Abstract
Kaposi sarcoma is the most common neoplasm caused by Kaposi sarcoma–associated herpesvirus (KSHV). It is prevalent among the elderly in the Mediterranean, inhabitants of sub-Saharan Africa, and immunocompromised individuals such as organ transplant recipients and AIDS patients. Current treatments for Kaposi sarcoma can inhibit tumor growth but are not able to eliminate KSHV from the host. When the host’s immune system weakens, KSHV begins to replicate again, and active tumor growth ensues. New therapeutic approaches are needed. Cannabidiol (CBD), a plant-derived cannabinoid, exhibits promising antitumor effects without inducing psychoactive side effects. CBD is emerging as a novel therapeutic for various disorders, including cancer. In this study, we investigated the effects of CBD both on the infection of endothelial cells (ECs) by KSHV and on the growth and apoptosis of KSHV-infected ECs, an in vitro model for the transformation of normal endothelium to Kaposi sarcoma. While CBD did not affect the efficiency with which KSHV infected ECs, it reduced proliferation and induced apoptosis in those infected by the virus. CBD inhibited the expression of KSHV viral G protein–coupled receptor (vGPCR), its agonist, the chemokine growth-regulated protein α (GRO-α), vascular endothelial growth factor receptor 3 (VEGFR-3), and the VEGFR-3 ligand, vascular endothelial growth factor C (VEGF-C). This suggests a potential mechanism by which CBD exerts its effects on KSHV-infected endothelium and supports the further examination of CBD as a novel targeted agent for the treatment of Kaposi sarcoma.
Keywords: cannabidiol, Kaposi sarcoma, Kaposi sarcoma–associated herpesvirus, viral G protein–coupled receptor, vascular endothelial growth factor receptor 3
Introduction
Kaposi sarcoma–associated herpesvirus (KSHV), also termed human herpesvirus 8 (HHV-8), is the etiological agent of Kaposi sarcoma, a vascular neoplasm.1,2 While KSHV usually establishes a lifelong latent infection in the host, additional factors, including immunosuppression, can facilitate the transformation of infected cells into an active malignancy.3,4 KSHV produces a set of viral proteins that promote its survival and spread. These proteins can co-opt normal cellular receptors to facilitate viral entry into target cells, mimic cellular receptors to evade the immune system, and foster tumor cell proliferation.5,6
One such viral protein, KSHV viral G protein–coupled receptor (vGPCR), is believed to be a key contributor to malignant transformation because it can immortalize endothelial cells7,8 and induce Kaposi sarcoma–like lesions in a transgenic animal model.9,10 vGPCR is constitutively active. In vitro, it can be detected in target cells during lytic infection.11 It is also expressed in scattered tumor cells within Kaposi sarcoma lesions.12,13 vGPCR is highly homologous to the human CXC chemokine receptors CXCR1 and CXCR2,14,15 and ligands of these receptors, including interleukin-8 (IL-8) and growth-regulated protein α (GRO-α), can augment the effects of vGPCR.16,17 Although some cellular G protein–coupled receptor kinases may inhibit vGPCR to a small degree,18 and chemokines such as interferon γ–induced protein 10 (IP-10)19 and stromal cell–derived factor 1α (SDF-1α) have been reported to inhibit vGPCR signaling,20 no effective means to block the effects of vGPCR have advanced to clinical use.
Cannabidiol (CBD) was first isolated in 1940.21 It is a major component of the plant Cannabis sativa, which is also the source of Δ9-tetrahydrocannabinol (Δ9-THC).22 Due to its multiple biological activities, CBD has been identified as a potential clinical agent. Moreover, CBD affects these activities without the psychoactive side effects that typify Δ9-THC.23 Recent studies have documented the potential antitumorigenic properties of CBD in the treatment of various neoplasms, including breast cancer,24 lung cancer,25 bladder cancer,26 glioblastoma,27 and leukemia.28 CBD induces these effects through a variety of mechanisms and signaling pathways. For example, it inhibits the growth and metastasis of breast cancer by downregulating the expression of inhibitor of differentiation 1 (ID-1),24 limits the invasion of lung cancer cells into adjacent tissues by reducing plasminogen activator inhibitor 1 (PAI-1) levels,25 and induces the programmed cell death of bladder cancer cells by affecting a continuous calcium influx.26 In addition, CBD can enhance the inhibitory properties of Δ9-THC on the growth and survival of glioblastoma cell lines29; however, the precise molecular mechanisms by which CBD mediates these effects are poorly understood.30
KSHV-infected endothelial cells are commonly used as an in vitro model for Kaposi sarcoma.7,8,31,32 We used primary human dermal microvascular endothelial cells (HMVECs) to assess the effects of CBD on infection, proliferation, and programmed cell death. CBD inhibited proliferation and enhanced apoptosis in KSHV-infected HMVECs by blocking the expression of vGPCR, GRO-α, vascular endothelial growth factor receptor 3 (VEGFR-3), and vascular endothelial growth factor C (VEGF-C). These data support the further evaluation of CBD as a novel therapeutic to treat Kaposi sarcoma.
Results
CBD does not modulate the infection of HMVECs by KSHV
CBD can alter vascular permeability33,34 and therefore may affect viral entry into endothelial cells. To investigate whether CBD may enhance KSHV infection of endothelial cells, we exposed HMVECs to green fluorescent protein (GFP)-tagged KSHV or to a mock infection in the presence of various concentrations of CBD. Under control conditions (0 µM CBD), KSHV infected an average of 25% of HMVECs per well (Fig. 1). We observed no significant difference in infection efficiency when the cells were pretreated with up to 10 µM CBD (Fig. 1). These data suggest that CBD does not modulate the infection of endothelial cells by KSHV.
Figure 1.
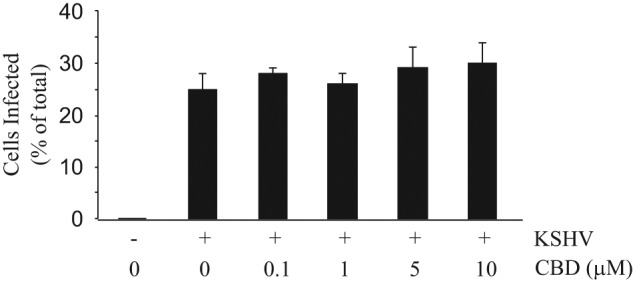
CBD does not modulate the infection of HMVECs by KSHV. Percentage of KSHV-infected HMVECs by fluorescence. HMVECs were pretreated with various concentrations of CBD or a vehicle control, followed by infection with GFP-KSHV virions or a mock infection. Cells were then washed with 1X PBS and cultured in normal medium. After 48 hours, green fluorescent cells (indicative of GFP-KSHV infection) were counted under a fluorescent microscope. Infection was calculated as a percentage of total cells. Data represent the mean ± SD.
CBD preferentially inhibits the proliferation of KSHV-infected HMVECs versus normal HMVECs
Recent studies have indicated various antitumorigenic properties of CBD, including the inhibition of proliferation in breast cancer and glioblastoma cells.24,27 This prompted us to assess the effects of CBD on the growth of mock-infected HMVECs and KSHV-infected HMVECs (KSHV/HMVEC), models for normal endothelium and nascent Kaposi sarcoma, respectively, using an MTS-based assay. This assay measures changes in metabolic activity as a reflection of changes in proliferation and/or survival. We found a decrease in the percentage of proliferating mock-infected cells when treated with CBD at concentrations between 2.5 and 10 µM; however, even at 10 µM CBD, proliferation was reduced by only 20% of the controls (Fig. 2A). At concentrations between 1.5 and 10 µM, CBD inhibited significantly more proliferation in the virus-infected HMVECs (IC50 = 2.08 µM) than in the mock-infected HMVECs (Fig. 2A and 2B). In fact, at 10 µM, CBD reduced proliferation in the virus-infected cells by 79% of the controls (Fig. 2A). These data suggest that at select concentrations, CBD preferentially inhibits the proliferation of KSHV-infected endothelium versus normal endothelium.
Figure 2.
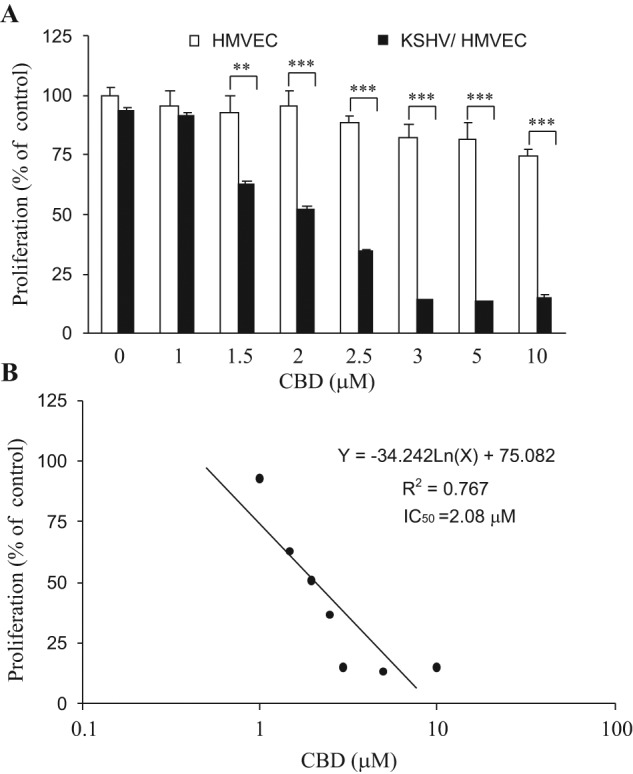
CBD preferentially inhibits the proliferation of KSHV-infected HMVECs. (A) Percentage of proliferating cells as measured by an MTS-based assay. Mock-infected HMVECs (HMVEC) and KSHV-infected HMVECs (KSHV/HMVEC) were incubated for 48 hours with various concentrations of CBD or a vehicle control. The proliferation index of untreated HMVECs was established as 100%, and all other cells and conditions were calculated as a percentage of this control. Data indicate the mean ± SD. **P < 0.01 and ***P < 0.001 indicate the difference in proliferation of KSHV/HMVEC versus HMVEC at each CBD concentration. (B) Regression analysis of the effect of CBD on the proliferation of KSHV-infected HMVECs.
CBD preferentially induces apoptosis in KSHV-infected HMVECs versus normal HMVECs
Previous studies have shown that CBD induces apoptosis in various tumor cells.26,27 Using mock-infected HMVECs and KSHV-infected HMVECs, we assessed the differential effects of CBD on programmed cell death. While CBD induced dose-dependent apoptosis in both cell types, at 0.25 to 1.0 µM, CBD induced significantly more cell death in the virus-infected HMVECs than in the mock-infected HMVECs (Fig. 3A). In the virus-infected cells, the in vitro EC50 for CBD was 1.04 µM (Fig. 3B), while the EC50 of the mock-infected cells was calculated as 1.68 µM. When treated with 2.0 to 10 µM CBD, there was no significant difference in apoptosis between the 2 cell types (Fig. 3A). At these higher concentrations, CBD induced between 80% and 100% apoptosis in both mock- and virus-infected cells (Fig. 3A). These dose-response data indicate that endothelial cells infected with KSHV are more sensitive to CBD-induced apoptosis than mock-infected endothelium and suggest that at specific concentrations, CBD may preferentially kill Kaposi sarcoma tumor cells versus normal endothelium.
Figure 3.
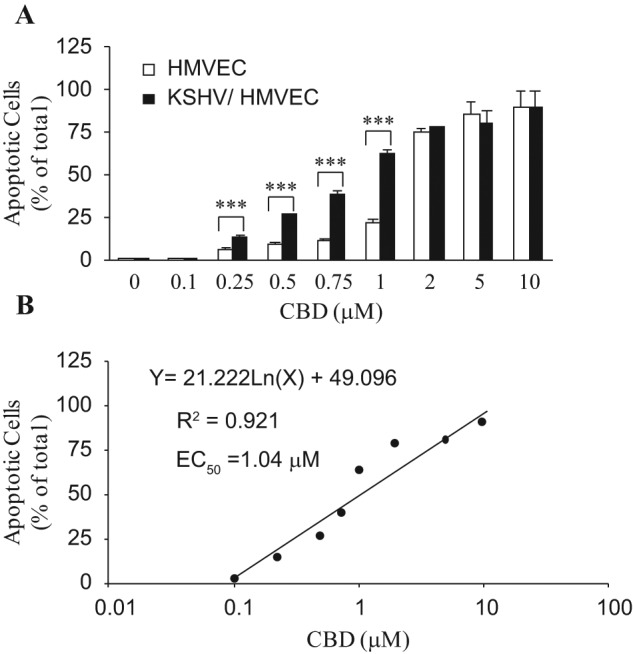
CBD preferentially induces apoptosis in KSHV-infected HMVECs. (A) Percentage of apoptotic cells as assayed by TUNEL. KSHV-infected HMVECs (KSHV/HMVEC) or mock-infected HMVECs (HMVEC) were treated with various concentrations of CBD or a vehicle control for 24 hours. Data were calculated as apoptotic cells/total cells. Data represent the mean ± SD. ***P < 0.001 indicates the difference in apoptosis levels of KSHV/HMVEC versus HMVEC at each CBD concentration. (B) Regression analysis of the effect of CBD on the apoptosis of KSHV-infected HMVECs.
CBD inhibits the expression of KSHV vGPCR
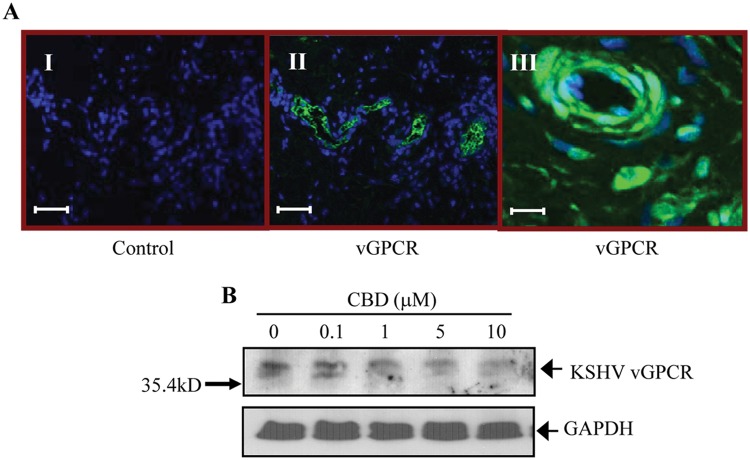
To explore the mechanism(s) by which CBD inhibits the growth of KSHV/HMVECs and induces their programmed cell death, we examined the effect of CBD on KSHV vGPCR, a protein that immortalizes endothelial cells and promotes Kaposi sarcoma tumorigenesis.7,9 vGPCR facilitates the transformation of KSHV-infected cells and enhances the proliferation of KSHV-infected endothelium.8,10 To confirm that vGPCR is expressed in Kaposi sarcoma, we examined protein levels and localization in Kaposi sarcoma lesions by immunohistochemical analysis. We found vGPCR expression in irregular vascular formations and scattered spindle cells of the Kaposi sarcoma tumor sections (Fig. 4A, panels II and III). Lack of staining in the isotype control–treated section illustrates antibody specificity (Fig. 4A, panel I).
Figure 4.
CBD inhibits the expression of KSHV vGPCR. (A) Representative immunohistochemical analysis of KSHV vGPCR expression in cutaneous Kaposi sarcoma lesions (panels II and III). Kaposi sarcoma lesion stained with an antibody isotype control (panel I). For panels I and II, scale bars = 50 µm. For panel III, scale bar =10 µm. (B) Representative Western blot analysis of KSHV vGPCR levels in whole cell lysates of KSHV/HMVECs after incubation with various concentrations of CBD or a vehicle control for 24 hours. GAPDH was used as a loading control.
In an earlier publication, we demonstrated that at low doses, Δ9-THC, a psychoactive cannabinoid related to CBD, enhanced the expression of vGPCR in KSHV-infected HMVECs.35 Here, by Western blot analysis, we examined the effects of CBD on the expression of vGPCR in such cells. We found that CBD altered vGPCR expression in KSHV-infected HMVECs; however, in contrast to Δ9-THC, CBD induced dose-dependent inhibition (Fig. 4B). Moreover, the concentrations at which CBD preferentially induced apoptosis and reduced proliferation in the KSHV/HMVECs were those at which vGPCR expression was also inhibited in these cells (Figs. 2, 3, and 4B). This suggests a potential mechanism through which CBD exerts its anticancer effects in KSHV-associated neoplasms.
CBD reduces levels of GRO-α in media conditioned by KSHV-infected HMVECs
Although vGPCR is a constitutively active G protein–coupled receptor, IL-8 and GRO-α can enhance its activity.16,17 Therefore, we measured the levels of these cytokines in the conditioned media of KSHV/HMVECs after treatment with various concentrations of CBD or a control using ELISA (Fig. 5). We observed a significant dose-dependent decrease in GRO-α in the conditioned media (Fig. 5A), with an in vitro IC50 of 1.66 µM (Fig. 5B). In contrast, CBD did not affect a statistically significant change in IL-8 levels in the conditioned media (Fig. 5C).
Figure 5.
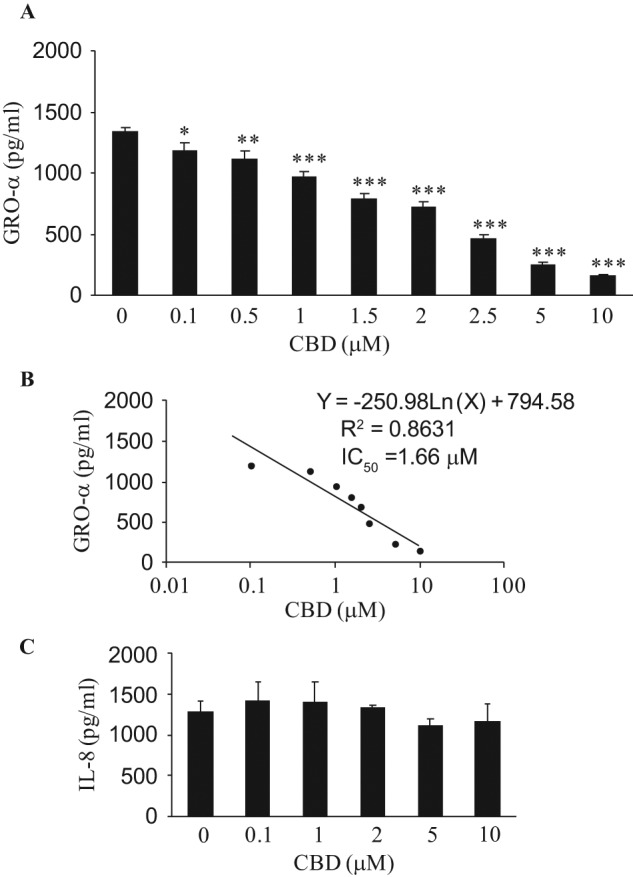
CBD reduces levels of GRO-α in media conditioned by KSHV-infected HMVECs. (A) GRO-α and (C) IL-8 levels in KSHV/HMVEC-conditioned media as assayed by ELISA. After KSHV/HMVECs were incubated with various CBD concentrations or a vehicle control for 18 hours, GRO-α (A) and IL-8 levels (C) were measured by ELISA. Data represent the mean ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001 for CBD treatments versus a control (0 µM CBD). (B) Regression analysis of the effect of CBD on GRO-α expression in KSHV/HMVEC-conditioned media.
CBD downregulates the expression of VEGFR-3 and VEGF-C
Upon activation, the VEGFR-3 receptor, a key molecule for lymphangiogenesis,36 promotes KSHV-induced infection, growth, and transformation of endothelial cells.37 To examine the activation status of VEGFR-3, we transiently transfected a vGPCR expression plasmid or vector control into a stable 293 cell line, manipulated to express high levels of VEGFR-3 (293/VEGFR-3). We immunoprecipitated VEGFR-3 from whole cell lysates and subsequently performed Western blot analysis with a phosphotyrosine antibody (Fig. 6A). We observed significant tyrosine phosphorylation in the cells transfected with vGPCR (+) as compared to those transfected with the vector control (–) (Fig. 6A). To confirm these observations in a primary cell line with endogenous VEGFR-3 expression, we repeated the experiment in HMVECs. Similarly, we observed significantly greater VEGFR-3 activation in the HMVECs transfected with vGPCR as compared to those transfected with the vector control (Fig. 6B). Taken together, these data indicate that vGPCR activates VEGFR-3 in 293/VEGFR-3 cells as well as in primary endothelial cells. When we examined total VEGFR-3 levels in KSHV-infected HMVECs, we observed high levels of the protein under control conditions (Fig. 6C, lane 0). This is consistent with existing data that demonstrate the enhancement of VEGFR-3 expression by KSHV38,39 and with high endogenous expression of VEGFR-3 in Kaposi sarcoma.40,41 Upon treatment with various concentrations of CBD, VEGFR-3 levels were significantly reduced (Fig. 6C), suggesting another mechanism whereby CBD may affect the proliferation and viability of Kaposi sarcoma through the VEGFR-3 signaling pathway.
Figure 6.
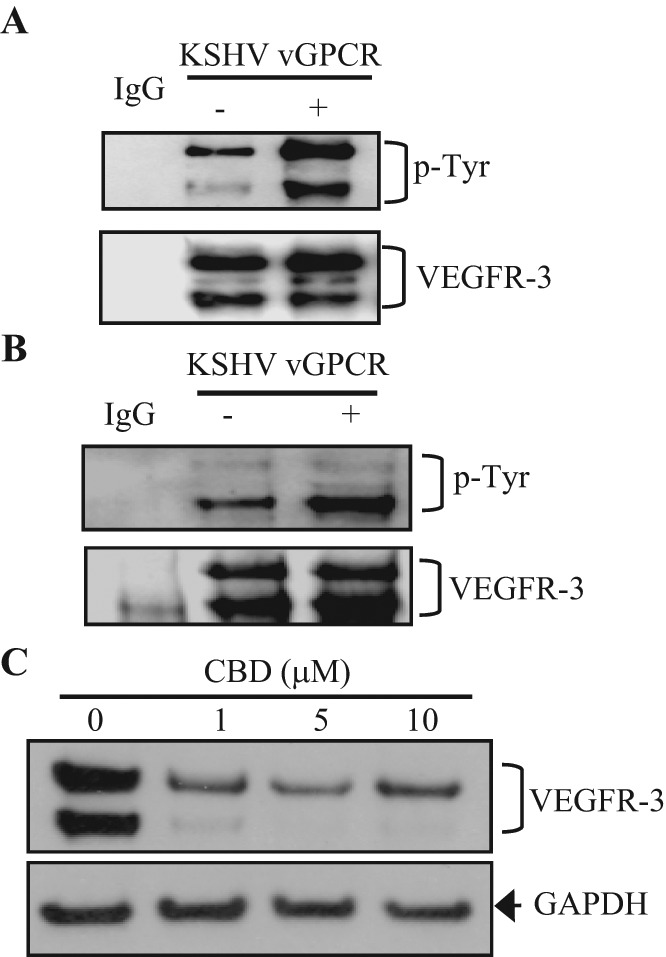
VEGFR-3 is activated by KSHV vGPCR and inhibited by CBD. (A) VEGFR-3 activation as assayed by VEGFR-3 immunoprecipitation and Western blot analysis. 293/VEGFR-3 cells were transfected with a KSHV vGPCR expression plasmid (+) or an empty vector (–). Total cell lysates were collected 48 hours after transfection and used for VEGFR-3 immunoprecipitation. Tyrosine phosphorylation of VEGFR-3 was detected by Western blot analysis. Total VEGFR-3 was used as a loading control. (B) VEGFR-3 activation as assayed by VEGFR-3 immunoprecipitation and Western blot analysis in HMVECs. HMVEC cells were transfected with a KSHV vGPCR expression plasmid (+) or an empty vector (–) and assayed as in A. (C) VEGFR-3 expression by Western blot analysis in KSHV/HMVECs. KSHV/HMVECs were incubated with various CBD concentrations for 18 hours. Total cell lysates were collected and VEGFR-3 expression measured by Western blot analysis. GAPDH was used as a loading control.
Next, by ELISA, we examined levels of VEGF-C and VEGF-D, the cognate ligands of VEGFR-3,42 in the conditioned media of KSHV/HMVECs after treatment with various concentrations of CBD (Fig. 7). We observed a significant dose-dependent decrease in VEGF-C levels in the conditioned media (Fig. 7A), with an in vitro IC50 of 7.87 µM (Fig.7B); however, CBD had no effect on VEGF-D expression (Fig. 7C). These data demonstrate that CBD inhibits the expression of VEGF-C in KSHV/HMVECs, while VEGF-D levels remain very low with/without CBD treatment. These data are consistent with CBD-induced reduction of VEGFR-3 levels (Fig. 6C), and together, they suggest that CBD may be an inhibitor of VEGFR-3/VEGF-C signaling in Kaposi sarcoma.
Figure 7.
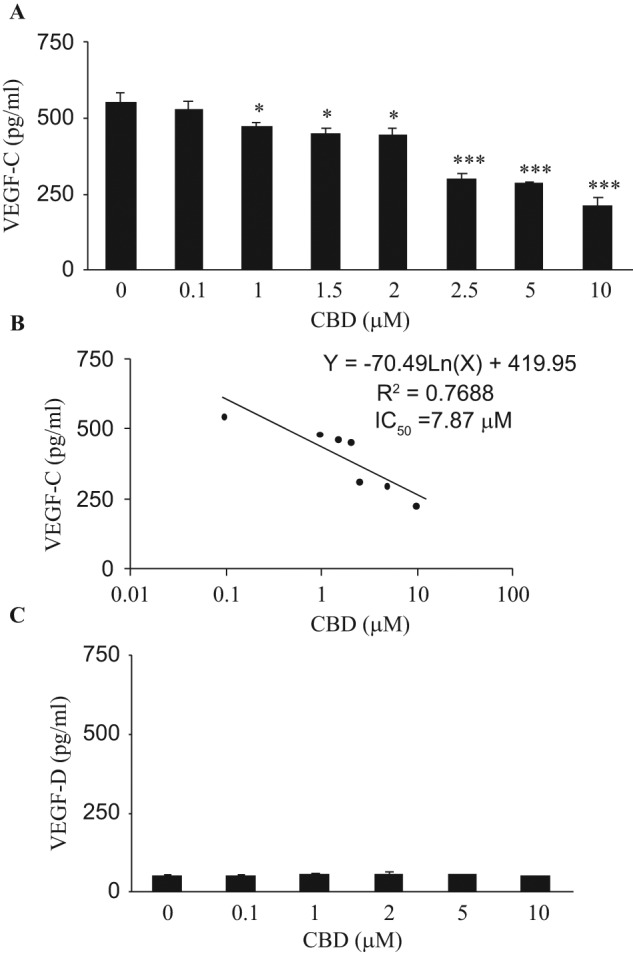
CBD inhibits the expression of VEGF-C. (A) VEGF-C and (C) VEGF-D levels in KSHV/HMVEC-conditioned media as assayed by ELISA. After KSHV/HMVECs were incubated with various CBD concentrations or a vehicle control for 18 hours, VEGF-C (A) and VEGF-D levels (C) were measured by ELISA. Data indicate the mean ± SD. *P < 0.05 and ***P < 0.001 for CBD treatments versus a control (0 µM CBD). (B) Regression analysis of the effect of CBD on VEGF-C expression in KSHV/HMVEC-conditioned media.
Discussion
CBD has been evaluated clinically for the treatment of various conditions, including anxiety,43 psychosis,44 and pain.45 In contrast to other members of the cannabinoid family, CBD has a strong safety profile and induces no psychotropic effects.23,30 Therefore, it has become an attractive agent in the search for new anticancer therapies.23 Our current study demonstrated that CBD preferentially enhanced apoptosis and inhibited the proliferation of KSHV-infected endothelial cells. This selective targeting of KSHV-induced neoplasia suggests that CBD may have a desirable therapeutic index when used to treat cancer. Moreover, a recent study demonstrated that CBD can be delivered effectively by nasal and transdermal routes,46 which may be particularly valuable for the treatment of Kaposi sarcoma oral or skin lesions.47
The molecular mechanisms by which CBD exerts its therapeutic effects are not fully understood, although CBD has been shown to act as an inverse agonist of the cannabinoid receptors CB1 and CB2.48 We found that CBD reduced the levels of vGPCR, GRO-α, VEGFR-3, and VEGF-C in KSHV-infected endothelium. These proteins are believed to play important roles in the initiation, growth, metastasis, and survival of Kaposi sarcoma.
vGPCR is lytically expressed in Kaposi sarcoma lesions but not in normal endothelium.15 It is presumed to be paramount in the transformation of normal cells to KSHV-associated cancers.5 Also, vGPCR promotes the growth of Kaposi sarcoma and helps to protect endothelial cells from programmed cell death.10,49 Although vGPCR is a constitutively active receptor, GRO-α is one of the ligands that can enhance its effects.17 GRO-α also plays an important role in wound healing, inflammation, angiogenesis, and tumorigenesis.50 Its transcripts increase in abundance with age in many human tissues, particularly the skin,51 and therefore, its inhibition may be of relevance for the treatment of classic age-related Kaposi sarcoma.52
VEGF-C and its receptor, VEGFR-3, are closely associated with tumorigenesis and tumor lymphatic metastasis.53,54 Kaposi sarcoma is believed to be derived from KSHV-infected lymphatic endothelial cells that express high levels of VEGF-C and VEGFR-3.40,41 VEGF-C/VEGFR-3 signaling modulates KSHV-induced transformation and growth of endothelial cells.37 Moreover, KSHV vGPCR can enhance endothelial cell transformation through activation of VEGFR-2 and VEGFR-3.55 Therefore, targeting the VEGFR-3 signaling pathway with CBD presents a potential means to treat highly vascularized tumors like Kaposi sarcoma.
We demonstrated that at higher experimental concentrations, that is, 2.5 to 10 µM, CBD inhibited the expression of VEGF-C in KSHV-infected endothelial cells. CBD significantly inhibited the expression of GRO-α beginning at a lower experimental concentration (1.0 µM) and with a lower overall IC50 (1.66 µM v. 7.87 µM). The varying efficacies with which CBD inhibited GRO-α and VEGF-C may be due to different forms of regulation at the transcriptional and/or translational levels; however, further study is required to characterize the specific molecular mechanisms responsible. In adults, VEGFR-3 is predominantly expressed by lymphatic endothelium and tumor vasculature and by a subset of normal endothelial cells, including HMVECs56 (Fig. 6B). As such, CBD could be expected to affect normal endothelial cells at higher concentrations. In contrast, the GRO-α receptor, vGPCR, is not expressed by normal endothelial cells.15 Based on these data, we hypothesize that while higher concentrations of CBD may target the expression of both VEGF-C and GRO-α, lower concentrations of CBD could significantly impact the proliferation and apoptosis of KSHV-infected cells and spare normal endothelium (as shown in Figs. 2A and 3A) by predominantly targeting signaling through GRO-α and vGPCR.
With the advent of highly active antiretroviral therapy for the treatment of AIDS in the 1990s, the incidence of AIDS-associated Kaposi sarcoma has decreased.4 However, the number of patients living with AIDS continues to increase, and as they live longer, it is likely that AIDS-associated Kaposi sarcoma will also rise.57 New treatments are needed to prevent or control the disease. Our data support the evaluation of CBD as a novel target-specific therapeutic for KSHV-induced neoplasms, including Kaposi sarcoma. We demonstrated that CBD could preferentially induce apoptosis and attenuate the proliferation of KSHV-infected HMVECs by inhibiting the expression of vGPCR, GRO-α, VEGFR-3, and VEGF-C. Further investigation to elucidate more precisely the mechanisms by which CBD induces its inhibitory effects may help guide the development of CBD as a treatment for KSHV-associated neoplasia.
Materials and Methods
Cells
Primary HMVECs (adult) were purchased from Lonza (Allendale, NJ) and maintained in EBM-2 basal medium, supplemented with EGM-2 MV BulletKit (Lonza). GFP–BCBL-1 cells were a gift from Dr. Jeffrey Vieira (Department of Laboratory Medicine, University of Washington, Seattle, WA). They were maintained in RPMI 1640 medium and supplemented as described previously.58 The 293/VEGFR-3 cell line (Genentech, South San Francisco, CA) was maintained in DMEM with 10% FBS.
Reagents
CBD was purchased from Tocris Bioscience (Ellisville, MO). TPA was purchased from Sigma-Aldrich (St. Louis, MO). Anti–KSHV vGPCR antibody was purchased from Cell Sciences (Canton, MA). All other antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA).
Plasmids and transfections
The KSHV vGPCR expression plasmid (pcDNA3.1vGPCR) was constructed as follows: KSHV genomic DNA was extracted from KSHV-positive BCBL-1 cells. The vGPCR gene was amplified from the KSHV genomic DNA, using the primers purchased from Invitrogen (Carlsbad, CA) (upstream sequence: 5′-GGAATTCATGGCGGCCGACCATTTCC-3′; downstream sequence: 5′-GTCTAGACGTGGTGGCGCCGGACATG-3′). The purified PCR product was digested with EcoR I and Xba I and inserted into the pcDNA3.1 plasmid digested with same restriction endonucleases to create pcDNA3.1vGPCR. HMVECs and 293/VEGFR-3 cells were transiently transfected with pcDNA3.1vGPCR or a vector control (pcDNA3.1) using Superfect Transfection Reagent from Qiagen (Valencia, CA).
Kaposi sarcoma tissue samples
Tissue samples from Kaposi sarcoma skin lesions of diagnosed HIV-positive patients were obtained after informed consent at Beth Israel Deaconess Medical Center (BIDMC). The protocol and consent form were approved by the BIDMC review board in accordance with an assurance filed with and approved by the US Department of Health and Human Services.
Immunohistochemistry
Kaposi sarcoma tissue samples were fixed in 4% formaldehyde solution and paraffin embedded. Serial sections were prepared by the Dana-Farber/Harvard Cancer Center Research Pathology Core (Boston, MA). Immunohistochemical staining was performed per instructions from Upstate Biotechnology (Waltham, MA). Vectashield, a DAPI-containing mounting medium, and FITC-conjugated secondary antibody were purchased from Vector Laboratories (Burlingame, CA). Kaposi sarcoma tissue sections were observed under a Zeiss LSM 510 META upright confocal microscope (Oberkochen, Germany).
GFP-KSHV virus propagation and infection
GFP–BCBL-1 cells were grown to a density of 5 × 105 cells/mL, induced with TPA at 20 ng/mL, and grown for 5 days. To harvest the virus, cells were pelleted at 500g for 15 minutes. The supernatant was removed and centrifuged at 15,000g for 4 hours. The pellet was resuspended in 1/100 growth volume complete media as discussed previously and centrifuged at 300g for 5 minutes. Purified KSHV virion was titrated by real-time PCR as described previously.35,37
Sixty-percent confluent HMVECs were pretreated for 2 hours with various CBD concentrations or a vehicle control. Subsequently, they were either mock infected or infected with GFP-KSHV in 24-well plates at 37°C for 3 hours, washed, and incubated at 37°C for 2 days in HMVEC medium, as described above. KSHV infections were performed at a multiplicity of infection of 5 to 6 KSHV copies per cell. Green fluorescent cells were counted under a fluorescent microscope (200× magnification) (Diaphot 300, Nikon, Tokyo, Japan) or detached by 5 mM EDTA in PBS and analyzed on a FACScan flow cytometer (BD Biosciences, San Jose, CA, USA) to determine the percentage of cells infected.
Cell stimulation, immunoprecipitation, and Western blot analysis
Cells were starved for 2 hours in serum-free media and subsequently stimulated with various concentrations of CBD as indicated in 0.5% BSA media for 24 hours (unless otherwise noted). After stimulation, total cell lysates were collected and processed for immunoprecipitation and Western blot analysis as described previously.37
Proliferation assay
The proliferation assay was performed using CellTiter 96 AQueous One Solution Cell Proliferation Assay (MTS, Promega, Madison, WI) per the manufacturer’s instructions. The number of proliferating cells was calculated as a percentage of total cells.
Apoptosis assay
KSHV-infected and mock-infected HMVECs were incubated in 0.5% BSA media with various concentrations of CBD (0-10 µM) for 24 hours. The In Situ Cell Death Detection Kit, Fluorescein (Roche Applied Science, Mannheim, Germany) was used for the detection and quantification of apoptosis. Cells were stained by the TUNEL method and observed under a fluorescent microscope to determine double-stranded DNA breaks per the manufacturer’s instructions.
Cytokine ELISA
Media conditioned by KSHV/HMVEC cells treated with various concentrations of CBD were collected and assayed by ELISA per the manufacturer’s instructions as follows: IL-8 (Human CXCL8/IL-8 Immunoassay, R&D Systems, Minneapolis, MN), GRO-α (Human CXCL1/GRO-α Immunoassay, R&D Systems), VEGF-D (Human VEGF-D Immunoassay, R&D Systems), and VEGF-C (Human VEGF-C Assay Kit, IBL-America, Minneapolis, MN).
Statistical analysis
Statistical significance was determined using the Student 2-tailed t test. Data represent the mean ± SD of at least 3 independent experiments, with P < 0.05 considered statistically significant. To calculate the IC50 and EC50 values, regression analyses were performed based on the proliferation and apoptosis data and the VEGF-C and GRO-α expression data, respectively.Western blot analysis and immunohistochemistry were repeated at least 3 times, and representative blots or images are shown.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received the following financial support for the research, authorship, and/or publication of this article: This work was supported by divisional funds.
References
- 1. Chang Y, Cesarman E, Pessin MS, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science. 1994;266(5192):1865-9 [DOI] [PubMed] [Google Scholar]
- 2. Antman K, Chang Y. Kaposi’s sarcoma. N Engl J Med. 2000;342(14):1027-38 [DOI] [PubMed] [Google Scholar]
- 3. Marcelin AG, Calvez V, Dussaix E. KSHV after an organ transplant: should we screen? Curr Top Microbiol Immunol. 2007;312:245-62 [DOI] [PubMed] [Google Scholar]
- 4. Martellotta F, Berretta M, Vaccher E, et al. AIDS-related Kaposi’s sarcoma: state of the art and therapeutic strategies. Curr HIV Res. 2009;7(6):634-8 [DOI] [PubMed] [Google Scholar]
- 5. Ganem D. KSHV-induced oncogenesis. In:Arvin A, Campadelli-Fiume G, Mocarski E, et al., editors. Human herpesviruses: biology, therapy, and immunoprophylaxis. Cambridge: Cambridge University Press; 2007. Chapter 56. Available from: http://www.ncbi.nlm.nih.gov/books/NBK47373 [PubMed] [Google Scholar]
- 6. Mesri EA, Cesarman E, Boshoff C. Kaposi’s sarcoma and its associated herpesvirus. Nat Rev Cancer. 2010;10(10):707-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boshoff C, Schulz TF, Kennedy MM, et al. Kaposi’s sarcoma-associated herpesvirus infects endothelial and spindle cells. Nat Med. 1995;1(12):1274-8 [DOI] [PubMed] [Google Scholar]
- 8. Flore O, Rafii S, Ely S, et al. Transformation of primary human endothelial cells by Kaposi’s sarcoma-associated herpesvirus. Nature. 1998;394(6693):588-92 [DOI] [PubMed] [Google Scholar]
- 9. Yang TY, Chen SC, Leach MW, et al. Transgenic expression of the chemokine receptor encoded by human herpesvirus 8 induces an angioproliferative disease resembling Kaposi’s sarcoma. J Exp Med. 2000;191(3):445-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sodhi A, Chaisuparat R, Hu J, et al. The TSC2/mTOR pathway drives endothelial cell transformation induced by the Kaposi’s sarcoma-associated herpesvirus G protein-coupled receptor. Cancer Cell. 2006;10(2):133-43 [DOI] [PubMed] [Google Scholar]
- 11. Arvanitakis L, Geras-Raaka E, Varma A, Gershengorn MC, Cesarman E. Human herpesvirus KSHV encodes a constitutively active G-protein-coupled receptor linked to cell proliferation. Nature. 1997;385(6614):347-50 [DOI] [PubMed] [Google Scholar]
- 12. Cesarman E, Nador RG, Bai F, et al. Kaposi’s sarcoma-associated herpesvirus contains G protein-coupled receptor and cyclin D homologs which are expressed in Kaposi’s sarcoma and malignant lymphoma. J Virol. 1996;70(11):8218-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bais C, Santomasso B, Coso O, et al. G-protein-coupled receptor of Kaposi’s sarcoma-associated herpesvirus is a viral oncogene and angiogenesis activator. Nature. 1998;391(6662):86-9 [DOI] [PubMed] [Google Scholar]
- 14. Burger M, Burger JA, Hoch RC, et al. Point mutation causing constitutive signaling of CXCR2 leads to transforming activity similar to Kaposi’s sarcoma herpesvirus-G protein-coupled receptor. J Immunol. 1999;163(4):2017-22 [PubMed] [Google Scholar]
- 15. Cannon M. The KSHV and other human herpesviral G protein-coupled receptors. Curr Top Microbiol Immunol. 2007;312:137-56 [DOI] [PubMed] [Google Scholar]
- 16. Gershengorn MC, Geras-Raaka E, Varma A, Clark-Lewis I. Chemokines activate Kaposi’s sarcoma-associated herpesvirus G protein-coupled receptor in mammalian cells in culture. J Clin Invest. 1998;102(8):1469-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lane BR, Liu J, Bock PJ, et al. Interleukin-8 and growth-regulated oncogene alpha mediate angiogenesis in Kaposi’s sarcoma. J Virol. 2002;76(22):11570-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Geras-Raaka E, Arvanitakis L, Bais C, et al. Inhibition of constitutive signaling of Kaposi’s sarcoma-associated herpesvirus G protein-coupled receptor by protein kinases in mammalian cells in culture. J Exp Med. 1998;187(5):801-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Geras-Raaka E, Varma A, Ho H, Clark-Lewis I, Gershengorn MC. Human interferon-gamma-inducible protein 10 (IP-10) inhibits constitutive signaling of Kaposi’s sarcoma-associated herpesvirus G protein-coupled receptor. J Exp Med. 1998;188(2):405-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Geras-Raaka E, Varma A, Clark-Lewis I, Gershengorn MC. Kaposi’s sarcoma-associated herpesvirus (KSHV) chemokine vMIP-II and human SDF-1alpha inhibit signaling by KSHV G protein-coupled receptor. Biochem Biophys Res Commun. 1998;253(3):725-7 [DOI] [PubMed] [Google Scholar]
- 21. Mechoulam R, Shvo Y. Hashish, I: the structure of cannabidiol. Tetrahedron. 1963;19(12):2073-8 [DOI] [PubMed] [Google Scholar]
- 22. Lerner M. Marihuana: tetrahydrocannabinol and related compounds. Science. 1963;140(3563):175-6 [DOI] [PubMed] [Google Scholar]
- 23. Izzo AA, Borrelli F, Capasso R, Di Marzo V, Mechoulam R. Non-psychotropic plant cannabinoids: new therapeutic opportunities from an ancient herb. Trends Pharmacol Sci. 2009;30(10):515-27 [DOI] [PubMed] [Google Scholar]
- 24. McAllister SD, Christian RT, Horowitz MP, Garcia A, Desprez PY. Cannabidiol as a novel inhibitor of Id-1 gene expression in aggressive breast cancer cells. Mol Cancer Ther. 2007;6(11):2921-7 [DOI] [PubMed] [Google Scholar]
- 25. Ramer R, Rohde A, Merkord J, Rohde H, Hinz B. Decrease of plasminogen activator inhibitor-1 may contribute to the anti-invasive action of cannabidiol on human lung cancer cells. Pharm Res. 2010;27(10):2162-74 [DOI] [PubMed] [Google Scholar]
- 26. Yamada T, Ueda T, Shibata Y, et al. TRPV2 activation induces apoptotic cell death in human T24 bladder cancer cells: a potential therapeutic target for bladder cancer. Urology. 2010;76(2):509.e1-7 [DOI] [PubMed] [Google Scholar]
- 27. Torres S, Lorente M, Rodriguez-Fornes F, et al. A combined preclinical therapy of cannabinoids and temozolomide against glioma. Mol Cancer Ther. 2011;10(1):90-103 [DOI] [PubMed] [Google Scholar]
- 28. McKallip RJ, Jia W, Schlomer J, et al. Cannabidiol-induced apoptosis in human leukemia cells: a novel role of cannabidiol in the regulation of p22phox and Nox4 expression. Mol Pharmacol. 2006;70(3):897-908 [DOI] [PubMed] [Google Scholar]
- 29. Marcu JP, Christian RT, Lau D, et al. Cannabidiol enhances the inhibitory effects of delta9-tetrahydrocannabinol on human glioblastoma cell proliferation and survival. Mol Cancer Ther. 2010;9(1):180-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mechoulam R, Peters M, Murillo-Rodriguez E, Hanus LO. Cannabidiol: recent advances. Chem Biodivers. 2007;4(8):1678-92 [DOI] [PubMed] [Google Scholar]
- 31. Delgado T, Carroll PA, Punjabi AS, et al. Induction of the Warburg effect by Kaposi’s sarcoma herpesvirus is required for the maintenance of latently infected endothelial cells. Proc Natl Acad Sci U S A. 2010;107(23):10696-701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hansen A, Henderson S, Lagos D, et al. KSHV-encoded miRNAs target MAF to induce endothelial cell reprogramming. Genes Dev. 2010;24(2):195-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. El-Remessy AB, Al-Shabrawey M, Khalifa Y, et al. Neuroprotective and blood-retinal barrier-preserving effects of cannabidiol in experimental diabetes. Am J Pathol. 2006;168(1):235-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rajesh M, Mukhopadhyay P, Batkai S, et al. Cannabidiol attenuates high glucose-induced endothelial cell inflammatory response and barrier disruption. Am J Physiol Heart Circ Physiol. 2007;293(1):H610-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang X, Wang JF, Kunos G, Groopman JE. Cannabinoid modulation of Kaposi’s sarcoma-associated herpesvirus infection and transformation. Cancer Res. 2007;67(15):7230-7 [DOI] [PubMed] [Google Scholar]
- 36. Tammela T, Zarkada G, Wallgard E, et al. Blocking VEGFR-3 suppresses angiogenic sprouting and vascular network formation. Nature. 2008;454(7204):656-60 [DOI] [PubMed] [Google Scholar]
- 37. Zhang X, Wang JF, Chandran B, et al. Kaposi’s sarcoma-associated herpesvirus activation of vascular endothelial growth factor receptor 3 alters endothelial function and enhances infection. J Biol Chem. 2005;280(28):26216-24 [DOI] [PubMed] [Google Scholar]
- 38. Carroll PA, Brazeau E, Lagunoff M. Kaposi’s sarcoma-associated herpesvirus infection of blood endothelial cells induces lymphatic differentiation. Virology. 2004;328(1):7-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Masood R, Cesarman E, Smith DL, Gill PS, Flore O. Human herpesvirus-8-transformed endothelial cells have functionally activated vascular endothelial growth factor/vascular endothelial growth factor receptor. Am J Pathol. 2002;160(1):23-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jussila L, Valtola R, Partanen TA, et al. Lymphatic endothelium and Kaposi’s sarcoma spindle cells detected by antibodies against the vascular endothelial growth factor receptor-3. Cancer Res. 1998;58(8):1599-604 [PubMed] [Google Scholar]
- 41. Weninger W, Partanen TA, Breiteneder-Geleff S, et al. Expression of vascular endothelial growth factor receptor-3 and podoplanin suggests a lymphatic endothelial cell origin of Kaposi’s sarcoma tumor cells. Lab Invest. 1999;79(2):243-51 [PubMed] [Google Scholar]
- 42. Lohela M, Bry M, Tammela T, Alitalo K. VEGFs and receptors involved in angiogenesis versus lymphangiogenesis. Curr Opin Cell Biol. 2009;21(2):154-65 [DOI] [PubMed] [Google Scholar]
- 43. Bergamaschi MM, Queiroz RH, Chagas MH, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naive social phobia patients. Neuropsychopharmacology. 2011;36(6):1219-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bhattacharyya S, Morrison PD, Fusar-Poli P, et al. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010;35(3): 764-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Johnson JR, Burnell-Nugent M, Lossignol D, et al. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage. 2010;39(2):167-79 [DOI] [PubMed] [Google Scholar]
- 46. Paudel KS, Hammell DC, Agu RU, Valiveti S, Stinchcomb AL. Cannabidiol bioavailability after nasal and transdermal application: effect of permeation enhancers. Drug Dev Ind Pharm. 2010;36(9):1088-97 [DOI] [PubMed] [Google Scholar]
- 47. Nokta M. Oral manifestations associated with HIV infection. Curr HIV/AIDS Rep. 2008;5(1):5-12 [DOI] [PubMed] [Google Scholar]
- 48. Thomas A, Baillie GL, Phillips AM, et al. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. 2007;150(5):613-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mutlu AD, Cavallin LE, Vincent L, et al. In vivo-restricted and reversible malignancy induced by human herpesvirus-8 KSHV: a cell and animal model of virally induced Kaposi’s sarcoma. Cancer Cell. 2007;11(3):245-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bechara C, Chai H, Lin PH, Yao Q, Chen C. Growth related oncogene-alpha (GRO-alpha): roles in atherosclerosis, angiogenesis and other inflammatory conditions. Med Sci Monit. 2007;13(6):RA87-90 [PubMed] [Google Scholar]
- 51. Fimmel S, Devermann L, Herrmann A, Zouboulis C. GRO-alpha: a potential marker for cancer and aging silenced by RNA interference. Ann N Y Acad Sci. 2007;1119:176-89 [DOI] [PubMed] [Google Scholar]
- 52. Di Lorenzo G. Update on classic Kaposi sarcoma therapy: new look at an old disease. Crit Rev Oncol Hematol. 2008;68(3):242-9 [DOI] [PubMed] [Google Scholar]
- 53. Karpanen T, Egeblad M, Karkkainen MJ, et al. Vascular endothelial growth factor C promotes tumor lymphangiogenesis and intralymphatic tumor growth. Cancer Res. 2001;61(5):1786-90 [PubMed] [Google Scholar]
- 54. Petrova TV, Bono P, Holnthoner W, et al. VEGFR-3 expression is restricted to blood and lymphatic vessels in solid tumors. Cancer Cell. 2008;13(6):554-6 [DOI] [PubMed] [Google Scholar]
- 55. Bais C, Van Geelen A, Eroles P, et al. Kaposi’s sarcoma associated herpesvirus G protein-coupled receptor immortalizes human endothelial cells by activation of the VEGF receptor-2/KDR. Cancer Cell. 2003;3(2):131-43 [DOI] [PubMed] [Google Scholar]
- 56. Bahram F, Claesson-Welsh L. VEGF-mediated signal transduction in lymphatic endothelial cells. Pathophysiology. 2010;17(4):253-61 [DOI] [PubMed] [Google Scholar]
- 57. Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst. 2011;103(9):753-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Vieira J, O’Hearn P, Kimball L, Chandran B, Corey L. Activation of Kaposi’s sarcoma-associated herpesvirus (human herpesvirus 8) lytic replication by human cytomegalovirus. J Virol. 2001;75(3):1378-86 [DOI] [PMC free article] [PubMed] [Google Scholar]