Abstract
Clinically severe or morbid obesity (BMI over 40 or 50) entails far more serious health consequences than moderate obesity for patients and creates additional challenges for providers. The paper provides time trends for extreme weight categories (BMI>40 and >50) until 2010 using data from the Behavioral Risk Factor Surveillance System. Between 2000 and 2010, the prevalence of a BMI over 40 (type III obesity) calculated from self-reported height and weight increased by 70%, the prevalence of BMI over 50 increased even faster. While rates at every point in time are higher among Hispanics and Blacks, there were no significant differences in trends between them or to Non-Hispanic Whites. The growth rate appears to have slowed down since 2005. Adjusting for self-report biases, we estimate that in 2010 15.5 million adult Americans or 6.6 percent of the population had an actual BMI over 40. The prevalence of clinically severe obesity continues to be increasing, although less rapidly in more recent years than prior to 2005.
Keywords: Morbid obesity, epidemiology, BRFSS, prevalence
INTRODUCTION
Over the last 3 decades, mean body-mass index (BMI) has increased by 0.4 kg/m2 per decade worldwide.1 According to recent studies, the US has the highest mean BMI among high income countries,1 resulting in 1 in 3 adults having a BMI over 30 based on objective measurement2 or 1 in 4 adults based on self-reported height and weight.3 The prevalence of (moderate) obesity may be stabilizing or at least increases are occurring at much smaller rates than prior to 2005 in the US.2–4 This plateauing may or may not apply to more severe/morbid obesity (any BMI cutpoint over 40). Few trend estimates exist for morbid obesity because surveys using objective measurements lack the sample size, while surveys using self-reported height and weight require a different interpretation of cut points for prevalence estimates. Between 1986 and 2000, when the prevalence of a BMI over 30 based on self-reported height and weight roughly doubled, the prevalence of a BMI of 40 quadrupled and the prevalence of a BMI of 50 or greater quintupled.5 This paper provides an update of those trends since 2000.
The typical definition of obesity, a body mass index (BMI) of over 30 (irrespective of whether objectively measured or based on self-report), obscures the heterogeneity among that group. Severely obese individuals who are 100 or 200 pounds (45–90 kg) or more overweight have on average far more complex health issues and encounter very different challenges in the health care system than the majority of (moderately) obese individuals (BMI 30–35). Physician offices and hospitals require additional resources for severely obese patients, who exceed limits on standard measuring and lifting equipment and may not fit standard imaging equipment, operating tables, or wheelchairs. It also affects health care personnel and the National Institute for Occupational Safety and Health started a program in 2009 to identify evidence-based best practices for handling severely obese patients to reduce occupational injuries.6
Clinically severe or morbid obesity is not a rare pathological condition afflicting a fixed proportion of the population, nor is it directly coupled to the prevalence of moderate obesity. Instead, severe obesity is part of a population BMI distribution that has become more heterogeneous (a larger proportion of individuals far away from the average) while shifting to the right simultaneously (an increase in mean BMI).7,8 Fast growth of morbid obesity has also been reported in other countries.9 Changes in the prevalence of such severe levels of obesity disproportionately affect morbidity and health care costs because the risks of disease and severity of conditions rapidly and continuously increase with higher BMI levels.10
METHODS
This study analyzes data from the Behavioral Risk Factor Surveillance System (BRFSS), a cross-sectional telephone survey of noninstitutionalized adults, between 1986 and 2010.11
Individuals are classified into weight categories based on the body mass index (BMI) (weight in kilograms divided by the square of height in meters) calculated from self-reported weight and height. In addition to the standard “obese” category, defined as a BMI of greater than or equal to 30 kg/m2, the main groups of interest are more extreme categories: BMI>=40 (type III obesity); and BMI>=50.
Self-report on average understates weight (more so for women) and overstates height (more so for men).12 The underreporting of weight increases with weight and prevalence at the same cutpoints are therefore lower than if BMI were calculated by independent measurement. A cutpoint of 40 for direct measurement would be more comparable with a cutpoint for self-report of 37.3 for men and 37.0 for women based on our calculations using NHANES 2007–2008 (we also show this “adjusted” trend). The effect on relative change trends is relatively minor unless reporting biases change. A diminishing reporting bias over time, possibly due to increased awareness about obesity and increased self-monitoring, would lead to overestimates. We used the NHANES to assess this possibility, but found no evidence for changes in reporting biases between 1999 and 2008. Similarly, Gorber and Tremblay13 report no change over time in self-report bias in the US, although there was an increasing (rather than diminishing) bias in Canada.
The descriptive statistics in Table 1 use sampling weights and adjust standard errors for the BRFSS design. The main statistical analysis underlying Figure 1 uses individual-level logistic regression with an indicator of weight category as the dependent variable. Time trend is measured as a linear spline with knots at 1991, 1996, 2001, and 2006 (i.e., linear trends within each 5-year period, but those slopes can differ between 1986–1990, 1991–1995, 1996–2000, 2001–2005, and 2006–2010). The results are adjusted for sociodemographic changes to isolate the unique trend in obesity rates. Regressors include: age (in 5-year intervals), educational achievement (less than high school, high school, some college, college degree), racial group (white, black, Hispanic, other), and sex. State indicators are included to control for the changing survey participation by states over time. Tests are based on the regression model and all results are statistically significant at p<0.01 unless indicated otherwise. The adjusted results are based on the sociodemographic characteristics in the year 2010 survey. We also estimated separate models stratifying by sex and by race/ethnicity.
Table 1.
The prevalence of different levels of obesity among US adults: 2000–2010
| Equivalent to measured | |||||
|---|---|---|---|---|---|
| Number of observations | BMI> 30 | BMI> 40 | BMI> 50 | BMI> 40 | |
| 2000 | 172,755 | 19.8 (19.1–20.6) | 2.12 (2.00–2.26) | .27 (.23–.31) | 3.90 (3.69–4.11) |
| 2001 | 195,522 | 21.0 (20.2–21.7) | 2.24 (2.05–2.43) | .28 (.23–.32) | 4.21 (3.93–4.49) |
| 2002 | 232,460 | 21.3 (20.3–22.4) | 2.42 (2.24–2.59) | .31 (.27–.35) | 4.45 (4.12–4.78) |
| 2003 | 247,913 | 22.2 (21.9–22.5) | 2.62 (2.50–2.73) | .35 (.31–.39) | 4.85 (4.69–5.01) |
| 2004 | 283,826 | 22.9 (22.6–23.2) | 2.69 (2.58–2.79) | .34 (.30–.37) | 4.91 (4.77–5.07) |
| 2005 | 333,052 | 23.9 (23.6–24.2) | 3.0 (2.88–3.11) | .41 (.36–.45) | 5.30 (5.15–5.44) |
| 2006 | 331,367 | 24.4 (24.1–24.8) | 3.14 (3.01–3.26) | .44 (.40–.48) | 5.50 (5.35–5.57) |
| 2007 | 403,600 | 25.7 (25.4–36.0) | 3.40 (3.28–3.51) | .46 (.42–.51) | 5.98 (5.83–6.13) |
| 2008 | 389,290 | 26.1 (25.8–26.4) | 3.38 (3.27–3.49) | .46 (.42–.50) | 6.10 (5.95–6.25) |
| 2009 | 406,700 | 26.7 (26.4–27.0) | 3.69 (3.57–3.81) | .48 (.44–.52) | 6.41 (6.26–6.57) |
| 2010 | 423,284 | 27.2 (27.0–27.5) | 3.68 (3.56–3.80) | .55 (.50–.60) | 6.55 (6.40–6.70) |
Notes: Descriptive statistics, based on self-reported height and weight in Behavioral Risk Factor Surveillance Survey; 95% confidence interval in parentheses. The last column uses cutpoints BMI>37.3 for men and BMI>37 for women, to make prevalence roughly equivalent to an objectively measured cutpoint of 40.
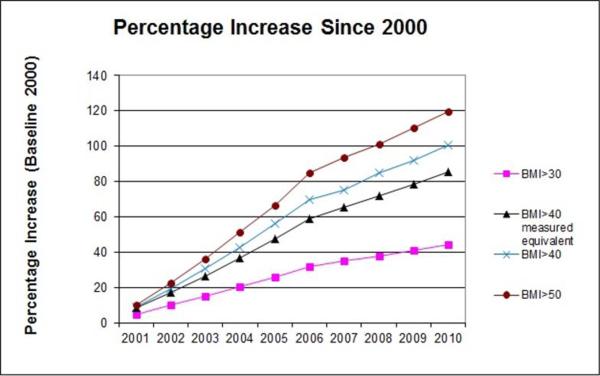
Figure 1. Prevalence growth by severity of obesity (in percent over 1986 baseline).
Notes: Author's calculation based on Behavioral Risk Factor Surveillance Survey, BMI cutpoints calculated based on self-reported height and weight. Adjusted line (squares) uses cutpoint of 37.3 for men and 37.0 for women to make it comparable to BMI>40 calculated from objective height and weight measurement. 200 indicates a 200% increase over baseline, i.e. a tripling of baseline rates.
RESULTS
Figure 1 shows the growth rates since 1986, with 1986 rates as the base. The higher the weight groups, the more rapid the rate of growth. The percentage of the population with a BMI over 50 based on reported height and weight has increased more than 10-fold. The prevalence of extreme BMI levels continues to rise at a fast rate, but there is a noticeable (and statistically significant) slowdown since 2005. This slowdown is recent as there was no difference in the trend pattern between 2001–2005 compared to 1991–1995 or to 1996–2000.
At every point in time, the prevalence of obesity differs across subgroups. For higher levels (BMI>40), it is about 50% higher among women than among men and about double among non-Hispanic black than among Hispanics or non-Hispanic whites (with no major differences between the latter). However, the trend estimates for all groups are very similar – when redrawing Figure 1 using only statistically significant differences, the lines at every BMI level would be indistinguishable across subgroups. For all levels of obesity (regardless of cutpoint), the increases over time are faster among younger age groups (below 35 or 40).
Table 1 provides descriptive statistics for 2000–2010. The final column uses a cutpoint of 37.3 for men and 37 for women with self-reported data, resulting in a prevalence rate comparable to a BMI cutpoint of 40 using objective measurement. That rate increased from 3.9% of the population to 6.6% during the decade, about a 70% increase. A cutpoint of 40 based on self-reported height and weight gives lower rates of prevalence, from 2.1% to 3.7%, but a relative increase of over 70%. There is a general pattern also reflected in Figure 1 over a longer time horizon: The higher the BMI group, the faster the growth rate in prevalence.
DISCUSSION
These trend estimates indicate that morbid obesity rates (at any cutpoint above 40) in the US continue to rise rapidly, although the near exponential growth has noticeably flattened out since 2005. The relative rate of increase is similar across population subgroups, even though the prevalence at every point in time differs across groups.2 The trajectories do not differ across groups, but So rather than having different trajectories, the most disadvantaged group appear to be just a few years ahead of others.
There are at least three limitations in the BRFSS: First, it excludes persons who do not have landline telephones and wireless-only households are more likely to be younger, to be black or Hispanic. Second, response rates have declined over time and the CASRO response rate in many states is now below 50%. The third and most problematic limitation is that height and weight reporting biases may change over time, which could impact the self-reported trend data in this report. Based on NHANES data from 1999–2008, we do not find any significant change in reporting biases, but that could be different for the most severely obese group.
We also use NHANES to calculate cutpoints in self-reported data to correspond to objective measurement for a BMI>40. Using those cutpoints, our prevalence estimates are within the confidence intervals of NHANES estimates for every year, suggesting that NHANES and BRFSS results may actually be more similar than commonly believed. However, because of the much larger sample size, BRFSS estimates a highly significant trend towards continuing increases in severe obesity, even though there has been a slowdown in recent years.
Clinically severe obesity, far from being a pathological condition that only affects a fixed percentage of genetically vulnerable individuals, appears to be an integral part of the US population's weight distribution. The traditional clinical approach of targeting high risk cases is only temporary and palliative in this situation, but cannot stem the trend. While this offers new business opportunities for providers specializing in treating severe obesity, the social and human costs are large.
ACKNOWLEDGEMENTS
This project was supported by grant number grant R01HD057193 from NICHD (RS) and T32 HS000046 from the Agency for Healthcare Research and Quality (AH). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH or the Agency for Healthcare Research and Quality.
Footnotes
Conflict of interest. The authors declare no conflict of interest.
REFERENCES
- 1.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377(9765):557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Vital signs: state-specific obesity prevalence among adult - United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(30):951–955. [PubMed] [Google Scholar]
- 4.Yanovski SZ, Yanovski JA. Obesity prevalence in the United States--up, down, or sideways? N Engl J Med. 2011 Mar 17;364(11):987–989. doi: 10.1056/NEJMp1009229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sturm R. Increases in clinically severe obesity in the US: 1986–2000. Archives of Internal Medicine. 2003;163(18):2146–2148. doi: 10.1001/archinte.163.18.2146. [DOI] [PubMed] [Google Scholar]
- 6.Galinsky T, Hudock S, Streit J. Addressing the need for research on bariatric patient. Rehabil Nurs. 2010;35(6):242–247. doi: 10.1002/j.2048-7940.2010.tb00054.x. [DOI] [PubMed] [Google Scholar]
- 7.Sturm R, Bao Y. Socioeconomics of obesity. In: Kushner RF, Bessesen DH, editors. Treatment of the Obese Patient. Humana Press Inc.; Totowa, NJ: 2007. pp. 174–194. [Google Scholar]
- 8.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288(14):1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 9.Basterra-Gortari FJ, Beunza JJ, Bes-Rastrollo M, et al. Increasing trend in the prevalence of morbid obesity in Spain: from 1.8 to 6.1 per thousand in 14 years. Rev Esp Cardiol. 2011;64(5):424–426. doi: 10.1016/j.recesp.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004 Dec;12(12):1936–1943. doi: 10.1038/oby.2004.243. [DOI] [PubMed] [Google Scholar]
- 11. [Accessed March 22, 2012];Centers for Disease Control, Behavioral Risk Factor Surveillance Survey. homepage at: http://www.cdc.gov/brfss/.
- 12.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 13.Gorber SC, Tremblay MS. The bias in self-reported obesity from 1976 to 2005: a Canada-US comparison. Obesity (Silver Spring) 2010;18(2):354–361. doi: 10.1038/oby.2009.206. [DOI] [PubMed] [Google Scholar]