Abstract
Background:
Questions remain as to the effect that obesity has on patients managed for symptomatic lumbar disc herniation. The purpose of this study was to determine if obesity affects outcomes following the treatment of symptomatic lumbar disc herniation.
Methods:
An as-treated analysis was performed on patients enrolled in the Spine Patient Outcomes Research Trial for the treatment of lumbar disc herniation. A comparison was made between patients with a body mass index of <30 kg/m2 (nonobese) (n = 854) and those with a body mass index of ≥30 kg/m2 (obese) (n = 336). Baseline patient demographic and clinical characteristics were documented. Primary and secondary outcomes were measured at baseline and at regular follow-up time intervals up to four years. The difference in improvement from baseline between operative and nonoperative treatment was determined at each follow-up period for both groups.
Results:
At the time of the four-year follow-up evaluation, improvements over baseline in primary outcome measures were significantly less for obese patients as compared with nonobese patients in both the operative treatment group (Short Form-36 physical function, 37.3 compared with 47.7 points [p < 0.001], Short Form-36 bodily pain, 44.2 compared with 50.0 points [p = 0.005], and Oswestry Disability Index, −33.7 compared with −40.1 points [p < 0.001]) and the nonoperative treatment group (Short Form-36 physical function, 23.1 compared with 32.0 points [p < 0.001] and Oswestry Disability Index, −21.4 compared with −26.1 points [p < 0.001]). The one exception was that the change from baseline in terms of the Short Form-36 bodily pain score was statistically similar for obese and nonobese patients in the nonoperative treatment group (30.9 compared with 33.4 points [p = 0.39]). At the time of the four-year follow-up evaluation, when compared with nonobese patients who had been managed operatively, obese patients who had been managed operatively had significantly less improvement in the Sciatica Bothersomeness Index and the Low Back Pain Bothersomeness Index, but had no significant difference in patient satisfaction or self-rated improvement. In the present study, 77.5% of obese patients and 86.9% of nonobese patients who had been managed operatively were working a full or part-time job. No significant differences were observed in the secondary outcome measures between obese and nonobese patients who had been managed nonoperatively. The benefit of surgery over nonoperative treatment was not affected by body mass index.
Conclusions:
Obese patients realized less clinical benefit from both operative and nonoperative treatment of lumbar disc herniation. Surgery provided similar benefit over nonoperative treatment in obese and nonobese patients.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
Obesity, commonly defined as a body mass index (BMI) of ≥30 kg/m2, affects one-third of the adult U.S. population, accounts for 10% of all U.S. health-care expenditures, and is associated with numerous clinical sequelae1-4. The impact of obesity on musculoskeletal and spinal disease, including low back pain, facet arthritis, and degenerative disc disease, has been well documented5-11. Although some studies have reported increased postoperative complications after spine surgery, multiple studies have demonstrated a beneficial effect from surgery on obese patients with the appropriate indications12-15.
Despite the recognized importance of the effect of obesity on musculoskeletal conditions, the link between obesity and lumbar disc herniation has received little attention. It is difficult to draw conclusions from prior studies on this topic, as the data are somewhat contradictory14,16-21.
Because of the lack of clarity on the role that obesity plays in patients with lumbar disc herniation, we sought to use the Spine Patient Outcomes Research Trial (SPORT) database to further explore this issue22. The purpose of this study was to determine if obesity affects outcomes following the treatment, both operative and nonoperative, of lumbar disc herniation. The hypothesis of the current study was that obese patients would have less clinical improvement over baseline function than nonobese patients after treatment for symptomatic lumbar disc herniation.
Materials and Methods
Study Design
Enrollment in SPORT was conducted at thirteen multidisciplinary spine practices in eleven states across the United States. The study design and methods of SPORT have been previously published22.
Patients
The SPORT protocol was approved by the human subject committees at each participating center. Criteria for inclusion in the lumbar disc herniation cohort were age greater than eighteen years, radicular pain for at least six weeks with a positive nerve root tension sign and/or neurological deficit, and a confirmatory cross-sectional imaging study demonstrating intervertebral disc herniation at a level and side corresponding to their symptoms. Exclusion criteria included cauda equina syndrome, a progressive neurological deficit, malignancy, scoliosis of >15°, herniation cephalad to L2, prior back surgery, and other established contraindications to elective surgery.
Study Interventions
Patients were offered participation in either a randomized cohort or a concurrent observational cohort. Those in the randomized cohort received computer-generated random treatment assignments. Those in the observational cohort chose their treatment with their physician. Patients in the operative treatment group were designated to undergo lumbar discectomy. Patients in the nonoperative treatment group were managed with minimum nonsurgical treatment, which included active physical therapy, education, counseling with home exercise instruction, and nonsteroidal anti-inflammatory drugs if tolerated. Additionally, patients could receive any therapies above the minimum required protocol that were deemed appropriate by their physician. Because of the extensive crossover in the randomized cohort in which some patients who had been randomized to the nonoperative treatment group instead received operative treatment and vice versa, and because of the similar baseline characteristics and outcomes when comparing the randomized and observational cohorts when analyzed by treatment, the two groups were combined in this as-treated analysis.
Study Measures
Data used in this study were obtained from patient questionnaires completed at baseline, six weeks, three months, six months, one year, two years, three years, and four years after enrollment or surgery. The primary outcome measures included the physical function and bodily pain domains of the Short Form-36 (SF-36)23 and the American Academy of Orthopaedic Surgeons MODEMS (Musculoskeletal Outcomes Data Evaluation and Management System) version of the Oswestry Disability Index24. The secondary outcome measures included patient self-reported improvement, work status, and satisfaction with current symptoms and with treatment25. Symptom severity was measured by means of the Low Back Pain Bothersomeness Index and the Sciatica Bothersomeness Index26-28. The SF-36 scales range from 1 to 100 points, with higher scores indicating less severe symptoms. The Oswestry Disability Index also ranges from 0 to 100 points, but higher scores indicate more severe symptoms. The Sciatica Bothersomeness Index ranges from 0 to 24 points, and the Low Back Pain Bothersomeness Index ranges from 0 to 6 points; in these indices, higher scores indicate more severe symptoms.
Statistical Analysis
The primary analyses compared changes in the clinical outcome measures from baseline as a function of the patient BMI at the time of enrollment in the study. BMI was calculated as the weight in kilograms divided by the height in meters squared according to National Institutes of Health (NIH) criteria29. For study purposes, the patients were divided into two groups on the basis of BMI: nonobese (BMI, <30 kg/m2) and obese (BMI, ≥30 kg/m2). The baseline characteristics of nonobese and obese patients were compared with use of a chi-square test for categorical variables and a t test for continuous variables. The primary analyses compared operative and nonoperative treatments with use of changes from baseline at each follow-up evaluation, with a mixed effects longitudinal regression model, including a random individual effect to account for the correlation between repeated measurements within individuals. A formal interaction term of the treatment and obesity was in the model for comparing the treatment effect in the subgroups. Because of the crossover, analyses were based on treatments actually received in the combined randomized and observational cohorts. In these as-treated analyses, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. Times were measured from the beginning of treatment, which was the time of surgery for the operative treatment group and the time of enrollment for the nonoperative treatment group. Therefore, all changes from baseline prior to surgery were included in the estimates of the nonoperative treatment effect. After surgery, changes were assigned to the operative treatment group with follow-up evaluations measured from the date of surgery. Repeated measures of outcomes were used as the dependent variables, and treatment received was included as a time-varying covariate.
To adjust for potential confounding, baseline variables associated with missing data or treatment received were included as adjusting covariates in longitudinal regression models (marital status, smoking status, compensation, herniation location, working status, depression, other comorbidities, self-rated health trend, duration of the most recent episode, or treatment preference). In addition, data for race, center, age, sex, and baseline outcome scores (for SF-36, the Oswestry Disability Index, the Sciatica Bothersomeness Index, and the Low Back Pain Bothersomeness Index) were included in the longitudinal regression models. Secondary and binary outcomes were analyzed with use of generalized estimating equations that assumed a compound symmetry working correlation structure. The outcomes were stratified by obesity, and outcomes between these subgroups at each time point were compared with use of a multiple-degrees-of-freedom Wald test. Across the four-year duration of follow-up, overall comparisons of area-under-curve between these subgroups were made with use of a Wald test.
Computations were done with use of SAS procedures PROC MIXED for continuous data and PROC GENMOD for binary and non-normal secondary outcomes (SAS version 9.1, Windows XP Pro; SAS Institute, Cary, North Carolina). Significance was defined as p < 0.05 on the basis of a two-sided hypothesis test with no adjustments made for multiple comparisons. Such adjustments were not made because the analyses of the current study are not multiple independent comparisons from which one is looking for a single significant result, but rather consist of the longitudinal assessment over time of different dimensions of outcomes, including symptoms, function, and disability.
Source of Funding
Funds were received from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) (U01-AR45444), the Office of Research on Women’s Health, the National Institutes of Health, the National Institute of Occupational Safety and Health, and the Centers for Disease Control and Prevention. The Multidisciplinary Clinical Research Center in Musculoskeletal Diseases is funded by NIAMS (P60-AR048094). Funds were used for statistical analysis and manuscript publication.
Results
In this study of patients with lumbar disc herniation, 854 patients had a BMI of <30 kg/m2 and were defined as nonobese and 336 patients had a BMI of ≥30 kg/m2 and were defined as obese. The mean BMI (and standard deviation) was 25.2 ± 2.8 kg/m2 for the nonobese group and 35.0 ± 4.5 kg/m2 for the obese group (p < 0.001). Differences between the groups at baseline are noted in the Appendix. Significant demographic differences were noted between the groups in sex, education, income under $50,000, and presence of a compensation claim. No significant difference was observed in the baseline work status of patients working full or part-time jobs when obese patients (59%) were compared with nonobese patients (61%) (p = 0.20). Some comorbidities differed significantly between the groups at baseline (see Appendix). The obese patient group had a higher percentage of hypertension, diabetes, depression, stomach problems, bowel problems, and other problems (see Appendix).
Compared with nonobese patients, obese patients had worse baseline scores for all three primary outcome measures: the Oswestry Disability Index (52.4 compared with 48.4 points; p = 0.003), the SF-36 bodily pain domain (25.0 compared with 27.9 points; p = 0.025), and the SF-36 physical function domain (32.5 compared with 39.7 points; p < 0.001). No significant baseline difference was observed between the groups in the SF-36 mental component summary score. A significantly higher percentage of obese patients had a preference for surgery compared with nonobese patients (55% compared with 48%; p = 0.003). Additionally, a significantly higher percentage of obese patients underwent surgery compared with nonobese patients (73% compared with 63%; p = 0.002) (see Appendix).
Operative details for those patients managed operatively are presented in Table I. When compared with nonobese patients, obese patients had a significantly greater operative time (mean, 86.5 compared with 72.3 minutes; p < 0.001), intraoperative blood loss (mean, 83.2 mL compared with 56.1 mL; p < 0.001), and length of stay (mean, 1.2 compared with 0.89 day; p < 0.001). No significant differences were observed between the groups with regard to the incidence of nerve root injury, wound hematoma, wound infection, perioperative mortality, recurrence, or additional surgery rate.
TABLE I.
Operative Treatments, Complications, and Events
| Variables | Nonobese Cohort | Obese Cohort | P Value |
| BMI (kg/m2) | <30 | ≥30 | |
| Lumbar disc herniation* (no. of patients) | 854 | 336 | |
| Discectomy level† (no. of patients) | |||
| L2-L3 | 11 (2%) | 3 (1%) | 0.65 |
| L3-L4 | 20 (4%) | 7 (3%) | 0.75 |
| L4-L5 | 202 (36%) | 110 (44%) | 0.026 |
| L5-S1 | 323 (58%) | 130 (52%) | 0.21 |
| Operation time‡ (min) | 72.3 ± 33.5 | 86.5 ± 43.5 | <0.001 |
| Blood loss‡ (mL) | 56.1 ± 90.8 | 83.2 ± 121.4 | <0.001 |
| Blood replacement† (no. of patients) | 0.76 | ||
| Intraoperative replacement | 5 (1%) | 1 (0%) | |
| Postoperative transfusion | 0 (0%) | 0 (0%) | |
| Length of stay‡ (d) | 0.89 ± 0.8 | 1.2 ± 1.2 | <0.001 |
| Intraoperative complications§ (no. of patients) | |||
| Dural tear or spinal fluid leak | 14 (3%) | 10 (4%) | 0.34 |
| Nerve root injury | 1 (0%) | 1 (0%) | 0.86 |
| Other | 1 (0%) | 2 (1%) | 0.47 |
| None | 536 (97%) | 233 (95%) | 0.23 |
| Postoperative complications or events# (no. of patients) | |||
| Nerve root injury | 0 (0%) | 1 (0%) | 0.68 |
| Wound hematoma | 3 (1%) | 1 (0%) | 0.77 |
| Wound infection | 13 (2%) | 5 (2%) | 0.97 |
| Other | 18 (3%) | 9 (4%) | 0.95 |
| None | 516 (94%) | 230 (94%) | 0.99 |
| Postoperative mortality (death) | |||
| Within six weeks after surgery | 0 (0%) | 0 (0%) | |
| Within three months after surgery | 1 (0.1%)‡ | 0 (0%) | |
| Additional surgery rate | |||
| One year | 32 (6%) | 14 (6%) | 0.962 |
| Two years | 40 (7%) | 24 (10%) | 0.235 |
| Three years | 43 (8%) | 28 (11%) | 0.105 |
| Four years | 51 (9%) | 31 (13%) | 0.149 |
| Recurrent disc herniation | 32 (6%) | 17 (7%) | |
| Complication or other | 13 (2%) | 8 (3%) | |
| New condition | 4 (1%) | 5 (2%) |
Includes patients from both the randomized arm and the observational arm.
N = 556 in the nonobese cohort and 250 in the obese cohort.
The values are given as the mean and the standard deviation.
N = 552 in the nonobese cohort and 246 in the obese cohort.
N = 550 in the nonobese cohort and 246 in the obese cohort.
The changes in primary outcome measures of the operatively managed patients are shown in Figure 1 and Table II. With regard to the change from baseline function to the four-year follow-up evaluation in the operative treatment group, when compared with nonobese patients, obese patients had significantly less improvement in scores for the SF-36 physical function (37.3 compared with 47.7 points; p < 0.001), the SF-36 bodily pain (44.2 compared with 50.0 points; p = 0.005), and the Oswestry Disability Index (−33.7 compared with −40.1 points; p < 0.001). No significant difference between groups was observed in the change from baseline in the SF-36 mental component summary score to the four-year follow-up evaluation. At the four-year follow-up evaluation, in the operative treatment group, when compared with nonobese patients, obese patients had significantly less improvement in the Sciatica Bothersomeness Index (−10.1 compared with −12.1 points; p < 0.001) and the Low Back Pain Bothersomeness Index (−1.9 compared with −2.3 points; p = 0.011). However, at baseline, no significant difference was observed in patient satisfaction or self-rated improvement when obese patients were compared with nonobese patients in the operative treatment group. At the four-year follow-up evaluation, 77.5% of obese patients and 86.9% of nonobese patients who had been managed operatively were working a full or part-time job (p = 0.014) (see Appendix).
Fig. 1.
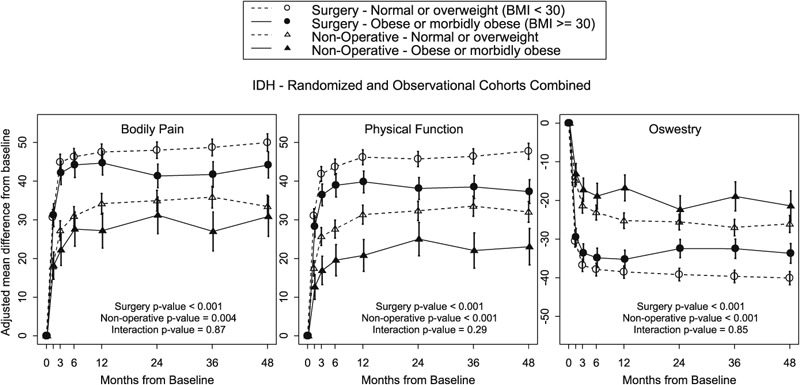
Change in primary outcome measures from baseline following surgical and nonoperative treatment of lumbar intervertebral disc herniation (IDH) in both obese and nonobese patients.
TABLE II.
Change from Baseline in Primary Outcome Measures of Operatively and Nonoperatively Managed Patients According to BMI at One, Two, Three, and Four Years of Follow-up Evaluation*†
| Change from Baseline |
||||
| Outcome Scale | One Year | Two Years | Three Years | Four Years |
| Operative treatment group | ||||
| SF-36 bodily pain‡ | ||||
| Nonobese patients | 47.5 ± 1.1 | 48 ± 1.1 | 48.7 ± 1.1 | 50.0 ± 1.2 |
| Obese patients | 44.7 ± 1.6 | 41.3 ± 1.6 | 41.7 ± 1.7 | 44.2 ± 1.7 |
| P value | 0.13 | <0.001 | <0.001 | 0.005 |
| SF-36 physical function‡ | ||||
| Nonobese patients | 46.2 ± 1 | 45.7 ± 1 | 46.4 ± 1 | 47.7 ± 1.1 |
| Obese patients | 39.8 ± 1.4 | 38.1 ± 1.4 | 38.5 ± 1.5 | 37.3 ± 1.6 |
| P value | <0.001 | <0.001 | <0.001 | <0.001 |
| SF-36 mental component summary‡ | ||||
| Nonobese patients | 7.7 ± 0.4 | 6.8 ± 0.4 | 7 ± 0.4 | 6.5 ± 0.5 |
| Obese patients | 7.9 ± 0.6 | 5.7 ± 0.6 | 5.1 ± 0.7 | 4.9 ± 0.7 |
| P value | 0.80 | 0.17 | 0.022 | 0.055 |
| Oswestry Disability Index§ | ||||
| Nonobese patients | −38.5 ± 0.8 | −39.2 ± 0.8 | −39.6 ± 0.8 | −40.1 ± 0.9 |
| Obese patients | −35.2 ± 1.2 | −32.4 ± 1.2 | −32.5 ± 1.3 | −33.7 ± 1.3 |
| P value | 0.023 | <0.001 | <0.001 | <0.001 |
| Nonoperative treatment group | ||||
| SF-36 bodily pain‡ | ||||
| Nonobese patients | 34.1 ± 1.4 | 34.9 ± 1.4 | 35.8 ± 1.4 | 33.4 ± 1.5 |
| Obese patients | 27.2 ± 2.3 | 31.2 ± 2.4 | 27 ± 2.6 | 30.9 ± 2.6 |
| P value | 0.008 | 0.17 | 0.002 | 0.39 |
| SF-36 physical function‡ | ||||
| Nonobese patients | 31.3 ± 1.2 | 32.3 ± 1.3 | 33.5 ± 1.3 | 32.0 ± 1.4 |
| Obese patients | 20.8 ± 2.1 | 25 ± 2.2 | 22 ± 2.3 | 23.1 ± 2.4 |
| P value | <0.001 | 0.004 | <0.001 | <0.001 |
| SF-36 mental component summary‡ | ||||
| Nonobese patients | 4.4 ± 0.6 | 4.2 ± 0.6 | 4 ± 0.6 | 4.6 ± 0.6 |
| Obese patients | 4.2 ± 0.9 | 5.4 ± 1 | 4.3 ± 1 | 3.4 ± 1.1 |
| P value | 0.84 | 0.29 | 0.80 | 0.32 |
| Oswestry Disability Index§ | ||||
| Nonobese patients | −25.2 ± 1 | −25.6 ± 1 | −27 ± 1.1 | −26.1 ± 1.1 |
| Obese patients | −16.8 ± 1.7 | −22.3 ± 1.8 | −18.9 ± 1.9 | −21.4 ± 2 |
| P value | <0.001 | 0.12 | <0.001 | 0.034 |
The values are given as the mean and the standard error in points.
The values have been adjusted for race, center, age, sex, marital status, smoking status, compensation, herniation location, working status, depression, other comorbidities (including stroke, diabetes, osteoporosis, cancer, fibromyalgia, chronic fatigue syndrome, posttraumatic stress disorder, alcohol or drug dependency, hypertension, migraine, anxiety, and diseases of the heart, lungs, liver, kidneys, blood vessels, nervous system, stomach, or bowels), self-rated health trend, duration of the most recent episode, treatment preference, and baseline score (for SF-36, the Oswestry Disability Index, the Sciatica Bothersomeness Index, and the Low Back Pain Bothersomeness Index).
The SF-36 scores range from 0 to 100 points, with higher scores indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100 points, with lower scores indicating less severe symptoms.
The changes in primary outcome measures of the nonoperatively managed patients are reported in Table II. With regard to the change from baseline function to the four-year follow-up evaluation, when compared with nonoperatively managed nonobese patients, nonoperatively managed obese patients also had significantly less improvement in the SF-36 physical function (23.1 compared with 32.0 points; p = 0.034) and the Oswestry Disability Index (−21.4 compared with −26.1 points; p < 0.001) scores, but no significant difference in the SF-36 bodily pain score (30.9 compared with 33.4 points; p = 0.39). No significant difference was observed between groups in the change from baseline in the SF-36 mental status component score at the four-year follow-up evaluation. No significant differences were observed in the secondary outcome measures, including work status, between obese and nonobese patients who had been managed nonoperatively (see Appendix).
At all follow-up time points and for all primary and secondary outcome measures, there was a significant treatment effect, in favor of surgery, in both the obese and nonobese groups (Table III) (see Appendix). The only exception to this was the measure of work status (see Appendix), for which the treatment effect was not significant in obese patients, suggesting that surgery offers no benefit over nonoperative treatment with regard to return to full or part-time work among obese patients. No significant difference in treatment effect was observed for any of the primary or secondary outcome measures when comparing obese and nonobese patients at the four-year follow-up evaluation (Table III) (see Appendix). This result suggests that surgery offers a similar benefit over nonsurgical treatment regardless of the patient BMI.
TABLE III.
Treatment Effect of Nonobese Patients Compared with Obese Patients for Primary Outcome Measures*
| Treatment Effect† |
||||
| Outcome Scale | One Year | Two Years | Three Years | Four Years |
| SF-36 bodily pain‡ (points) | ||||
| Nonobese patients | 13.4 (10 to 16.7) | 13.1 (9.7 to 16.5) | 12.9 (9.4 to 16.4) | 16.5 (12.9 to 20.2) |
| Obese patients | 17.5 (12.3 to 22.6) | 10.2 (4.8 to 15.6) | 14.7 (8.9 to 20.5) | 13.3 (7.4 to 19.3) |
| P value | 0.18 | 0.36 | 0.58 | 0.35 |
| SF-36 physical function‡ (points) | ||||
| Nonobese patients | 14.8 (11.8 to 17.9) | 13.4 (10.4 to 16.5) | 12.9 (9.7 to 16) | 15.7 (12.4 to 19) |
| Obese patients | 19 (14.4 to 23.7) | 13.1 (8.3 to 18) | 16.5 (11.3 to 21.6) | 14.3 (8.9 to 19.6) |
| P value | 0.13 | 0.91 | 0.23 | 0.64 |
| SF-36 mental component summary‡ (points) | ||||
| Nonobese patients | 3.3 (1.9 to 4.7) | 2.5 (1.2 to 3.9) | 2.9 (1.5 to 4.4) | 2 (0.5 to 3.4) |
| Obese patients | 3.7 (1.6 to 5.8) | 0.3 (−1.9 to 2.5) | 0.8 (−1.5 to 3.1) | 1.5 (−0.9 to 4) |
| P value | 0.74 | 0.083 | 0.12 | 0.77 |
| Oswestry Disability Index§ (points) | ||||
| Nonobese patients | −13.3 (−15.8 to −10.8) | −13.6 (−16.1 to −11.1) | −12.7 (−15.2 to −10.1) | −14 (−16.7 to −11.3) |
| Obese patients | −18.5 (−22.2 to −14.7) | −10.1 (−14 to −6.2) | −13.5 (−17.8 to −9.3) | −12.3 (−16.7 to −8) |
| P value | 0.021 | 0.13 | 0.72 | 0.50 |
The values are given as the mean, with the 95% confidence interval in parentheses. The values are adjusted for race, center, age, sex, marital status, smoking status, compensation, herniation location, working status, depression, other comorbidities (including stroke, diabetes, osteoporosis, cancer, fibromyalgia, chronic fatigue syndrome, posttraumatic stress disorder, alcohol or drug dependency, hypertension, migraine, anxiety, and diseases of the heart, lungs, liver, kidneys, blood vessels, nervous system, stomach, or bowels), self-rated health trend, duration of most recent episode, treatment preference, and baseline score (for SF-36, the Oswestry Disability Index, the Sciatica Bothersomeness Index, and the Low Back Pain Bothersomeness Index).
Treatment effect is the difference between the operative and nonoperative mean change from baseline. Analysis is done with use of a mixed model with a random subject intercept term. Treatment is a time-varying covariate in which the patient experience prior to surgery is attributed to the nonoperative arm and time is measured from enrollment and the patient postoperative outcomes are attributed to the operative arm and time is measured from time of surgery.
The SF-36 scores range from 0 to 100 points, with higher scores indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100 points, with lower scores indicating less severe symptoms.
Discussion
The results of the current study demonstrated that obese patients are more likely to undergo surgical intervention for lumbar disc herniation than nonobese patients and that obesity leads to increased operative time, blood loss, and length of hospital stay. The link between obesity and increased surgical intervention for lumbar disc herniation has been previously reported5,30. In two separate cross-sectional studies assessing >3700 patients, Böstman demonstrated a significant association between increased BMI and operative treatment of lumbar disc herniation5,30. Although the explanation of this finding remains largely unknown, the finding from the current study that obese patients have a pretreatment preference for surgery may provide the answer.
The perioperative findings in this study are at odds with the medical literature. A prospective study by Andreshak et al. comparing perioperative findings between obese and nonobese patients undergoing lumbar spine surgery demonstrated no difference in operative time, blood loss, or length of hospital stay12. The explanation for this difference in findings may be that the present study only included patients with a diagnosis of lumbar disc herniation and the study by Andreshak et al.12 evaluated patients with a variety of diagnoses. This discrepancy warrants further investigation because of the known increased risk of infection associated with these perioperative factors31,32.
We believe that our results largely supported the hypothesis that obesity is associated with worse outcomes after operative or nonoperative treatment of lumbar disc herniation. At the four-year follow-up evaluation, both operatively and nonoperatively managed obese patients had significantly less improvement in the primary outcome measures of the study. The only exception was the statistically similar improvement from baseline in the SF-36 bodily pain score in obese and nonobese patients managed nonoperatively. Disease-specific secondary outcome measures demonstrated a worse outcome for operatively managed obese patients in the Sciatica Bothersomeness Index, the Low Back Pain Bothersomeness Index, and work status. The published data on this topic are limited and serve to both support and refute the findings of the current study. In a review of nearly 1100 cases of sciatica treated nonoperatively, multivariate analysis showed that obesity was associated with adverse six-month outcomes19. More recently, Cole and Jackson evaluated the use of minimally invasive techniques to treat lumbar disc herniation in obese patients and concluded that this minimally invasive approach is the preferred technique to manage these patients because of favorable results and a trend toward reduced infectious complications33.
In the current study, recurrence of disc herniation and need for additional surgical procedures did not differ significantly between obese and nonobese patients. This finding contradicts other published literature21. In 2010, Meredith et al.21 retrospectively reviewed seventy-five patients who had undergone a microdiscectomy, eight (10.7%) of whom had experienced a recurrent herniation. Meredith et al. associated obesity with a twelve times higher likelihood of postoperative recurrent herniation and a thirty times higher likelihood of requiring a reoperation and concluded that weight loss counseling should be incorporated in preoperative discussions21. Because of the small sample size of that previous study, the findings of our study are likely more representative of the general population.
The current study advances the literature by identifying the expected results of operative and nonoperative intervention in obese patients with the specific diagnosis of symptomatic lumbar disc herniation. To our knowledge, this study has the largest series in the literature specific to lumbar disc herniation. This study also has the benefit of a prospective design, in which large samples of geographically diverse patients received treatment at multiple medical centers and were followed for several years. These attributes served to limit bias, increase the precision of our findings, and provide favorable generalizability of our results to clinical practice.
There were important methodological limitations to consider with this as-treated subgroup analysis of data. The initial SPORT study had been powered to compare operative treatment with nonoperative treatment for lumbar disc herniation and had not been powered for specific subgroup analyses. Even though the initial SPORT study22 had not been powered to detect differences in clinical outcome based on BMI, the current subgroup analysis did detect such differences with significance. Confounding baseline variables in the current study, including sex, level of education, income, the presence of a compensation claim, and medical comorbidities, differed between the obese patients and the nonobese patients. These differences may have affected the results of the present study. Other limitations included a lack of reassessment of BMI at specific postoperative time points. In other studies, obese patients had gained an average of 1.5 kg by the twenty-month average follow-up period34. This reassessment of BMI at specific postoperative time points would have helped to identify the effect of surgery on obesity and whether pain from a spine etiology limits the ability of obese patients to lose weight. Finally, the imprecision of BMI as a marker of obesity was another important limitation. Other measures, such as skin-fold thickness or body surface area, may be more specific measures of obesity to include in future studies.
Appendix
Tables showing the patient baseline demographic characteristics, comorbid conditions, clinical findings, and health status measures, the change from baseline in secondary outcome measures of operatively managed patients according to BMI, and the treatment effect of surgery measured by secondary outcome measures according to BMI are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables showing the patient baseline demographic characteristics, comorbid conditions, clinical findings, and health status measures, the change from baseline in secondary outcome measures of operatively managed patients according to BMI, and the treatment effect of surgery measured by secondary outcome measures according to BMI
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Centers for Disease Control and Prevention. Fact sheet – CDC health disparities and inequalities report – U.S., 2011. http://www.cdc.gov/minorityhealth/reports/CHDIR11/FactSheet.pdf. Accessed 2011 Aug 29.
- 2.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861-7 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Obesity and overweight: fact sheet. 2011. http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 2011 Aug 29.
- 4.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009 Sep-Oct;28(5):w822-31 Epub 2009 Jul 27 [DOI] [PubMed] [Google Scholar]
- 5.Böstman OM. Prevalence of obesity among patients admitted for elective orthopaedic surgery. Int J Obes Relat Metab Disord. 1994 Oct;18(10):709-13 [PubMed] [Google Scholar]
- 6.Yusuf E, Bijsterbosch J, Slagboom PE, Rosendaal FR, Huizinga TW, Kloppenburg M. Body mass index and alignment and their interaction as risk factors for progression of knees with radiographic signs of osteoarthritis. Osteoarthritis Cartilage. 2011 Sep;19(9):1117-22 Epub 2011 Jun 16 [DOI] [PubMed] [Google Scholar]
- 7.Runhaar J, Koes BW, Clockaerts S, Bierma-Zeinstra SM. A systematic review on changed biomechanics of lower extremities in obese individuals: a possible role in development of osteoarthritis. Obes Rev. 2011 Dec;12(12):1071-82 doi: 10.1111/j.1467-789X.2011.00916.x. Epub 2011 Aug 3 [DOI] [PubMed] [Google Scholar]
- 8.Fransen M, Woodward M, Norton R, Coggan C, Dawe M, Sheridan N. Risk factors associated with the transition from acute to chronic occupational back pain. Spine (Phila Pa 1976). 2002 Jan 1;27(1):92-8 [DOI] [PubMed] [Google Scholar]
- 9.Ohba T, Saito T, Kawasaki N, Maekawa S, Haro H. Symptomatic spinal epidural lipomatosis with severe obesity at a young age. Orthopedics. 2011 Jun 14;34(6):233 doi: 10.3928/01477447-20110427-25 [DOI] [PubMed] [Google Scholar]
- 10.Kalichman L, Guermazi A, Li L, Hunter DJ. Association between age, sex, BMI and CT-evaluated spinal degeneration features. J Back Musculoskelet Rehabil. 2009;22(4):189-95 [DOI] [PubMed] [Google Scholar]
- 11.Walid MS, Zaytseva N. History of spine surgery in older obese patients. Ger Med Sci. 2011 Feb 28;9:Doc05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997 Oct;10(5):376-9 [PubMed] [Google Scholar]
- 13.Gepstein R, Shabat S, Arinzon ZH, Berner Y, Catz A, Folman Y. Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clin Orthop Relat Res. 2004 Sep;(426):138-44 [DOI] [PubMed] [Google Scholar]
- 14.Kardaun JW, White LR, Shaffer WO. Acute complications in patients with surgical treatment of lumbar herniated disc. J Spinal Disord. 1990 Mar;3(1):30-8 [PubMed] [Google Scholar]
- 15.Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, Harrop J, Sharan A, Ratliff JK. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007 Apr;6(4):291-7 [DOI] [PubMed] [Google Scholar]
- 16.Heliövaara M. Body height, obesity, and risk of herniated lumbar intervertebral disc. Spine (Phila Pa 1976). 1987 Jun;12(5):469-72 [DOI] [PubMed] [Google Scholar]
- 17.Kanayama M, Togawa D, Takahashi C, Terai T, Hashimoto T. Cross-sectional magnetic resonance imaging study of lumbar disc degeneration in 200 healthy individuals. J Neurosurg Spine. 2009 Oct;11(4):501-7 [DOI] [PubMed] [Google Scholar]
- 18.Younes M, Béjia I, Aguir Z, Letaief M, Hassen-Zrour S, Touzi M, Bergaoui N. Prevalence and risk factors of disk-related sciatica in an urban population in Tunisia. Joint Bone Spine. 2006 Oct;73(5):538-42 Epub 2006 Apr 19 [DOI] [PubMed] [Google Scholar]
- 19.Bejia I, Younes M, Zrour S, Touzi M, Bergaoui N. Factors predicting outcomes of mechanical sciatica: a review of 1092 cases. Joint Bone Spine. 2004 Nov;71(6):567-71 [DOI] [PubMed] [Google Scholar]
- 20.Lean ME, Han TS, Seidell JC. Impairment of health and quality of life using new US federal guidelines for the identification of obesity. Arch Intern Med. 1999 Apr 26;159(8):837-43 [DOI] [PubMed] [Google Scholar]
- 21.Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010 Jul;10(7):575-80 Epub 2010 Mar 27 [DOI] [PubMed] [Google Scholar]
- 22.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006 Nov 22;296(20):2441-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473-83 [PubMed] [Google Scholar]
- 24.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine (Phila Pa 1976). 1996 Mar 15;21(6):741-9 [DOI] [PubMed] [Google Scholar]
- 25.Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987 Apr;12(3):264-8 [DOI] [PubMed] [Google Scholar]
- 26.Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, Singer DE. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976). 1996 Aug 1;21(15):1777-86 [DOI] [PubMed] [Google Scholar]
- 27.Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, Singer DE. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 1996 Aug 1;21(15):1787-94; discussion 1794-5 [DOI] [PubMed] [Google Scholar]
- 28.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976). 1995 Sep 1;20(17):1899-908; discussion 1909 [DOI] [PubMed] [Google Scholar]
- 29.National Institutes of Health. Assessing your weight and health risk. 2011. http://www.nhlbi.nih.gov/health/public/heart/obesity/lose_wt/risk.htm. Accessed 2011 Aug 29.
- 30.Böstman OM. Body mass index and height in patients requiring surgery for lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 1993 Jun 1;18(7):851-4 [DOI] [PubMed] [Google Scholar]
- 31.Boltz MM, Hollenbeak CS, Julian KG, Ortenzi G, Dillon PW. Hospital costs associated with surgical site infections in general and vascular surgery patients. Surgery. 2011 Nov;150(5):934-42 Epub 2011 Jun 15 [DOI] [PubMed] [Google Scholar]
- 32.Chikawa T, Sakai T, Bhatia NN, Sairyo K, Utunomiya R, Nakamura M, Nakano S, Shimakawa T, Minato A. Retrospective study of deep surgical site infections following spinal surgery and the effectiveness of continuous irrigation. Br J Neurosurg. 2011 Oct;25(5):621-4 [DOI] [PubMed] [Google Scholar]
- 33.Cole JS, 4th, Jackson TR. Minimally invasive lumbar discectomy in obese patients. Neurosurgery. 2007 Sep;61(3):539-44; discussion 544 [DOI] [PubMed] [Google Scholar]
- 34.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976). 2009 Mar 1;34(5):495-500 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables showing the patient baseline demographic characteristics, comorbid conditions, clinical findings, and health status measures, the change from baseline in secondary outcome measures of operatively managed patients according to BMI, and the treatment effect of surgery measured by secondary outcome measures according to BMI


