Abstract
Background
Palliative care education is often lacking in graduate medical education curricula. Studies show that many physicians are uncomfortable discussing end-of-life issues with patients and providing palliative care to dying patients and their families. We used a case-based approach to improve resident confidence in delivering bad news, discussing poor prognoses, explaining the dying process, and providing palliative care in the intensive care unit.
Methods
The medical intensive care unit (MICU) curriculum involved a 3-pronged approach, including role modeling by the attending physician and palliative care team, tutorials, and a case-based debriefing at the end of each month-long rotation. Case-based debriefing consisted of discussions by the house officers of cases they encountered during the MICU rotation. Sessions were moderated by a staff physician trained in palliative care and a palliative care advanced practice nurse. Open-ended questions stimulated the residents' reflection on their decisions and guided the discussion pertinent to palliative care.
Using a survey instrument with a 4-point Likert scale, house officers assessed themselves before and after the rotation, rating their confidence in 9 areas of palliative care. Paired t tests were used to compare the cohort's scores before and after the rotation.
Results
A total of 214 house officers completed prerotation and postrotation surveys from April 2007 to September 2011. After completing the course, house officers demonstrated statistically significant improvement in confidence with conducting family conferences (mean 2.6 before vs 3.1 after [P<0.001]), delivering bad news (mean 3.1 before vs 3.5 after [P<0.001]), discussing do not resuscitate orders (3.1 before vs 3.6 after [P<0.001]), discussing comfort care (mean 2.8 before vs 3.4 after [P<0.001]), discussing withdrawal of life-sustaining treatment (mean 2.6 before vs 3.2 after [P<0.001]), managing pain (mean 3.0 before vs 3.5 after [P<0.001]), managing terminal symptoms (mean 2.8 before vs 3.4 after [P<0.001]), assessing decision-making capacity (mean 2.8 before vs 3.4 after [P<0.001]), and discussing advance directives (mean 2.8 before vs 3.4 after [P<0.001]).
Conclusion
Using a multidisciplinary team to teach a structured curriculum that includes a case-based debriefing improves house officer confidence in discussing end-of-life care and providing palliative care to patients in the intensive care setting.
Keywords: Graduate medical education, intensive care unit, palliative care
INTRODUCTION
Many physicians are uncomfortable discussing end-of-life issues and care goals with patients and families and providing palliative care to dying patients. Temel et al1 demonstrated a result of this discomfort, showing that only 20% of patients with metastatic cancer had a documented code status on their outpatient charts. In teaching hospitals, these conversations are commonly led by house officers. However, end-of-life discussions can be challenging even for an experienced physician, especially because medical decisionmaking has evolved from a paternalistic approach to one that is patient and family centered. Patient-centered care presumes active involvement of patients and their families in decisionmaking about individual options for treatment and requires skillful communication and coordination. These discussions are becoming more challenging as the population ages and medical technology advances. However, house officers are not being taught how to conduct these conversations. One recent study revealed that only one-third of residents felt comfortable leading these conversations and very few had received formal training in delivering bad news or leading end-of-life discussions.2 Furthermore, miscommunication can occur with inadequately trained residents as manifested by the absence of do not resuscitate (DNR) orders for patients who did not want resuscitation.3
With the ongoing growth of hospitalist and intensivist models of care delivery, end-of-life conversations may occur more often upon admission to the hospital or intensive care unit (ICU). These conversations do not take place in the primary care clinic. Therefore, we implemented our house officer curriculum in the medical intensive care unit (MICU).
Multidisciplinary palliative care teams have increased in the United States. These teams can be a resource for teaching end-of-life care, supporting house officers who may experience personal difficulties with end-of-life cases, and demonstrating the importance of interdisciplinary teamwork. We used just such a team for our course. These interdisciplinary educators used a case-based approach within a structured curriculum to improve resident confidence in delivering bad news, discussing poor prognoses, explaining the dying process, and providing palliative care within the MICU.
METHODS
A structured curriculum was implemented as part of the MICU rotation for house officers. The curriculum involved a 3-part approach that included tutorials, role modeling by the attending physician and the palliative care team, and a case-based debriefing at the end of each rotation. We used experiential learning, small group sessions, reflection, and didactics to teach the principles of palliative care medicine and improve house officer confidence.
The tutorial involved small group teaching sessions as part of the repeating scheduled curriculum for the MICU led by an intensivist trained in palliative care. Through discussion of current events that affect both individual patients and the delivery of healthcare on a larger scale, the seminar-style tutorial covered legal and ethical aspects of palliative care.
The palliative care team consisted of a nurse practitioner or registered nurse trained in palliative care, along with either the attending physician for the MICU or the attending physician for the palliative care team. The palliative care team that had helped coordinate care with the house officers caring for patients either role modeled discussions with patients and their families for the residents or allowed the residents to lead the discussion and then provided feedback.
The case-based debriefing session served as a significant event analysis toward the end of every MICU rotation. House officers chose cases for discussion based on their own patient care experiences during their MICU month. Debriefing sessions typically featured difficult or challenging situations, as well as cases that house officers found personally rewarding. A staff physician trained in palliative care and a palliative care advanced practice nurse moderated these learning encounters and asked open-ended questions to stimulate resident reflection about their decisions and to guide the discussion pertinent to palliative care. The sessions also functioned as a forum for house officers to discuss how cases affected them personally.
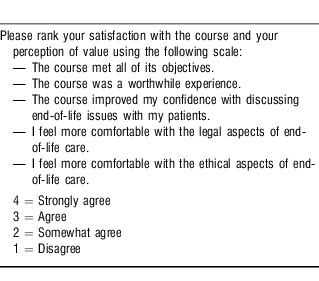
We assessed metrics using a modified survey instrument from David Weissman and Bruce Ambuel to measure house officer self-confidence and concerns about end-of-life clinical skills and decisionmaking with a 4-point Likert scale.4 Before and after the rotation, house officers evaluated their confidence in 9 areas of palliative care (Table 1). House officers answered questions about conducting family conferences, delivering bad news, discussing DNR orders, transitioning to comfort care, discussing treatment withdrawal, assessing and managing pain, assessing and managing terminal symptoms, assessing decisionmaking capacity, and discussing advance directives with patients. We used paired t tests to compare scores for the cohort before and after the rotation. House officers also assessed their satisfaction with the course at the end of each rotation using a Likert scale survey (Table 2).
Table 1.
Resident Self-Assessment of Competence in Providing End-of-Life Care
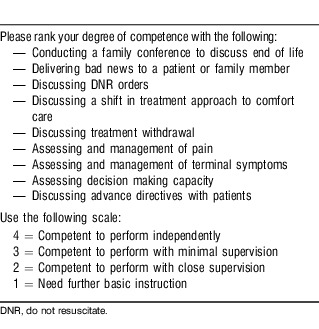
Table 2.
Resident Satisfaction With Palliative Care Course Survey
RESULTS
A total of 214 house officers participated in the course and completed surveys from April 2007 to September 2011 during their MICU rotation. House officers' specialties included emergency medicine, preliminary medicine, and categorical medicine; they were in years 1 through 3 of training. Preliminary medicine house officers consisted of first-year anesthesia, radiology, dermatology, and ophthalmology interns. Categorical house officers rotate on the MICU once in their intern year and then twice a year afterward.
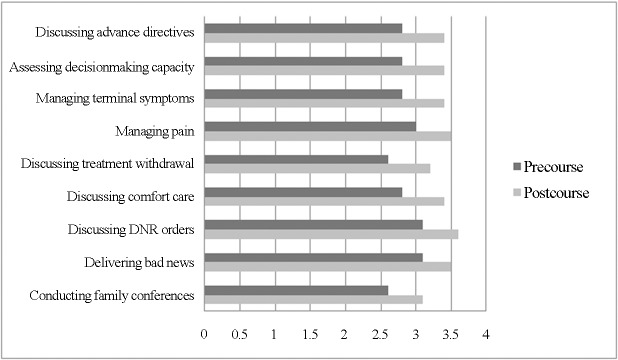
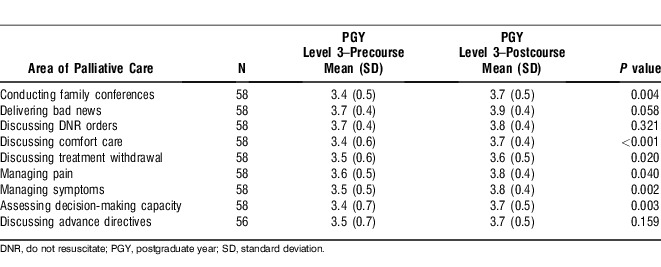
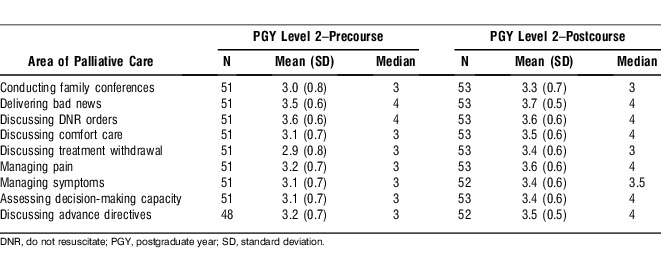
Our structured curriculum improved house officer confidence in all 9 measured areas of palliative and end-of-life care (Table 3 and Figure 1). Among internal medicine categorical house officers, confidence with palliative care continued to improve through all 3 years of training and demonstrated sustained improvement in the third year of residency (Tables 4-6). However, as shown in Table 6, by their third year of training, residents no longer perceived significant improvement in 3 of the palliative care areas: delivering bad news, discussing DNR orders, and discussing advance directives.
Table 3.
Improvement in House Staff Confidence With Providing End-of-Life Care
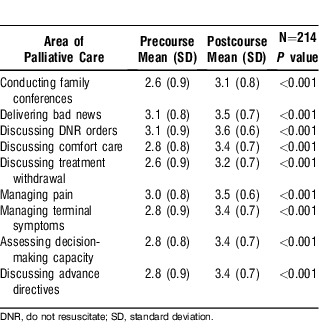
Figure 1.
Comparison of precourse and postcourse scores of residents' self-assessments of their competence in providing end-of-life care.
Table 4.
Improvement in Interns' Confidence With Providing End-of-Life Care
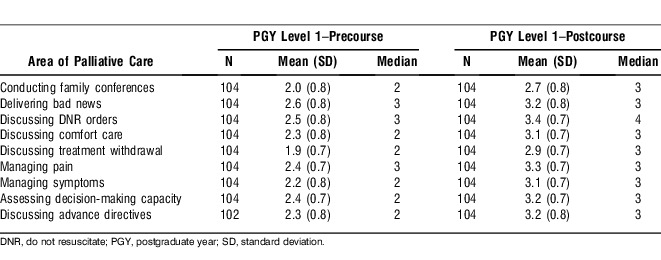
Table 6.
Improvement in 3rd-Year Residents' Confidence With Providing End-of-Life Care
More than 90% of house officers either strongly agreed or agreed that the course met all of its objectives, was a worthwhile experience that improved their confidence in discussing end-of-life issues, and improved their comfort with the legal and ethical aspects of end-of-life care (Figure 2).
Figure 2.
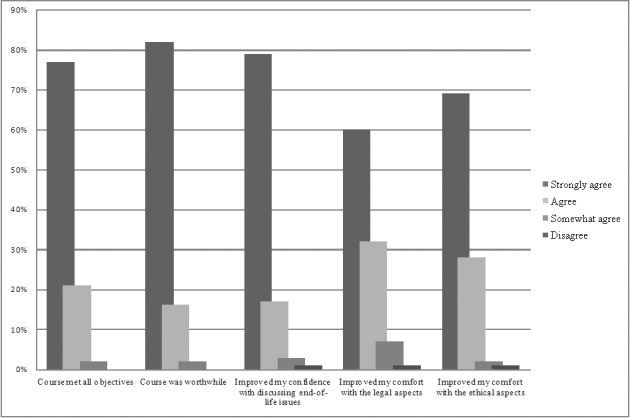
Residents' satisfaction with the palliative care education course.
DISCUSSION
First-year house officers self-reported a need for close supervision when discussing or providing end-of-life care. Residents' confidence in the domains of palliative care improved over time as they progressed in their training program. However, without a comparable control group, we were unable to determine how much of this improvement may have been a result of the course or experiential learning that would occur otherwise during internal medicine training. Nonetheless, we found clear improvement in house officer confidence in the measured 9 points of palliative care after the rotation. These results suggest that our teaching approach likely played a significant role in improving house officer confidence over all 3 years of residency. The only areas that did not show improvement among third-year residents were discussing DNR orders, discussing advance directives, and delivering bad news. Because third-year house officers would have already rotated through the curriculum 3 times, they may no longer have felt that the course increased their confidence in regard to discussing these points with patients and their families. Even so, they continued to report benefits in other areas, such as conducting family conferences, discussing comfort care and withdrawal of treatment, managing pain and terminal symptoms, addressing ethical issues, and assessing decision-making capacity.
A structured end-of-life curriculum taught by a multidisciplinary team using case-based discussions leads to improved house staff confidence in conducting family conferences, discussing end-of-life issues, and providing palliative care. As palliative care teams become more integrated into healthcare systems, they must likewise be incorporated into medical education programs. In some palliative care models in intensive care units, the palliative care team provides the care without involving the intensive care house staff or participating in resident education; however, the palliative care team can be an important resource for teaching end-of-life care and modeling the benefits of interdisciplinary teamwork to house officers. We found that employing an interdisciplinary team of palliative care experts to facilitate case-based learning helped house officers learn to cope with the stress of managing dying patients and supporting their families. We believe that this curriculum provided a valuable educational forum for residents to reflect on the psychosocial and ethical challenges in the management of critically ill patients and to receive supportive feedback from peers and faculty. By teaching palliative care in a structured and supportive curriculum, we hope that physicians will be more comfortable and competent in conducting these discussions with patients and their families and providing compassionate care to dying patients.
CONCLUSION
Our study demonstrates that a multidisciplinary team and structured curriculum can successfully improve house officer confidence with providing palliative and end-of-life care. Future study is required to evaluate house officer competence in leading family discussions, discussing end-of-life care, and providing palliative care.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
Epitoma
Despite residents feeling uncomfortable discussing death and dying with patients and families as well as providing palliative care, formal training on end-of-life care is still lacking from most residency programs. The authors developed an innovative curriculum involving a multidisciplinary team and using real cases the residents had managed during their critical care rotation to teach residents how to have an end-of-life conversation and provide palliative care. House officers who participated in the course improved their confidence with discussing and providing palliative care and felt that the course met its goals and was worthwhile. The authors provided a practical curriculum embedded within the medical intensive care unit rotation to teach end-of-life care and support house officers as they learn to communicate bad news and deal with death and dying.
—Guest Editor Leonardo Seoane, MD
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Interpersonal and Communication Skills, Systems-Based Practice, and Practice-Based Learning and Improvement.
Table 5.
Improvement in 2nd-Year Residents' Confidence With Providing End-of-Life Care
REFERENCES
- 1.Temel JS, Greer JA, Admane S, et al. Code status documentation in the outpatient electronic medical records of patients with metastatic cancer. J Gen Intern Med. 2010 Feb;25(2):150–153. doi: 10.1007/s11606-009-1161-z. Epub 2009 Nov 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siddiqui MF, Holley JL. Residents' practices and perceptions about do not resuscitate orders and pronouncing death: an opportunity for clinical training. Am J Hosp Palliat Care. 2011 Mar;28(2):94–97. doi: 10.1177/1049909110374599. Epub 2010 Aug 27. [DOI] [PubMed] [Google Scholar]
- 3.Deep KS, Griffith CH, Wilson JF. Discussing preferences for cardiopulmonary resuscitation: what do resident physicians and their hospitalized patients think was decided? Patient Educ Couns. 2008 Jul;72(1):20–25. doi: 10.1016/j.pec.2008.01.017. Epub 2008 Mar 11. [DOI] [PubMed] [Google Scholar]
- 4.Weissman DE, Ambuel B, Norton AJ, Wang-Cheng R, Schiedermayer D. A survey of competencies and concerns in end-of-life care for physician trainees. J Pain Symptom Manage. 1998 Feb;15(2):82–90. doi: 10.1016/s0885-3924(97)00253-4. [DOI] [PubMed] [Google Scholar]