommended that further Rasch analyses are conducted to corroborate these results.
There are two versions of the ICOAP; one for knee OA and the other for hip OA. The current study only used the knee OA version because only these patients were included. Further studies examining the fit between the hip version and the Rasch model would be useful. It would be interesting to investigate whether knee and hip OA patients produce different ICOAP scores when their estimated levels of pain are equivalent. Thus a study including both patient types and an examination of DIF would be particularly desirable.
In conclusion, the Constant and Intermittent subscales of the ICOAP fit the Rasch model following removal of a few items. The Total scale can be adjusted to improve its fit to the model, but significant changes were required and a number of participants misfit raising concerns over its external validity. It is recommended that the Constant and Intermittent subscales are used rather than the Total scale. Clinicians and researchers wishing to use parametric statistics with these subscales may use the conversion values provided in the Appendix.
Contributions
Professors Walsh and Lincoln worked on the conception and design and obtaining of funding for the study. Mrs Wheeler contributed to administrative support to the design and execution of recruitment processes and patient and public involvement. Dr Moreton was responsible for the analysis and interpretation of the data and drafting the article. All authors provided critical appraisal of the article and approved the final version before submission. Dr Moreton takes responsibility for the integrity of this work and can be contacted at bryan.moreton@nottingham.ac.uk.
Role of funding source
This research was funded by Arthritis Research UK. The design of the project was approved by the study sponsors.
Conflict of interests
The authors have no competing interests to declare.
Acknowledgements
The authors are grateful to Professor Michael Doherty, Professor Brigitte Scammell, Linda Miller and Deborah Wilson for their assistance with the study, and to all the study participants for their time and attention.
Contributor Information
B.J. Moreton, Email: bryan.moreton@nottingham.ac.uk.
M. Wheeler, Email: maggie.wheeler@nottingham.ac.uk.
D.A. Walsh, Email: david.walsh@nottingham.ac.uk.
N.B. Lincoln, Email: nadina.lincoln@nottingham.ac.uk.
Appendix.
Items 1, 3, 4, and 5 from the Constant Pain subscale should be summed to provide a score from 0 to 16. Items 6, 7, 10 and 11 from the Intermittent Pain subscale should be summed to provide a score from 0 to 16. The raw score can then be converted to an interval scale using the corresponding ‘Rasch score’ value.
| Subscale | Raw score | Rasch score | Standard error |
|---|---|---|---|
| Constant pain | 0 | −7.48 | 1.47 |
| 1 | −6.29 | 1.19 | |
| 2 | −5.17 | 1.07 | |
| 3 | −4.10 | 1.01 | |
| 4 | −3.14 | 0.98 | |
| 5 | −2.22 | 0.96 | |
| 6 | −1.32 | 0.94 | |
| 7 | −0.44 | 0.93 | |
| 8 | 0.42 | 0.91 | |
| 9 | 1.22 | 0.87 | |
| 10 | 1.94 | 0.83 | |
| 11 | 2.60 | 0.82 | |
| 12 | 3.23 | 0.82 | |
| 13 | 3.88 | 0.84 | |
| 14 | 4.58 | 0.90 | |
| 15 | 5.39 | 1.05 | |
| 16 | 6.35 | 1.43 | |
| Intermittent pain | 0 | −4.77 | 1.42 |
| 1 | −3.94 | 0.97 | |
| 2 | −3.27 | 0.81 | |
| 3 | −2.73 | 0.76 | |
| 4 | −2.20 | 0.75 | |
| 5 | −1.65 | 0.74 | |
| 6 | −1.10 | 0.73 | |
| 7 | −0.57 | 0.73 | |
| 8 | −0.06 | 0.72 | |
| 9 | 0.46 | 0.73 | |
| 10 | 1.00 | 0.74 | |
| 11 | 1.55 | 0.75 | |
| 12 | 2.11 | 0.77 | |
| 13 | 2.70 | 0.80 | |
| 14 | 3.34 | 0.88 | |
| 15 | 4.16 | 1.05 | |
| 16 | 5.20 | 1.44 | |
References
- 1.Peat G., McCarney R., Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dieppe P.A., Lohmander L.S. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365:965–973. doi: 10.1016/S0140-6736(05)71086-2. [DOI] [PubMed] [Google Scholar]
- 3.Rosemann T., Laux G., Szecsenyi J., Wensing M., Grol R. Pain and osteoarthritis in primary care: factors associated with pain perception in a sample of 1,021 patients. Pain Med. 2008;9:903–910. doi: 10.1111/j.1526-4637.2008.00498.x. [DOI] [PubMed] [Google Scholar]
- 4.Katz J.N., Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–252. doi: 10.1016/s0039-6109(05)70381-9. [DOI] [PubMed] [Google Scholar]
- 5.Tennant A., Conaghan P. The Rasch measurement model in rheumatology: what is it and why use it? When should it be applied, and what should one look for in a Rasch paper? Arthritis Rheum. 2007;57:1358–1362. doi: 10.1002/art.23108. [DOI] [PubMed] [Google Scholar]
- 6.Hawker G.A., Davis A.M., French M.R., Cibere J., Jodan J.M., March L. Development and preliminary psychometric testing of a new OA pain measure – an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16:409–414. doi: 10.1016/j.joca.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawker G.A., Stewart L., French M.R., Cibere J., Jodan J.M., March L. Understanding the pain experience in hip and knee osteoarthritis – an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16:415–422. doi: 10.1016/j.joca.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 8.Hawker GA. Measure of intermittent and constant osteoarthritis pain: ICOAP. In: OARSI User Guide, 2010.
- 9.Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum. 1989;18:14–17. doi: 10.1016/0049-0172(89)90010-3. [DOI] [PubMed] [Google Scholar]
- 10.Gonçalves R.S., Cabri J., Pinheiro J.P., Ferreira P.L., Gil J. Cross-cultural adaptation and validation of the Portuguese version of the intermittent and constant osteoarthritis pain (ICOAP) measure for the knee. Osteoarthritis Cartilage. 2010;18:1058–1061. doi: 10.1016/j.joca.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Kessler S., Grammozis A., Gϋnther K.P., Kirschner S. Testtheoretische Überprüfung der deutschen Version des Intermittent and Constant Osteoarthritis Pain Score (ICOAP) – ein Fragebogen zur Schmerzerfassung bei Patienten mit Gonarthrose. Z Orthop Unfallchir. 2011;149:22–26. doi: 10.1055/s-0030-1249967. [DOI] [PubMed] [Google Scholar]
- 12.Maillefert J.F., Kloppenburg M., Fernandes L., Punzi L., Gϋnther K.P., Martin Mola E. Multi-language translation and cross-cultural adaption of the OARSI/OMERACT measure of intermittent and constant osteoarthritis pain (ICOAP) Osteoarthritis Cartilage. 2009;17:1293–1296. doi: 10.1016/j.joca.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Davis A.M., Lohmander L.S., Wong R., Venkataramanan V., Hawker G.A. Evaluating the responsiveness of the ICOAP following hip or knee replacement. Osteoarthritis Cartilage. 2010;18:1043–1045. doi: 10.1016/j.joca.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Bond M., Davis A.M., Lohmander L.S., Hawker G.A. Responsiveness of the OARSI–OMERACT osteoarthritis pain and function measures. Osteoarthritis Cartilage. 2012;20:541–547. doi: 10.1016/j.joca.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 15.OARSI OARSI initiatives: pain indexes. http://www.oarsi.org/index2.cfm?section=OARSI_Initiatives&content=Pain_Radiological_Indexes
- 16.Wright T., Goldring S. Reaching consensus and highlighting future directions for research: the osteoarthitis summit breakout sessions. HSS J. 2012;8:80–83. doi: 10.1007/s11420-011-9252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Es P.P., Luijsterburg P.A.J., Dekker J., Koopmanschap M.A., Bohnen A.M., Verhaar J.A.N. Cost-effectiveness of exercise therapy versus general practitioner care for osteoarthritis of the hip: design of a randomised clinical trial. BMC Musculoskelet Disord. 2011;12:232. doi: 10.1186/1471-2474-12-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verkleij S.P.J., Luijsterburg P.A.J., Koes B.W., Bohnen A.M., Bierma-Zeinstra S.M.A. Effectiveness of diclofenac versus acetaminophen in primary care patients with knee osteoarthritis: [NTR1485], DIPA-trial: design of a randomized clinical trial. BMC Musculoskelet Disord. 2010;11:7. doi: 10.1186/1471-2474-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rasch G. University of Chicago; Chicago: 1960. Probabilistic Models for Some Intelligence and Attainment Tests. [Google Scholar]
- 20.Ko Y., Lo N.N., Yeo S.J., Yang K.Y., Yeo W., Chong H.C. Rasch analysis of the Oxford Knee Score. Osteoarthritis Cartilage. 2009;17:1163–1169. doi: 10.1016/j.joca.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Tennant A., Pallant J.F. Unidimensionality matters! (A tale of two smiths?) Rasch Meas Trans. 2006;20:1048–1051. [Google Scholar]
- 22.Pallant J.F., Tennant A. An introduction to the Rasch measurement model: an example using the Hospital Anxiety and Depression Scale (HADS) Br J Clin Psychol. 2007;46:1–18. doi: 10.1348/014466506x96931. [DOI] [PubMed] [Google Scholar]
- 23.Kellgren J.H., Lawrence J.S. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–501. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doherty M., Hawkey C., Goulder M., Gibb I., Hill N., Aspley S. A randomised controlled trial of ibuprofen, paracetamol or a combination tablet of ibuprofen/paracetamol in community-derived people with knee pain. Ann Rheum Dis. 2011;70:1534–1541. doi: 10.1136/ard.2011.154047. [DOI] [PubMed] [Google Scholar]
- 25.Hays R.D., Prince-Embury S., Chen H. The Psychological Corporation; San Antonio, TX: 1998. RAND-36 Health Status Inventory. [Google Scholar]
- 26.Andrich D., Lyne A., Sheridan B., Luo G. RUMM Laboratory; Perth: 2003. RUMM2020. [Google Scholar]
- 27.Andrich D. A rating formulation for ordered response categories. Psychometrika. 1978;43:561–573. [Google Scholar]
- 28.Masters G.N., Wright B.D. The partial credit model. In: van der Linden W.J., Hambleton R.K., editors. Handbook of Modern Item Response Theory. Springer; New York: 1997. [Google Scholar]
- 29.Shea T.L., Tennant A., Pallant J.F. Rasch model analysis of the Depression, Anxiety and Stress Scales (DASS) BMC Psychiatry. 2009:9. doi: 10.1186/1471-244X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pallant J.F., Keenan A.-M., Misajon R.A., Conaghan P.G., Tennant A. Measuring the impact and distress of osteoarthritis from the patients' perspective. Health Qual Life Outcomes. 2009;7:37. doi: 10.1186/1477-7525-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramp M., Khan F., Misajon R.A., Pallant J.F. Rasch analysis of the Multiple Sclerosis Impact Scale (MSIS-29) Health Qual Life Outcomes. 2009;7:58. doi: 10.1186/1477-7525-7-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith E.V. Detecting and evaluating the impact of multidimensionality using item fit statistics and principal component analysis of residuals. J Appl Meas. 2002;3:205–231. [PubMed] [Google Scholar]
- 33.Linacre J.M. When to stop removing items and persons in Rasch misfit analysis? Rasch Meas Trans. 2010;23:1241. [Google Scholar]
- 34.Baghaei P. Local dependency and Rasch measures. Rasch Meas Trans. 2008;21:1105–1106. [Google Scholar]
- 35.Wright B.D. Local dependency, correlations and principal components. Rasch Meas Trans. 1996;10:509–511. [Google Scholar]
- 36.Keefe F.J., Somers T.J. Psychological approaches to understanding and treating arthritis pain. Nat Rev Rheumatol. 2010;6:210–216. doi: 10.1038/nrrheum.2010.22. [DOI] [PubMed] [Google Scholar]
- 37.Curtis D.D. Person misfit in attitude surveys: influences, impacts and implications. Intern Educ J. 2004;5:125–144. [Google Scholar]
- 38.Younger J., McCue R., Mackey S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep. 2009;13:39–43. doi: 10.1007/s11916-009-0009-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Linacre J.M. Sample size and item calibration stability. Rasch Meas Trans. 1994;7:328. [Google Scholar]