Abstract
Background
Intraoperative nerve monitoring (IONM) has been used in head and neck surgery since the 1970s. Its utilization for monitoring and protecting the recurrent laryngeal nerve, however, is a controversial subject. This paper details the use, value, and cost of this technology within a single institution.
Methods
We conducted a retrospective chart review, analysis of surgery time with and without IONM, analysis of postoperative vocal cord function, and review of the literature.
Results
IONM did not reduce the operative time during either thyroid lobectomies or total thyroidectomies in 119 surgeries. Use of IONM increased the cost of each surgery by $387. IONM did not decrease the number of injured nerves (postoperative paresis).
Conclusions
IONM has proven to be highly useful in certain circumstances but has not been definitively proven to protect the nerve any more effectively than the gold standard of nerve visualization. In our study, the use of IONM did not reduce the time of thyroid surgery and did increase the cost. While IONM may, in special clinical circumstances such as revision and malignant thyroid surgery, increase the value of the operation, its use for every thyroid surgery does not appear to be cost effective or valuable to the patient.
Keywords: Head and neck surgery, intraoperative nerve monitoring, Nerve Integrity Monitor tube, recurrent laryngeal nerve, thyroid, vocal cord paralysis
INTRODUCTION
Thyroid surgery is a technically specific surgery involving highly detailed anatomy. The recurrent laryngeal nerve (RLN) is the most important structure at risk during thyroidectomies. The gold standard for protecting the nerve is identifying it through careful dissection before proceeding with the removal of the thyroid gland. In the 1950s, Riddell1 reported this technique of comparing identification and nonidentification of the nerve during thyroidectomies. Since that report, nerve visualization, anatomical knowledge, and surgeons' experience have been the most important tools for protecting the RLN and still serve as the standard of care. The variability in the nerve's course can lead to trouble with identification and increase the risk of injury when surgeons are inexperienced. Although the rate of injury to the nerve has been reported to be relatively low—up to 6% for temporary paresis and up to 2% for paralysis—most believe that these types of injury must be reduced further.2
Multiple devices over the years have helped surgeons identify the course of the RLN. Feinstein3 first mentioned electromyography (EMG) use in diagnosing disorders of the RLN in 1946. Delgado et al4 were the first to use EMG intraoperatively to identify the facial nerve in 1979, but Brennan and colleagues were the first to publish their data on RLN monitoring in 2001.5
Intraoperative nerve monitoring (IONM) has become the most widely used adjunct for identifying the RLN and allows real-time identification and functional assessment of the RLN in the operative field. The Nerve Integrity Monitor tube (Xomed, Jacksonville, FL) and the Dragon Stick-on Electrode (IOM Products, Inc., Ventura, CA) are 2 popular devices used to monitor the nerve via EMG.6 This technology uses both spontaneous and evoked potentials to monitor the functionality of the vocalis muscle and the RLN. Spontaneous EMG allows visualization of spontaneous muscle action potentials (MAPs) from nerves with tonic or background activity and also from mechanical stimuli such as dissection or retraction. The surgeon can use a probe to send a stimulatory impulse to the nerve stimulating the vocalis muscle; in turn, the surface electrodes on the endotracheal tube pick up if the vocal cord muscles respond to the stimulus. An injured nerve will require a higher stimulus than an intact one, allowing for the detection of early injury.6
The use of this technology in thyroid surgery has been a much debated topic for years. No consensus exists regarding IONM's effectiveness in preventing RLN injury. Multiple papers have failed to prove with statistical significance that the use of IONM during thyroid surgery decreases the rate of RLN palsy or paresis.7 A large prospective evaluation study8 showed that IONM helps during revision surgery, but research has not proven IONM use to be more effective than nerve identification alone for protecting the nerve during thyroid surgery.
This study assessed whether or not the use of IONM is cost effective in thyroid surgeries. We hypothesized that the use of IONM might decrease operating time enough to cover the cost of the device and/or decrease the overall cost of the surgery.
METHODS
This study was conducted with the approval of the Ochsner Clinic Foundation Institutional Review Board (IRB Number: 2011.014.C). Our retrospective chart review compared the duration of total thyroidectomies and thyroid lobectomies from a single surgeon with and without the aid of IONM in an effort to determine cost effectiveness. We compared the means and medians of the surgery time with and without implementation of IONM. We also analyzed perioperative vocal cord paresis and paralysis and reviewed the current and past literature.
RESULTS
A single surgeon performed 119 thyroid surgeries between 2007 and 2010: 76 lobectomies and 43 total thyroidectomies with 162 nerves at risk. The surgeon used IONM in 31 of the surgeries (21 lobectomies, 10 total thyroidectomies).
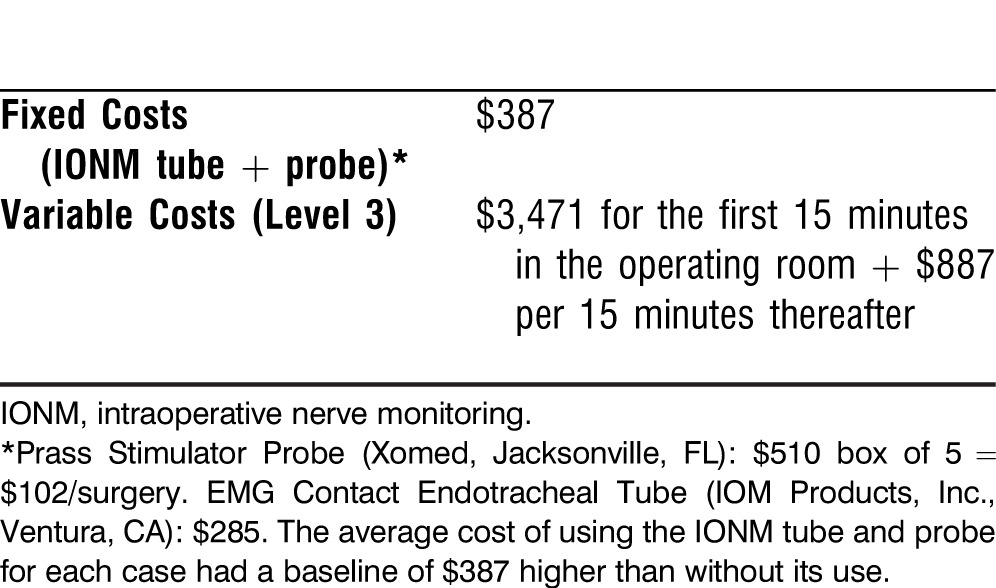
The average time of a lobectomy was 81.5 minutes, and a total thyroidectomy took an average of 101.7 minutes (Table 1). Lobectomies using IONM were on average 4.2 minutes longer than cases performed without IONM, but total thyroidectomies using IONM were on average 2.6 minutes shorter than non-IONM cases (Table 2). The use of IONM increased the base price of each case by $387 (Table 3).
Table 1.
Average Surgery Time in Minutes by Type of Procedure
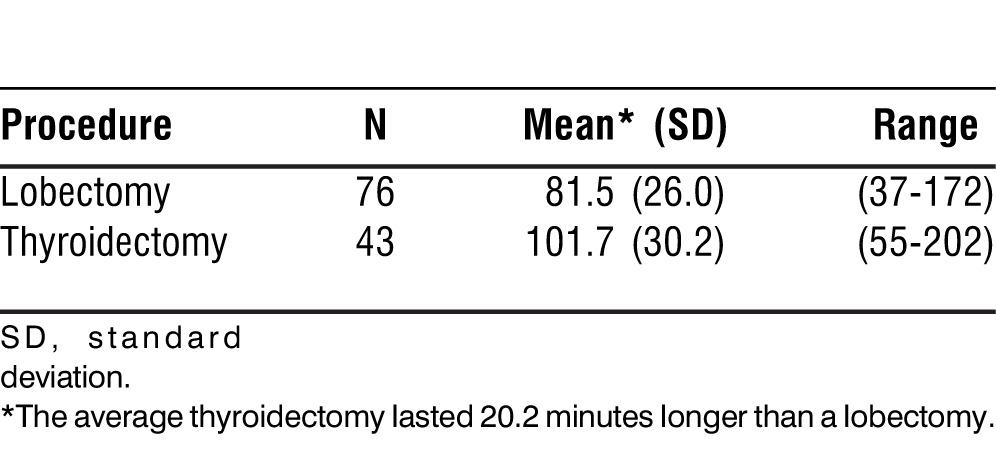
Table 2.
Average Surgery Time by Procedure and Intraoperative Nerve Monitoring (IONM) Use
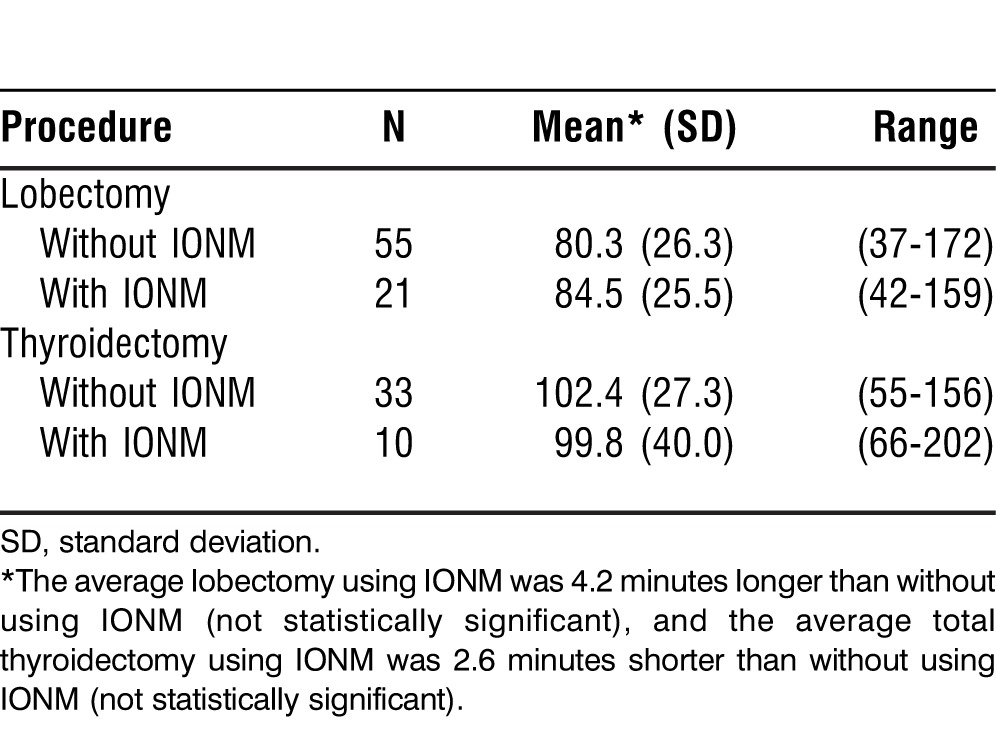
Table 3.
Operating Room Cost
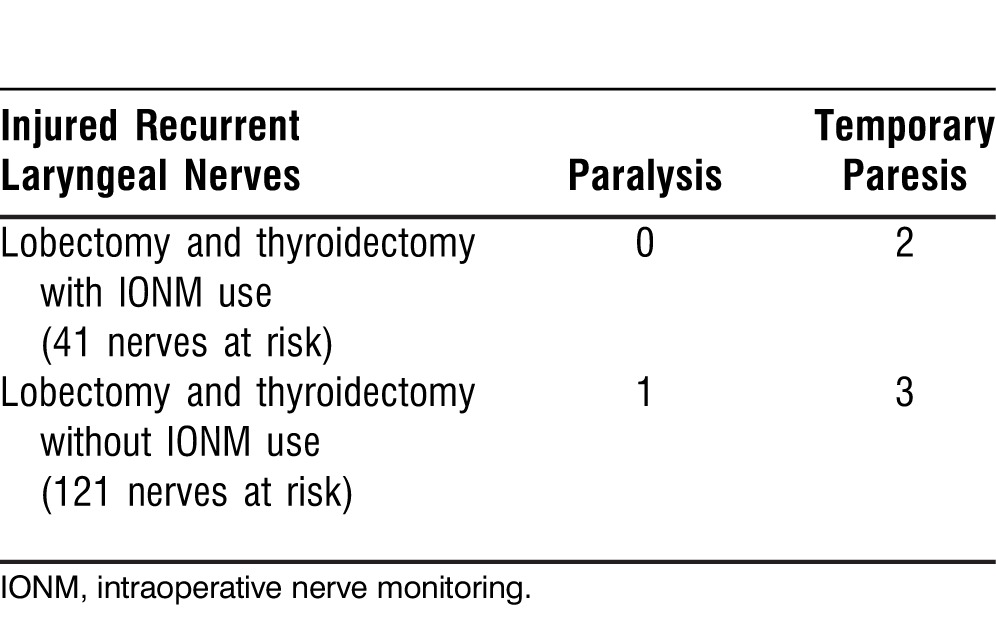
Six of the 162 nerves at risk were injured during surgery (3.7%). With IONM in use, 2 of 41 (4.9%) nerves at risk were injured in a manner that caused temporary paresis. Without IONM, 3 of 121 (2.5%) nerves at risk suffered temporary paresis. The single case of paralysis occurred when IONM was not used (0.8% of 121 nerves at risk) (Table 4).
Table 4.
Number of Nerves Injured
DISCUSSION
The use of IONM during thyroid surgery has been and will continue to be a highly debated subject. IONM's use for thyroid surgery as an adjunct for decreasing nerve injury during thyroid lobectomies and total thyroidectomies is questionable, although it has proven valuable in certain circumstances, such as revision thyroid surgery in which anatomical landmarks are obscured. However, IONM has not been definitively proven to decrease the rate of RLN injury any more effectively than nerve visualization alone. In 2004, Dralle and colleagues8 assessed thyroidectomy in 3 groups: no RLN identification, visual identification alone, and visual identification plus IONM identification. They concluded that for surgeons performing fewer thyroid operations on average, IONM decreased the number of paralyzed nerves. However, further examination did not show a difference in RLN injury rates. In one of the largest retrospective studies of a single surgeon, Shindo and Chheda9 in 2007 showed no statistically significant difference in paresis between visualization alone and IONM plus visualization. Thomusch and colleagues10 showed in 2004 with 15,403 at-risk nerves that IONM can be effective in assisting surgeons but “did not prevent injuries” and “did not make an unsafe surgeon into a safe surgeon.” IONM is an adjunct that may be helpful, but it should never replace the meticulous technique of the surgeon.
In this study, IONM increased the length of lobectomies by 4.2 minutes on average but decreased the length of total thyroidectomies by 2.6 minutes. These numbers are not statistically significant. The cost of each surgery with IONM was $387 higher than without its use (Table 3). The actual cost is probably higher when using the IONM system because a nerve monitor technician must be present in the operating room for every case in which the system is employed. Therefore, the use of IONM increased the total cost of surgeries by at least $11,997 ($387 multiplied by 31 surgeries with IONM) without any definitive increase in value: IONM would have to either increase the safety or decrease the cost of the operation, neither of which IONM did in this analysis.
Our rate for temporary paresis and paralysis of 3.7% was on par with the average reported range.7 When using IONM during the surgery, the rate of temporary paresis was actually 2.4% higher than when not used. An injury to 1 of 162 (0.6%) at-risk nerves resulted in a paralysis; IONM was not used during that case. The difference in the rate of RLN palsies with or without the use of IONM was not statistically significant.
Important limitations of this study include the small number of cases, the retrospective analysis, and the lack of histopathology of the thyroid disease for each case. This last concern led the authors to consider that IONM is definitely valuable in patients with prior cervical exploration/thyroidectomy, malignant pathology, previous head and neck radiation, Hashimoto thyroiditis, and/or unilateral vocal fold paralysis in which thyroidectomy is indicated on the opposite lobe.
CONCLUSION
The use of the IONM for every thyroid surgery does not prove cost effective or valuable to the patient. We found no statistically significant surgical time decrease using IONM—it actually tended toward increased surgical time during lobectomies—and an overall increased cost of surgery. While previous literature has proven distinct advantages in using IONM in revision and malignant thyroid surgery,8 we found no record of cost analysis. To our knowledge our data—while limited in power—are the first of their kind.
Footnotes
This study was conducted with the approval of the Ochsner Clinic Foundation Institutional Review Board: 2011.014.C.
The authors have no financial or proprietary interest in the subject matter of this article.
Presented at the Triological Society Combined Sections Meeting held January 26-28, 2012, in Miami Beach, FL.
Epitoma
Most academic medical centers in the United States have begun working on pursuit of value projects as they collectively prepare for the changes in healthcare delivery and reimbursement over the next 2-3 years. An essential premise of these projects is an understanding of the value proposition for both patients and their payer groups. The value proposition to both groups is equated to driving quality patient care to the highest level while decreasing the cost of healthcare delivery. This study is a resident-driven analysis of the value proposition as it pertains to patients undergoing thyroidectomy where an established complication might include temporary or permanent recurrent laryngeal nerve paralysis with resultant hoarseness, shortness of breath, and/or dysphagia.
—Guest Editor Ronald G. Amedee, MD
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, and Systems-Based Practice.
REFERENCES
- 1.Riddell VH. Injury to recurrent laryngeal nerves during thyroidectomy; a comparison between the results of identification and non-identification in 1022 nerves exposed to risk. Lancet. 1956 Sep 29;271(6944):638–641. doi: 10.1016/s0140-6736(56)92333-9. [DOI] [PubMed] [Google Scholar]
- 2.Miller MC, Spiegel JR. Identification and monitoring of the recurrent laryngeal nerve during thyroidectomy. Surg Oncol Clin N Am. 2008 Jan;17(1):121–144. doi: 10.1016/j.soc.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Feinstein B. The application of electromyography to affections of the facial and the intrinsic laryngeal muscles. Proc R Soc Med. 1946 Oct;39(12):817–819. [PMC free article] [PubMed] [Google Scholar]
- 4.Delgado TE, Bucheit WA, Rosenholtz HR, Chrissian S. Intraoperative monitoring of facila muscle evoked responses obtained by intracranial stimulation of the facila nerve: a more accurate technique for facila nerve dissection. Neurosurgery. 1979 May;4(5):418–421. doi: 10.1227/00006123-197905000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Brennan J, Moore EJ, Shuler KJ. Prospective analysis of the efficacy of continuous intraoperative nerve monitoring during thyroidectomy, parathyroidectomy, and parotidectomy. Otolaryngol Head Neck Surg. 2001 May;124(5):537–543. doi: 10.1067/mhn.2001.115402. [DOI] [PubMed] [Google Scholar]
- 6.Dillon FX. Electromyographic (EMG) neuromonitoring in otolaryngology-head and neck surgery. Anesthesiol Clin. 2010 Sep;28(3):423–442. doi: 10.1016/j.anclin.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Angelos P. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin North Am. 2009 Oct;89(5):1157–1169. doi: 10.1016/j.suc.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004 Dec;136(6):1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007 May;133(5):481–485. doi: 10.1001/archotol.133.5.481. [DOI] [PubMed] [Google Scholar]
- 10.Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004 Nov;389(6):499–503. doi: 10.1007/s00423-003-0444-9. Epub 2004 Jan 13. [DOI] [PubMed] [Google Scholar]


