Abstract
Background
Primary open angle glaucoma is reported to blind 150,000 people in the Nigerian population and over 7000 in Rivers State, and requires constant follow-up. Compliance is a challenge, given that most inhabitants live below the poverty line. This study was performed to determine how Nigerian patients are affected economically by the disease.
Methods
Consecutive adult patients attending the eye clinic of the University of Port Harcourt Teaching Hospital, Rivers State, Nigeria, with a diagnosis of primary open angle glaucoma and on outpatient antiglaucoma treatment in the first 6 months of 2006, were recruited for the study. The lowest paid government worker was on USD50 (N7500.00) per month and the gross domestic product per capita was USD1150 for the period under review.
Results
We enrolled 120 consecutive patients of mean age 52.7 ± 10.4 years, with a male to female ratio of 2:3. The most common occupations were in the civil service (n = 56, 46.7%). All participants were on topical antiglaucoma treatment. The average cost of medical antiglaucoma medication was N6000 (USD40) per month. Computed to include indirect costs, including medical laboratory tests, transportation, and care by patient escorts, an average sum of USD105.4 (N15,810) was spent by each patient per month. Most of the patients (73.3%) were responsible for their own treatment costs. No patient accepted the cheaper option of surgery (USD275.4, N41,310). Eighty of the patients (66.7%) visited our eye clinic monthly. Direct and indirect loss to the economy was USD3,064587 per annum from those already blind. This was in addition to the USD 4.1 million being spent yearly on medical treatment by those who were visually impaired by glaucoma.
Conclusion
Middle-income earners spent over 50% of their monthly income and low-income earners spend all their monthly earnings on treatment for glaucoma. This situation often resulted in noncompliance with treatment and hospital follow-up visits. To reduce the economic burden of glaucoma, trabeculectomy performed by experienced surgeons should be offered as first-line treatment for glaucoma in this country, rather than medical therapy.
Keywords: economic burden, chronic glaucoma, blindness, Rivers State, Nigeria
Introduction
Glaucoma is recognized as an important cause of blindness. This is justified, because it is the second leading cause of blindness worldwide (after cataract),1–3 and is responsible for about a third of those currently blind. The prevalence of glaucoma is about 1% in the population older than 50 years, and the rate increases with age, being particularly high in Blacks.5 The disease affects an estimated 67 million people globally.1,4 Glaucoma is documented to blind 1% of people in Africa,1 and is also reported to blind 147,000 people in the Nigerian population aged over 40 years.5 Studies done locally show that glaucoma is responsible for 0.76% of the prevalence of blindness and 0.28% of those with impaired vision.5,6
Most cases of blindness (75%–80%) can be prevented.5,7 Although glaucoma cannot be prevented or cured, it is controllable, but once the visual field is lost it can never be regained.8–10 The number of blind people in Nigeria aged 40 years and over is about 1.13 million, with 150,000 being blind because of glaucoma nationwide.5 In a study performed in a general hospital in Ibadan, Nigeria, 29% of those with bilateral blindness suffered from glaucoma.11 In a community-based study of rural patients in the same area of southwestern Nigeria, glaucoma accounted for 21.1% of eye problems, and was also responsible for a third of cases of blindness.6
Primary open angle glaucoma is the most frequent type of glaucoma occurring in our region.12,13 Primary open angle glaucoma is mostly associated with damage caused by intraocular hypertension, which can be delayed by medication, surgery, or laser therapy. In a study conducted in a sample rural population from Rivers State in 1998, glaucoma was not found to cause blindness in both eyes, but to be a cause of blindness in at least one eye in 11.7% of cases.14 Ten years later, in a national survey of blindness and visual impairment in the same state of Nigeria, glaucoma was found to be responsible for up to 16.7% of cases of blindness.5 Those who are presently blind number at least 7615, with a further 3000 people with at least varying degrees of visual impairment.5
Glaucoma is characterized by chronic and progressive damage to the optic nerve. This condition has been shown to lead inexorably to blindness at a rapid rate if treatment is not instituted within months, and up to 3 years in some cases. However, in a study from Glasgow,9 it was calculated that if medical treatment was instituted in a timely manner and sustained, the rate of progression of visual field deterioration reduced significantly to 3% per annum, suggesting it might have taken at least 33 years for glaucomatous eyes to progress to blindness, but most did not present early enough at first onset of the disease, and so blindness appeared to ensue rapidly.
Surgery is the recommended first-line treatment for chronic glaucoma, particularly the high pressure type, in young Blacks.10,13,15 In order to reduce the delay in uptake of surgery, it is important to remember when counseling patients to tell them that if antiglaucoma medications are used for over a year, the success of surgical intervention is markedly reduced due to the resultant fibrosis and pemphigoid reaction resulting from their long-term use.9
However, in developed countries, it is documented that there is a reduction in use of surgical procedures to treat the condition, especially as first-line therapy. The greater part of medical expenditure is on medication at present, with new, more potent, better tolerated, but more costly drugs replacing the older and less expensive ones.4 Evidence from one trial suggests that for mild open angle glaucoma, the visual field deterioration when patients are followed up for over 5 years does not differ significantly according to whether treatment is with medication or trabeculectomy. Clearly, this assumes that medications are used consistently over that period. Reduced vision, cataract, and eye discomfort are more likely with trabeculectomy, which may reduce uptake of the procedure.10,15 Therefore, there is no cure and only control is possible, with lifelong follow-up needed in most cases. Observations by investigators in the field of glaucoma have predicted that this trend will lead to increased rates of blindness from the disease over the decades to come.16
Glaucoma undoubtedly puts significant stress on family finances. Cost of illness studies have shown that glaucoma is very important because direct medical costs are significant, with direct and indirect nonmedical costs also being very considerable.17,18 This in turn has caused noncompliance on the part of patients, particularly among those on “modern” topical medication, especially with multiple schedules, leading to a vicious circle which ultimately worsens the visual outcome. The current move from first-line surgical treatment to newer, more potent, better tolerated, but more expensive topical medications is another factor leading to noncompliance, particularly when patients, for various economic reasons, can no longer continue to pay for their treatment.4 The indirect costs of the repeat visits necessary for intraocular pressure checks have also been implicated. Treatment costs are directly related to disease severity and number of treatments used, and most Nigerians are living below the poverty line. In this region, we observed that patients find it difficult to maintain compliance with the treatment modalities for glaucoma, and the economic challenges involved may be contributory. The economic loss to society as a result of glaucoma is also considerable. Therefore, this study was performed to determine the extent to which glaucoma challenges patients economically in this part of the world. The circumstances surrounding and promoting this financial burden were also investigated, so that recommendations, if any, can be made to mitigate it.
Materials and methods
All consecutive adult patients attending the eye clinic of the University of Port Harcourt Teaching Hospital, Rivers State, Nigeria, with a diagnosis of chronic primary open angle glaucoma (International Classification of Diseases, 9th Revision code 365.11) and no fewer than 4 months of outpatient treatment within the period of January–June 2006 were included in this study in order for responses to be comparable. All pediatric, angle closure, and secondary glaucoma patients were excluded.
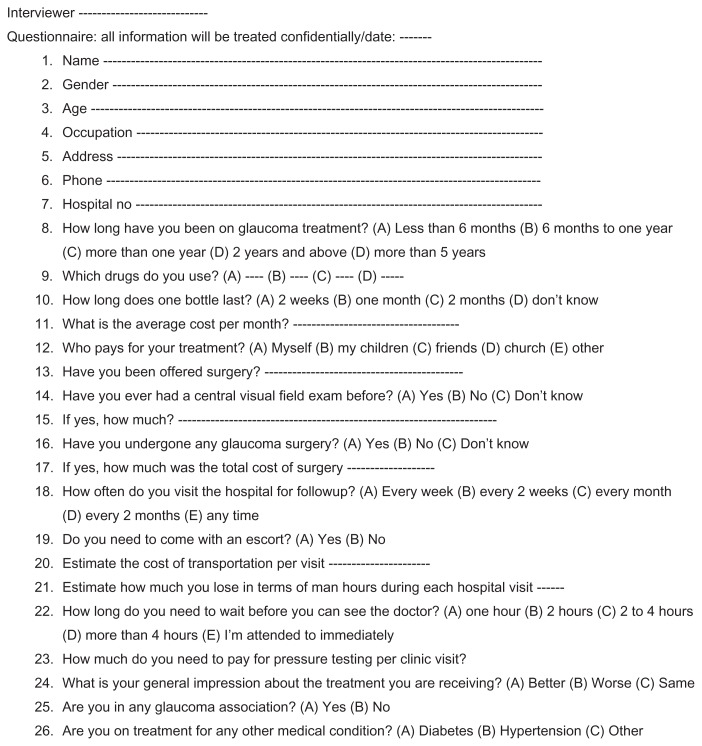
Informed consent was taken from the participants after adequate verbal explanation was given in the best understood language/dialect. Questionnaires (see Figure 1) were administered to each patient after an adequate explanation of each item. Productivity losses were determined based on work days lost on account of hospital visits.19,20 At the time of this study, the lowest paid government worker earned USD106.7 (N16,000) per month. Estimates of nonmedical costs included change of residence in order to compensate for reduced vision, burden on carer, paid home help, and loss of income.21 Direct and indirect losses to the state economy incurred by those who were already blind from glaucoma was calculated using cost of illness methodology recommended in similar studies by Shamanna et al22 and by Cook23 using gross domestic product per capita, which was taken to be USD1150 for the period under review, ie, 2006.24 Direct costs measure the cost of resources used to treat a particular illness, while indirect costs measure the value of resources lost due to a particular illness, in this case, primary open angle glaucoma.25
Figure 1.
Questionnaire on economic burden of glaucoma.
The overall prevalence of blindness was taken to be 0.8% in all age groups in the South South zone of Nigeria where Rivers State is located.5 The number of people blinded by glaucoma was estimated to be 7615 (glaucoma is responsible for 16.7% of cases of blindness in Rivers State), assuming a total population in the region of 5.7 million.26 Twenty percent of cases of blindness were estimated to be in the economically productive age group (16–64 years), based on blindness prevalence data. It was also assumed that 10% of the total productive time of one economically productive member of the family of each individual blinded by glaucoma is lost in taking care of the blind person.22,23,25 This number of blind people was also taken to be economically productive at 25% of the productivity level of a sighted member of the labor force. Using these data and assumptions,23 the annual economic loss for Rivers State as a result of glaucoma was calculated as follows:
direct loss = number of people blind because of glaucoma in the state × 0.20 × gross domestic product per capita
indirect loss = number of people blind because of glaucoma in the state × 0.1 × gross domestic product per capita
economic productivity of blind people = number of people blind because of glaucoma in the state × 0.20 × 0.25 × gross domestic product per capita
net loss = direct loss + indirect loss − economic productivity of people blind because of glaucoma.
Blindness from glaucoma in children was not factored in. The exchange rate for the Naira dollar was taken to be N150.00 for USD1. The hospital pharmacy and two nearby independent retail pharmacies were consulted to corroborate the figures given by the patients, and their copies of accounting payment slips were checked for the commonly prescribed antiglaucoma medications given to patients at the time of this study. A 5 mL bottle of an ocular medication prescribed twice daily or a 2.5 mL equivalent prescribed once daily was taken as a one-month supply for any given patient along with a 30-day supply of antioxidants. The cost of surgery was taken as the standard cost that was charged by the hospital at the time of the study. Responses to each question were filled in on the form by the interviewer. Analysis was performed with the aid of a simple calculator and a statistician.
Results
Demographics
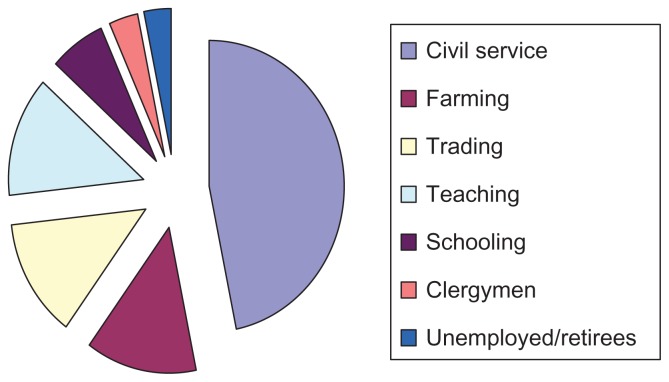
A total of 120 consecutive patients who gave their informed consent were included in the survey. In total, there were 72 (60%) females and 48 (40%) males, giving a male to female ratio of 2:3. The study group was of mean age 52.7 ± 10.4 (range 24–78) years (see Table 1). Civil servants formed the largest occupational group (n = 56, 46.7%), but the sample also included farmers (n = 16, 13.3%), traders (n = 16, 13.3%), and teachers (n = 16, 13.3%), with a few students (n = 8, 6.7%) and clergymen (n = 4, 6.7%). Others were either unemployed or retirees (n = 4, 3.33%, see Figure 2).
Table 1.
Age and gender distribution of the study population
| Age group (years) | Male | Female | Total | ||
|---|---|---|---|---|---|
|
|
|
||||
| n | % | n | % | ||
| 20–29 | 6 | 5.0 | 3 | 2.5 | 9 (7.5%) |
| 30–39 | 6 | 5.0 | 8 | 6.7 | 14 (11.7%) |
| 40–49 | 11 | 9.2 | 12 | 10.0 | 23 (19.2%) |
| 50–59 | 7 | 5.8 | 18 | 15.0 | 25 (20.8%) |
| 60–69 | 10 | 8.3 | 24 | 20.0 | 34 (28.3%) |
| 70–79 | 8 | 6.7 | 7 | 5.8 | 15 (12.5%) |
| Total | 48 | 40 | 72 | 60 | 120 (100%) |
Figure 2.
Occupational status of the study population.
Concurrent chronic ailments
Twenty-four (20%) of the participants are already on treatment for diabetes, while 40 (33.3%) were on treatment for hypertension. However, 56 (46.7%) had no systemic illness.
Direct treatment costs
All the participants were on medical treatment with antiglaucoma drugs at the time of interview. None of the respondents had consented to undergo surgery. The majority had been on treatment for the previous 2 years (n = 48, 40%), while 40 (33.3%) had been receiving treatment for 6 months to one year. Eight patients (6.7%) had been on treatment for over a year, while 24 (20%) had been on treatment for less than 6 months.
The patients were mainly on topical antiglaucoma treatment, with 112 on other regular medications, including beta blockers, eg, timolol (93.3%), eight on prostaglandin analogs, eg, latanoprost (6.7%), and eight on acetazolamide (6.7%). From the reported experience of the respondents, one 5 ml bottle of topical medication lasted for 2 weeks (n = 56, 46.7%) to one month (n = 56, 46.7%) on average. The monthly cost of medications was between N650 (USD4.3) and N8220 (USD54.8), with an average of N6000 (USD40).
Eight respondents (73.3%) were financially responsible for their own treatment, while 16 (13.3%) reported that their children paid for their treatment. A further 16 patients reported that other sources, including churches and other organizations, were paying for their treatment (13.3%). Sixteen (13.3%) subjects reported that they had been offered surgery as an alternative, but none of them had taken up this option. The current cost of surgery in the hospital is N30,000 (USD200). One hundred and twelve (93.3%) subjects said that they had undergone central visual field examination at some point in the past, at a mean cost of N2500 (USD16.7). The frequency with which this test is repeated varies from patient to patient, but on average was recommended every 4–6 months in our study sample. The cost of intraocular pressure testing was on average about N300 (USD2) per visit.
Direct nonmedical costs
Some of the patients visited the clinic fairly regularly, with 16 of them (13.3%) visiting every 2 weeks, and 80 (66.7%) visiting once a month. Sixteen patients visited the clinic irregularly. Only 24 (20%) were escorted to the clinic. Another 24 (20%) had access to a private vehicle for transport, while the rest had to use public transport, with the cost of each trip ranging between N600 (USD4) and N3000 (USD20s), and an average of N2500 (USD16.7) per visit. The average estimated monthly income for these patients ranged from zero (n = 10, 8.3%) to N97,000 (USD646.7, n = 20, 16.7%), with a mean of N31,770 (USD211.8).
Indirect (productivity) costs
Using the human per capita method,25 the estimated number of hours lost while waiting for the doctor was 3–8 hours per visit, with an average of USD30 lost per visit to the hospital. However, four subjects (6.7%) said that they lost up to USD200 (N30,000) per visit (n = 25, 20.8%) when waiting for this length of time at the hospital. This is in addition to the time the escorts spent away from work. Twelve patients said they did not lose any income by coming to hospital.
Quality of life
Thirty-two of the respondents reported feeling better than when they had first presented (53.3%). Twenty-four felt that they were worse despite treatment (40%), while four felt that there was no change (6.7%). None of the subjects belonged to an umbrella body like the Nigeria Glaucoma Association, with all patients being seen in the same general ophthalmic clinic.
Effect on Rivers State economy
The direct loss to the Rivers State economy attributable to glaucoma was calculated to be 7615 × 0.20 × 1150 = USD1,751,450.00, and the indirect loss was calculated to be 7615 × 0.1 × 1150 = USD875,275.00. Loss of economic productivity in people blind as a result of glaucoma was 7615 × 0.20 × 0.25 × 1150 = USD437,862.50. The net loss to the Rivers State economy per annum was USD1,751,450.00 + 875,275.00 − 437,862.50 = USD3,064,587.50, ie, approximately USD3.1 million per year.
Total economic burden
The average glaucoma patient on medical treatment whose average monthly income was about USD211.8 spent an average of USD105.4 per month on antiglaucoma drugs, tests, transport, and time away from work. This equates to 49.76% of their monthly income, approximately half of the monthly income for the patients with glaucoma attending the eye clinic, and totally unaffordable on the monthly income of the lowest paid government worker earning USD50 (N7500) per month. This translates into USD1264.8 per annum per person for treatment of glaucoma. A further 7% are visually impaired to various degrees from glaucoma,6 giving a figure of USD4,095,000 being spent annually on treatment for the disease. In addition to this is the USD3.1 million lost yearly to cover the costs of treating associated health conditions that glaucoma patients may also have. In total, uptake of the surgical option would have cost USD275.4 (N41,310) up front on average, particularly if it is successful and there is no need for repeat surgery.
Discussion
Almost all the respondents in our sample of consecutive patients opted for medical rather than surgical treatment of glaucoma, even though quite a number of them were educated (see Figure 2). Many quoted the high cost of surgery as a factor in their decision. Another study has reported the same problem of poor uptake of glaucoma surgery in Edo State, Nigeria.27 After analyzing the medical and surgical therapy costs, the same study further concluded that the costs were comparable over a 3-year period. However, the investigators also acknowledged that the associated indirect costs were not taken into consideration, and these would have been much higher in some cases than for direct treatment of glaucoma. In another study, Varma et al reported that treatment of glaucoma was very cost-effective when the costs associated with diagnostic assessment were excluded. However, it may be difficult for diagnostic costs to be separated from treatment costs, and all have to be paid for one way or another. However, despite the initial high cost, the surgical option may be better in the long term for selected cases, in particular younger people, and also when compliance may be an issue. A study by Cantor et al using a Markov model in the US29 showed that the difference between the cost of medication and the cost of filtering surgery is only USD200 over a period of 5 years, therefore justifying the continued use of medication and reduction in first-line management with surgery in their country. However, this may not be feasible in reality because this was a simulated study where everything goes according to plan and there is insurance to cover costs. This is practically nonexistent in our study location (Rivers State). The authors also conceded at the end of their study that their findings still need to be validated by both retrospective and prospective observational studies.29
Therefore, the choice of treatment, whether surgical or medical, needs to be individualized. The human misery and social cost of blindness, especially in countries that can ill afford it, like Nigeria, are profound. Loss of productivity from high numbers of blind people is enormous. Therefore, cost of illness methodology is useful in measuring the economic burden of disease, and estimates the maximum amount that could potentially be saved or gained if a given disease was eradicated. These studies have been instrumental in public health policy because they highlight the magnitude of the impact of an illness on society or a part of society.25 It has been calculated that up to USD3.1 million per annum is lost in Rivers State alone as a result of blindness from glaucoma. A further USD1300 (N195,000) is spent on treating this condition per person per annum. An additional 7% of people are visually impaired by glaucoma,6 so approximately USD 4.1 million is required to be spent yearly on its treatment. In our study, most subjects suffering from glaucoma could not afford to have the condition treated because about half of their monthly income would be consumed on care and purchase of medication. Rivers State is a region where glaucoma is responsible for fewer cases of blindness from glaucoma than some studies have documented.6,11 Other states in Nigeria with a higher burden of suffering from glaucoma will likely lose more. However, there are very few data in Nigeria with which we can compare our results. A related paper in the same geopolitical zone as ours looked at the cost of medical and surgical management of glaucoma over a 3-year period and found out that there was no statistically significant difference between the costs of the two treatment options.27
Although none of the patients took up the surgical option for glaucoma within the study period, successful surgery may still be cheaper in the long term than constant use of medication, which is not necessarily used consistently. In fact, the global economic productivity loss due to blindness was estimated to be USD19 billion in 2000.30 Even a developed economy cannot afford the costs of avoidable blindness, and vision loss has been ranked seventh in the causes of loss of well-being in an Australian study.31
In our series, glaucoma was seen more often in females than in males, though this was a hospital-based study and generally there is no gender predilection in the open angle type of glaucoma which is more common in this region. One of the risk factors for glaucoma is advancing age,9,32 with the condition becoming more common in the elderly.33 Due to a general proportionate increase in the elderly population, the numbers of patients with glaucoma will likely increase in the coming years.34
In our series, the average age of the patients was 52.6 years, with some patients aged over 70 years. This age range is similar to other studies –53.5 years,23 where the peak age range was between 41 and 70 years.6 Within this age group, additional medical challenges requiring attention become more frequent. This obviously requires efficient allocation of health care resources for management of the entire spectrum of disease from suspected to advanced glaucoma and from juvenile onset glaucoma to glaucoma in the elderly. Management of the disease has to be cost-effective. This is important, considering that the average monthly income of the respondents in our study was only USD211.8. Early disease recognition is also important, because this helps to contain both direct and indirect costs19,20,34,35 and also limits loss of economic productivity from functional visual loss or impairment as a result of delayed treatment. Once vision is impaired, the cost of accessing eye care increases. Visually impaired individuals need to get someone else who is most likely to be economically productive to leave whatever he or she is doing and assist in getting them to the hospital. If this assistance is not possible regularly, eye care is not going to be regular and vision is likely to get worse.
The primary reason for failure to use eye care services in Ethiopia has been documented as the indirect costs (overall, reported by 40% of respondents) associated with accessing appropriate services.36 Therefore, the focus right now is on cost-effective remedies and problems that can be prevented by primary health care measures, as in the Vision 2020 initiative, which has the potential to increase global economic productivity if properly implemented.1,6,17 The World Health Organization has already developed strategies for dealing with a number of diseases, including trachoma, onchocerciasis, childhood blindness, and refractive errors within the Vision 2020 framework. However, glaucoma does not seem to fit into this category, being a progressive condition which can only be detected when there is evidence of loss of function.1,7,33
It is generally agreed that more needs to be done to address glaucoma.8 The indirect burden on the family of accessing eye care may be lessened by encouraging patients to have surgery earlier without trying medication first, before they require assistance to reach the hospital, and by improving the efficiency of existing services. A more patient-friendly hospital will improve efficiency and uptake of eye care. This is obviously a challenge in our hospital at the moment because most patients spend hours waiting to access care at every point, from obtaining folders, to seeing the doctor, to queuing to buy drugs from the pharmacy. However, major moves have been made in this regard, considering that prior to now, there was a central pharmacy, central records, and a central pay point. This made for long hours spent queuing because patients from different clinics had to line up to be attended to at a single point. Steps have now been taken to make each department a total package as far as possible, with each having its own card issuing and records point, its own pay point, and its own pharmacy. This makes for a more patient-friendly hospital, with eye patients in particular not having to go about looking for where to access services. However, there is still room for improvement in terms of efficiency of service delivery.
Up to 40% of the patients in our series had been on intraocular pressure-lowering medications for at least 2 years prior to the time of data collection. In the private sectors in Malawi and Sri Lanka, the cost of innovator products (the pharmaceutical product first given marketing authorization) was three times more than that of generic medicines.20 The same is achievable here, as observed in the prices of products in the hospital pharmacy. Generic products should be promoted by educating professionals and consumers, by implementing appropriate policies and incentives, and by introducing market competition and/or price regulation. Improving governance and management efficiency and assessing local supply options may improve availability. Prices could be reduced by improving purchasing efficiency, eliminating taxes, and regulating markups.
Few patients in our locality agree to undergo a surgical procedure when they are still able to see, because they do not perceive a need. Clearly, this attitude needs to be changed with ongoing health education, because successful surgery will reduce the costs of glaucoma in the long term. Early detection and prompt surgical management is recommended to achieve rapid and sustained intraocular pressure control, which would be expected to reduce hospital visits and expenditure on costly drugs which are not affordable on a lifelong basis for the average glaucoma patient, as shown by this study. The initial cost is very high, ie, as much as USD275.4 (N41,310) up front which is beyond the reach of the average patient. This figure equates to more than 5 months’ salary for the lowest paid worker, which may partly explain the lack of uptake of the surgical option despite the obvious economic benefits. If government and policymakers were to absorb the costs of surgical treatment of glaucoma, particularly for those who have not had medical treatment beforehand, or at least subsidize it, there is likely to be better uptake which will, in turn, mean better control of intraocular pressure in the long term and less loss to the economy.
Furthermore, it has been noted by Taylor et al that, for each dollar spent in the prevention of vision loss and eye care, there is a 5 dollar return to the community.30,36,37 It is important for policymakers to know this, so that effective health care strategies can be adopted to mitigate the effects of glaucoma on the economy.
Most of the subjects with glaucoma in our study were civil servants (46.7%), whose average income is less than USD250 per month, with some of them earning the minimum wage. Also, up to a third of them had related systemic diseases, including diabetes and hypertension, which have a strong association with glaucoma due to the problems they create with optic nerve perfusion,33 and upon which resources are also being spent. Further, it has been documented that patients with chronic disease, eg, diabetes mellitus, have medical expenditure that is 2.4 times higher than the expenditure incurred by the same group in the absence of diabetes.38 This added cost adds further to the financial burden of glaucoma. The number of clinic attendances required for checkups may increase for each added medical condition, and it appears that patients are required to visit the hospital on certain days of the week or month on a repeated and endless cycle. It is well documented that conditions like diabetes worsen the outcome of glaucoma.38 In an American study, 51.8% of direct medical expenditure was incurred by people with diabetes and over the age of 65 years. Patients with comorbid ocular conditions, including cataracts or who have had cataract surgery, diabetic retinopathy, and blindness, had significantly higher total and condition-related health care charges than patients without these conditions (P < 0.0001).38,39 Therefore, the economic burden associated with glaucoma is quite substantial, and priority needs to be placed on research into eye disorders like glaucoma that lead to vision loss, and to develop treatment regimens that are cost-effective and practical to reduce the social and financial burden to patients and to society as a whole.
Conclusion
The economic costs associated with visual impairment from glaucoma are considerable. The present analysis demonstrates that the main economic consequences of visual impairment lie beyond health care systems, and that visual impairment, particularly from glaucoma, has a considerable negative impact on productivity. Visual impairment leads to incapacity and dependence, so our government should be encouraged to finance health innovations that aim to preserve vision. Attention should be focused on individuals diagnosed to have glaucoma necessitating surgery who have not been on medical treatment because the latter reduces the success rate of surgery.
For Rivers State, the costs calculated here as representing the economic burden of glaucoma for those who are already blind because of the disease as well as those undergoing treatment come to a total of USD7.2 million per annum, and is likely to be an underestimate of the true financial burden of glaucoma in Nigeria because they omit intangibles, such as heart ache, pain and suffering, care provided by nonpaid caregivers, and several areas of health care spending where people with glaucoma probably use services at higher rates than people without glaucoma. Eliminating or reducing the health problems caused by glaucoma could significantly improve the quality of life for these people and their families, while at the same time potentially reducing national expenditure by health care services and increasing productivity in the Nigerian economy.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Lewallen S, Courtright P. Blindness in Africa: present situation and future needs. Br J Ophthalmol. 2001;85:897–903. doi: 10.1136/bjo.85.8.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klauss V, Schaller UC. International initiatives for the prevention of blindness. Ophthalmologe. 2007;104:855–859. doi: 10.1007/s00347-007-1613-y. German. [DOI] [PubMed] [Google Scholar]
- 3.Hu S. Blindness as a challenging medical and social problem in China. Yan Ke Xue Bao. 2002;18:4–8. [PubMed] [Google Scholar]
- 4.Rouland JF, Berdeaux G, Lafuma A. The economic burden of glaucoma and ocular hypertension: implications for patient management: a review. Drugs Aging. 2005;22:315–321. doi: 10.2165/00002512-200522040-00004. [DOI] [PubMed] [Google Scholar]
- 5.Kyari F, Gudlavaletti MV, Sivsubramaniam S, et al. Prevalence of blindness and visual impairment in Nigeria. Invest Ophthalmol Vis Sci. 2009;50:2033–2039. doi: 10.1167/iovs.08-3133. [DOI] [PubMed] [Google Scholar]
- 6.Adegbehingbe BO, Majengbasan TO. Ocular health status of rural dwellers in south-western Nigeria. Aust J Rural Health. 2007;15:269–272. doi: 10.1111/j.1440-1584.2007.00906.x. [DOI] [PubMed] [Google Scholar]
- 7.Klauss V, Schaller UC. Tropical ophthalmology – prevention and therapy. Ophthalmologe. 2004;101:741–763. doi: 10.1007/s00347-004-1039-8. German. [DOI] [PubMed] [Google Scholar]
- 8.Foster A, Resnikoff S. The impact of Vision 2020 on global blindness. Eye. 2005;19:1133–1135. doi: 10.1038/sj.eye.6701973. [DOI] [PubMed] [Google Scholar]
- 9.Smith RJH. The enigma of primary open angle glaucoma. Trans Ophthalmol Soc. 1986;105:618–633. [PubMed] [Google Scholar]
- 10.Wormald R, Wilkins MR, Bunce C. Post-operative 5-fluorouracil for glaucoma surgery. Cochrane Database Syst Rev. 2000;2:CD001132. doi: 10.1002/14651858.CD001132. [DOI] [PubMed] [Google Scholar]
- 11.Oluleye TS, Ajaiyeoba AI, Akinwale MO, Olusanya BA. Causes of blindness in Southwestern Nigeria: a general hospital clinic study. Eur J Ophthalmol. 2006;16:604–607. doi: 10.1177/112067210601600416. [DOI] [PubMed] [Google Scholar]
- 12.Omoti AE. A review of the choice of treatment in primary open angle glaucoma. Niger J Clin Pract. 2005;8:29–34. [PubMed] [Google Scholar]
- 13.Enock ME, Omoti AE, Momoh RO. Glaucoma in a suburban tertiary care hospital in Nigeria. J Ophthalmic Vis Res. 2010;5:87–91. [PMC free article] [PubMed] [Google Scholar]
- 14.Omoni AO, Osuntokun BO. The epidemiology of blindness and visual impairment in a fishing Village in Oyorokotor, Rivers state. The Niger Health J. 2005;15:255–260. [Google Scholar]
- 15.Burr J, Azuara-Blanco A, Avenell A. Medical versus surgical interventions for open angle glaucoma. Cochrane Database Syst Rev. 2005;2:CD004399. doi: 10.1002/14651858.CD004399.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73:115–121. [PMC free article] [PubMed] [Google Scholar]
- 17.West SK. Looking forward to 20/20: a focus on the epidemiology of eye diseases. Epidemiol Rev. 2000;22:64–70. doi: 10.1093/oxfordjournals.epirev.a018025. [DOI] [PubMed] [Google Scholar]
- 18.Frick KD, Foster A. The magnitude and cost of global blindness: an increasing problem that can be alleviated. Am J Ophthalmol. 2003;135:471–476. doi: 10.1016/s0002-9394(02)02110-4. [DOI] [PubMed] [Google Scholar]
- 19.Lee PP, Levin LA, Walt JG, et al. Cost of patients with primary open-angle glaucoma: a retrospective study of commercial insurance claims data. Ophthalmology. 2007;114:1241–1247. doi: 10.1016/j.ophtha.2006.10.031. [DOI] [PubMed] [Google Scholar]
- 20.Mendis S, Fukino K, Cameron A, et al. The availability and affordability of selected essential medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ. 2007;85:279–288. doi: 10.2471/BLT.06.033647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lafuma A, Brézin A, Lopatriello S, et al. Evaluation of non-medical costs associated with visual impairment in four European countries: France, Italy, Germany and the UK. Pharmacoeconomics. 2006;24:193–205. doi: 10.2165/00019053-200624020-00007. [DOI] [PubMed] [Google Scholar]
- 22.Shamanna BR, Dandona L, Rao GN. Economic burden of blindness in India. Indian J Ophthalmol. 1998;46:169–172. [PubMed] [Google Scholar]
- 23.Cook C. The economic burden of blindness, the cost of Vision 2020 and the cost benefit of Vision 2020 in Southern Africa. East Afr J Ophthalmol. 2008;14:31–35. [Google Scholar]
- 24.Nigerian National Bureau of Statistics. Poverty profile. 2006. [Accessed October 25, 2011]. Available from: http://www.nigerianstat.gov.ng.
- 25.Segel JE. Cost of illness studies – a primer RTI-UNIC Center of Excellence in Health. Promotion Economics. 2006:1–39. [Google Scholar]
- 26.Ngex. Nigeria places. River State. [Accessed October 25, 2011]. Available from: http://www.ngex.com/nigeria/places/states/rivers.htm.
- 27.Omoti AE, Edema OT, Akpe BA, Musa P. Cost analysis of medical versus surgical management of glaucoma in Nigeria. J Ophthalmic Vis Res. 2010;5:232–239. [PMC free article] [PubMed] [Google Scholar]
- 28.Varma R, Lee PP, Goldberg I, Kotak S. An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol. 2011;152:515–522. doi: 10.1016/j.ajo.2011.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cantor LB, Katz LJ, Cheng JW, Tong KB, Peabody JW. Economic evaluation of medical, laser trabeculoplasty and filtering surgery in treating patients with glaucoma in the United States. Curr Med Res Opin. 2008;24:2905–2918. doi: 10.1185/03007990802379996. [DOI] [PubMed] [Google Scholar]
- 30.Hiratsuka Y, Ono K, Kanai A. The present state of blindness in the world. Nippon Ganka Gakkai Zasshi. 2001;105:369–373. Japanese. [PubMed] [Google Scholar]
- 31.Taylor HR, Pezzullo ML, Keeffe JE. The economic impact and cost of visual impairment in Australia. Br J Ophthalmol. 2006;90:272–275. doi: 10.1136/bjo.2005.080986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:811–890. [No authors listed] [PMC free article] [PubMed] [Google Scholar]
- 33.American Academy of Ophthalmology. Basic and clinical science course 2008–2009 ed. Glaucoma. 10:191–205. [Google Scholar]
- 34.Schmier JK, Halpern MT, Jones ML. The economic implications of glaucoma: a literature review. Pharmacoeconomics. 2007;25:287–308. doi: 10.2165/00019053-200725040-00003. [DOI] [PubMed] [Google Scholar]
- 35.Doshi A, Singh K. Cost-effective evaluation of the glaucoma suspect. Curr Opin Ophthalmol. 2007;18:97–103. doi: 10.1097/ICU.0b013e328040bfcf. [DOI] [PubMed] [Google Scholar]
- 36.Melese M, Alemayehu W, Friedlander E, Courtright P. Indirect costs associated with accessing eye care services as a barrier to service use in Ethiopia. Trop Med Int Health. 2004;9:426–431. doi: 10.1111/j.1365-3156.2004.01205.x. [DOI] [PubMed] [Google Scholar]
- 37.Taylor HR. Costs of interventions for visual impairment. Am J Ophthalmol. 2007;143:561–565. doi: 10.1016/j.ajo.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 38.Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26:913–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 39.Pasquale LR, Dolgitser M, Wentzloff JN, et al. Health care charges for patients with ocular hypertension or primary open-angle glaucoma. Ophthalmology. 2007;115:633–638. doi: 10.1016/j.ophtha.2007.04.059. [DOI] [PubMed] [Google Scholar]