Abstract
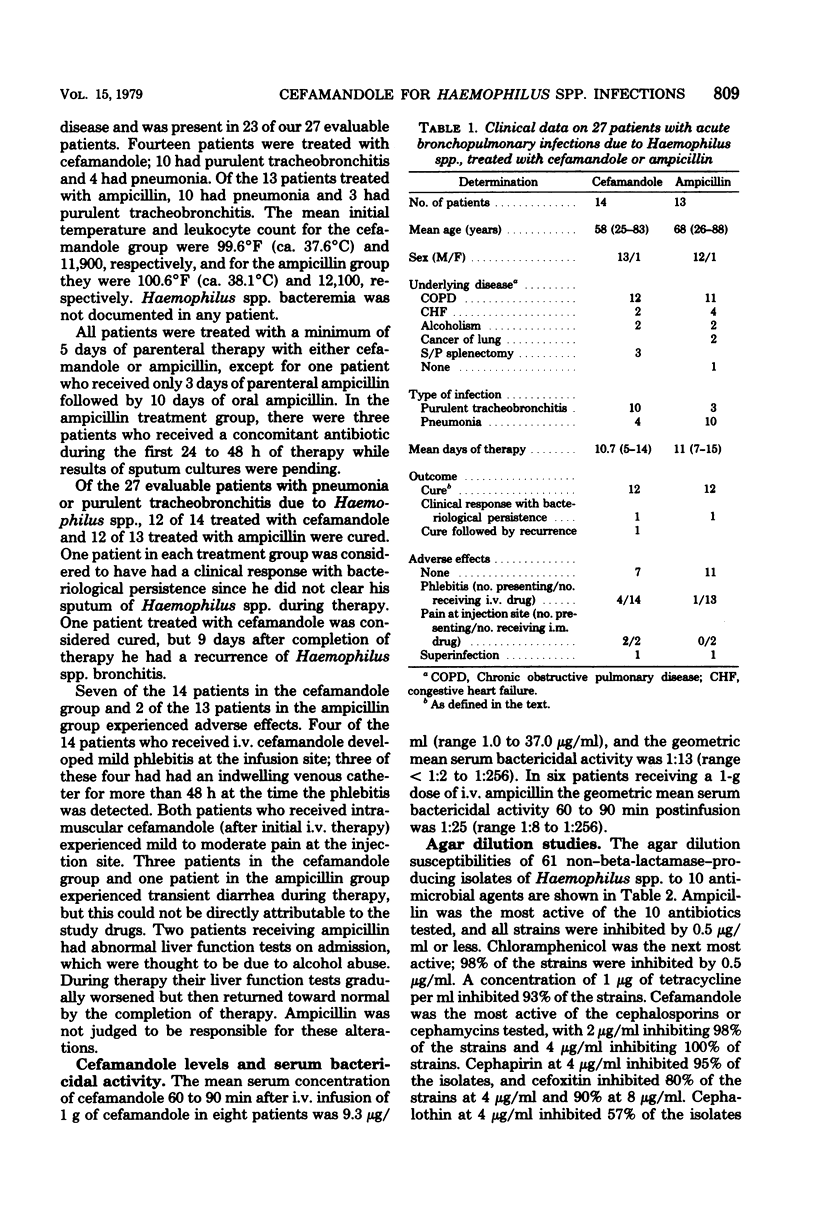
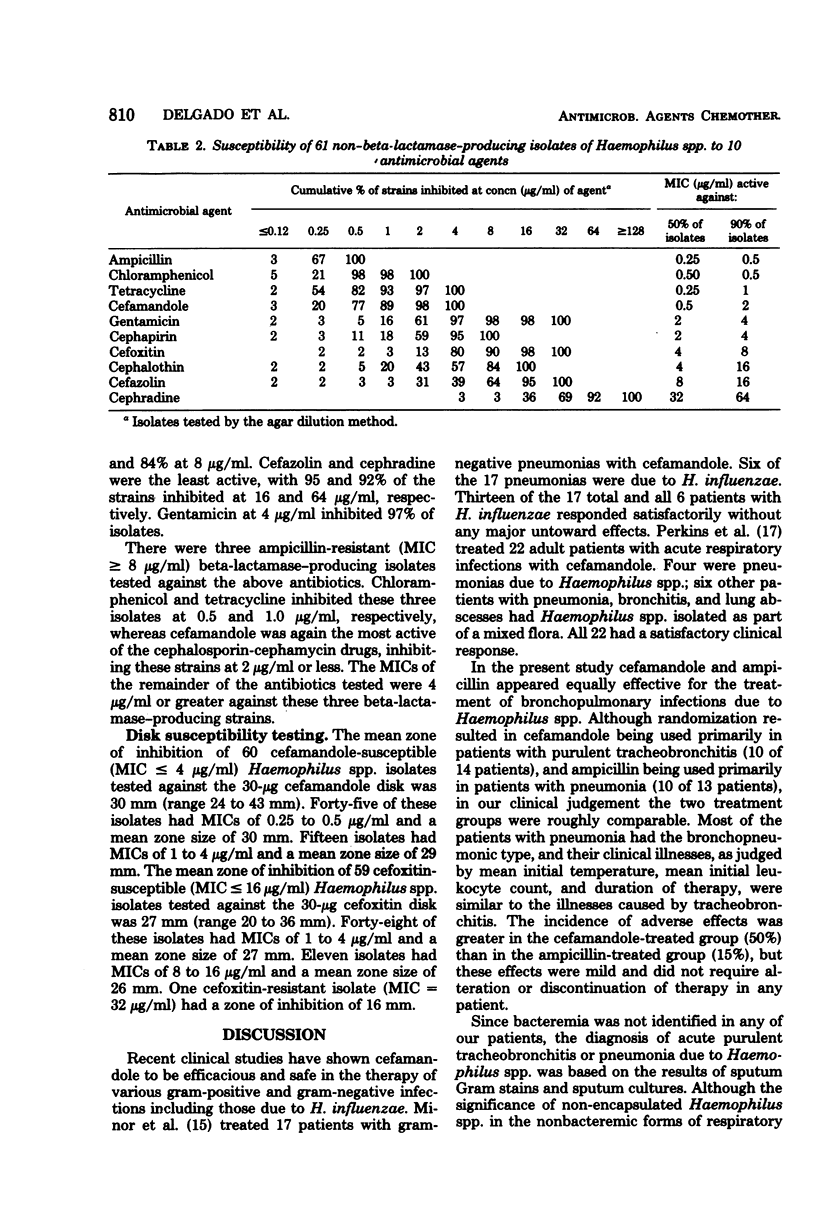
A prospective, randomized, single-blind comparison of parenteral cefamandole and ampicillin was conducted in 27 hospitalized adult patients with pneumonia or purulent tracheobronchitis due to Haemophilus spp. Patients received either parenteral cefamandole or ampicillin in a dose of 1 g every 6 h. Cefamandole was as effective and safe as ampicillin. Of the 14 patients treated with cefamandole, 13 were considered cured, as were 12 of the 13 treated with ampicillin. One patient in each treatment group improved clinically but did not clear his sputum of Haemophilus spp. One patient treated with cefamandole had a recurrence of Haemophilus spp. bronchitis 9 days after cure. Adverse effects were more common in the cefamandole-treated group (50% versus 15%), but were mild and did not require discontinuation of therapy in any patient. The in vitro susceptibilities of 64 clinical isolates of Haemophilus spp. to 10 antibiotics were determined. Cefamandole was the most active of the cephalosporin-cephamycin antibiotics tested, inhibiting 98% of 61 non–beta–lactamase–producing isolates at 2 μg/ml and 100% at 4 μg/ml. Cefamandole inhibited the three ampicillin-resistant isolates at 2 μg/ml or less. Cephapirin, cefoxitin, and cephalothin were the next most active, whereas cefazolin and cephradine were the least active.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Azimi P. A. Clinical and laboratory investigation of cefamandole in infections of infants and children. Antimicrob Agents Chemother. 1978 Jun;13(6):955–957. doi: 10.1128/aac.13.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett J. V., Brodie J. L., Benner E. J., Kirby W. M. Simplified, accurate method for antibiotic assay of clinical specimens. Appl Microbiol. 1966 Mar;14(2):170–177. doi: 10.1128/am.14.2.170-177.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas R. M., Devitt L. Pneumonia in New Guinea. I. Bacteriological findings in 632 adults with particular reference to haemophilus influenzae. Med J Aust. 1973 Jan 13;1(2):42–49. [PubMed] [Google Scholar]
- Everett E. D., Rham A. E., Jr, Adaniya R., Stevens D. L., McNitt T. R. Haemophilus influenzae pneumonia in adults. JAMA. 1977 Jul 25;238(4):319–321. [PubMed] [Google Scholar]
- Griffith R. S., Black H. R., Brier G. L., Wolny J. D. Cefamandole: in vitro and clinical pharmacokinetics. Antimicrob Agents Chemother. 1976 Nov;10(5):814–823. doi: 10.1128/aac.10.5.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson J. A., McCormick J. B., Hayes P., Thornsberry C., Kirvin L. Epidemiologic characteristics of infections caused by ampicillin-resistant Hemophilus influenzae. Pediatrics. 1976 Sep;58(3):388–391. [PubMed] [Google Scholar]
- Jorgensen J. H., Alexander G. A. Comparative activities of selected beta-lactam antibiotics against Haemophilus influenzae. Antimicrob Agents Chemother. 1978 Feb;13(2):342–343. doi: 10.1128/aac.13.2.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan W., Ross S., Rodriguez W., Controni G., Saz A. K. Haemophilus influenzae type B resistant to ampicillin. A report of two cases. JAMA. 1974 Jul 15;229(3):298–301. [PubMed] [Google Scholar]
- King G., James J. F., Swanson J. Studies on gonococcus infection. XI. Comparison of in vivo and vitro association of Neisseria gonorrhoeae with human neutrophils. J Infect Dis. 1978 Jan;137(1):38–43. doi: 10.1093/infdis/137.1.38. [DOI] [PubMed] [Google Scholar]
- Levin D. C., Schwarz M. I., Matthay R. A., LaForce F. M. Bacteremic hemophilus influenzae pneumonia in adults. A report of 24 cases and a review of the literature. Am J Med. 1977 Feb;62(2):219–224. doi: 10.1016/0002-9343(77)90317-5. [DOI] [PubMed] [Google Scholar]
- Manten A., van Klingeren B., Dessens-Kroon M. Chloramphenicol resistance in Haemophilus influenzae. Lancet. 1976 Mar 27;1(7961):702–702. doi: 10.1016/s0140-6736(76)92832-4. [DOI] [PubMed] [Google Scholar]
- Minor M. R., Sande M. A., Dilworth J. A., Mandell G. L. Cefamandole treatment of pulmonary infection caused by gram-negative rods. J Antimicrob Chemother. 1976 Mar;2(1):49–53. doi: 10.1093/jac/2.1.49. [DOI] [PubMed] [Google Scholar]
- O'Callaghan C. H., Morris A., Kirby S. M., Shingler A. H. Novel method for detection of beta-lactamases by using a chromogenic cephalosporin substrate. Antimicrob Agents Chemother. 1972 Apr;1(4):283–288. doi: 10.1128/aac.1.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomeh M. O., Starr S. E., McGowan J. E., Jr, Terry P. M., Nahmias A. J. Ampicillin-resistant Haemophilus influenzae type B infection. JAMA. 1974 Jul 15;229(3):295–297. [PubMed] [Google Scholar]
- Ward J. I., Tsai T. F., Filice G. A., Fraser D. W. Prevalence of ampicillin- and chloramphenicol-resistant strains of Haemophilus influenzae causing meningitis and bacteremia: national survey of hospital laboratories. J Infect Dis. 1978 Sep;138(3):421–424. doi: 10.1093/infdis/138.3.421. [DOI] [PubMed] [Google Scholar]


