Abstract
Rosai-Dorfman disease is a benign lymphohistiocytosis that often involve lymph nodes and present as massive lymphadenopathy with sinus histiocytosis. The disease is rarely associated with intracranial involvement. Herein, we report a 33-years-old man with recent onset of unconsciousness. According to his past medical history, he was suffering from frontal headache, ataxia and dizziness with no sensory or motor defect since August 2010. At initial work up, MRI showed infiltrating mass in the left parietal region. Microscopically, the mass consisted of infiltration of abundant lymphoplasma cells, neutrophils and some histiocytes scattered in fibrotic background. Emperipolesis (lymphocytophagocytosis) of histiocytic cells made the diagnosis of Rosai-Dorfman disease. Rosai-Dorfman disease should be added in the list of differential diagnosis for a dural mass mimicking meningioma or cerebral mass mimicking glioma, therefore, immunohistochemical staining for EMA, S100 and CD1a should be performed to rule out the differential diagnosis.
Keywords: Emperipolesis, intracranial Rosai-Dorfman disease
INTRODUCTION
In 1969, Rosai-Dorfman disease first reported by Juan Rosai and Ronald Dorfman as sinus histiocytosis with massive lymphadenopathy in young black male.[1] The disease presenting with bilateral, painless, massive cervical lymphadenopathy with a protracted clinical course in up to 90% of the patients.[2] Clinical findings in most instances are malaise, fever, normocytic anemia, hemolytic anemia, neutrophilia, elevated erythrocyte sedimentation rate and polyclonal gammopathy.[3,4] Rosai-Dorfman disease (prevalence=1/200000) predominantly affected the children and young adult with a mean age of presentation of 20.6 years and with a slight male predominance, but the disease can be seen in the range of 1 to 74 years old.[4,5] Extranodal involvement is documented in 43% of the patients, occasionally accompanied with lymphadenopathy early or later in the disease course.[2–5] The most common extranodal sites, in the decreasing order of frequency, are skin, nasal cavity, paranasal sinus, eyelid, orbit, bone, salivary gland and central nervous system.[2–5] The central nervous system can be involved in less than 5% of the Rosai-Dorfman disease and in 90% of these cases, the leptomeninges are afflicted.[6–8] CNS Rosai-Dorfman disease shows a predilection for males, and typically presents during the 4th to 5th decade with the mean age of 39.4 years old.[9]
CASE REPORT
A 33-years-old man was referred to our hospital on December 2010, his complaint was unconsciousness. According to his past medical history, he was suffering from frontal headache, ataxia and dizziness with no sensory or motor defect since August 2010. He was married and worked in Butcher shop since many years ago. His economic and health condition was not suitable. He had low literacy. His familial history was non-contributory. At initial work up, brain CT scan and MRI showed infiltrating mass adjacent to lateral ventricle with effacement of anatomical sign of the left parietal region. Left frontal horn was collapsed and left temporal horn was dilated [Figure 1]. There was subfalcine hernia to the right side [Figure 2]. No definite lesion was found at the dura. Laboratory tests were unremarkable.
Figure 1.
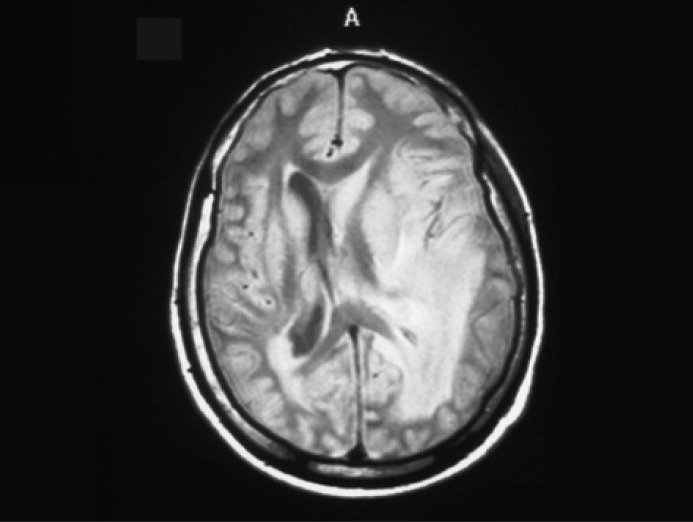
Left periventricular mass that occupy temporal white matter and extend to adjacent gray matter
Figure 2.
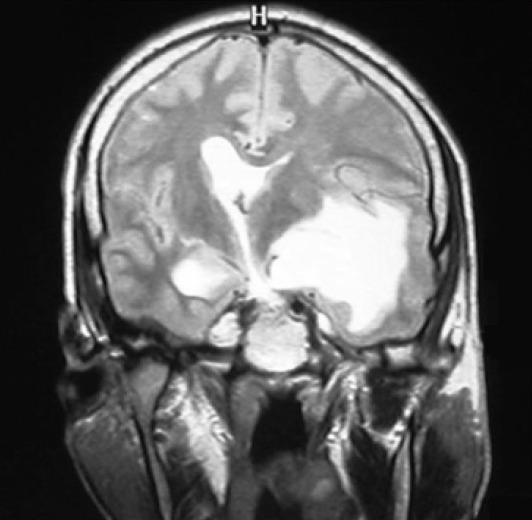
There is enhancing mass that shows subfalcine hernia to right side
He was candidate for surgical operation with an initial diagnosis of glioma versus lymphoma. The lesion was excised and was sent to our laboratory for pathologic examination. It was gray- white in color and rubbery in consistency.
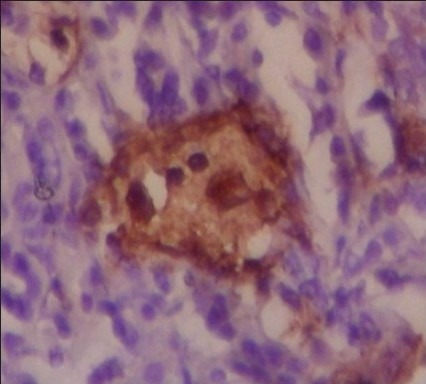
Microscopically, it consisted of infiltration of abundant lymphoplasma cells, neutrophils and some histiocytes scattered in fibrotic background [Figure 3a].
Figure 3a.
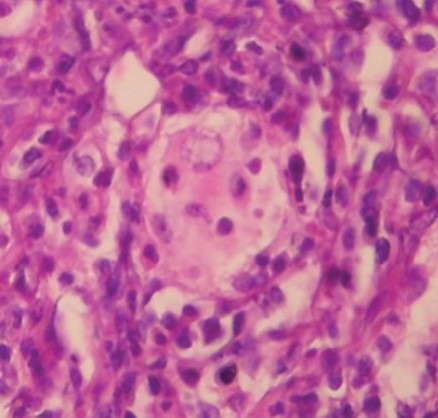
Lesion is composed of attenuated infiltrate of lymphoplasma cells, neutrophils and histiocytic cells with eosinophilic granular cytoplasm. Histiocytic cells occasionally show emperipolesis
The infiltration of lymphoplasma cells and neutrophils were so intense that obscured background histiocytes. Some histiocytes showed sheet like arrangement without granulomatous formation. The cytoplasm of the histiocytes was pale and eosinophilic, and sometimes foamy. The vesiculated nuclei of the histiocytes were not folded. Emperipolesis (lymphocytophagocytosis) of histiocytic cells made the diagnosis of Rosai-Dorfman disease [Figure 3a].
Immunohistochemical staining was performed to rule out the meningioma and confirm the diagnosis. It was noticeable that plasma cells were immunoreactive for EMA [Figure 3b]. Suspected cells were negative for epithelial membrane antigen (EMA) and positive for S100 [Figure 3c].
Figure 3b.
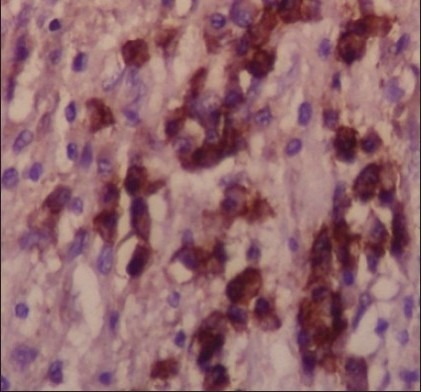
infiltrated plasma cells are immunoreactive for EMA
Figure 3c.
Histiocytic cells with emperipolesis are immunoreactive for S-100 protein and negative for EMA
DISCUSSION
An involvement of temporal lobe of CNS parenchyma is unusual presentation of the disease that occurred in our patient. CNS can be involved less than 5% of Rosai-dorfman disease.[6,7] In 70% of CNS-Rosai-Dorfman disease, the presentation is limited to the brain or to the spinal cord and is not associated with lymphadenopathy.[10] Approximately, 75% of CNS afflictions are intracranial, whereas 25% involve the spine.[10] Over 90% of CNS Rosai-Dorfman disease leptomeninges are only involved.[8]
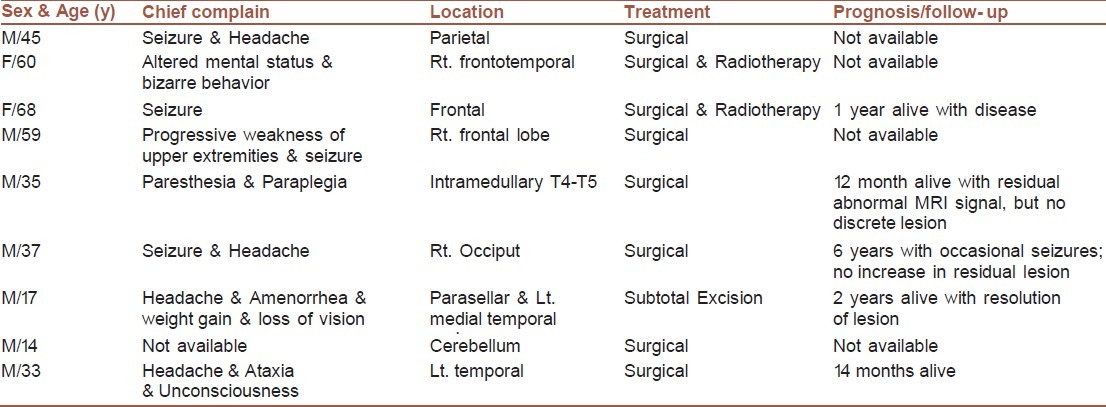
At literature, we founded 8 cases in additional to our case that had been afflicted with intra-axial CNS-Rosai-Dorfman disease. Their clinical data are summarized in Table 1. 70% of the patients were male, and the disease occurred in the range of 14 to 68 years old. The main complain of the patients were related to the site of involvement that were mostly frontotemporal region. The common treatment was surgical (maybe due to uncertain diagnosis), and prognosis was good at least for the short term follow-up.
Table 1.
The characteristic of CNS-Rosai-dorfman disease
In the present case, clinical differential diagnosis included several diseases (such as glioma and lymphoma), characterized by the extensive infiltrating mass adjacent to the left ventricle. Obviously, a precise diagnosis could not been reached on clinical grounds alone.
Histologically, Rosai-Dorfman disease is characterized by an attenuated infiltration of lymphoplasma cells and pale histiocytes of varying size, either interspersed or in sheet like pattern. These histiocytes have round or oval vesicular nuclei with well-defined, delicate nuclear membranes and single prominent nucleoli. Over 70% of the case, the histiocytes show emperipolesis that is characteristic of Rosai-Dorfman disease. Occasionally, neutrophils and eosinophils are noted. Fibrosis in the background can be seen in extranodal involvement of disease. On immunohistochemical examination, histiocytes are immunoreactive for S-100 protein, HAM 56, α1 antitrypsin, α1 chymotrypsin, lysozyme, Mac 387 and Ki-1, but are negative for CD 1a and EMA.[5,6,11,12]
Although it is difficult to diagnose the CNS-Rosai-Dorfman disease on frozen section examination, it is easy to find emperiopolesis in FNA or in cytologic examination, and thus the role of fine-needle aspiration cytology in its diagnosis is more powerful.[13]
The histopathologic differential diagnosis of this particular case included lymphoma, plasma cell granuloma, plasma cell rich meningioma and Langerhans cell histiocytosis. In our case, lymphoma was unlikely, considering the lack of monotonous atypical lymphocytes. It might be difficult to distinguish Rosai-Dorfman disease from plasma cell granuloma in the absence of emperipolesis. Langerhans cell histiocytosis was unlikely, because Langerhans histiocytes with their folded nuclei and eosinophil infiltrates were absent. Plasma cell rich meningioma was unlikely, because there were no staining for EMA. In our case, the plasma cells were immunoreactive for EMA.
The choice of treatment for Rosai-Dorfman disease is not well-established. Common treatments are surgical, steroids, chemotherapeutic agents and radiation. Surgical resection seems to be the most effective treatments.[14] Recurrence after surgical therapy is rare and limited to uncompleted debulking, multi-organ involvement and large mass.[3,15,16] Spontaneous regression could happen.[17] Prognosis of the disease is good, and no death was reported to CNS-Rosai-Dorfman disease. Our patient is alive after the follow-up of 14 months.
The precise etiology of Rosai-Dorfman disease remains unknown. The researches reveal some association between RDD and bacteria (Klebsiella), virus (Epstein barr virus, parvovirus B 19), immune dysfunction (or an aberrant response to an unspecified antigen, HHV-6 or EBV), defective Fas/FasL signaling.[6,13–18] The high frequency of cases in some part of the world may be due to the environmental factors.[3]
CONCLUSIONS
Rosai-Dorfman disease should be added in the list of differential diagnosis for a dural mass mimicking meningioma or cerebral mass mimicking glioma. It can be misinterpret as plasma cell granuloma, plasma cell rich meningioma and Langerhans cell histiocytosis in histopathological examinations due to an intense infiltration of inflammatory cells, therefore, immunohistochemical staining for EMA, S100 and CD1a should be performed to rule out the differential diagnosis, but it is noticeable that plasma cells are EMA positive in this lesion. Because of easily illustration of emperiopolesis cytological process like FNA are helpful and can be done for planning of treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadeno-pathy: a newly recognized benign clinicopathological entity. Arch Pathol. 1969;87:63–70. [PubMed] [Google Scholar]
- 2.Foucar E, Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): Review of the entity. Semin Diagn Pathol. 1990;7:19–73. [PubMed] [Google Scholar]
- 3.Vemuganti GK, Naik MN, Honavar SG. Rosai dorfman disease of the orbit. J Hematol Oncol. 2008;1:7. doi: 10.1186/1756-8722-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fukoshima T, Yachi K, Ogino A, Ohta T, Watanabe T, Yoshino A, et al. Isolated intracranial rosai-Dorfman disease without dural attachment-case report. Neurol Med Chir (Tokyo) 2011;51:136–40. doi: 10.2176/nmc.51.136. [DOI] [PubMed] [Google Scholar]
- 5.Walid MS, Grigorian AA. Ethmo-spheno-intracranial Rosai-Dorfman disease. Indian J Cancer. 2010;47:80–1. doi: 10.4103/0019-509X.58870. [DOI] [PubMed] [Google Scholar]
- 6.Andriko JA, Morrison A, Colegial CH, Davis BJ, Jones RV. Rosai-Dorfman disease isolated to the central nervous system: A report of 11 cases. Mod Pathol. 2001;14:172–8. doi: 10.1038/modpathol.3880278. [DOI] [PubMed] [Google Scholar]
- 7.Wu M, Anderson AE, Kahn LB. A report of intracranial Rosai-Dorfman disease with literature review. Ann Diagn Pathol. 2001;5:96–102. doi: 10.1053/adpa.2001.23027. [DOI] [PubMed] [Google Scholar]
- 8.Kattner KA, Stroink AR, Roth TC, Lee JM. Rosai-Dorfman disease mimicking parasagittal meningioma: case presentation and review of the literature. Surg Neurol. 2000;53:452–7. doi: 10.1016/s0090-3019(00)00197-x. discussion 457. [DOI] [PubMed] [Google Scholar]
- 9.Kumar R, Singhal U, Kumar Mahapatra A. Intracranial Rosai-Dorfman syndrome: Case Review. Pan Arab J Neurosurg. 2011;15:58–63. [Google Scholar]
- 10.Hollowell JP, Wolfla CE, Shah NC, Mark LP, Whittaker MH. Rosai-Dorfman disease causing cervical myelopathy. Spine (Phila Pa 1976) 2000;25:1453–6. doi: 10.1097/00007632-200006010-00020. [DOI] [PubMed] [Google Scholar]
- 11.Huang HY, Liang CL, Yang BY, Sung MT, Lin JW, Chen WJ. Isolated Rosai-Dorfman disease presenting as peripheral mononeuropathy and clinically mimicking a neurogenic tumor. Surg Neurol. 2001;56:344–7. doi: 10.1016/s0090-3019(01)00577-8. [DOI] [PubMed] [Google Scholar]
- 12.Raslan O, Ketonen LM, Fuller GN, Schellingerhout D. Intracranial Rosai-Dorfman Disease with Relapsing Spinal Lesions. J Clin Oncol. 2008;26:3087–9. doi: 10.1200/JCO.2007.15.7701. [DOI] [PubMed] [Google Scholar]
- 13.Deshpande AH, Nayak S, Munshi MM. Cytology of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) Diagn Cytopathol. 2000;22:101–5. doi: 10.1002/(sici)1097-0339(20000301)22:3<181::aid-dc10>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 14.Lee-Wing M, Oryschak A, Attariwala G, Ashenhurst M. Rosai-Dorfman disease presenting as bilateral lacrimal gland enlargement. Am J Ophthalmol. 2001;131:677–8. doi: 10.1016/s0002-9394(00)00864-3. [DOI] [PubMed] [Google Scholar]
- 15.Di Rocco F, Garnett MR, Puget S, Pueyerredon F, Roujeau T, Jaubert F, et al. Cerebral localization of Rosai-Dorfman disease in a child. J Neurosurg. 2007;107(2 Suppl):147–51. doi: 10.3171/PED-07/08/147. [DOI] [PubMed] [Google Scholar]
- 16.Jurić G, Jakić-Razumović J, Rotim K, Zarković K. Extranodal sinus histiocytosis (Rosai-Dorfman disease) of the brain parenchyma. Acta Neurochir (Wien) 2003;145:145–9. doi: 10.1007/s00701-002-1031-5. discussion 149. [DOI] [PubMed] [Google Scholar]
- 17.Hinduja A, Aguilar LG, Steineke T, Nochlin D, Landolfi JC. Rosai-Dorfman disease manifesting as intracranial and intraorbitallesion. J Neurooncol. 2009;92:117–20. doi: 10.1007/s11060-008-9733-z. [DOI] [PubMed] [Google Scholar]
- 18.McClain KL, Natkunam Y, Swerdlow H. Atypical cellular disorders. Hematology Am Soc Hematol Educ Program. 2004;1:283–96. doi: 10.1182/asheducation-2004.1.283. [DOI] [PubMed] [Google Scholar]


