Abstract
Background:
Obsessive compulsive disorder has been reported in patients with multiple sclerosis (MS). Obsessive compulsive disorder (OCD) is a kind of anxiety disorder characterized by a combination of repetitive thoughts and repetitive behaviors for reducing anxiety. We aimed to investigate the frequency of OCD in patients with MS.
Materials and Methods:
112 patients with multiple sclerosis participated in this study. Demographic data were obtained through using patients’ medical records. MS clinical subtypes, the duration of disease and neurological signs were determined. The Kurtzke Expanded Disability Status Scale (EDSS) was used to quantify disability in MS, which was confirmed by psychiatrist through using DSM-IV criteria for OCD. The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was used to rate the severity of OCD. Data analysis was performed by SPSS for Windows software (version 15.0) and Chi-square test and Exact test were used for analyzing data.
Results:
The frequency of OCD in patients with MS was 16.1%. The OCD was significantly correlated with a higher EDSS score (X2 = 86.515, P = 0.0001). OCD was also significantly correlated with the duration of disease, phenotypic subgroup, cranial nerve involvement, cerebellar, autonomic, sensory and motor nerve involvement.
Conclusions:
OCD might be considered in quantifying disability of patients with MS. It might be suggested that all the patients with MS to be screened for OCD.
Keywords: Obsessive compulsive disorder, multiple sclerosis, Frequency
INTRODUCTION
Obsessive compulsive disorder (OCD) is an anxiety disorder characterized by a combination of obsession, i.e. repetitive thoughts or images caused by severe anxiety and compulsion that is repetitive behaviors for reducing anxiety. OCD prevalence is 1-3 % among adults and pediatric population.[1] In Iran, the prevalence of OCD is 8.87%, and it is more common among the persons residing in urban regions and the ones who have a positive OCD among their families.[2] Comorbidity of OCD with depression and anxiety disorders is very common.[3,4]
The exact etiology of OCD is unknown, but it is believed that serotonin neurotransmitter may play a role in pathogenesis of OCD.[5] Gene deletions have been reported in animal models with symptoms similar to OCD. In patients with OCD, brain dysfunction has been also have a role in pathogenesis of OCD.[11]
Multiple sclerosis (MS) is an autoimmune disorder characterized by the destruction of myelin in central nervous system. The peak prevalence is between ages 20 and 40 and it is twice more common in women than in men. Sensory dysfunction of the limbs is the most common clinical symptom in these patients.[12] In some areas, prevalence of MS is rising.[13,14] MS has 4 phenotypes: relapsing-remitting, primary progressive, progressive relapsing and secondary progressive.[12] The exact etiology of MS is unknown, but it is believed that MS is the result of interaction between genes and the environment.[15] The two most important environmental factors are viral infections and ultraviolet B radiation exposure.[16,17] Furthermore, MS exacerbation is associated with stressful life.[18] The best diagnostic test for MS is MRI, but it is not specific for MS.[19]
Comorbidity of MS and psychiatric disorders have been documented. Depression is the most common mental disorder in MS.[20] Other psychiatric disorders include: bipolar disorder, pseudo-bulbar affect, anxiety, personality changes, cognitive disorders, acoustic hallucinations, binge eating and impulse control disorders.[21–24]
OCD has been reported in patients with multiple sclerosis.[23,25–29] In some previous studies, the prevalence of OCD in multiple sclerosis was 8.6%. The etiology of OCD in multiple sclerosis is unknown, but some researchers believe that OCD is the result of disruption of the functional connection between cortical-cortical and/or cortical-subcortical brain regions.[29] It has been reported that the patients with brain-white matter abnormalities due to multiple sclerosis, cerebrovascular diseases, and paraneoplastic leucoencephalopathy may develop OCD symptoms.[28] Autoimmunity may play a role in pathogenesis of OCD in multiple sclerosis. Researchers have shown a link between OCD and autoimmunity.[30] Anti-brain antibodies have been reported in patients with OCD.[31]
For more clarification of the relationship between OCD and multiple sclerosis, we aimed to investigate the frequency of OCD in a group of patients with multiple sclerosis.
MATERIALS AND METHODS
Subjects
112 consecutive known cases of multiple sclerosis participated in this study whose disease was diagnosed during the year 2008 at outpatient MS clinic in GHAEM hospital (Mashhad, Iran). Patients with serious neurological or psychiatric diseases such as epilepsy, drug abuse, mental retardation, psychosis, depression, anxiety, etc…and patients who did not accept to join the study were excluded from the study. Our Institutional Ethics Committee also approved our research project. An informed consent was obtained from the patients participating in the study or from their parents. Demographic data including age, gender, educational level, and marriage status were collected through using patients’ medical records. Definite diagnosis of MS was made by neurologist using Mc Donald criteria.[32] Clinical manifestations including MS clinical subtypes (relapsing-remitting, primary progressive, progressive relapsing and secondary progressive), the duration of disease, neurological signs such as, cortical dysfunction, cranial nerve involvement, cerebellar involvement, and sensory, motor or autonomic nerve involvement. The drugs used by the patients were determined.
Scales
The Kurtzke Expanded Disability Status Scale (EDSS) was used to quantify the disability in multiple sclerosis.[33] Firstly, the patients screened for OCD symptoms by psychiatrist, she also ruled out depression and anxiety in these patients; and the OCD was confirmed through using DSM-IV criteria for OCD. The family history of OCD was determined by psychiatrist via asking the patient and by additional information supplied by others (parents). Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was used to rate the severity of OCD symptoms where a score between 8 and 15 was mild, between 16 and 23 was moderate, between 24 and 31 was severe, and between 32 and 40 was very severe.[34] For this purpose, a check list was prepared by psychiatrist and it was completed during an interview with the patient. An example of this check list was illustrated in Figure 1. Target symptoms were determined and the score was calculated for each patient. Then, the relationship between OCD and MS was evaluated.
Statistical analysis
Data analysis was performed by SPSS for Windows software (version 15.0) and Chi-square test and the Exact test were used for data analysis. The P value ≤ 0.05 was considered statistically significant.
RESULTS
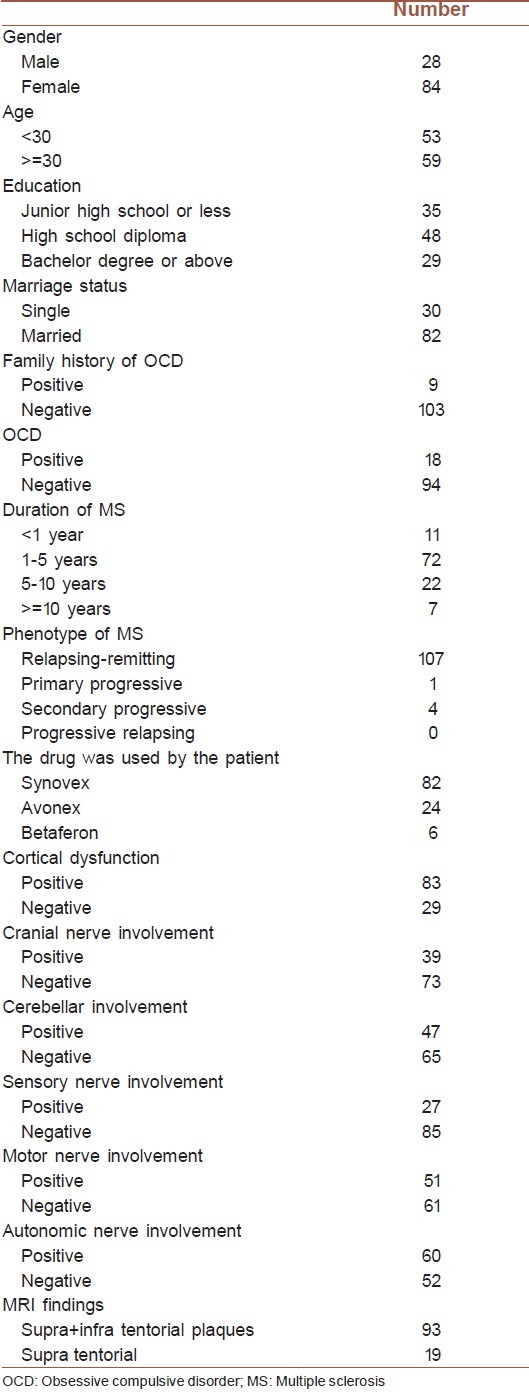
A total of 112 patients participated in this study (25% male and 75% female and female/male ratio: 2.29). Mean age was 31.9 (range: 14-48 years). 25.9% of the patients had bachelor degree or higher, and 73.2% of all patients were married. Demographic data and clinico-pathological profiles were illustrated in Table 1.
Table 1.
Demographic data and clinico pathological profiles
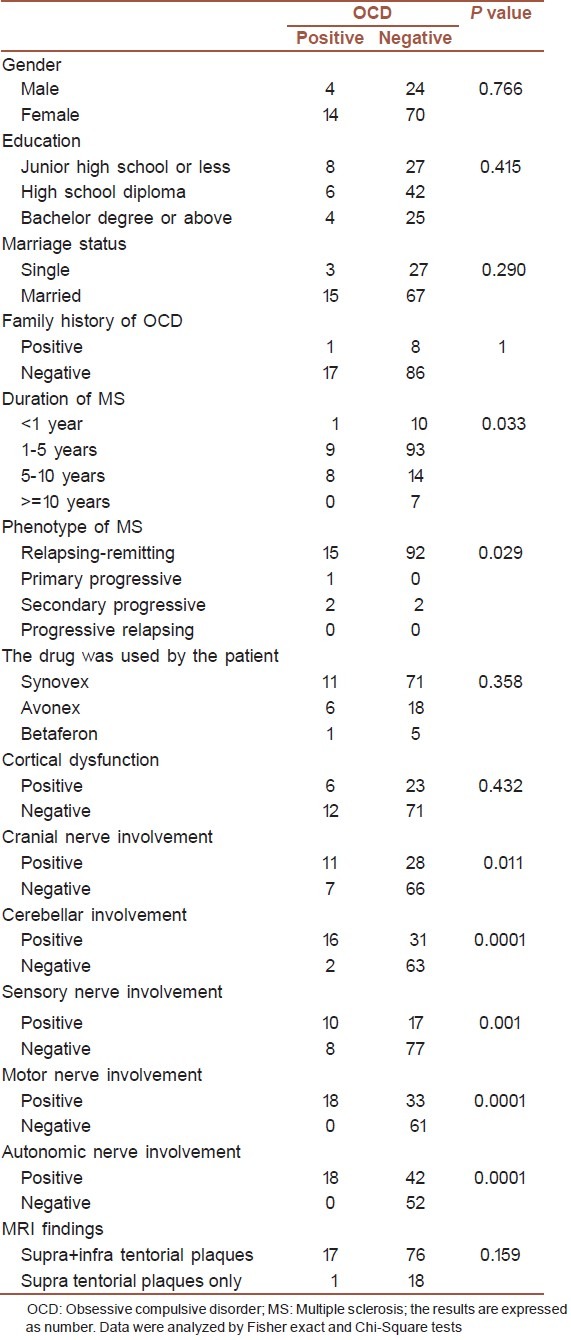
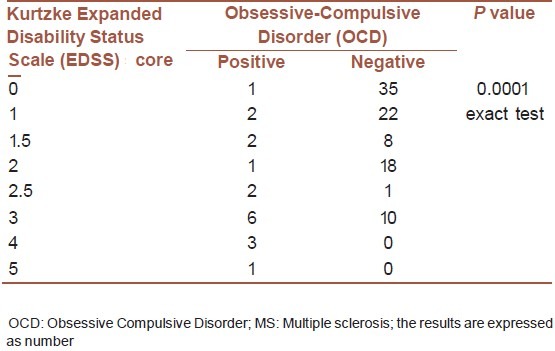
OCD was confirmed in 18 patients out of 112 patients (16.1%). Only 9 patients had a positive family history for OCD. According to the exact test results, EDSS score was ≥ 3 in 10 patients out 18 patients with OCD. OCD was significantly correlated with a higher EDSS score (X2 = 86.515, P = 0.0001). The predominant phenotype was relapsing-remitting (95.5%), and there was no case of progressive relapsing phenotype. Exact test analysis showed an association between OCD and phenotypic subgroups in patients with multiple sclerosis (X2 = 8.970, P = 0.029). Duration of the disease was ≥ 10 years in 7 patients (6.3%) with multiple sclerosis. The OCD was significantly correlated with the duration of disease in patients with multiple sclerosis (According to Exact test: X2 = 9.135, P = 0.033). There was also a significant correlation between OCD and cranial nerve involvement (according to Chi-square test: X2 = 6.531, P = 0.011), cerebellar involvement (according to Chi-square test: X2 = 19.390, P = 0.0001) and sensory nerve involvement (according to Chi-square test: X2 = 11.593, P = 0.001). All of the patients with OCD had also autonomic nerve involvement (according to Chi-square test: X2 = 18.587, P = 0.0001) and motor nerve involvement (according to Chi-square test: X2 = 25.652, P = 0.0001).
Only 9 patients had a positive family history for OCD, but according to Chi-square test results, there was no statistically significant correlation between OCD and family history. There was also no statistically significant correlation between OCD and demographic variables including age, gender, educational level, and marriage status.
Most commonly, the patients used the SYNOVEX for treatment of MS, but according to the Exact test results, the type of drug that was used by the patient had no statistically significant correlation with OCD. Cortical dysfunction was observed in 74.1% of the patients, but there was no association between OCD and cortical dysfunction. The relationship between OCD and other variables was illustrated in Table 2.
Table 2.
The relationship between OCD and other variables
OCD was confirmed in 18 patients out of 112, and severe symptoms were found in 4.7% of these patients. According to EDSS scale, there was an association between the severity of MS and OCD in these patients (X2 = 86.515, P = 0.0001).
The relationship between OCD and EDSS scores was summarized in Table 3.
Table 3.
The relationship between OCD and EDSS scores
DISCUSSION
This study was performed on 112 patients with multiple sclerosis. In this cross-sectional study, the prevalence of OCD in patients with multiple sclerosis was determined.
In our study, the prevalence of OCD in patients with multiple sclerosis is 16.1% that is higher than the prevalence of OCD in general population.[35] Assarian et al. measured the prevalence of OCD among 293 Iranian high school students. In their study, the prevalence of OCD was 8.87%.[2] The prevalence of OCD in Beiske et al. study was reported to be 19.3%, which is close to our findings.[36]
In Korostil et al. study that was performed on 140 consecutive cases of MS, the prevalence of obsessive compulsive disorder was 8.6%.[27] In Feinstein et al. study, the percentage of OCD in 150 patients with multiple sclerosis was 15.8%.[37] The differences in prevalence may partially be due to the cultural factors and the area that the patients live[2] or the drug beta interferon that has been reported to raise anxiety disorders prevalence in patients with MS.[35] In chronic usage, the drug beta interferon may cause mood alterations and anxiety attacks.[38] In our study, the patients did not differ in ethnicity. In contrast to Feinstein et al.'s findings,[37] in our study, there was an association between OCD and the duration of disease, phenotypic subgroups and with a higher EDSS score that describes patient's reaction to a debilitating disorder. In our study, the OCD was significantly correlated with cranial nerve involvement, cerebellar involvement, autonomic nerve involvement, and motor and sensory nerve involvement. These findings are compatible with the previous reports of brain dysfunction in patients with OCD. Kalatzis et al., have shown that the OCD patients have abnormalities at the prefrontal and temporo-central brain regions.[7] In another study, pathological changes were found at different locations in patients with OCD.[8–10] But, it is not clear if OCD was induced by neurological dysfunction as a stressor or it was a separate disease. Furthermore, it is believed that cerebral lesions in periventricular white matter, caudate nuclei and deep subcortical white matter can simulate OCD symptoms.[39]
In our study, there was no statistically significant correlation between OCD and a positive family history of OCD, which is consistent with Aouizerate et al. study.[33] Assarian et al. have shown a positive family history of OCD among the first or second degree relatives.[2]
In our study, there was no statistically significant correlation between OCD and demographic variables including age, gender, educational level, and marriage status in patients with multiple sclerosis. In epidemiological studies, OCD was slightly more common in women, but the difference was not statistically significant and there was no statistically significant correlation between OCD and socio-demographic status of the patients.[40]
Collectively, our study aimed at investigating the prevalence of OCD in patients with multiple sclerosis.
The OCD was significantly correlated with the duration of disease, phenotypic subgroup, cranial nerve involvement, cerebellar involvement, autonomic nerve involvement, and sensory and motor nerve involvement as well as with a higher EDSS score. Our findings suggest that, in addition to functional disability and motor dysfunction, other factors including obsessive compulsive disorder should be considered in quantifying disability of the patients with multiple sclerosis. But more investigations are mandatory because of limitations of our study including small sample size and other limitations of a cross-sectional study, in general, that this kind of study can not establish causality.
ACKNOWLEDGMENTS
This research was the result of an approved medical student thesis project (No. 6257).
The authors would like to thank the vice-chancellery of research of Mashhad University of Medical Sciences.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zaudig M. Obsessive-compulsive disorder-clinical picture, diagnosis, and therapy. Z Psychosom Med Psychother. 2011;57:3–50. doi: 10.13109/zptm.2011.57.1.3. [DOI] [PubMed] [Google Scholar]
- 2.Assarian F, Biqam H, Asqarnejad A. An epidemiological study of obsessive-compulsive disorder among high school students and its relationship with religious attitudes. Arch Iran Med. 2006;9:104–7. [PubMed] [Google Scholar]
- 3.Zaudig M. Heterogeneity and comorbidity of obsessive-compulsive disorder. (292, 294-6).Nervenarzt. 2011;82:290. doi: 10.1007/s00115-010-2966-z. [DOI] [PubMed] [Google Scholar]
- 4.Shabani A, Alizadeh A. The specific pattern of obsessive-compulsive symptoms in patients with bipolar disorder. JRMS. 2008;13:48–54. [Google Scholar]
- 5.Schirmbeck F, Esslinger C, Rausch F, Englisch S, Meyer-Lindenberg A, Zink M. Antiserotonergic antipsychotics are associated with obsessive-compulsive symptoms in schizophrenia. Psychol Med. 2011 Nov;41(11):2361–73. doi: 10.1017/S0033291711000419. [DOI] [PubMed] [Google Scholar]
- 6.Yang XW, Lu XH. Molecular and cellular basis of obsessive-compulsive disorder-like behaviors: Emerging view from mouse models. Curr Opin Neurol. 2011;24:114–8. doi: 10.1097/WCO.0b013e32834451fb. [DOI] [PubMed] [Google Scholar]
- 7.Kalatzis I, Piliouras N, Glotsos D, Ventouras E, Papageorgiou C, Rabavilas A, et al. Identifying Differences in the P600 Component of ERP-Signals between OCD Patients and Controls Employing a PNN-based Majority Vote Classification Scheme. Conf Proc IEEE Eng Med Biol Soc. 2005;4:3994–7. doi: 10.1109/IEMBS.2005.1615337. [DOI] [PubMed] [Google Scholar]
- 8.Zitterl W, Wimberger D, Demal U, Hofer E, Lenz G. Nuclear magnetic resonance tomography findings in obsessive-compulsive disorder. Nervenarzt. 1994;65:619–22. [PubMed] [Google Scholar]
- 9.Gohle D, Juckel G, Mavrogiorgou P, Pogarell O, Mulert C, Rujescu D. Electrophysiological evidence for cortical abnormalities in obsessive-compulsive disorder - a replication study using auditory event-related P300 subcomponents. J Psychiatr Res. 2008;42:297–303. doi: 10.1016/j.jpsychires.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Kathmann N, Rupertseder C, Hauke W, Zaudig M. Implicit sequence learning in obsessive-compulsive disorder: Further support for the fronto-striatal dysfunction model. Biol Psychiatry. 2005;58:239–44. doi: 10.1016/j.biopsych.2005.03.045. [DOI] [PubMed] [Google Scholar]
- 11.Shimizu E. The paradigm of abnormal sensory gating in fear extinction as pathophysiology in obsessive-compulsive disorder. Seishin Shinkeigaku Zasshi. 2011;113:54–9. [PubMed] [Google Scholar]
- 12.Stüve O, Oksenberg J. GeneReviews. Seattle (WA): University of Washington, Seattle; 1993-2006. Multiple Sclerosis Overview. [Google Scholar]
- 13.Marrie RA, Yu N, Blanchard J, Leung S, Elliott L. The rising prevalence and changing age distribution of multiple sclerosis in Manitoba. Neurology. 2010;74:465–71. doi: 10.1212/WNL.0b013e3181cf6ec0. [DOI] [PubMed] [Google Scholar]
- 14.Sahraian MA, Khorramnia S, Ebrahim MM, Moinfar Z, Lotfi J, Pakdaman H. Multiple sclerosis in Iran: A demographic study of 8,000 patients and changes over time. Eur Neurol. 2010;64:331–6. doi: 10.1159/000321649. [DOI] [PubMed] [Google Scholar]
- 15.Comabella M, Khoury SJ. Immunopathogenesis of multiple sclerosis. Clin Immunol. 2012;142:2–8. doi: 10.1016/j.clim.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Owens GP, Gilden D, Burgoon MP, Yu X, Bennett JL. Viruses and multiple sclerosis. Neuroscientist. 2011;17:659–76. doi: 10.1177/1073858411386615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramagopalan SV, Handel AE, Giovannoni G, Rutherford Siegel S, Ebers GC, Chaplin G. Relationship of UV exposure to prevalence of multiple sclerosis in England. Neurology. 2011;76:1410–4. doi: 10.1212/WNL.0b013e318216715e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitsonis CI, Potagas C, Zervas I, Sfagos K. The effects of stressful life events on the course of multiple sclerosis: a review. Int J Neurosci. 2009;119:315–35. doi: 10.1080/00207450802480192. [DOI] [PubMed] [Google Scholar]
- 19.Sahraian MA, Radue EW, Haller S, Kappos L. Black holes in multiple sclerosis: Definition, evolution, and clinical correlations. Acta Neurol Scand. 2010;122:1–8. doi: 10.1111/j.1600-0404.2009.01221.x. [DOI] [PubMed] [Google Scholar]
- 20.Alajbegovic A, Loga N, Tiro N, Alajbegovic S, Todorovic L, Jasminika-Djelilovic Depression in multiple sclerosis patients. Med Arh. 2011;65:115–8. [PubMed] [Google Scholar]
- 21.Iacovides A, Andreoulakis E. Bipolar disorder and resembling special psychopathological manifestations in multiple sclerosis: A review. Curr Opin Psychiatry. 2011;24:336–40. doi: 10.1097/YCO.0b013e328347341d. [DOI] [PubMed] [Google Scholar]
- 22.da Silva AM, Vilhena E, Lopes A, Santos E, Gonçalves MA, Pinto C, et al. Depression and anxiety in a Portuguese MS population: Associations with physical disability and severity of disease. J Neurol Sci. 2011;306:66–70. doi: 10.1016/j.jns.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 23.Wilkening A, Haltenhof H. Mental disorders associated with multiple sclerosis. Dtsch Med Wochenschr. 2006;131:154–8. doi: 10.1055/s-2006-924938. [DOI] [PubMed] [Google Scholar]
- 24.Ceschin L, Giannunzio V, Favaro A, Santonastaso P. Pica in an eating disordered woman with multiple sclerosis: impulse dys-control, compulsive symptom or self-medication attempt? Eat Weight Disord. 2010;15:e116–8. doi: 10.1007/BF03325290. [DOI] [PubMed] [Google Scholar]
- 25.George MS, Kellner CH, Fossey MD. Obsessive-compulsive symptoms in a patient with multiple sclerosis. J Nerv Ment Dis. 1989;177:304–5. doi: 10.1097/00005053-198905000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Miguel EC, Stein MC, Rauch SL, O’Sullivan RL, Stern TA, Jenike MA. Obsessive-compulsive disorder in patients with multiple sclerosis. J Neuropsychiatry Clin Neurosci. 1995;7:507–10. doi: 10.1176/jnp.7.4.507. [DOI] [PubMed] [Google Scholar]
- 27.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13:67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- 28.Fontenelle LF, Harrison BJ, Yücel M, Pujol J, Fujiwara H, Pantelis C. Is there evidence of brain white-matter abnormalities in obsessive-compulsive disorder?: A narrative review. Top Magn Reson Imaging. 2009;20:291–8. doi: 10.1097/RMR.0b013e3181e8f22c. [DOI] [PubMed] [Google Scholar]
- 29.Douzenis A, Michalopoulou PG, Voumvourakis C, Typaldou M, Michopoulos I, Lykouras L. Obsessive-compulsive disorder associated with parietal white matter multiple sclerosis plaques. World J Biol Psychiatry. 2009;10:956–60. doi: 10.1080/15622970701762528. [DOI] [PubMed] [Google Scholar]
- 30.Hoekstra PJ, Minderaa RB. Tic disorders and obsessive-compulsive disorder: Is autoimmunity involved? Int Rev Psychiatry. 2005;17:497–502. doi: 10.1080/02646830500382003. [DOI] [PubMed] [Google Scholar]
- 31.Maina G, Albert U, Bogetto F, Borghese C, Berro AC, Mutani R, et al. Anti-brain antibodies in adult patients with obsessive-compulsive disorder. J Affect Disord. 2009;116:192–200. doi: 10.1016/j.jad.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 32.McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–7. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 33.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS) Neurology. 1983;33:1444–52. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 34.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 35.Greenberg DA, Aminoff MJ, Simon RP. Clinical neurology. 5th ed. 2002. pp. 167–70. [Google Scholar]
- 36.Beiske AG, Svensson E, Sandanger I, Czujko B, Pedersen ED, Aarseth JH, et al. Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol. 2008;15:239–45. doi: 10.1111/j.1468-1331.2007.02041.x. [DOI] [PubMed] [Google Scholar]
- 37.Feinstein A, O’Connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Mult Scler. 1999;5:323–6. doi: 10.1177/135245859900500504. [DOI] [PubMed] [Google Scholar]
- 38.Exton MS, Baase J, Pithan V, Goebel MU, Limmroth V, Schedlowski M. Neuropsychological performance and mood states following acute interferon-beta-1b administration in healthy males. Neuropsychobiology. 2002;45:199–204. doi: 10.1159/000063671. [DOI] [PubMed] [Google Scholar]
- 39.Weiss AP, Jenike MA. Late-Onset Obsessive-Compulsive Disorder: A case series. J Neuropsychiatry Clin Neurosci. 2000;12:265–8. doi: 10.1176/jnp.12.2.265. [DOI] [PubMed] [Google Scholar]
- 40.Cilliçilli AS, Telcioglu M, Aşkin R, Kaya N, Bodur S, Kucur R. Twelve-month prevalence of obsessive-compulsive disorder in Konya, Turkey. Compr Psychiatry. 2004;45:367–74. doi: 10.1016/j.comppsych.2004.06.009. [DOI] [PubMed] [Google Scholar]


