Abstract
Children warrant access to care from clinical pharmacists trained in pediatrics. The American College of Clinical Pharmacy Pediatrics Practice and Research Network (ACCP Pediatrics PRN) released an opinion paper in 2005 with recommendations for improving the quality and quantity of pediatric pharmacy education in colleges of pharmacy, residency programs, and fellowships. While progress has been made in increasing the availability of pediatric residencies, there is still much to be done to meet the direct care needs of pediatric patients. The purpose of this Joint Opinion paper is to outline strategies and recommendations for expanding the quality and capacity of pediatric clinical pharmacy practitioners by 1) elevating the minimum expectations for pharmacists entering practice to provide pediatric care; 2) standardizing pediatric pharmacy education; 3) expanding the current number of pediatric clinical pharmacists; and 4) creating an infrastructure for development of pediatric clinical pharmacists and clinical scientists. These recommendations may be used to provide both a conceptual framework and action items for schools of pharmacy, health care systems, and policymakers to work together to increase the quality and quantity of pediatric training, practice, or research initiatives.
INDEX TERMS: fellowship, pediatric pharmacy, pharmacy education, standardization, residency
INTRODUCTION
Children* are an important segment of the population that pharmacists serve.1–3 In 2010, approximately 73.9 million children resided in the United States, representing 23.9% of the total population.4 Canadian statistics are similar to these, with 7.8 million children making up 23% of the population.5 While most children will spend the majority of childhood in good health, a significant number will still require medical care. According to the 2007 National Survey of Children's Health, over 31 million children, nearly half of the pediatric population, have at least one chronic health condition, and 60% of children have received a prescription medication during the previous 12 months.6 The prevalence of chronic medication use in children is on the rise, with the treatment of type 2 diabetes, asthma, hypertension, dyslipidemia, attention-deficit hyperactivity disorder, and depression accounting for the largest increases. Children accounted for approximately 20% of hospital admissions in 2010, a percentage that has remained relatively unchanged for the past decade (see ref. 9, Table 16, frequency distributions of number of overnight hospital stays during the past 12 months, by selected characteristics, United States, 2010).9 A recent survey of the prescribing patterns at 52 children's hospitals found that on the first day of admission, the median drug exposure was four distinct medications in infants and five in children between 1 and 18 years of age.10 At 30 days of life, cumulative exposure had risen to 25 and 42 medications in infants and older children, respectively. Moreover, of the top 15 medications prescribed for each age group in the survey (infants, children 1–9 years of age, and children 10–17 years of age), half of the medications were on the Institute for Safe Medication Practices list of high-alert medications.11 It is therefore logical to assume that most pharmacists, regardless of setting, will encounter pediatric prescriptions which will necessitate assessing their safety and effectiveness to ensure optimal care.12
All health care providers (including pharmacists) experience significant challenges in providing optimal care for children. Understanding the changes in pharmacokinetic and pharmacodynamic parameters associated with growth and development, the necessity for dose calculations based on body weight or body surface area, the frequent modification of commercially available dosage forms to make them suitable for administration to young patients, and the distinctive aspects of providing medication education for children and their caregivers are all essential aspects of pediatric patient care. Pediatric clinical pharmacists have a documented impact on improvements in pediatric patient safety, quality of life, and economic outcomes dating back to the early 1970s.13–22 A survey conducted in 1983, over a quarter of a century ago, reported that 63% of children's hospitals had established clinical pharmacy services.23 As specialized services, such as pediatrics, have become an expected part of pharmacy practice, more recent publications have highlighted the valuable role of pediatric clinical pharmacists in new settings, ranging from the pediatric cardiac intensive care unit to pediatric nephrology and oncology clinics.24–26 These studies demonstrate the value and impact that highly skilled pediatric clinical pharmacists can have in all settings where direct patient care is rendered.
The importance of highly skilled pediatric clinical pharmacists has also been recognized outside of the pharmacy profession. The American Academy of Pediatrics has asserted that pharmacists who are trained, qualified, experienced, and/or who possess expertise in pediatric pharmacotherapy should be collaborating for the benefit of all pediatric patients in level III neonatal intensive care units27 and pediatric intensive care units28 and in hematology/oncology practice settings.29 The Joint Commission confers on pediatric clinical pharmacists a significant role in pediatric medication safety initiatives. In a 2008 Sentinel Event Alert on preventing pediatric medication errors, their recommendations included having a pediatric pharmacy practitioner on all committees charged with making decisions about medication management, assigning pharmacists with pediatric expertise to high-risk patient care services such as neonatal critical care, pediatric critical care, and pediatric oncology, ensuring that practitioners involved in the care of infants and children have comprehensive, specialized training and, at all times, providing other health care providers with access to a pharmacist having pediatric expertise.30
Members of the American College of Clinical Pharmacy Pediatrics Practice and Research Network (ACCP Pediatrics PRN) and the Pediatric Pharmacy Advocacy Group (PPAG), referred to in this paper as “the Joint Opinion Group,” strongly affirm that children warrant access to care from clinical pharmacists trained in pediatrics. In 2005, the ACCP Pediatrics PRN released an opinion paper containing a status report and recommendations for improving the quality and quantity of pediatric pharmacy education in colleges of pharmacy, residency programs, and fellowships.31 The goal of these recommendations was to increase the numbers of students and residents pursuing a career in pediatrics as a means of meeting the patient care needs for pediatric clinical pharmacists. Since the publication of that paper, progress has been made with respect to the number of residencies in pediatric practice areas. However, there remain continuing and new challenges in pediatric pharmacy education, practice, and research. The purpose of this Joint Opinion paper is to outline four strategies for continuing to expand the quality and capacity of pediatric clinical pharmacists by 1) elevating the minimum expectations for pharmacists entering practice to provide pediatric care; 2) standardizing pediatric pharmacy education; 3) expanding the current number of pediatric clinical pharmacists, and (4) creating an infrastructure for development of pediatric clinical pharmacists and clinical scientists. It is hoped that this paper will provide a supportive framework for schools of pharmacy, health care systems, and policymakers considering expansion of training, practice, or research initiatives. The ultimate goal of the Joint Opinion Group is to improve access to pediatric clinical pharmacy services for all infants, children, and adolescents, as well as those with continuing genetic, metabolic, and oncologic needs.
STRATEGY 1. ELEVATE THE MINIMUM EXPECTATIONS FOR PHARMACISTS ENTERING PRACTICE TO PROVIDE PEDIATRIC CARE
Children requiring medical care deserve to have the services of a health care team made up of highly trained practitioners, including pharmacists. All pharmacists should receive a basic pediatric pharmacotherapy education in order to meet the needs of children. Knowledge of common pediatric disease states, pharmacokinetic, and pharmacodynamic differences related to growth and maturation, dosing considerations, and medication error prevention strategies is necessary for appropriate assessment and preparation of all pediatric prescriptions. Completion of a postgraduate year 1 (PGY1) program at a pediatric hospital or completion of multiple pediatric rotations, mentored by an experienced pediatric clinical pharmacist in a PGY1 program at a health care system that includes a children's hospital, should meet the requirements for the position of pediatric staff pharmacist or to serve as a student preceptor at most institutions. To be considered a pediatric clinical pharmacist and a residency preceptor, the Joint Opinion Group recommends a requirement for completion of a PGY2 pediatric residency or a PGY1 residency and a minimum of 3 to 4 years of pediatric medicine-focused clinical experience, a level of expertise similar to the published criteria to sit for the current board certification examinations.
A more uniform approach that provides intra-professional assurances and clinical credentials, however, is still needed. In 2009, ACCP released a white paper suggesting that a board certification process would be necessary in potential specialties such as pediatrics due to the unique aspects of clinical pharmacy practice in this patient population.32 The Board of Pharmacy Specialties (BPS) has recently completed a role delineation study which supports the development of a mechanism for credentialing pediatric pharmacy specialist.33 If BPS certification in pediatric pharmacy is established, the Joint Opinion Group recommends that it be an essential credential for all pharmacists who provide direct pediatric patient care. In addition, all preceptors for pediatric Advanced Pharmacy Practice Experiences (APPEs), PGY1, and PGY2 pediatric rotations and pediatric college faculty should become board certified in pediatric pharmacy. The Joint Opinion Group gratefully acknowledges the ongoing work of the professional organizations working with BPS to foster support for the certification and credentialing of pediatric clinical pharmacists.
STRATEGY 2. STANDARDIZE PEDIATRIC PHARMACY EDUCATION
Recommended Standards for Doctor of Pharmacy Curricula
Basic concepts in pediatric patient care should be part of the standard Doctor of Pharmacy (PharmD) curriculum.31 Currently, both the quantity and quality of the pediatric elements within PharmD curricula are not well defined. The Accreditation Council for Pharmacy Education (ACPE) Accreditation Standards and Guidelines state that education about “special populations,” such as pediatrics, must be included, addressing pathophysiologic and pharmacotherapy alterations, dosage calculation and adjustments, and drug monitoring for positive or negative outcomes.34 However, these standards fail to address pediatrics specifically and do not describe or delineate the extent and scope to which pediatrics should be included in curricula. Thus, a clear need for additional guidance on the incorporation of pediatric topics and standardization among schools exists.
The Joint Opinion Group strongly recommends more integration of pediatric pharmacotherapy into PharmD curricula and believes that proficiency in pediatric pharmacotherapy is vital for all pharmacists providing care for children. This goal may be achieved by collaborating with adult-based faculty to incorporate the unique aspects of pediatric pharmacotherapy, as a part of curricula. An elective course in pediatric pharmacotherapy should be available to all interested student pharmacists to provide in-depth knowledge of treatment for a variety of common pediatric disease states such as hematologic/oncologic, genetic, and metabolic conditions. Published descriptions of pediatric pharmacy elective courses are available to guide schools in course development, including a recent paper which documented statistically significant increases on examination scores in students enrolled in the elective course compared to their peers who received only the pediatric content provided in the required curricula.35–38 Where university resources are limited, collaboration and sharing of knowledge between and among schools of pharmacy, schools of medicine, or nursing and pediatric clinical pharmacists in clinical practice is highly encouraged. The Joint Opinion Group recommends that school administration and faculties work with health care systems to create shared or distance learning opportunities that address pediatric pharmacy-related content and experiences when these facilities do not exist on campus.
Core pediatric disease topics should be reinforced during experiential education. All schools of pharmacy should offer the opportunity for Introductory Pharmacy Practice Experiences (IPPEs) and APPEs in pediatric patient care settings. Schools without pediatric pharmacy faculty or without enough pediatric practice sites to meet the needs of their students should collaborate with pediatric clinical pharmacists practicing at other local hospitals or work with other schools to offer these experiences to students. To promote the development of future pediatric practitioners, schools should develop a mechanism, perhaps through an expansion of affiliation agreements, to match students interested in pediatrics to pediatric-specific APPEs, thereby ensuring the opportunity for these students to explore pediatric clinical practice and gain valuable experience prior to applying for a residency. All students interested in pediatric clinical pharmacy practice should also have the opportunity to have a pediatric pharmacy faculty member as an advisor or mentor. The Joint Opinion Group recommends the development of a pediatric mentor program to match pregraduates with faculty or affiliate faculty with training and/or significant practice experience in providing direct care to children. If the number of students interested in having a mentor in pediatrics exceeds the capacity of the available faculty, the school may wish to explore collaborative mentoring with a faculty member well matched to the student in other aspects, who can aid the student in forming a relationship with a pediatric pharmacist in clinical practice. Last, the ACCP Pediatrics PRN and PPAG should partner to develop a database of their members who would be willing to mentor a student.
Recommended Standards for Faculty Who Teach Pediatric Pharmacy
Experts who are actively involved in the care of children should provide pediatric education at all levels. Pediatric clinical pharmacists are responsible for the future growth of pediatric pharmacy and must be willing and available to provide education in a variety of didactic and experiential settings. The Joint Opinion Group recommends that every school of pharmacy employ or contract with at least one full-time pediatric medicine-trained faculty member. This individual should have completed PGY2 residency training and/ or pediatric pharmacy fellowship training or a PGY1 residency with 3 to 4 years of pediatric clinical practice experience. This faculty member should not only be involved in clinical practice but also be a contributor to pediatric scholarship. In order to meet the needs of their students, most schools will also need to engage qualified affiliate or adjunct faculty members with expertise in pediatric pharmacotherapy for didactic and experiential teaching. Affiliate or adjunct faculty should have attained a similar level of training and experience as the full-time faculty member. The Joint Opinion Group recommends that pediatric faculty strive to collaborate and increase their availability or exposure through innovative means such as cofunded faculty, webcasts, podcasts, broadcasted lectures or simulations which potentially could be made available to a broader audience.
Recommended Standards for Residency Training Programs
As stated by Murphy et al,37 PGY1 residency training provides opportunity for pharmacy graduates to “enhance and broaden their competencies.” All PGY1 residencies, regardless of setting, should offer a pediatric rotation. It is important to provide fundamental pediatric education to PGY1 residents, as many will provide care for children in ambulatory or acute care settings such as family medicine clinics, emergency departments, and community hospitals. A PGY1 pediatric rotation can provide opportunities for residents to explore and expand their pediatric experiences. Furthermore, it would provide residents the foundation to develop the necessary entry level pediatric knowledge and background to practice for a wide variety of ages; including infants, children, and adolescents. If the institution itself does not provide pediatric patient care, the residency program director should collaborate with pediatric clinical pharmacists at other local institutions to provide one or more rotation sites. Preceptors for resident rotations in pediatric patient care settings should meet the qualifications outlined above for preceptors of students, as well as those recommended by the American Society of Health-System Pharmacists (ASHP).40
PGY2 residency training in pediatric pharmacy should focus on specialized practice to prepare graduates to assume pediatric clinical pharmacist practice positions and/or academic appointments. These programs should meet the standards set forth in the ASHP Educational Outcomes, Goals, and Objectives for PGY2 Pharmacy Residencies in Pediatrics, developed in collaboration with PPAG.41 At this level of training, residents should build on their PGY1 foundation and become well versed in pediatric patient care as described in the ASHP standards. They should be exposed to an array of pediatric patient care experiences and other pediatric care providers and specialists with the goal of having an expanded knowledge base of medication use in a variety of clinical settings.
STRATEGY 3. EXPAND THE CURRENT NUMBER OF PEDIATRIC CLINICAL PHARMACISTS
Specific estimates of the number of pediatric clinical pharmacists needed in direct patient care are not available in current pharmacy workforce projections. Members of the Joint Opinion Group recommend that a national study of pediatric pharmacy practice be undertaken to establish projected needs for the pharmacy labor force. An estimate of the workforce could be based on several factors including pediatric health care use, number of practicing pediatricians, and types of environments where pediatric pharmacy expertise is needed, such as the care of complex patients treated in institutional settings. According to the American Medical Association, 13% of all physicians in the United States are pediatric health care providers.42 There are approximately 200 accredited pediatric medical residencies and over 8000 residents in 3-year training programs for pediatric practice, not including fellowships for subspecialties.43 Data from the Bureau of Labor Statistics show that there are approximately one-third as many pharmacists as physicians; in 2011, there were 272,320 pharmacists in the United States, compared to 602,830 physicians.44 In contrast to the percentage of pediatricians among physicians, the percentage of pharmacists practicing in pediatrics is currently much smaller. According to the Children's Hospital Association (CHA), there are approximately 2000 pediatric clinical pharmacists and 1700 pharmacy technicians for 17,500 dedicated pediatric beds in 101 of their members that responded to a recent survey.45 Coupled with ASHP National Survey data that indicate only 42% of pediatric hospital directors may have adequate numbers of trained pediatric pharmacists to address the direct care needs, the profession's capacity to provide adequate professional staffing for children's hospitals is clearly inadequate.46
In addition to CHA statistics, there are more than 175 children's hospitals and more than 35,000 dedicated inpatient pediatric beds in the United States, including both free-standing institutions and those associated with a larger health care system.43 Despite the growing number of pediatric health care facilities and beds devoted to neonatal and pediatric critical care, the 2012 ASHP Residency Directory lists only 28 PGY1 pharmacy practice residencies in children's hospitals and 35 PGY2 pediatric pharmacy residency programs or a total of 63 programs.47 These programs provide a total of 69 PGY1 and 43 PGY2 resident positions, respectively. Only eight children's hospitals offer both PGY1 and PGY2 residency training programs. While this represents an increase from the 22 pediatric residency programs cited in the 2005 PRN paper,31 it is inadequate to meet even current needs. As the next step toward increasing collective capacity, the Joint Opinion Group recommends that all children's hospitals that offer PGY1 training develop PGY2 residency programs. In addition, all institutions with PGY2 pediatric programs make an effort to increase the number of positions they offer. The group also recommends that future pharmacy labor projections include an assessment of human resource requirements for pharmacy practice specialties, including pediatrics.
STRATEGY 4. CREATE AN INFRASTRUCTURE FOR DEVELOPMENT OF PEDIATRIC CLINICAL PHARMACISTS AND CLINICAL SCIENTISTS
In addition to addressing the need for more clinical pharmacist involvement in education and patient care, the Joint Opinion Group supports the growing role of pharmacists in pediatric clinical research. Despite financial incentives provided through the Pediatric Research Equity Act and the Best Pharmaceuticals for Children Act to stimulate research, there are still significant gaps in the availability of clinical studies demonstrating the safety and efficacy of many medications routinely used in children.48 Pediatric clinical pharmacists, pediatric clinical pharmacologists, and clinical scientists play a vital role in alleviating these gaps. A greater emphasis must be placed on pediatric fellowship training and increased research activities in other related pediatric pharmacy training programs to prepare sufficient numbers of individuals who can contribute to pediatric research and maximize their impact on knowledge generated through such research. In addition, pediatric clinical pharmacists and clinical scientists need to be more fully integrated into the national infrastructure for pediatric research. Protected research time and internal startup funding may be necessary to enable this to occur. The Joint Opinion Group recommends the expansion of participation in national and international practice-based research networks (PBRNs) and collaborative trials to facilitate interprofessional and translational research, as well as increased involvement on institutional review boards and national advisory committees.
Pediatric fellowship training devoted to pediatric clinical pharmacy or pharmacology research has even larger workforce challenges. The current ACCP Directory of Residencies, Fellowships and Graduate Programs lists only three pediatric fellowships. The American Board of Clinical Pharmacology website includes four clinical pharmacology fellowship programs located in pediatric institutions. These clinical pharmacology fellowship programs are typically open to medical residents and pharmacists who desire intense clinical pharmacology training and research experience. The actual number of pediatric clinical pharmacy and clinical pharmacology fellowships is unknown because of the paucity of advertising and information available on these programs. The advancement of pediatric research and science requires more high quality fellowship-trained pediatric pharmacists. The Joint Opinion Group recommends that all children's hospitals with active pediatric research programs and fellowship-trained pediatric clinical pharmacists develop or expand the number of pediatric fellowships, which they offer. The group also recommends the creation of a web repository for collecting, storing, and accessing clinical pharmacy and pharmacology fellowship-related programmatic information. Lastly, pharmacy trainees interested in research careers should be encouraged to consider alternative pathways for training, such as Doctor of Philosophy (PhD) clinical scientist programs. For current faculty and practitioners who wish to expand or optimize their research skills, programs such as the ACCP Focused Investigator Training or Research Academy are available.
Essential Pediatric Research Curriculum in PharmD and Postgraduate Programs
In 2010, the ACCP Task Force on Research in the Professional Curriculum made recommendations for an essential research curriculum to be included in the professional program leading to the PharmD degree.49 There are many ways in which schools of pharmacy can foster specific interest in pediatric research, most importantly by incorporating coursework related to developmental pharmacology (pediatric pharmacokinetics, pharmacogenomics, and pharmacodynamics) in the core therapeutics curriculum and by increasing exposure to and availability of PhD programs. With this knowledge, the pediatric clinical pharmacist will be able to identify gaps in our current knowledge and develop capabilities for future research. It is recommended that the essentials of pediatric research be taught by pediatric and/or research subject matter experts when possible. These concepts may be addressed or reinforced in a separate course or a module of core topics such as research methods or literature evaluation. In addition, all PharmD programs should strive to incorporate a requirement for completion of a research project, to be used as the basis to teach translational research. The opportunity for conducting pediatric research should be made available to all students considering a career in this area.50–55
Both PGY1 and PGY2 residency training programs are required to provide trainees with research experiences. As with PharmD programs, all interested pharmacy residents should have the opportunity to participate in pediatric clinical research. While core research knowledge gained from PharmD and residency experiences is essential for pediatric pharmacy practice in order to accurately perform and interpret clinical research, preparation of the research-focused pediatric clinical pharmacist, pharmacologist or PhD exceeds this level of training.49,51–54
With an emphasis on scholarship, pediatric fellowship training programs should provide advanced learning experiences in study conceptualization, design, implementation, analysis, and dissemination of results. Scholastic activities should focus on pathophysiology and therapeutics for infants, children, and adolescents, with special training regarding research issues specific to this population such as ethical concerns related to a vulnerable population, strategies for obtaining data with noninvasive or minimally invasive sampling, and methods for assessing adverse events. Coursework or workshops in grant writing, research methodology, and biostatistics should be offered as part of preparation for a pediatric research career. Development of teaching skills should also be part of the fellowship training program, including lecture preparation, examination of different learning styles, composition of exam questions, and course development. Continued clinical practice through service as a consultant or in the clinic is also recommended to maintain clinical skills and to establish a link between clinical practice and the development of new research questions.
As previously stated, several fellowship programs are currently available for pediatric clinical pharmacists wishing to pursue a research career, but the number of available programs needs to be expanded and peer-reviewed. The Joint Opinion Group recommends that all pediatric fellowship training programs voluntarily undergo a multidisciplinary peer review process, such as that offered by ACCP or the American College of Clinical Pharmacology. This review would help to ensure the quality of new and existing training programs.55 An increase in the number of fellowship-trained pediatric clinical pharmacists and clinical scientists will elevate the visibility of pediatric pharmacy, increase the number of pharmacy-trained clinical investigators, and provide more opportunities for interdisciplinary synergy to stimulate the flow of innovative ideas and drug information for the advancement of pediatric health care.
CONCLUSIONS
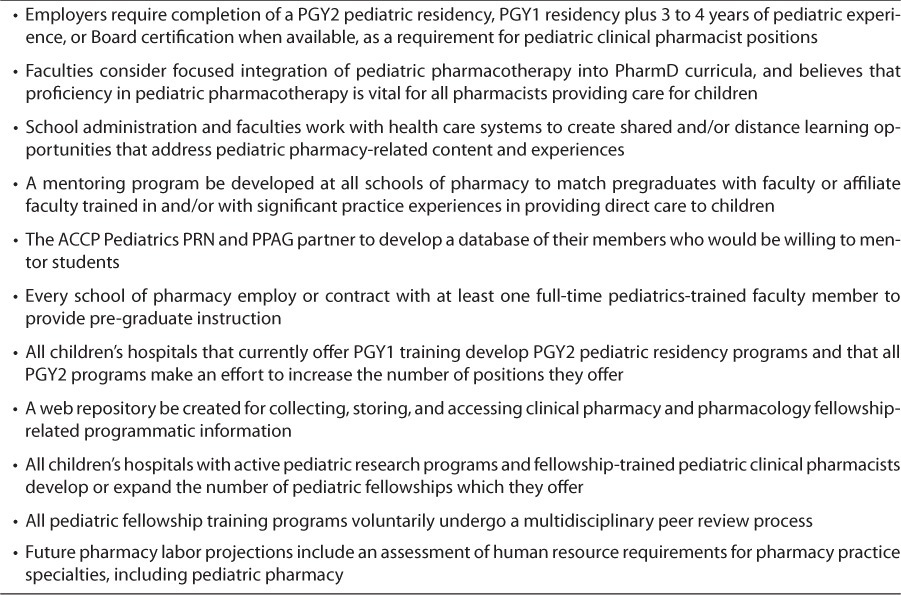
The Joint Opinion Group believes that a strategic approach is needed to increase the workforce and collective capacities of our profession for providing pediatric clinical pharmacy services. The recommendations outlined in this opinion paper (Table) are provided to encourage focused collaboration among schools of pharmacy, health care facilities, and professional organizations to enrich the quality of health care and improve access to pediatric clinical pharmacist care for all children.
Table.
Summary of The Joint Opinion Group Recommendations for Meeting the Pediatric Patient's Need for a Clinical Pharmacist
ACKNOWLEDGMENTS
We wish to acknowledge the contributions of Kelly Bobo, Gretchen Brummel, Sandra Benivedes Caballero, Audrey Kennedy, David Knoppert, Bernard Lee, Sherry Luedtke, Kalen Manesco, Tracy Sandritter, Holly Watson, and Mary Worthington.
ABBREVIATIONS
- ACCP
American College of Clinical Pharmacy
- ACPE
Accreditation Council for Pharmacy Education
- APPE
Advanced Pharmacy Practice Experience
- ASHP
American Society of Health-System Pharmacists
- BPS
Board of Pharmacy Specialties
- IPPE
Introductory Pharmacy Practice Experience
- PBRN
practice-based research networks
- PGY1
postgraduate year 1
- PharmD
Doctor of Pharmacy
- PhD
Doctor of Philosophy
- PPAG
Pediatric Pharmacy Advocacy Group
- PRN
Practice and Research Network
Footnotes
DISCLOSURE The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
This paper represents the opinions of the Pediatrics Practice and Research Network of the American College of Clinical Pharmacy (ACCP) and the Pediatric Pharmacy Advocacy Group (PPAG). It does not necessarily represent an official ACCP or PPAG commentary, guideline, or statement of policy or position.
REFERENCES
- 1.Kliegman RM, Stanton B, St Geme J Nelson Textbook of Pediatrics. 19th ed. Philadelphia: WB Saunders; 2011. [Google Scholar]
- 2.Rudolph C, Rudolph A, Lister G Rudolph's Pediatrics. 22nd ed. New York: McGraw-Hill; 2011. [Google Scholar]
- 3.Avery ME, Lewis R. Pediatric Medicine. 2nd ed. Baltimore: Williams & Wilkins; 1994. [Google Scholar]
- 4.US Census Bureau. Population estimates: national characteristics, vintage 2011. http://www.census.gov/popest/data/national/asrh/2011/index.html. Accessed September 24, 2012.
- 5.Statistics Canada. http://www.statcan.gc.ca/start-debut-eng.html. Accessed: June 10, 2012.
- 6.Child and Adolescent Health Measurement Initiative. Data resource center for child and adolescent health, 2012. http://www.childhealthdata.org. Accessed February 20, 2012.
- 7.Cox ER, Halloran DR, Homan SM, Welliver S, Mager DE. Trends in the prevalence of chronic medication use in children: 2002–2005. Pediatrics. 2008;122(5):e1053–e1061. doi: 10.1542/peds.2008-0214. [DOI] [PubMed] [Google Scholar]
- 8.Daniels SR, Greer FR. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122(1):198–208. doi: 10.1542/peds.2008-1349. Committee on Nutrition. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. National health interview survey, 2010. http://www.cdc.gov/nchs/nhis.htm. Accessed February 24, 2012.
- 10.Feudtner C, Dai D, Hexem KR, Luan X, Metjian TA. Prevalence of polypharmacy exposure among hospitalized children in the United States. Arch Pediatr Adolesc Med. 2012;166(1):9–16. doi: 10.1001/archpediatrics.2011.161. [DOI] [PubMed] [Google Scholar]
- 11.Institute for Safe Medication Practices. ISMP's list of high-alert medications. 2011. http://ismp.org/Tools/highalertmedications.pdf. Accessed February 20, 2012.
- 12.Haase M, Luedtke S. Assessment of pediatric services in community pharmacies. J Pediatr Pharmacol Ther. 2001;6(3):218–224. [Google Scholar]
- 13.Klotz R. Is the pediatric pharmacist needed? Hosp Pharm. 1971;6(7):18–20. [Google Scholar]
- 14.Levin RH. Clinical pharmacy practice in a pediatric clinic. Drug Intell Clin Pharm. 1972;40(6):171–176. [Google Scholar]
- 15.Cupit GC. An approach to pediatric pharmacy practice. Hosp Pharm. 1974;9(10):399–400. 402. [Google Scholar]
- 16.Folli HL, Poole RL, Benitz WE, Russo JC. Medication error prevention by clinical pharmacists in two children's hospitals. Pediatrics. 1987;79(5):718–722. [PubMed] [Google Scholar]
- 17.Buck ML, Conner JJ, Snipes CJ, Hopper JE. Comprehensive pharmaceutical services for pediatric patients. Am J Hosp Pharm. 1993;50(1):78–84. [PubMed] [Google Scholar]
- 18.Hahn K, Marlowe K, Chicella M. Survey of pharmaceutical services in pediatric resuscitation. Am J Health Syst Pharm. 2001;58(17):1626–1628. doi: 10.1093/ajhp/58.17.1626. [DOI] [PubMed] [Google Scholar]
- 19.Krupicka MI, Bratton SL, Sonnenthal K, Goldstein B. Impact of a pediatric clinical pharmacist in the pediatric intensive care unit. Crit Care Med. 2002;30(4):919–921. doi: 10.1097/00003246-200204000-00035. [DOI] [PubMed] [Google Scholar]
- 20.Condren ME, Haase MR, Luedtke SA, Gaylor AS. Clinical activities of an academic pediatric pharmacy team. Ann Pharmacother. 2004;38(4):574–578. doi: 10.1345/aph.1D384. [DOI] [PubMed] [Google Scholar]
- 21.Wang JK, Herzog NS, Kaushal R, Park C, Mochizuki C, Weingarten SR. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007;119(1):e77–e85. doi: 10.1542/peds.2006-0034. [DOI] [PubMed] [Google Scholar]
- 22.Gardner B, Graner K. Pharmacists' medication reconciliation-related clinical interventions in a children's hospital. Jt Comm J Qual Patient Saf. 2009;35(5):278–282. doi: 10.1016/s1553-7250(09)35039-4. [DOI] [PubMed] [Google Scholar]
- 23.Scott SA, Smith RS, Mason HL. Pharmaceutical services in hospitals treating pediatric patients. Am J Hosp Pharm. 1985;42(10):2190–2196. [PubMed] [Google Scholar]
- 24.Moffett BS, Mott AR, Newlson DP, Gurwitch KD. Medication dosing and renal insufficiency in a pediatric cardiac intensive care unit: impact of pharmacist consultation. Pediatr Cardiol. 2008;29(4):744–748. doi: 10.1007/s00246-007-9170-3. [DOI] [PubMed] [Google Scholar]
- 25.So TY, Layton JB, Bozik K et al. Cognitive pharmacy services at a pediatric nephrology and hypertension clinic. Ren Fail. 2011;33(1):19–25. doi: 10.3109/0886022X.2010.536291. [DOI] [PubMed] [Google Scholar]
- 26.Tuffana HW, Abdelhadi O, Omar SA. Clinical pharmacy services in the outpatient pediatric oncology clinics at a comprehensive cancer center. Int J Clin Pharm. 2012;34(1):27–31. doi: 10.1007/s11096-011-9600-4. [DOI] [PubMed] [Google Scholar]
- 27.Stark AR. Levels of neonatal care. Pediatrics. 2004;114(5):1341–1347. doi: 10.1542/peds.2004-1697. American Academy of Pediatrics Committee on Fetus and Newborn. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg DI, Moss MM, American Academy of Pediatrics Guidelines and levels of care for pediatric intensive care units. Pediatrics. 2004;114(4):1114–1125. doi: 10.1542/peds.2004-1599. [DOI] [PubMed] [Google Scholar]
- 29.Corrigan JJ, Feig SA. Guidelines for pediatric cancer centers. Pediatrics. 2004;113(6):1833–1835. doi: 10.1542/peds.113.6.1833. American Academy of Pediatrics. [DOI] [PubMed] [Google Scholar]
- 30.The Joint Commission. Sentinel Event Alert: Preventing pediatric medication errors. Issue 39, April 11, 2008. http://www.joint-commission.org/assets/1/18/SEA_39.PDF. Accessed February 20, 2012. [PubMed]
- 31.Aucoin RG, Buck ML, Dupuis LL et al. Pediatric pharmacotherapeutic education: current status and recommendations to fill the growing need. Pharmacotherapy. 2005;25(9):1277–1282. doi: 10.1592/phco.2005.25.9.1277. [DOI] [PubMed] [Google Scholar]
- 32.Blair MM, Freitag RT, Keller DL et al. Proposed revision to the existing specialty and specialist certification framework for pharmacy practitioners. Pharmacotherapy. 2009;29(4):3e–13e. doi: 10.1592/phco.29.4.489. [DOI] [PubMed] [Google Scholar]
- 33.Board of Pharmacy Specialties. BPS Issues call for petitions in critical care pharmacy and pediatric pharmacy. May 24, 2012. http://www.bpsweb.org/news/pr_052412.cfm/. Accessed June 24, 2012.
- 34.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed February 20, 2012.
- 35.Slain D, Wong-Berringer A, Blake B Pharmacotherapy Didactic Curriculum Toolkit 2009. American College of Clinical Pharmacy Educational Affairs Committee B. http://www.accp.com. Accessed March 19, 2012.
- 36.Scott CS, Deloatch KH. Advanced pediatric pharmacotherapy: an elective course with service learning. Am J Pharm Educ. 1998;62(4):420–426. [Google Scholar]
- 37.LaRochelle JM, Diaz CJ. Evaluation of pediatric pharmacotherapy education in a college of pharmacy. Curr Pharm Teaching Learning. 2011;3:313–319. [Google Scholar]
- 38.Elliot JP, Koerner PH, Heasley J, Kamal K. The impact of elective active-learning courses in pregnancy/lactation and pediatric pharmacotherapy. Am J Pharm Educ. 2012;76(2) doi: 10.5688/ajpe76226. article 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murphy JE, Nappi JM, Bosso JA et al. American College of Clinical Pharmacy's vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;26:722–733. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]
- 40.American Society of Health-System Pharmacists. Accreditation standard for postgraduate year one (PGY1) pharmacy residency programs. September 23, 2005. http://www.ashp.org/DocLibrary/Accreditation/ASD-PGY1-Standard.aspx. Accessed February 20, 2012.
- 41.American Society of Health-System Pharmacists. Educational outcomes, goals, and objectives for postgraduate year two (PGY2) pharmacy residencies in pediatrics. Prepared in collaboration with the Pediatric Pharmacy Advocacy Group, March 2008. http://www.ashp.org/DocLibrary/Accreditation/Regulations-Standards/RTPObjPediatricMarch2008.aspx. Accessed November 2, 2012.
- 42.Smart DR. Physician Characteristics and Distribution in the US. 2010 ed. Chicago, IL: American Medical Association; 2010. [Google Scholar]
- 43.National Resident Matching Program. Results and data: 2011 main residency match, April 2011. http://www.nrmp.org/data/resultsanddata2011.pdf. Accessed February 20, 2012.
- 44.US Department of Labor, Bureau of Labor Statistics. Occupational employment and wages, May 2011. 29-0000 Healthcare practitioners and technical occupations (major group). http://www.bls.gov/oes/current/oes290000.htm. Accessed November 2, 2012.
- 45.Children's Hospital Association. Annual Survey on Utilization and Financial Indicators of Children's Hospitals. 2011. (personal communication, Amy Keegan, September 17, 2012)
- 46.Pedersen CA, Schneider PJ, Sheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: monitoring and patient education–2009. Am J Health Syst Pharm. 2010;67(7):542–558. doi: 10.2146/ajhp090596. [DOI] [PubMed] [Google Scholar]
- 47.American Society of Health-system Pharmacists. Residency directory. http://www.ashp.org/menu/Accreditation/Residency-Directory.aspx. Accessed February 20, 2012.
- 48.National Institutes of Health, National Institutes for Child Health and Human Development. Best Pharmaceuticals for Children Act: Title V–Best Pharmaceuticals for Children Act Amendments of 2007. http://bpca.nichd.nih.gov/. Accessed February 20, 2012.
- 49.American College of Clinical Pharmacy. Lee MW, Clay PG, Kennedy WK et al. The essential research curriculum for doctor of pharmacy programs. Pharmacotherapy. 2010;30(9):344e–349e. doi: 10.1592/phco.30.9.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dowling TC, Murphy JE, Kalus JS et al. Recommended education for pharmacists as competitive clinical scientists. Pharmacotherapy. 2009;29(2):236–244. doi: 10.1592/phco.29.2.236. [DOI] [PubMed] [Google Scholar]
- 51.Campbell WH, Anderson WK, Burckart GJ et al. Institutional and faculty roles and responsibilities in the emerging environment of university-wide interdisciplinary research structures: report of the 2001–2002 research and graduate affairs committee. Am J Pharm Educ. 2002;66(4):28S–33S. [Google Scholar]
- 52.Leslie SW, Corcoran GB, MacKichan JJ et al. Pharmacy scholarship reconsidered: the report of the 2003–2004 research and graduate affairs committee. Am J Pharm Educ. 2004;68(3):S6. [Google Scholar]
- 53.American College of Clinical Pharmacy. The research agenda of the American College of Clinical Pharmacy. Pharmacotherapy. 2007;27(2):312–324. doi: 10.1592/phco.27.2.312. [DOI] [PubMed] [Google Scholar]
- 54.Kao DJ, Hudmon KS, Corelli RL. Evaluation of a required senior research project in a Doctor of Pharmacy curriculum. Am J Pharm Educ. 2011;75(1):5. doi: 10.5688/ajpe7515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.American College of Clinical Pharmacy. ACCP guidelines for clinical research fellowship training programs, October 2004. http://www.accp.com/docs/positions/guidelines/pos15.pdf. Accessed February 20, 2012.


