Abstract
Background
To describe the causes of graft loss, patient death and survival figures in kidney transplant patients in Spain based on the recipient's age.
Methods
The results at 5 years of post-transplant cardiovascular disease (CVD) patients, taken from a database on CVD, were prospectively analysed, i.e. a total of 2600 transplanted patients during 2000–2002 in 14 Spanish renal transplant units, most of them receiving their organ from cadaver donors. Patients were grouped according to the recipient's age: Group A: <40 years, Group B: 40–60 years and Group C: >60 years. The most frequent immunosuppressive regimen included tacrolimus, mycophenolate mofetil and steroids.
Results
Patients were distributed as follows: 25.85% in Group A (>40 years), 50.9% in Group B (40–60 years) and 23.19% in Group C (>60). The 5-year survival for the different age groups was 97.4, 90.8 and 77.7%, respectively. Death-censored graft survival was 88, 84.2 and 79.1%, respectively, and non death-censored graft survival was 82.1, 80.3 and 64.7%, respectively. Across all age groups, CVD and infections were the most frequent cause of death. The main causes of graft loss were chronic allograft dysfunction in patients <40 years old and death with functioning graft in the two remaining groups. In the multivariate analysis for graft survival, only elevated creatinine levels and proteinuria >1 g at 6 months post-transplantation were statistically significant in the three age groups. The patient survival multivariate analysis did not achieve a statistically significant common factor in the three age groups.
Conclusions
Five-year results show an excellent recipient survival and graft survival, especially in the youngest age group. Death with functioning graft is the leading cause of graft loss in patients >40 years. Early improvement of renal function and proteinuria together with strict control of cardiovascular risk factors are mandatory.
Keywords: cardiovascular mortality, graft survival, patient survival, renal function, renal transplantation
Introduction
During the last two decades, the introduction of new immunosuppressants has been associated with a decline in the prevalence of acute rejection and with an improvement in 1-year graft survival [1–3]. However, in contrast to the short-term survival, the long-term outcome of both transplant recipients and their grafts has not improved as expected [4].
Therefore, the optimization of long-term outcome has become increasingly important. The demographic modification of the donor and the recipient may help to explain the lack of improvement. Recipient characteristics at the time of transplantation have evolved in a time-dependent manner and nowadays recipient age is on the increase. This increase in recipient age may have an important impact on graft loss, patient survival and patient death as well as the possible risk factors involved in survival such as cardiovascular risk factors, which are the main cause of graft loss in the long term [1, 5]. Accurately determining the possible causes involved in survival is essential for effective long-term management of the patient.
Thus, the aim of this study was to assess the graft and patient 5-year survival according to recipient age and determine the possible causes involved.
Materials and methods
Population
All transplanted patients during 2000–2002 across 14 renal transplant units in Spain were included in a database (Renal Forum Database) focused on cardiovascular risk factors [6]. No exclusion criteria were considered; so, this database represents the full record of these hospitals in the first 3 years of the 21st century and also includes patients who are participating in clinical trials. Three age groups were established according to recipient age: <40, 40–60 and >60 years old.
Database and clinical variables
The cardiovascular disease (CVD) database was initiated in 2000. All participating units register data concerning all the renal transplants performed in each centre. Data collection is carried out every 12 months, via a database provided for that purpose, in every centre. These data are transferred annually to an independent biometry unit that merges and analyse the results from the suggestions made by a working group created within the ‘Renal Forum’ framework. The ‘Renal Forum’ group and the ‘Renal Forum database’ are supported by an unrestricted grant from Astellas.
The Renal Forum database includes donor and particularly recipient characteristics: age, original disease, time on dialysis, serology, immunological data and pre-transplant cardiovascular condition. In this way, body mass index (BMI), arterial hypertension, hyperlipidaemia, diabetes, smoking and pre-transplant CVD were specifically recorded. Immunosuppressive treatment at the point of transplantation was also recorded.
After surgery, the frequency and number of acute rejections, incidence of acute tubular necrosis (ATN), graft survival and causes of graft loss and patient survival as well as of mortality, renal function and proteinuria were recorded. Cardiovascular events were also recorded, as well as modifications of immunosuppression and the presence of concomitant medications such as statins and angiotensin converting enzyme inhibitors/angiotensin receptor blockers (ACEIs/ARBs). These data were annually collected.
Ethics
This study (no intervention) was approved by all the departments of Nephrology of the 14 hospitals assuring data confidentiality.
A blinded code was assigned to each participating hospital to take into consideration the centre effect.
Statistical methods
The objective was to analyse the 5-year follow-up data of patients after kidney transplantation, specifically:
Descriptive analysis of the variables of interest in the 5 years: absolute and relative frequencies of the qualitative variables, and measures of association and dispersion (average, medium standard deviation, minimum, and maximum) of the quantitative ones.
Study of the graft and patient survival: number of losses and exitus, causes of graft loss and patient death, curves of Kaplan–Meier.
Measuring whether there was a statistically significant relationship between patient characteristics and groups defined for the 48-month study. Using the corresponding tests for independent data: in the case of quantitative variables, t-test (if there is normality) or the Mann–Whitney (when we did not prune to assume normality in the data). In the case of qualitative variables, χ2 test.
Multivariate analysis that allows the identification of risk factors related to graft loss and patient death. The Cox regression model to calculate the rate of graft loss and death as a function of time (until you see the event of interest) and forecast variables.
Results
During 2000–2002, 2822 renal transplantations were performed across 14 hospitals in Spain. We excluded from this analysis 222 double transplants: liver–kidney, pancreas–kidney and heart–kidney. Therefore, 2600 renal transplants, including double-kidney transplantation in a single recipient (2.5%), were the subject of this study.
Donor, surgery and recipient characteristics are shown in Table 1. The mean recipient age was 49.7 ± 13.7 and 12.5% were hyperimmunized. The main cause of chronic renal failure (CRF) in patients <60 years was chronic glomerulonephritis and the main cause of CRF in patients >60 years was adult polycystic kidney disease. HLA-DR mismatching was 0.9 ± 0.6 and HLA-A and -B, 2.6 ± 1.
Table 1.
Recipient and donor baseline characteristics
| Recipient baseline characteristics | Total | <40 | 40–60 | >60 | P-value |
|---|---|---|---|---|---|
| Age at transplantation | — | 25.85% | 50.96% | 23.19% | |
| Sex (male) | 60% | ||||
| Cause of chronic renal failure | |||||
| Chronic glomerulonephritis | 26.2% | 34.9% | 26.5% | 15.8% | 0.001 |
| Adult polycystic kidney disease | 15.3% | 4.2% | 20.4% | 16.5% | |
| Interstitial nephropathy | 13.4% | 19.6% | 10.5% | 12.8% | |
| Nephroangiosclerosis | 6.9% | 2.5% | 6.4% | 12.6% | |
| Diabetes | 6.6% | 3.1% | 7.1% | 9.3% | |
| Unknown origin | 19.8% | 16.4% | 19.5% | 24.1% | |
| Others | 11.9% | 19.3% | 9.6% | 8.8% | |
| Time on dialysis (months) | 39.3 ± 46.7 | ||||
| Type of dialysis | |||||
| Haemodialysis | 81% | ||||
| Peritoneal dialysis | 15% | ||||
| Both | 2.7% | ||||
| Predialysis | 0.9% | ||||
| Hyperimmunized patients | |||||
| *PRA historical or current ≥50% | 10.1% | 11.2% | 11.2% | 6.5% | 0.05 |
| Prior transplants | |||||
| No | 84% | 76.7% | 84.1% | 91.8% | |
| Yes | 16% | 23.3% | 15.9% | 8.2% | |
| Type of transplant | |||||
| Double | 2.4% | 0.1% | 0.8% | 8.5% | |
| Simple | 97.6% | 99.9% | 99.2% | 91.5% | |
| Incompatibilities | |||||
| HLA-DR HLA-AB | 0.9 ± 0.6/2.6 ± 1 | ||||
| HLA-DR + HLA-AB | 3.34 ± 1.1 | 3.42 ± 1.16 | 3.56 ± 1.18 | 0.01 | |
| Immunosupression | |||||
| Cyclosporine | 33.8% | 19.4% | 31.5% | 56.9% | 0.001 |
| Tacrolimus | 6.2% | 80.6% | 68.5% | 43.1% | |
| Cardiovascular status | |||||
| BMI | – | 23.11 ± 4.0 | 25.45 ± 4.2 | 26.25 ± 3.9 | 0.001 |
| Arterial hypertension | 75% | 71.9% | 76.0% | 76.2% | n.s. |
| SBP (mmHg)-6 months | 130.4 | 137.9 | 144.2 | 0.001 | |
| DBP (mmHg)-6 months | 78.9 | 80.1 | 77.8 | 0.001 | |
| ACEI/ARB-6 months | 14.8% | 16.8% | 14.6% | 12.9% | n.s. |
| ACEI/ARB-12 months | 20.7% | 19.0% | 23.0% | 17.4% | 0.05 |
| Diabetes mellitus | 9.2% | 4.0% | 9.9% | 13.3% | 0.001 |
| Type I | 3.5% | 2.8% | 4.2% | 2.7% | 0.001 |
| Type II | 5.7% | 1.2% | 5.8% | 10.6% | 0.001 |
| Dyslipidaemia | 22.6% | 0.001 | |||
| Hypercholesterolaemia | 9.3% | 5.5% | 10.0% | 12.1% | |
| Hypertrigliceridaemia | 6.1% | 6.4% | 5.8% | 6.3% | |
| Both | 7.2% | 5.1% | 8.4% | 7.0% | |
| Smoke | |||||
| Non-smoker or ex-smoker >5 years | 76.0% | 76.1% | 72.6% | 83.4% | 0.001 |
| Smoker or ex-smoker <5 years | 24% | 23.9% | 27.4% | 16.6% | |
| Alcohol | |||||
| Yes | 5.6% | 3.9% | 7.0% | 4.5% | 0.01 |
| Metabolic Syndrome | 17.8% | 8.1% | 19.9% | 24.1% | 0.001 |
| ATN | 28.6% | 24.4% | 28.6% | 33.3% | 0.01 |
| Rejection (6 months) | 14.4% | 17.4% | 13.7% | 12.6% | 0.05 |
| Rejection (12 months) | 16.6% | 19.4% | 15.9% | 14.8% | n.s. |
| Proteinuria (6 months) >1 g/day | 5.7% | 3.8% | 5.9% | 7.6% | 0.05 |
| Proteinuria (g/day) | 0.4 ± 0.68 | 0.25 ± 0.52 | 0.31 ± 0.58 | 0.40 ± 0.76 | 0.01 |
| Hepatitis C | 16.0% | 18.8% | 15.7% | 13.1% | n.s. |
| Donor characteristics | |||||
| Donor age (years) | 46.9 ± 17 | 34.2 ± 14 | 46.2 ± 15 | 60.1 ± 14 | 0.001 |
| Male | 62.7% | 65.4 | 62.5% | 60.0% | n.s. |
| Causes of death | 0.001 | ||||
| Acute cerebrovascular accident | 56.0% | 39.8% | 57.6% | 70.0% | |
| Craneoencephalic traumatism | 34.7% | 51.0% | 31.4% | 24.1% | |
| Hypoxia | 4.6% | 4.3% | 5.8% | 2.5% | |
| Others | 4.7% | 4.9% | 5.2% | 3.4% | |
| Cold ischaemia time (h) | 19 ± 6 | 17.76 ± 5.6 | 18.76 ± 5.4 | 19.18 ± 5.6 | 0.001 |
SBP, hypercholesterolaemia, diabetes Type II, BMI, ATN and proteinuria increased significantly with age. Only 9.2% of the patients who received a kidney transplant were diagnosed with diabetes mellitus: 4.0% (<40), 9.9% (40–60), 13.3% (>60); there was a low proportion of obesity and nearly 15% had CVD. Metabolic syndrome prevalence increased significantly with age, but only 17.8% were diagnosed with pre-transplant metabolic syndrome. It can be noted that the incidence of acute rejection in the first 6 and 12 months was 14.4 and 16.6%, respectively. Acute rejection in the first 6 months decreased significantly by age.
The mean donor age was 46.9 ± 17, 63% were male, and the most frequent cause of death was stroke. Cold ischaemia time increased significantly by age. In these years, renal transplantation from living donors was anecdotic (0.38%).
Initial and 5-year immunosuppresion is represented in Table 2. The most frequent combination regimen was based on tacrolimus and mycophenolate mofetil with or without monoclonal antibodies anti-interleukin 2 receptor or thymoglobuline. Interestingly, 24% received antibodies as initial therapy. Patients on tacrolimus- or cyclosporine-based immunosuppresion at baseline were 63.5 and 32.6%, respectively. The most important concomitant medications were statins, ACEIs or ARA, increasing from 23, 5.4 and 9.5% at 6 months to 46, 9.5 and 29% at 48 months, respectively.
Table 2.
Immunosupression (baseline and 60 months later)
| Drug | <40 (%) |
40–60 (%) |
>60 (%) |
|||
|---|---|---|---|---|---|---|
| Basal | 60 months | Basal | 60 months | Basal | 60 months | |
| Steroids | 97.3 | 76.8 | 97.2 | 72.5 | 97.7 | 68.4 |
| Cyclosporine | 19.4 | 13.5 | 30.5 | 22.7 | 50.7 | 41.5 |
| Tacrolimus | 80.6 | 76.6 | 69.5 | 66.7 | 39.3 | 43.9 |
| Mycophenolate mofetil | 88.4 | 77.9 | 86.0 | 76.8 | 87.9 | 68.0 |
| Others (m-TORi Azathioprine) | 9.3 | 12.7 | 9.4 | 11.9 | 11.2 | 13.2 |
| Antibody induction | 20.4 | 23.8 | 30.3 | |||
Five-year graft survival
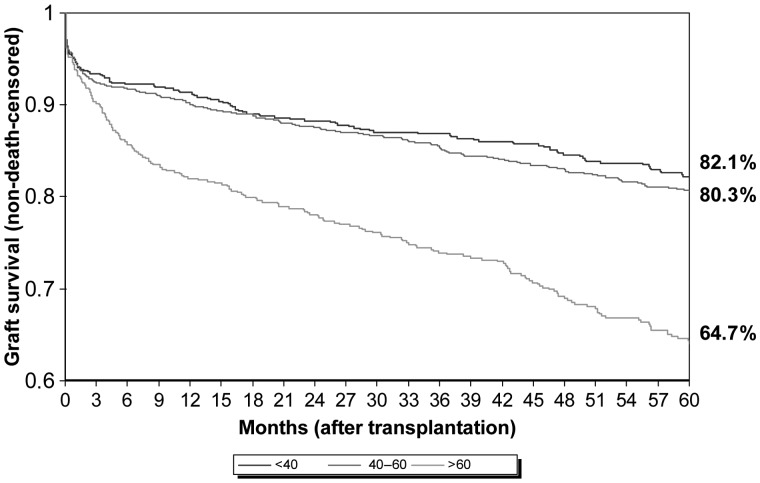
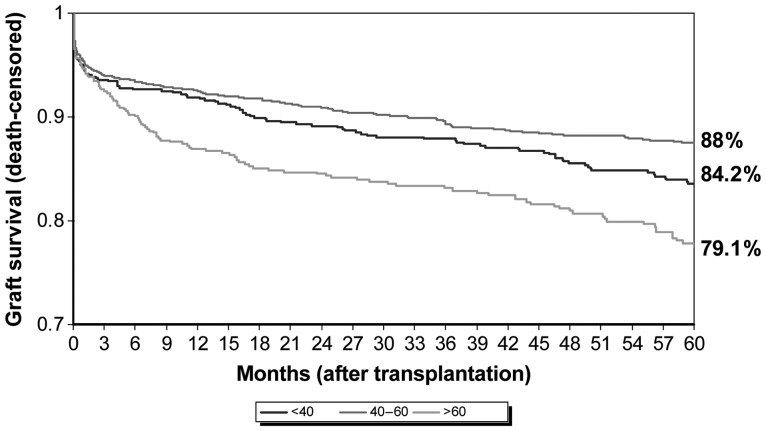
Death-censored graft survival was 88, 84.2 and 79.1%, respectively (Figure 1), and non-death-censored graft survival was 82.1, 80.3 and 64.7%, respectively (Figure 2). The main causes of graft loss were chronic allograft nephropathy in <40-year-old patients and death with functioning graft in the two remaining groups (Table 3).
Fig. 1.
Five-year graft survival by age group (non-death-censored).
Fig. 2.
Five-year graft survival by age group (death-censored).
Table 3.
Causes of graft loss by age group (5 years)
| Causes | <40 (%) | 40–60 (%) | >60 (%) | Total (%) |
|---|---|---|---|---|
| Acute rejection | 16.1 | 13.4 | 9.5 | 12.6 |
| Uropathy | 1.6 | 0.4 | 1.0 | 0.9 |
| Vascular | 0.8 | 2.1 | 2.5 | 2.0 |
| De novo GN | 1.6 | 0.0 | 0.5 | 0.5 |
| Recurrent GN | 5.6 | 1.7 | 0.5 | 2.1 |
| Exitus with a functioning graft | 7.3 | 30.5 | 37.5 | 27.9 |
| Chronic allograft nephropathy | 30.6 | 20.1 | 21.0 | 22.7 |
| Venous thrombosis | 9.7 | 8.4 | 3.5 | 6.9 |
| Arterial thrombosis | 5.6 | 4.6 | 4.0 | 4.6 |
| Arterial + venous thrombosis | 1.6 | 0.8 | 1.0 | 1.1 |
| Primary non-function | 1.6 | 4.2 | 6.0 | 4.3 |
| Recurrent disease | 3.2 | 0.4 | 1.0 | 1.2 |
| Surgery problems | 0.0 | 2.9 | 1.0 | 1.6 |
| Others | 5.6 | 3.8 | 7.5 | 5.5 |
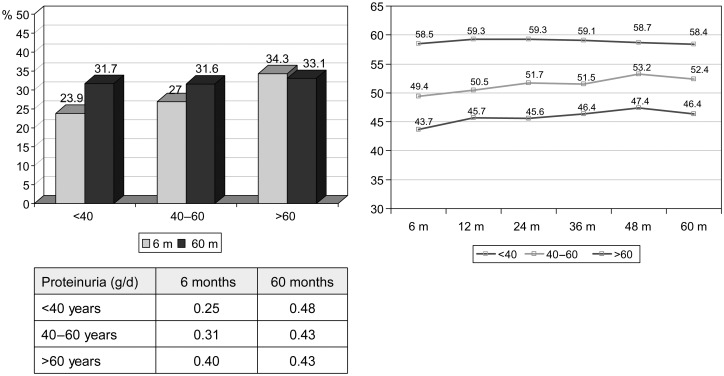
Risk factors for graft loss are shown in Table 4. Multivariate analysis showed that independent predictors for death-censored graft survival in the three age groups were elevated serum creatinine levels and proteinuria >1 g at 6 months post-transplantation. Figure 3 shows the evolution of proteinuria and glomerular filtration by age group. Diabetes was also a risk factor in those younger than 40 years, and older donors was a risk factor in recipients aged 40–60 years.
Table 4.
Risk factors for graft loss (5 years)
| Univariate analysis (P-value) | Multivariate analysis (all ages) | Multivariate analysis by age group |
|||
|---|---|---|---|---|---|
| HR (95% IC) P-value | <40 HR (95% IC) P-value | 40–60 HR (95% IC) P-value | >60 HR (95% IC) P-value | ||
| Recipient aged | ≤0.001 | — | — | — | — |
| Donor aged | ≤0.001 | — | — | 1.02 (1.0–1.05) ≤0.05 | — |
| Hyperimmunized | ≤0.05 | — | — | — | — |
| AH | ≤0.05 | — | — | — | |
| Diabetes | ≤0.001 | — | 4.85 (1.9–11.8) ≤0.001 | — | — |
| ATN | ≤0.001 | — | — | — | — |
| Acute rejection at 12 months | ≤0.001 | — | — | — | |
| Time on dialysis | ≤0.05 | — | — | — | |
| Serum creatinine: 6 months | ≤0.001 | 3.18 (1.6–6.2) ≤0.001 | 9.34 (3.5–25.0) ≤0.001 | 3.12 (1.6–7.6) ≤0.01 | 3.18 (1.6–6.2) ≤0.001 |
| Proteinuria: 6 months >1 g | ≤0.001 | 3.91 (1.8–8.4) ≤0.001 | 4.66 (2.1–10.6) ≤0.001 | 4.10 (2.1–8.2) ≤0.001 | 3.91 (1.8–8.4) ≤0.001 |
| Systolic arterial hypertension at 6 months | ≤0.001 | — | — | — | — |
| SBP at 6 months Hepatitis C | ≤0.001 | — | — | — | — |
Fig. 3.
Proteinuria at 6 and 60 months and glomerular filtration (modification of diet in renal disease) at 6, 12, 24, 36, 48 and 60 months by age group.
Five-year patient survival
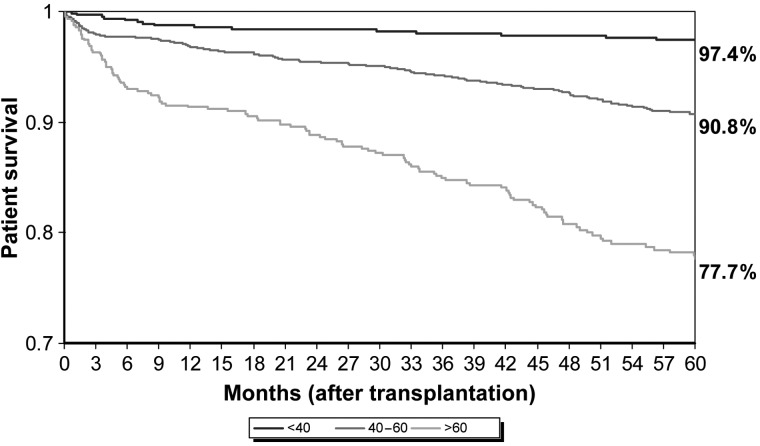
CVD (33.9%) was the most common cause of death across all age groups followed by infection (22.9%). Cardiovascular events by age group were distributed as follows: <40 (29 CV events), 40–60 (189 CV events) and >60 (136 CV events). Stroke was the main CV cause of death in recipients younger than 40 years old and ischaemic heart disease in older than 60 years. Malignancies were the third cause of death in these patients (Table 5). The 5-year recipient survival for the various age groups was 97.4, 90.8 and 77.7%, respectively (Figure 4). The patients' survival multivariate analysis did not show a statistically significant common factor in the three groups, but the use of ACEI/ARB was a significant risk factor in patients older than 60 years and diabetes reached statistical significance in the 40–60 age group (Table 6).
Table 5.
Causes of death by age group (5 years)
| Causes | <40 (%) | 40–60 (%) | >60 (%) | Total (%) |
|---|---|---|---|---|
| Infection | 25.0 | 20.8 | 24.5 | 22.9 |
| Cardiovascular disease | 33.9 | 35.6 | 31.0 | 33.9 |
| Cerebrovascular accident | 18.8 | 8.9 | 7.3 | 8.8 |
| Ischaemic heart disease | 6.3 | 7.9 | 8.2 | 7.9 |
| Other heart causes | 12.5 | 11.9 | 8.2 | 10.1 |
| Sudden death | 6.3 | 6.9 | 7.3 | 7.0 |
| Liver disease | 0.0 | 1.0 | 4.5 | 2.6 |
| Neoplasias | 12.5 | 13.9 | 11.8 | 12.8 |
| Accidental | 0.0 | 1.0 | 0.0 | 0.4 |
| Uncertain | 0.0 | 5.0 | 4.5 | 4.4 |
| Other | 12.5 | 16.8 | 17.3 | 16.7 |
| Unknown | 6.3 | 5.9 | 6.4 | 6.2 |
Fig. 4.
Five-year patient survival by age group.
Table 6.
Risk factors for patient death (overall and by age group)
| Univariate analysis (P-value) | Multivariate analysis | Multivariate analysis by age group |
|||
|---|---|---|---|---|---|
| HR (95% IC) P-value | HR (95% IC) P-value | 40–60 HR (95% IC) P-value | >60 HR (95% IC) P-value | ||
| Recipient aged | ≤0.001 | — | — | — | — |
| Donor aged | ≤0.001 | — | — | — | — |
| BMI | ≤0.05 | — | — | — | — |
| Diabetes | ≤0.001 | — | — | 2.15 (1.08–4.27) ≤0.05 | — |
| ATN | ≤0.05 | — | — | — | — |
| Glucose at 6 months | ≤0.001 | — | — | — | — |
| Serum creatinine at 6 months | ≤0.01 | — | — | — | — |
| SBP at 6 months | ≤0.05 | — | |||
| Hepatitis C | ≤0.05 | — | — | — | — |
| Cold ischaemia | ≤0.01 | — | — | — | — |
| Cyclosporine (versus tacrolimus) | ≤0.001 | — | — | — | — |
| Cardiovascular disease pre-Tx | ≤0.001 | — | — | — | — |
| ACEI/ARB | ≤0.05 | — | — | — | 2.32 (1.30–4.14) ≤0.01 |
HR, hazards ratio.
Discussion
In this study, we analysed the most important 5-year results of renal transplantation from deceased donors in the modern immunosuppressive era in Spain. Five-year results show an excellent recipient survival and graft survival, especially in the youngest age group. Considering that all transplant patients (even retransplants, hyperimmunized, and those older than 70 years) were included, donor and recipient ages have increased and the degree of HLA matching has worsened; the survival rates obtained confirm a clear improvement in the long-term management of renal-transplant patients and that new immunosuppressive regimens counteract suboptimal features for donors and recipients. Compared with other large national and international registries focused on long-term results in renal transplant [7–10], our results suggest an improvement in long-term graft survival and slightly better long-term patient survival rates. Of interest, this finding confirms previous observations of a study carried out in Spanish transplant patients who had a functioning allograft 1 year after transplantation [11]. In this study, long-term graft survival in Spanish kidney transplant recipients is more than double of that compared with the USA, but similar death-censored graft survival are observed in Spanish and US recipients [11]. Pre-transplant medical care, co-morbidities, such as CVD, and their management in each country's health system are possible explanations for the differences between the two countries.
Contrary to previous studies carried out in Spain [7], acute rejection is not an independent factor of allograft loss and death with functioning graft is the leading cause of graft loss in patients >40 years. Over the last two decades, there has been an association observed between the introduction of new immunosuppressants, especially tacrolimus and MMF, and a significant reduction in the incidence of acute rejection [1, 2]. As acute rejection results in a functional and structural damage of the graft, it has been assumed that a decrease in its incidence should result in an improvement of late graft outcome. However, this assumption has not been previously confirmed in epidemiological studies. Moreover, in this study, the mean donor and recipient age is higher compared with other studies [12], but the use of new immunosuppressants could counterbalance the major proportion of rejection episodes and subsequent incomplete recovery of renal function associated with senescent tissue [13].
Renal graft dysfunction is the result of both immunological and non-immunological insults. Some authors consider that the presence of the risk factors involved in the metabolic syndrome induces a prominent risk for graft loss but, in this study, components of metabolic syndrome do not appear to contribute greatly to chronic graft dysfunction and only AH, systolic blood pressure and diabetes were significantly involved in the univariate analysis. Diabetes is a risk factor for graft loss in recipients younger than 40 years old, but it did not reach statistical significance at older ages. The combination of TAC + MMF, which offers an acceptable cardiovascular risk profile [14], and is received by more than 60% of patients, could also be important to explain these results [6].
However, novel CVD factors as elevated creatinine levels and proteinuria >1 g at 6 months post-transplantation were risk factors associated with a poor 5-year graft survival in all age groups. At present, different studies [15–17] have shown that the presence of proteinuria, compared with its absence, is associated with an increased risk of graft loss, patient death and cardiovascular risk [18]. Likewise, the level of proteinuria is a key factor in the prognosis of renal graft failure [19]. Cherukuri et al. [20] and a recent study in the renal-transplant population demonstrated that the group with more than 1 g/day at 3 months showed a graft failure relative risk of 16.0 (95% CI, 3.5–72; P< 0.001) which represents more than twice the risk of those patients with a proteinuria between 0.15 and 0.5. So, the use of drugs decreasing the level of proteinuria, such as ACEI and ARB, and immunosuppressive drugs without this deleterious effect are strongly recommended in these patients.
Our results also highlight that creatinine level had a significant relationship with graft survival rate. This finding corroborates previous observations which established that with every 1 mg/dL increase in creatinine level, HR of graft loss increases by 1.8 units [21]. Renal function within the first year after transplantation has been shown to be an important parameter influencing long-term graft survival [22]. Moreover, a 5-year follow-up of a large US pivotal registration trial, which focused on the long-term outcome of tacrolimus- versus cyclosporine-based immunosuppression [23], showed that during the 5-year follow-up, the mean serum creatinine levels based on intent-to-treat analysis were always lower in the tacrolimus group than in the cyclosporine group. Thus, the combination of tacrolimus + MMF, which offers an acceptable risk profile and it is received by more than 60% of patients, could also be an important factor to explain these results.
The low rate of mortality in these 5 years can be explained by the fact that our population is Caucasian, with a low rate of diabetic patients and low proportion of patients with pre-transplant CVD, and therefore, their cardiovascular risk is lower than that of pre-transplant American [24] or North European [25] populations.
Finally, patients with graft function have a high long-term survival. Infections and CVD have been reported as the predominant causes of death. Prevention of stroke is mandatory in patients younger than 40 years. Attention to atherosclerotic risk factors may be the most important challenge to further improve the longevity of patients with successful renal transplants. To avoid deaths from infection, particularly common during the first year after transplantation, there are four important aspects to consider: patient selection, prophylactic measures, early diagnosis and effective treatment. Specific diagnostic tests and effective treatment are now available for all the commonly encountered infections and should be implemented earlier rather than later. Reduction or discontinuation of immunosuppression in the presence of serious infection is also recommended [26].
Conclusions
Our results show an excellent long-term recipient survival and graft survival with recent immunosuppressive regimens, especially in the youngest age group. Death with functioning graft is the leading cause of graft loss in patients >40 years. As the incidence of acute rejection has been progressively reduced by recent immunosuppressive regimens, the assessment of other risk factors for graft loss is becoming increasingly important. Novel CVD risk factors, such as renal function and proteinuria 6 months after transplantation, can be regarded as variables predicting long-term renal graft survival, and their assessment provides a useful tool for predicting long-term outcome. The choice of immunosuppressive regimen remains critical for preventing rejection and maintaining a good renal function and low levels of proteinuria. Thus, early improvement of renal function and proteinuria together with strict control of cardiovascular risk factors, especially in younger patients are mandatory.
Conflict of interest statement
The results presented in this paper have not been published previously in whole or part, except in abstract format.
References
- 1.Pascual M, Theruvath T, Kawai T, et al. Strategies to improve long-term outcomes after renal transplantation. N Engl J Med. 2002;346:580. doi: 10.1056/NEJMra011295. [DOI] [PubMed] [Google Scholar]
- 2.Woodroffe R, Yao GL, Meads C, et al. Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation. A systematic review and modelling study. Health Technol Assess. 2005;9:1. doi: 10.3310/hta9210. [DOI] [PubMed] [Google Scholar]
- 3.Hariharan S, Johnson CP, Bresnahan BA, et al. Improved graft survival after renal transplantation in the United States, 1998 to 1996. N Engl J Med. 2000;342:605. doi: 10.1056/NEJM200003023420901. [DOI] [PubMed] [Google Scholar]
- 4.Meier-Kriesche HU, Schold JD, Srinivas TR, et al. Lack of improvement in renal allograft survival despite a marked decrease of acute rejection rates over the most recent era. Am J Transplant. 2004;4:378. doi: 10.1111/j.1600-6143.2004.00332.x. [DOI] [PubMed] [Google Scholar]
- 5.Foley RN, Parfrey PS, Samak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32(Suppl 3):112–119. doi: 10.1053/ajkd.1998.v32.pm9820470. [DOI] [PubMed] [Google Scholar]
- 6.Morales JM, Marcen R, Andres A, et al. Renal transplantation in the modern immunosuppressive era in Spain: four-year results from a multicenter database focus on post-transplant cardiovascular disease. Kidney Int. 2008;74(Suppl 111):S94–S99. doi: 10.1038/ki.2008.547. [DOI] [PubMed] [Google Scholar]
- 7.Moreso F, Alonso A, Gentil MA, et al. for the Spanish Late Allograft Dysfunction Study Group. Improvement in late real allograft survival between 1990 and 2002 in Spain: results from a multicentre case-control study. Transplant Int. 2010;23:907–913. doi: 10.1111/j.1432-2277.2010.01075.x. [DOI] [PubMed] [Google Scholar]
- 8.Cecka JM. The OPTN/UNOS renal transplant registry. Clin Transpl. 2005:1–16. [PubMed] [Google Scholar]
- 9.Teraoka S, Nomoto K, Kikuchi K, et al. Outcomes of kidney transplants from non-heart-beating deceased donors as reported to the Japan Organ Transplant Network from April 1995–December 2003: a multi-center report. Clin Transpl. 2004:91–102. [PubMed] [Google Scholar]
- 10.Fabrizii V, Kovarik J, Bodingbauer M, et al. Long-term patient and graft survival in the Eurotransplant senior program: a single-center experience. Transplantation. 2005;80:582–9. doi: 10.1097/01.tp.0000168340.05714.99. [DOI] [PubMed] [Google Scholar]
- 11.Ojo AO, Morales JM, González-Molina M, et al. Comparison of the long-term outcomes of kidney transplantation: USA versus Spain. Nephrol Dial Transplant. 2012 doi: 10.1093/ndt/gfs287. doi:10.1093/ndt/gfs287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seron D, Arias M, Campistol JM, et al. for the Spanish Chronic Allograft Study Group. Late renal allograft failure between 1990 and 1998 in Spain: a changing scenario. Transplantation. 2003;76:1588–1594. doi: 10.1097/01.TP.0000092495.07385.3C. [DOI] [PubMed] [Google Scholar]
- 13.de Fijter JW, Mallat MJ, Doxiadis II, et al. Increased immunogenicity and cause of graft loss of old donor kidneys. J Am Soc Nephrol. 2001;12:1538. doi: 10.1681/ASN.V1271538. [DOI] [PubMed] [Google Scholar]
- 14.Morales JM, Dominguez-Gil B. Impact of Tacrolimus and Mycophenolate Mofetil combination on cardiovascular risk profile after kidney transplantation. J Am Soc Nephrol. 2006;17(Suppl 3):s296–s303. doi: 10.1681/ASN.2006080930. [DOI] [PubMed] [Google Scholar]
- 15.Roodnat JI, Mulder PGH, Van Riemsdijk IC, et al. Ischemia times and donor serum creatinine in relation to renal graft failure. Transplantation. 2003;75:799–804. doi: 10.1097/01.TP.0000056632.00848.8D. [DOI] [PubMed] [Google Scholar]
- 16.Ibis A, Altunoglu A, Akgüll A, et al. Early onset proteinuria after renal transplantation: a marker for allograft dysfunction. Trasplant Proc. 2007;39:938–940. doi: 10.1016/j.transproceed.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 17.Sancho A, Gavela E, Avila A, et al. Risk factors and prognosis for proteinuria in renal transplant recipients. Transplant Proc. 2007;39:2145–2147. doi: 10.1016/j.transproceed.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 18.Fernandez G, Plaza JJ, Sanchez-Plumed J, et al. Proteinuria: a new marker of long-term graft and patient survival in kidney transplantation. Nephrol Dial Transplant. 2004;19(Suppl 3):47–51. doi: 10.1093/ndt/gfh1015. [DOI] [PubMed] [Google Scholar]
- 19.Yildiz A, Erkoç R, Sever MS, et al. The prognostic importance of severity and type of post-transplant proteinuria. Clin Transpl. 1999;13:241–244. doi: 10.1034/j.1399-0012.1999.130304.x. [DOI] [PubMed] [Google Scholar]
- 20.Cherukuri A, Welberry-Smith MP, Tattersall JE, et al. The clinical significance of early proteinuria after renal transplantation. Transplantation. 2010;89:200–207. doi: 10.1097/TP.0b013e3181c352c5. [DOI] [PubMed] [Google Scholar]
- 21.Rayhill SC, D'Alessandro AM, Odorico JS, et al. Simultaneous pancreas–kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg. 2000;231:417–423. doi: 10.1097/00000658-200003000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hariharan S, McBride MA, Cherikh WS, et al. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62:311–318. doi: 10.1046/j.1523-1755.2002.00424.x. [DOI] [PubMed] [Google Scholar]
- 23.Vincenti F, Jensik SC, Filo RS, et al. A long-term comparison of tacrolimus (FK506) and cyclosporine in kidney transplantation: evidence for improved allograft survival at five years. Transplantation. 2002;73:775–782. doi: 10.1097/00007890-200203150-00021. [DOI] [PubMed] [Google Scholar]
- 24.Kim SJ, Schaubel DE, Fenton SA, et al. Mortality after kidney transplantation: a comparison between the United States and Canada. Am J Transplant. 2006;6:109–114. doi: 10.1111/j.1600-6143.2005.01141.x. [DOI] [PubMed] [Google Scholar]
- 25.Lindholm A, Albrechtsen D, Frodin L, et al. Ischemic heart disease: major cause of death and graft loss alter renal transplantation. Transplantation. 1995;60:451–457. doi: 10.1097/00007890-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Briggs D. Causes of death after renal transplantation. Nephrol Dial Transplant. 2001;16:1545–1549. doi: 10.1093/ndt/16.8.1545. [DOI] [PubMed] [Google Scholar]