Abstract
Methadone and buprenorphine are both efficacious treatments for opioid dependency, but they also have different pharmacological properties and clinical delivery methods that can affect their acceptability to patients. This study was intended to increase our knowledge of heroin-dependent individuals’ perceptions of methadone vs. buprenorphine maintenance based on actual experiences with each. The study sample consists of heroin-dependent men at the Rikers Island jail in New York City who were voluntarily randomly assigned to methadone or buprenorphine maintenance in jail. Methadone patients were more likely to report feeling uncomfortable the first few days, having side/withdrawal effects during treatment, and being concerned about continued dependency on medication after release. In contrast, buprenorphine patients’ main issue was the bitter taste. All of the buprenorphine patients stated that they would recommend the medication to others, with almost all preferring it to methadone. Ninety-three percent of buprenorphine vs. 44 percent of methadone patients intended to enroll in those respective treatments after release, with an added one-quarter of the methadone patients intending to enroll in buprenorphine instead. These results reinforce the importance of increasing access to buprenorphine treatment in the community for indigent heroin-dependent offenders.
Keywords: Buprenorphine treatment, Methadone treatment, Prisoners, Patient satisfaction
INTRODUCTION
Research and clinical experience have shown that methadone and buprenorphine are both highly efficacious treatments for chronic heroin dependency (e.g., Johnson et al., 1992; 2000). However, heroin-dependent individuals generally (Brown et al., 1975; Jansen et al., 1974; Hunt et al., 1985; Goldsmith, 1984; Zweben and Sorenson, 1988; Zule and Desmond, 1998; Stancliff et al., 2002) and among them, offenders and minorities in particular (Rosenblum et al., 1991; Zaller et al., 2009), express ambivalence about long-term methadone maintenance, including bone decalcification, overdosing, side effects, difficulties in withdrawing from the medication, and its persistent social stigma. Such beliefs and attitudes can adversely affect retention in methadone treatment (Kayman et al., 2006; Stancliffe et al., 2002; Rosenblum et al, 1991).
Buprenorphine treatment was introduced in the U.S. in 2002 and has the potential to avoid similar perceptions. First, buprenorphine’s pharmacologic profile as a partial mu-agonist indicates lesser agonist effects, such as respiratory depression, sedation and constipation, and milder medication withdrawal as compared with methadone (Center for Substance Abuse Treatment, 2004). Second, induction to buprenorphine may take place in a primary care setting and the medication may be obtained by up to a 30 day prescription, similar to other medicines. In contrast, the process of methadone delivery requires dedicated clinics with inconvenient restrictions and which concentrate methadone patients at one location, increasing the possibility of stigmatization(Madden et al., 2008; Stancliff et al., 2002).
The literature on patients’ perceptions of and satisfaction with buprenorphine maintenance as compared with methadone maintenance treatment is still limited. Several studies have compared side effects between patients randomly assigned to buprenorphine or methadone. Petitjean et al. (2001), Pani et al. (2000), Mattick et al. (2003) and Johnson et al. (2000) found no differences in numbers of side effects, except that: buprenorphine patients reported more serious headaches and less sedation (Petitjean et al., 2001); buprenorphine patients reported more depression and less constipation and insomnia (Pani et al., 2000); and methadone patients reported more of a “buzz” and “liking” their medication better (Mattick et al., 2003).
Studies comparing perceptions of opioid-dependent individuals regarding other aspects of buprenorphine and methadone treatment are rare. Schwartz et al. (2008) asked methadone maintenance patients and out-of-treatment opioid-dependent individuals about their attitudes to methadone and buprenorphine treatment; both groups had significantly more positive attitudes towards buprenorphine. However, it is unclear to what extent the subjects’ perceptions of buprenorphine were based on actual experience with that medication; indeed, the study found evidence that a “high percentage in both groups had not yet fully formed their thinking about buprenorphine.”
The current study is intended to increase our knowledge of heroin-dependent individuals’ satisfaction with and perceptions of buprenorphine maintenance vs. methadone maintenance, based on the actual experiences of similar individuals receiving these alternative medication-assisted treatments. This could assist in better understanding of the advantages and disadvantages of each treatment as experienced by patients and could help to improve the acceptability of these efficacious treatments.
METHODS
Setting
The setting of the study was the Key Extended Entry Program (KEEP) within the Rikers Island jail complex in New York City. KEEP provides methadone maintenance to eligible inmates who are opioid dependent. Eligibility requires a sentence of no more than one year of jail time or being detained in jail on legal charges that will not result in a jail sentence of more than 1 year, if convicted. KEEP clients receive referrals to participating community methadone programs at the time of their release (Tomasino et al., 2001).
Procedures
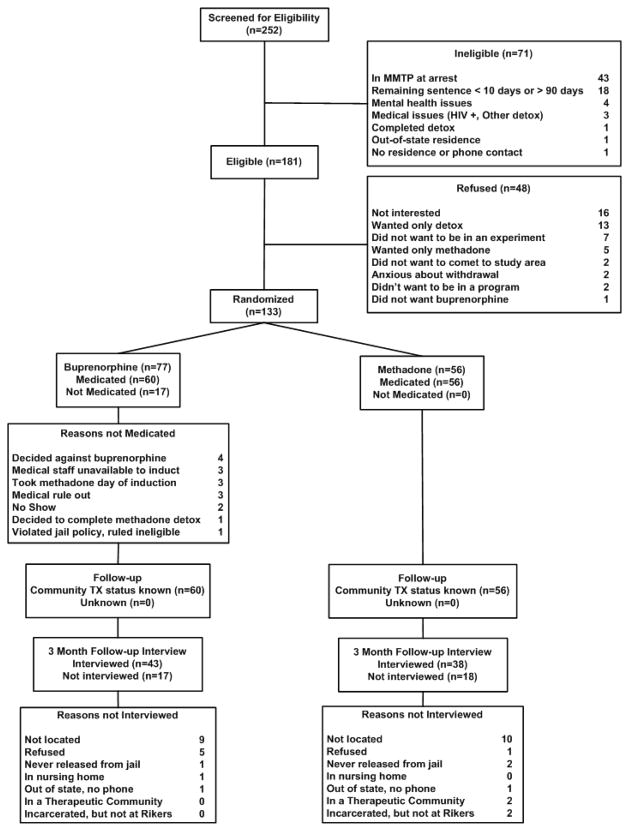
All inmates admitted to Rikers are evaluated for opioid dependence by KEEP intake staff and are prescribed methadone to treat their withdrawal symptoms. Those who are also legally eligible are offered methadone maintenance. The parent study was a short-term clinical trial of buprenorphine that voluntarily randomly assigned inmates to either maintenance with methadone (the standard of care at Rikers) or with buprenorphine (SuboxoneR, the buprenorphine/naloxone formulation) while in jail, followed with referrals to those respective treatments in the community after release. The clinical trial was open label. Within each study condition, dosage was set by agreement between the physician and the patient. In the methadone condition, patients could choose step-up to 30 mg or 70 mg. In the buprenorphine condition, the initial dosage was 4 mg but could potentially be stepped up to a maximum of 32 mg. None of the study subjects were receiving methadone or buprenorphine treatment at arrest. Subject flow is indicated in Figure 1. Additional details of the study procedures have been published previously, as have the outcomes of the clinical trial (Magura et al., 2009). The study was conducted in a men’s facility at Rikers between August 2006 and January 2008. At the time of the study the New York City Department of Health and Mental Hygiene, the agency responsible for providing medical services at Rikers, did not have the resources to introduce buprenorphine to the women’s facility.
Figure 1.
CONSORT diagram
The clinical trial was approved by the Institutional Review Boards ofNational Development and Research Institutes, Inc. and the NYC Department of Health and Mental Hygiene. The ClinicalTrials.gov identifier is NCT00367302.
Measures
Among other data collected, the study conducted an exit interview with subjects immediately prior to their release from jail; this provides the data for the present analysis. The exit interview was conducted with all but two patients in the clinical trial, both in the methadone group, resulting in a sample of 54 methadone and 60 buprenorphine patients for this analysis.
Side/withdrawal effects of medication
Patients were asked whether the medication gave them 18 specific side and opioid withdrawal effects. The listed symptoms were: sedation, nausea and/or vomiting, dizziness, sweating, confusion, blurred vision, dry mouth, fatigue and/or weakness, slurred speech, nervousness/malaise, depression, constipation, hot flushes, diarrhea, chills, ringing in ears, low libido and loss of appetite. A side/withdrawal effects index was computed by counting the number of side/withdrawal effects reported by each subject.
Perceived benefits of medication
Patients were asked to respond to three specific items pertinent to opioid agonist therapy: “It took away my hunger for heroin; it kept me from getting sick from withdrawal; it got me straight.” The responses were a 5-point Likert scale from “strongly agree” to “strongly disagree.”
Perceived drawbacks of medication or its delivery
Patients were asked to respond to two specific items that could apply to both medications: “I was uncomfortable the first few days; I didn’t like being watched while I took it.”
Most favorable feature of treatment
Patients were asked, ”what did you like most about the (methadone or buprenorphine) treatment you received?” Their verbatim answers were recorded; only one response could be given.
Least favorable feature of treatment
Patients were asked, “what did you like least about the (methadone or buprenorphine) treatment you received?” Their verbatim answers were recorded; only one response could be given.
Recommendation of buprenorphine and reasons for recommendation
Patients in the buprenorphine group were asked whether they “would recommend buprenorphine to others” and if so, why they would recommend it.
Evaluation of buprenorphine vs. methadone by buprenorphine patients
Those buprenorphine patients who also had prior experience with methadone maintenance either in the community or in jail were asked to compare their experiences with each medication on three structured items, each prefaced by: “How much do you agree with this statement regarding how bupernophine compares with methadone treatment? Buprenorphine holds me better; bupernorphine treatment is more convenient; with buprenorphine, its harder to continue using heroin.” The responses were obtained on a 5-point Likert scale from “strongly agree” to “strongly disagree.”
Intention to enroll in continuing community treatment
Patients were asked whether they intended to go to the (methadone or buprenorphine) program in the community to which they were referred, and if not, why not? Their verbatim answers were recorded.
Data Reduction and Analysis
Responses to the open-ended response questions were categorized and summarized using thematic coding (Coffey and Atkinson, 1996). We anticipated some themes based on previous research and experience with the study population, augmented by additional themes that emerged during individual inspection of the narrative responses. The process continued until no new themes were identified. Similar themes were aggregated into broader categories. Once the final set of categories was established for each open-ended question, the data were coded for all subjects.
Comparisons of buprenorphine vs. methadone subjects were conducted by the difference of means test for continuous data and Fisher’s Exact Test for 2 X 2 contingency tables, the latter using the method of summing small p-values. Since the analyses were exploratory, no corrections for multiple comparisons were made. Statistical significance was set at p < .05 (2-sided).
RESULTS
Sample chararactistics (Table 1)
Table 1.
Baseline Characteristics by Treatment Condition
| Buprenorphine (n=60) | Methadone (n=54) | |
|---|---|---|
| Black (%) | 25 | 26 |
| Hispanic (%) | 65 | 61 |
| Employed full- or part-time (%) | 35 | 50 |
| High school graduate/GED (%) | 72 | 65 |
| Homeless at arrest (%) | 10 | 17 |
| Incident arrest – property crime (%) | 45 | 54 |
| Incident arrest – drug-related (%) | 37 | 33 |
| Age in years (mean, sd) | 38.4 (7.9) | 40.8 ( 9.2) |
| Arrests as adult (mean, sd) | 22.3 (16.2) | 21.8 (18.5) |
| Heroin Use, No. Days in Last 30 Before Jail | 27.9 (6.5) | 28.6 (4.8) |
The sample was predominantly minority group with an average age of about 40 years. About two-thirds graduated from high school or received a GED and about two-fifths were employed full- or part-time at arrest. Property crimes were the most common reason for the incident arrest with drug-related offenses second. The sample’s arrest history was substantial, an average of about 22 arrests during adulthood. Near daily heroin use was typical. There were no statistically significant differences between the buprenorphine and methadone groups on these background characteristics at admission to treatment.
Medication delivery in jail
Eighty-two percent of buprenorphine and 75% of methadone patients completed their assigned treatment while in jail; this difference was not significant. The median medication doses at release, for those not withdrawn from medication before release, were 12 mg/day of buprenorphine (range 4–20 mg) and 30 mg/day of methadone (range 10–70 mg, with a large majority at exactly 30 mg. Although methadone patients had a choice of 30 mg or 70 mg maintenance doses, almost all chose 30 mg, stating that they wanted to avoid the risk of severe withdrawal if they did not continue methadone treatment after release. Methadone patients were in treatment at Rikers significantly longer than buprenorphine patients (31.8 vs. 23.2 days), but the difference became non-significant when administratively discharged patients were excluded from the comparison (Magura et al., 2009).
Side/withdrawal effects of medication
The scale means and standard deviations for the methadone and buprenorphine groups, respectively, were: 1.87 (3.63 ) vs. 0.78 (2.03), t=12.8, df=112, P<.001, indicating that methadone patients reported significantly more side/withdrawal effects on average than buprenorphine patients. Individual side/withdrawal effects that were significantly more frequent among methadone patients were depression (P < .01), constipation (P <.01), confusion (P <.01) and fatigue/weakness (P <.05).
Perceived benefits of medication
High percentages (90% or more) of both medication groups agreed that the medications relieved their cravings for heroin and prevented most opioid withdrawal symptoms.
Perceived drawbacks of medication or its delivery
Significantly more methadone than buprenorphine patients agreed with the statement, “I was uncomfortable the first few days” (85% vs. 53%, P <.001). In heroin users’ parlance, this usually refers to experiencing some symptoms of opioid withdrawal. Significantly more methadone than buprenorphine patients agreed with the statement, “I didn’t like being watched while I took it” (43% vs. 20%, P<.01).
Most favorable feature of treatment
The thematic coding of these open-ended responses resulted in seven categories:
Alleviates withdrawal symptoms (stops from getting sick or gets straight; includes feeling comfortable or normal)
Alleviates craving (stops craving or drug hunger).
No side effects (no nodding, no high, etc.)
Likes KEEP services or how treated by staff
Prefers current medication to the alternative (whether methadone or buprenorphine)
“Nothing” or no answer
Table 2 compares these responses for the two medication groups. The most common response was that the treatment alleviates withdrawal symptoms, which was mentioned significantly more often by methadone patients. The next most frequent responses were that the treatment alleviates craving (mentioned equally by both groups), that there were no side effects (mentioned more frequently by the buprenorphine group); that they liked the KEEP program (mentioned more frequently by the methadone group), and that they preferred buprenorphine to methadone treatment (mentioned more frequently by the buprenorphine group).
Table 2.
Most Liked Feature of Treatment* (in percent)
| Buprenorphine (n=60) | Methadone (n=54) | P | |
|---|---|---|---|
| Alleviates withdrawal | 42 | 61 | <.05 |
| Alleviates craving | 22 | 13 | n.s. |
| No side effects | 23 | 0 | <.001 |
| Likes KEEP services | 0 | 19 | <.001 |
| Prefers current medication | 12 | 0 | <.01 |
| Nothing or no answer | 2 | 7 | n.s. |
Based on coding from verbatim responses.
Least favorable feature of treatment
The thematic coding of these open-ended responses resulted in six categories:
Taste of the medication (“nasty” or “bitter”)
Physical effects (side effects, withdrawal symptoms, nodding, constipation, etc.)
Medication delivery process (for methadone, mainly the “line;” also KEEP and corrections staff attitudes in administering)
Continued drug dependency (staying “hooked;” includes anxiety about after release; having to obtain medication daily)
Other objection (don’t know enough about it; don’t like being watched; stigma, etc.)
Nothing bad to say
Table 3 compares these responses for the two medication groups. The most common response was “the taste,” which was given significantly more frequently by the buprenorphine patients. Methadone patients more often complained about the medication delivery process and the prospect of continued dependency on the medication. There were no significant differences between methadone and buprenorphine patients in mentions of physical effects, other objections or “nothing bad to say.”
Table 3.
Least Liked Feature of Treatment* (in percent)
| Buprenorphine (n=60) | Methadone (n=54) | P | |
|---|---|---|---|
| Taste of medication | 53 | 13 | <.001 |
| Physical effects | 17 | 28 | n.s. |
| Medication delivery | 9 | 30 | <.01 |
| Continued drug dependency | 3 | 20 | <.01 |
| Other objection | 12 | 4 | n.s. |
| Nothing bad to say | 7 | 6 | n.s. |
Based on coding from verbatim responses
Recommendation of buprenorphine and reasons for recommendation
All of the 60 buprenorphine patients stated that they would recommend buprenorphine treatment to others. The thematic coding of open-ended responses to the question of why they would recommend buprenorphine resulted in five categories (up to two answers per subject could be given on this question):
“It works;” e.g., treats the craving; takes away need for heroin or hustling; good treatment (55% of respondents).
Likes its pharmacology better than methadone; e.g., less addictive; fewer side effects; methadone makes you nod or get high; craving persists with methadone; lower dose of buprenorphine effective; buprenorphine makes you feel normal or normally alert ( 55%).
It’s “better” than methadone; no specific reason given (32 %).
Prefers its delivery system to methadone; e.g., prescriptions or don’t need to go every day (17%)
Faster treatment effect; e.g., buprenorphine works faster than methadone and/or lasts longer; can skip a day without getting sick (13 %).
Evaluation of buprenorphine vs. methadone by buprenorphine patients
Thirty-six (60%) of the buprenorphine patients also had prior experience with methadone maintenance either in the community or in jail. They replied to three questions comparing experiences with buprenorphine with methadone as follows: Buprenorphine holds me better” (92% agreed); “bupernorphine treatment is more convenient” (100% agreed); and “with buprenorphine, its harder to continue using heroin” (28% agreed, 3% disagreed, and 69% were neutral).
Intention to enroll in continuing community treatment
At the exit interview 93% of buprenorphine patients vs. 44%of methadone patients said that they intended to enroll in the respective community treatment after release (p<.001); the remainder said “no” or not sure.” Thematic coding of patients’ reasons for replying “no,” of whom 90% were methadone patients, resulted in the following: Desire to avoid continued drug dependency (32%); no perceived need or no treatment desired (23%); wants buprenorphine treatment instead (23%); and other reasons (23%). (Those who responded “not sure” whether they would enroll were not asked to elaborate.)
DISCUSSION
While numerous randomized clinical trials have been conducted investigating the outcomes of buprenorphine vs. methadone treatment, reporting on patients’ experiences and perceptions is almost always limited to drug use, serious adverse events and side effects, rather than satisfaction with treatment and a broader range of opinions about treatment. This study is the first to compare experiences with and perceptions of alternative opioid agonist treatments for individuals in a jail treatment setting who are equivalent on measured and presumably unmeasured baseline characteristics due to their random assignment to treatment. Consequently in this study, their experiences and perceptions are not confounded by differences in the program context or by personal background characteristics, including addiction histories or treatment preferences.
Reports of side/withdrawal effects were infrequent, but did occur more often among the methadone patients. The symptoms reported were indicative of side effects rather than classic symptoms of opioid withdrawal. This is unexpected in view of the modest maintenance dose of methadone (usually 30 mg), but in any event those side effects are consistent with what is documented on methadone.
Differences between the medication groups in what they liked “most” and “least” about treatment are indications of what was most salient, both positively and negatively, to the patients about their treatment. Thus, the fact that methadone patients mentioned alleviation of withdrawal more often than buprenorphine patients does not mean that buprenorphine patients experienced withdrawal symptoms more often. On the contrary, side/withdrawal effects were reported somewhat more frequently by the methadone patients, as mentioned above. Buprenorphine patients valued especially the absence of medication side effects, which may have been salient to them because of presumed prior negative experiences with methadone in that respect. In fact, one out of five buprenorphine patients spontaneously stated that the superiority of buprenorphine to methadone was what they liked most about treatment. No methadone patient stated such a preference for methadone over buprenorphine, but this could be attributed to lack of prior exposure to buprenorphine.
Bitter taste was a complaint for buprenorphine patients, but planned new formulations of the buprenorphine tablet apparently will reduce this, so that this should be less of an issue for buprenorphine treatment in the future. Moreover, it is doubtful that taste alone would dissuade individuals from either buprenorphine or methadone treatment in the community.
The manner in which methadone is delivered in the Rikers jail irritates many methadone patients; they must stand in a long line in the hallway where they can be observed by other inmates as well as correctional staff who pass through. Among other objections, this contributes to revealing the patients as addicts. In contrast, buprenorphine was administered with greater privacy, by having several patients sit in the KEEP clinic waiting room for 5–10 minutes under staff observation while their sublingual tablets dissolved.
The significantly more frequent concern of methadone patients about continued drug dependency with methadone is consistent with the evidence of more difficult drug withdrawal from methadone than from buprenorphine (Gowing and White, 2009; Eklund et al., 1997). This is also in accord with the finding that the methadone patients (who were not in methadone treatment at arrest) preferred the lower dose option at Rikers.
Buprenorphine patients were quite enthusiastic about their treatment; all would recommend it for others and almost all cited numerous ways that they considered it superior to methadone treatment, with which the majority had personal past experience. It is significant that these responses were spontaneous, not prompted.
There was a dramatic difference in methadone vs. buprenorphine patients’ intentions to continue in those respective treatments after release, with almost all of the buprenophine patients but less than half of the methadone patients intending to enroll. This is consistent with the buprenorphine patients’ stated reasons for enthusiasm about that medication. These intentions were also predictive of actual enrollment in methadone and buprenorphine treatment after release, as reported in our previous paper (Magura et al., 2009). One-quarter of the methadone patients who did not intend to enroll in methadone treatment said they preferred to enroll in buprenorphine treatment. Further, one-third of these methadone patients were concerned about continuing drug dependency, a recurring theme for these patients, which again is consistent with pharmacological evidence of a milder withdrawal profile for buprenorphine as compared with methadone.
Limitations of the Study
The setting of the study was a jail-based treatment program in New York City. It is unknown whether the results would be generalizable to heroin-dependent offenders in jail in other locations.
The findings could be affected by the fact that the typical 30 mg methadone dose in this study is a suboptimal dose for most patients, whereas the average buprenorphine dose of 12 mg is about the usual clinical dose.
The study focused on the physiological and subjective effects of the two medications as experienced or perceived by patients. While these are important factors in the acceptability of any medication, there are also differences in the manner that these medications can be delivered in the community (e.g., clinic-based vs. office-based) that were not explicitly queried and could also significantly affect the acceptability of these medications to patients.
CONCLUSION
The reluctance of out-of-treatment heroin-dependent offenders at Rikers to enroll and remain in community methadone treatment after release has been a chronic problem (Rosenblum et al., 1991; Magura et al., 1993). The study helps to better understand the reasons why offenders are more likely to enroll in buprenorphine than in methadone treatment in the community after their release. The high level of acceptability of buprenorphine treatment to heroin-dependent offenders who actually experience such treatment indicates the importance of increasing access to buprenorphine in the community for indigent offenders after incarceration (cf. Barry et al., 2007).
Footnotes
The study was funded by grant no. R21 DA020583 from the National Institute on Drug Abuse.
References
- Barry DT, Moore BA, Pantalon MV, Chawarski MC, Sullivan LE, O’Connor PG, Schottenfeld RS, Fiellin DA. Patient satisfaction with primary care office-based buprenorphine/naloxone treatment. Journal of General Internal Medicine. 2007;22 (2):242–5. doi: 10.1007/s11606-006-0050-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BS, Benn GJ, Jansen DR. Methadone maintenance: Some client opinions. American Journal of Psychiatry. 1975;132:623–626. doi: 10.1176/ajp.132.6.623. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Treatment Improvement Protocol (TIP) Series 40 DHHS Publication No (SMA) 04-3939. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. [PubMed] [Google Scholar]
- Coffey A, Atkinson P. Making Sense of Qualitative Data. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Eklund C, Hiltunen AJ, Melin L, Borg S. Abstinence fear in methadone maintenance withdrawal: a possible obstacle for getting off methadone. Substance Use & Misuse. 1997;32 (6):779–92. doi: 10.3109/10826089709039377. [DOI] [PubMed] [Google Scholar]
- Gowing L, Ali R, White JM. Buprenorphine for the management of opioid withdrawal. Cochrane Database Systematic Review. 2009;8(3):CD002025. doi: 10.1002/14651858.CD002025.pub4. [DOI] [PubMed] [Google Scholar]
- Goldsmith DS, Hunt DE, Lipton DS, Strug DL. Methadone folklore: Beliefs about side effects and their impact on treatment. Human Organization. 1984;43 (4):330–340. [Google Scholar]
- Hunt DE, Lipton DS, Goldsmith DS, Strug DL, Spunt B. It takes your heart: The image of methadone maintenance in the addict world and its effect on recruitment into treatment. International Journal of Addiction Research. 1985;20:1751–71. doi: 10.3109/10826088509047261. [DOI] [PubMed] [Google Scholar]
- Jansen DR, Brown BS, Bass UF. Comparison of attitudes and beliefs about methadone of clients retained and lost to treatment. Drug Forum. 1974;3:215–223. [Google Scholar]
- Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. JAMA. 1992;267 (20):2750–5. [PubMed] [Google Scholar]
- Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE. A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. New England Journal of Medicine. 2000;343:1290–7. doi: 10.1056/NEJM200011023431802. [DOI] [PubMed] [Google Scholar]
- Kayman DJ, Goldstein MF, Deren S, Rosenblum A. Predicting treatment retention with a brief “Opinions about Methadone” scale. Journal of Psychoactive Drugs. 2006;38:93–100. doi: 10.1080/02791072.2006.10399832. [DOI] [PubMed] [Google Scholar]
- Madden A, Lea T, Bath N, Winstock AR. Satisfaction guaranteed? What clients on methadone and buprenorphine think about their treatment. Drug Alcohol Review. 2008;27 (6):671–8. doi: 10.1080/09595230801935706. [DOI] [PubMed] [Google Scholar]
- Magura S, Rosenblum A, Lewis C, Joseph H. The effectiveness of in-jail methadone maintenance. Journal of Drug Issues. 1993;23(1):75–99. [Google Scholar]
- Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, Rosenblum A. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Dependence. 2009;99 (1–3):222–30. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Ali R, White J, O’Brien S, Wolk S, Danz C. Buprenorphine versus methadone maintenance therapy: A randomized double-blind with 405 opioid-dependent patients. Addiction. 2003;98:441–52. doi: 10.1046/j.1360-0443.2003.00335.x. [DOI] [PubMed] [Google Scholar]
- Pani PP, Maremmani I, Pirastu R, Tagliamonte A, Gessa GL. Buprenorphine: A controlled trial in the treatment of opioid dependence. Drug and Alcohol Dependence. 2000;60:39–50. doi: 10.1016/s0376-8716(99)00140-4. [DOI] [PubMed] [Google Scholar]
- Petitjean S, Stohler R, Deglon JJ, Livoti S, Waldvogel D, Uehlinger C, et al. Double-blind randomized trial of buprenorphine and methadonein opiate dependence. Drug and Alcohol Dependence. 2001;62:97–104. doi: 10.1016/s0376-8716(00)00163-0. [DOI] [PubMed] [Google Scholar]
- Rosenblum A, Magura S, Joseph H. Ambivalence toward methadone treatment among intravenous drug users. Journal of Psychoactive Drugs. 1991;23:21–7. doi: 10.1080/02791072.1991.10472571. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Mitchell SG, Peterson JA, Reisinger HS, Agar MH, Brown BS. Attitudes toward buprenorphine and methadone among opioid-dependent individuals. American Journal of Addiction. 2008;17 (5):396–401. doi: 10.1080/10550490802268835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stancliff S, Myers JE, Steiner S, Drucker E. Beliefs about methadone in an inner-city methadone clinic. Journal of Urban Health. 2002;79:571–578. doi: 10.1093/jurban/79.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasino V, Swanson AJ, Nolan J, Shuman H. The Key Extended Entry Program (KEEP): a methadone treatment program for opiate-dependent inmates. Mt Sinai Journal of Medicine. 2001;68:14–20. [PubMed] [Google Scholar]
- Zaller ND, Bazazi AR, Velazquez L, Rich JD. Attitudes toward methadone among out-of-treatment minority injection drug users: implications for health disparities. International Journal on Environmental Research and Public Health. 2009;6 (2):787–97. doi: 10.3390/ijerph6020787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zule WA, Desmond DP. Attitudes toward methadone maintenance: Implications for HIV prevention. Journal of Psychoactive Drugs. 1998;301:89–97. doi: 10.1080/02791072.1998.10399674. [DOI] [PubMed] [Google Scholar]
- Zweben JE, Sorensen JL. Misunderstandings about methadone. Journal of Psychoactive Drugs. 1988;20:275–281. doi: 10.1080/02791072.1988.10472498. [DOI] [PubMed] [Google Scholar]