Abstract
Background:
Meniscal repair offers the potential to avoid the long-term articular cartilage deterioration that has been shown to result after meniscectomy. Failure of the meniscal repair can occur several years postoperatively. Limited evidence on the long-term outcomes of meniscal repair exists.
Methods:
We performed a systematic review of studies reporting the outcomes of meniscal repair at a minimum of five years postoperatively. Pooling of data and meta-analysis with a random-effects model were performed to evaluate the results.
Results:
Thirteen studies met the inclusion criteria. The pooled rate of meniscal repair failure (reoperation or clinical failure) was 23.1% (131 of 566). The pooled rate of failure varied from 20.2% to 24.3% depending on the status of the anterior cruciate ligament (ACL), the meniscus repaired, and the technique utilized. The rate of failure was similar for the medial and the lateral meniscus as well as for patients with an intact and a reconstructed ACL.
Conclusions:
A systematic review of the outcomes of meniscal repair at greater than five years postoperatively demonstrated very similar rates of meniscal failure (22.3% to 24.3%) for all techniques investigated. The outcomes of meniscal repair at greater than five years postoperatively have not yet been reported for modern all-inside repair devices.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Meniscal tears are the most commonly treated knee injury1,2. The meniscus is vital to normal function and longevity of the knee, as meniscal loss causes increased contact pressures and articular cartilage degeneration3-8. Meniscal repair techniques have evolved substantially in the last few decades, with open techniques replaced by arthroscopic techniques. Arthroscopic techniques have evolved as well and include inside-out, outside-in, and all-inside repairs. All-inside repair devices continue to evolve, with numerous devices currently available. Inside-out and all-inside repairs are most commonly used today.
Although numerous studies have reported one to two-year outcomes of meniscal repair, reports of outcomes at greater than five years are limited9. The failure rate of meniscal repair increases from early to long-term follow-up10. Numerous authors have reported failures at greater than two years postoperatively10-19, yet most published studies focus on short-term outcomes9. We performed a systematic literature review and meta-analysis to better define the rate of clinical failure after meniscal repair at greater than five years postoperatively. We hypothesized that the overall successful results noted at short-term follow-up would be maintained at longer-term follow-up. Utilizing pooled data and meta-analysis with a random-effects model, we determined the effect of repair type, medial or lateral location, and anterior cruciate ligament (ACL) status on the failure rate as indicated by the currently available literature.
Materials and Methods
Literature Review
We performed a systematic literature review to determine the outcomes of meniscal repair at greater than five years postoperatively. Inclusion criteria included a primary outcome of meniscal repair status, a minimum of five years of follow-up for all patients in the cohort, primarily adult patients, a cohort size of greater than ten patients, ≤30% loss to follow-up, and English-language publication. MEDLINE (January 1, 1966, to April 1, 2010), and Embase (January 1, 1974, to April 1, 2010) were queried with use of the terms ([meniscus OR meniscal] AND repair). These queries returned 1097 and 1135 results, respectively. Additionally, the Cochrane database was queried and yielded no additional studies. After the publication of several additional potentially eligible studies during manuscript preparation was noted, the queries were repeated on June 24, 2011, specifically focusing on results published in 2010 and 2011. These additional queries yielded 172 and 235 results, respectively.
Two of the reviewers examined the citation information for each result from the databases for relevant studies. Sixty-seven potentially relevant studies were identified, and the abstracts (and if necessary full manuscripts) of these studies were reviewed. The bibliographies of all reviewed manuscripts were also reviewed to identify other potential studies.
Study Design
Thirteen studies (reporting on fourteen patient cohorts) met the inclusion criteria and were the focus of the present study10-22. The studies were published between 1989 and 2011. Two of the studies represented Level-III evidence (retrospective comparative studies), and eleven studies represented Level-IV evidence (retrospective case series). For multiple studies by the same authors, only one study was included unless clear information on the absence of overlap between the cohorts was available. When necessary, attempts were made to contact the authors of the included studies to clarify reported data or to obtain missing data. One study included a subgroup of inside-out repairs and a subgroup of all-inside repairs, whereas all of the other studies utilized a single technique. Both reviewers extracted data on the failure rate, medial or lateral meniscal location, ACL status and treatment, tear chronicity, vascular zone, and radiographic and clinical outcomes with use of a standardized data collection tool. The rate of follow-up averaged 88% and ranged from 70% to 100% (see Appendix).
Failure of the meniscal repair was defined as clinical failure according to the criteria of the individual study. This generally included recurrent mechanical symptoms. The majority of clinical failures required operative intervention, at which time a persistent or recurrent meniscal tear was confirmed. However, individuals with clear evidence of clinical failure who chose not to undergo surgical intervention were also included as failures. Particular attention was paid to ensuring that early failures that were mentioned in a study but not included in later follow-up data were identified. Any discrepancies in data extraction between reviewers were resolved by mutual agreement.
Statistical Methods
Pooled analysis was utilized to compare failure rates, including among subgroups when data allowed. The heterogeneity of the studies was assessed qualitatively as well as quantitatively with use of the chi-square test. In order to account for between-study variation, a random-effects model was developed in Review Manager (RevMan) (version 5; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark); this software utilizes the method of Dersimonian and Laird to calculate an overall pooled estimate of effect. That method uses an inverse-variance approach to adjust the study weights according to the extent of heterogeneity present among the effects reported in the individual studies23. Random-effects models for tear location and ACL status were analyzed. In order to be included in the model, a study had to include patients with failure in each subgroup (e.g., ACL-deficient and ACL-intact) so that a comparison could be made.
Source of Funding
This project was partially funded by grant 5K23AR052392-05 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health and by a Career Development Supplement Award from the American Orthopaedic Society for Sports Medicine (AOSSM).
Results
A total of fourteen cohorts in thirteen studies were included. The repair technique was open in five cohorts11-13,15,21, inside-out in five14,18-20,22, outside-in in one16, and all-inside (with use of meniscal arrows) in three10,17,22. The Appendix summarizes the patient populations and follow-up durations of the included studies. A total of 566 knees were included, with an overall failure rate of 23.1% (131 of 566) at greater than five years. Results of all-inside repair were limited to techniques involving meniscal arrows, with no reports available on more recent implants. The minimum duration of follow-up in the studies ranged from five to 11.9 years (mean, 7.4 years), and the studies included twenty to ninety-five knees. Steenbrugge et al.22 reported a meniscal failure rate of 0% at a minimum of 11.9 years postoperatively for inside-out repairs and a rate of 4.0% at a minimum of 11.9 years for all-inside repairs. The failure rates reported in all other studies were at least 16.0%.
Repair Technique
The failure rate of open meniscal repair at greater than five years ranged from 16.0% to 29.0% (see Appendix). Pooled analysis of open meniscal repair revealed a failure rate of 23.1% (thirty-three of 143). Two of the cohorts12,15 in the analysis included only ACL-intact knees and had a pooled failure rate of 26.8% (fifteen of fifty-six); one cohort11 included only ACL-deficient knees (generally treated with repair or extra-articular reconstruction) and had a failure rate of 21.9% (seven of thirty-two).
The failure rate of outside-in meniscal repair at greater than five years was reported in a single study16 to be 23.9% (twenty-one of eighty-eight). This cohort included only ACL-intact knees. No other studies of outside-in meniscal repair met the inclusion criteria for the study.
The failure rate of inside-out meniscal repair at greater than five years ranged from 0% to 26.9%. Pooled analysis of inside-out meniscal repair revealed a failure rate of 22.3% (forty-one of 184). One study22 reported no failures, whereas the failure rates of the other four studies were 26.9%, 26.7%, 23.7%, and 20.7%. One study18 included thirty-five knees treated with ACL reconstruction in addition to meniscal repair; the failure rate was 28.6% (ten of thirty-five). Two studies14,20 included only ACL-intact knees and had failure rates of 26.9% and 23.7%.
The failure rates of all-inside meniscal repair at greater than five years were 4.0%, 28.4%, and 28.6%. Pooled analysis of all-inside meniscal repair revealed a failure rate of 24.3% (thirty-six of 148). One study10 included ACL-deficient knees treated with reconstruction and had a failure rate of 28.6% (eight of twenty-eight).
Tear Location
Eight studies12,13,15,16,18-20,22 included detailed information on the location (medial or lateral) of meniscal repairs as well as the location of failures. The pooled data included 190 repairs of the medial meniscus and 119 repairs of the lateral meniscus. The pooled failure rate for medial meniscal repair was 24.2% (forty-six of 190) compared with 20.2% (twenty-four of 119) for lateral meniscal repair. Among studies reporting failures, the failure rate of medial meniscal repair ranged from 17.4% to 36.7%, whereas the failure rate for lateral meniscal repair ranged from 6.7% to 42.9%. The rate of meniscal repair failure was higher in the medial meniscal repairs in four studies16,18-20, whereas the opposite was true in three other studies12,13,15.
A random-effects model for tear location did not show a significant difference in the failure rate (p = 0.17). A nonsignificant trend toward a slightly lower failure rate in lateral meniscal repairs was observed (Fig. 1).
Fig. 1.
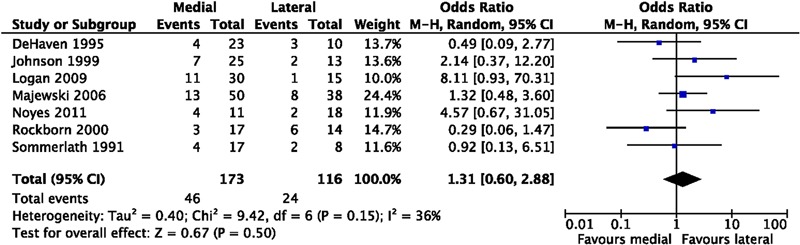
Random-effects model for the effect of meniscal tear location (medial or lateral) on the failure rate. M-H = Mantel-Haenszel, CI = confidence interval, and df = degrees of freedom.
ACL Status
Nine groups in eight studies12-16,18,20,22 included a subset of ACL-intact patients, and six groups in five studies10,11,13,18,22 included a subset of ACL-deficient patients. Three groups10,18,22 included a subset of patients treated with ACL reconstruction. The pooled rate of meniscal repair failure for ACL-intact knees was 22.7% (sixty-three of 278). The pooled rate of meniscal repair failure for ACL-deficient knees was 22.1% (thirty of 136), including 26.9% (eighteen of sixty-seven) for ACL-reconstructed knees.
A random-effects model for ACL status did not show a significant effect on the failure rate of meniscal repair (p = 0.86, Fig. 2). However, only three studies allowed for direct comparison between ACL-deficient and ACL-intact knees, with fifteen and four failures, respectively, in these groups.
Fig. 2.
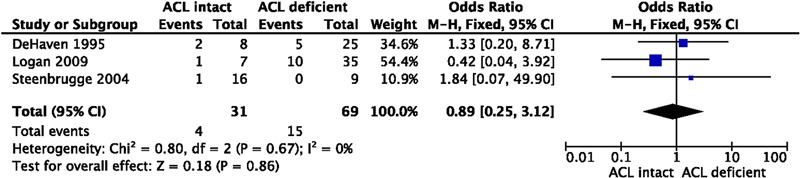
Random-effects model for the effect of anterior cruciate ligament (ACL) status (intact or deficient) on the failure rate. M-H = Mantel-Haenszel, CI = confidence interval, and df = degrees of freedom.
Rehabilitation
Twelve studies provided details regarding the weight-bearing status and immobilization utilized during postoperative rehabilitation. Older studies, including those using open repair techniques, were more likely to utilize strict non-weight-bearing and immobilization postoperatively. Four studies11,12,14,15 utilized strict non-weight-bearing and had a pooled failure rate of 25.7% (thirty-six of 140). Seven studies13,16-19,21,22 (eight groups) utilized partial weight-bearing and had a pooled failure rate of 21.7% (78 of 360). A single study allowed full weight-bearing in a brace and had a failure rate of 28.6% (eight of twenty-eight)10. Six studies11-15,21 utilized immobilization in a cast or splint postoperatively for at least four weeks and had a pooled failure rate of 23.7% (forty-seven of 198). Six studies10,16-19,22 (seven groups) allowed some degree of gentle early range of motion and had a pooled failure rate of 22.7% (seventy-five of 330).
Other Factors
Four groups in three studies13,15,22 included detailed information on the chronicity of the meniscal tears. Utilizing the definitions of acute and chronic tears provided in the individual studies, the pooled failure rates were 16.3% (eight of forty-nine) for acute tears and 15.5% (nine of fifty-eight) for chronic tears. Seven groups in six studies13,15,19-22 included detailed information on the vascular zone of the meniscal tears. Red-red meniscal zone repair had a pooled failure rate of 20.9% (twenty-nine of 139). Noyes et al.19 reported a failure rate of 20.7% (six of twenty-nine) for red-white meniscal tears. Limited information on meniscal tears in the white-white zone was present.
Timing of Failure
Six studies11,12,14,15,17,19 provided detailed information on repair failures occurring after two years postoperatively. Meniscal repair failures presenting two years or more postoperatively comprised 14.3% to 55.6% of all meniscal repair failures. Pooling of these studies revealed late failure (at more than two years) to represent 29.0% (twenty of sixty-nine) of all meniscal repair failures. Four other studies10,13,16,18 reported the mean length of time to meniscal failure, which ranged from 2.2 to 4.2 years postoperatively.
Other Outcomes
Six studies reported Lysholm knee scores after medium to long-term follow-up. Three studies12,13,15 indicated the mean Lysholm knee score for all meniscal repairs, with scores of 90, 95, and 96, respectively. Similarly, these studies reported Lysholm scores of >80 in 81% to 100% of patients. Five studies11,13,15-17 indicated the mean Lysholm score of the subgroup with successful meniscal repair, which ranged from 88 to 95. Two studies13,15 reported the mean Lysholm score of the subgroup with failed meniscal repair, which was 84 and 86, respectively (compared with 92 and 95 for the successful meniscal repair subgroup in the same study). Three studies10,14,17 indicated the mean International Knee Documentation Committee (IKDC) score in the subgroup with successful meniscal repair, with 90% to 100% having a normal or near-normal score.
Osteoarthritis
Five studies12-15,20 reported the prevalence of radiographic findings of osteoarthritis in all meniscal repairs with use of the Fairbank and/or Ahlbach classifications. The prevalence of radiographic findings of osteoarthritis ranged from 8% to 25%. These changes were generally mild (grade 1). Similarly, five studies13,15,16,19,21 reported the prevalence of radiographic findings of osteoarthritis in successful repairs, which ranged from 14% to 28%. Two studies13,15 allowed direct comparison of the prevalence of radiographic findings of osteoarthritis between successful and failed meniscal repairs. Both indicated higher rates of radiographic changes in failed repairs (56% compared with 14% and 57% compared with 15%, respectively).
Discussion
This systematic review of the outcomes of meniscal repair at greater than five years postoperatively demonstrated very similar rates of meniscal failure (22.3% to 24.3%) for all techniques. No outcomes of meniscal repair at greater than five years postoperatively have been reported for more recently developed all-inside devices. No significant difference in the rate of meniscal repair failure at long-term follow-up was seen for ACL-intact compared with ACL-deficient knees. The pooled rate of failure of medial meniscal repairs (24.2%) was slightly greater than that of lateral meniscal repairs (20.2%). Approximately 30% of all failures occurred after two years postoperatively. Our hypothesis regarding the maintenance of successful results at longer follow-up was not supported by the data, as the rate of repair failures was increased at intermediate-term follow-up compared with previously reported short-term results9.
Although numerous studies have reported short-term outcomes of various techniques of meniscal repair, relatively few have reported medium to long-term outcomes. Failure of meniscal repair after two years was not infrequent. In the present study, failures after two years represented nearly 30% of all failures. Additionally, in studies reporting the mean time to failure, the mean was uniformly greater than two years. Thus, the rate of meniscal repair failure appears to increase from short-term follow-up to medium to long-term follow-up. Lee and Diduch10 demonstrated an increase in the failure rate of meniscal repair with use of meniscal arrows from 9.4% at a mean of 2.3 years postoperatively to 28.6% at a mean of 6.6 years. An increase in the failure rate is likely to occur regardless of the repair technique and device. Lozano et al.9 reviewed the failure rate of all-inside meniscal repair and noted a similar trend.
Different methods of assessing meniscal repair healing have been reported, including clinical, second-look arthroscopy, and magnetic resonance imaging (MRI). Miao et al.24 recently compared these techniques and found that strict clinical evaluation resulted in lower estimates of the healing rate compared with MRI or second-look arthroscopy. A thorough clinical evaluation including history and physical examination remains the gold standard, and this may be supplemented with imaging studies when needed. Clinical failure requiring reoperation remains the most feasible basis on which to assess long-term outcomes of meniscal repair. In addition to reoperation, the definition of failure in the present study included clear evidence of clinical failure (generally mechanical symptoms). None of the included studies focused on the rate of failure assessed with use of second-look arthroscopy or MRI imaging.
Several studies have previously suggested a higher failure rate for medial compared with lateral meniscal repair14,18. We found four studies with a higher failure rate for medial meniscal repair and three studies with a higher failure rate for lateral meniscal repair. Overall, there was a small difference in the pooled failure rate between medial (24.2%) and lateral (20.2%) meniscal repairs. However, the results of the included studies were fairly heterogeneous and the actual difference in the failure rate was relatively small (Fig. 1).
ACL reconstruction has traditionally been thought, on the basis of the results of short-term studies, to be associated with a higher rate of successful meniscal healing compared with ACL-deficient25-27 and ACL-intact knees26,28-31. This has been hypothesized to be due to the increased blood in the joint associated with the surgically induced hemarthrosis and the more peripheral and vertical orientation of meniscal tears associated with ACL injuries32. However, in our systematic review of the medium to long-term outcomes of meniscal repair, ACL reconstruction was not associated with a lower failure rate. The failure rate was 22.7% in the eight studies (nine groups) reporting on meniscal repairs in ACL-intact knees compared with 26.9% in the three studies reporting on repairs (inside-out or all-inside) in ACL-reconstructed knees. However, our study may have had inadequate power to detect a difference between these subgroups. The number of studies reporting on long-term outcomes of meniscal repair combined with ACL reconstruction was somewhat limited, as older studies often included knees treated with ACL repair or extra-articular augmentation. Several recent studies have failed to demonstrate the benefit of ACL reconstruction on meniscal healing at medium to long-term time points10,18. However, in one study10, this may be attributed to the poor outcome of the all-inside repair device used. Our study failed to demonstrate improved rates of meniscal repair healing at greater than five years postoperatively.
Rehabilitation protocols after meniscal repair can vary from non-weight-bearing immobilization to full weight-bearing and immediate knee motion. Historically, open meniscal repairs were generally immobilized and treated with non-weight-bearing. More aggressive approaches now utilize various degrees of weight-bearing and knee motion postoperatively. Current approaches to rehabilitation after meniscal repair vary widely and generally rely on surgeon preference. The pooled rate of failure was relatively similar for non-weight-bearing protocols (25.7%) and partial weight-bearing protocols (21.7%). Only a single study allowed full weight-bearing. The pooled rate of failure did not differ between protocols utilizing immobilization (23.7%) and early knee motion (22.7%).
The rate of meniscal repair failure at greater than five years was relatively consistent in the included studies (16.0% to 29.0%), with the exception of the study by Steenbrugge et al.22 That study reported no failures among twenty inside-out repairs and a 4.0% rate of failure among twenty-five all-inside repairs. The authors documented ten patients lost to follow-up, all from the all-inside group. The authors documented variable tear locations relative to the periphery of the meniscus, including several white-white tears. Detailed information on the extent of clinical follow-up was not provided. Although the patient population, selection of tears to repair, operative technique, and indications for reoperation likely influence the rate of repair failure, the reason for such a large difference between that study and all other studies is unclear.
The present study has several limitations. The quality of a systematic literature review is dependent on the individual studies. The amount of detailed information on the characteristics of subgroup populations was highly variable among the included studies. When possible, the authors of the included studies were contacted to provide missing information, although such information was not always recoverable. There was inherent heterogeneity in the patient population, meniscal tear configurations, surgical technique, and postoperative rehabilitation among the included studies. However, this systematic review summarized the currently available literature on the medium to long-term outcomes of meniscal repair, and in some cases the results contradicted findings at earlier time points.
In summary, the outcomes of meniscal repair at greater than five years postoperatively demonstrated very similar rates of meniscal failure (22.3% to 24.3%) for all techniques. No outcomes of meniscal repair at greater than five years postoperatively have been reported for modern all-inside devices. At long-term follow-up, no significant difference in the rate of meniscal repair failure was seen for ACL-intact compared with ACL-deficient or ACL-reconstructed knees, and a small difference suggesting a higher failure rate for medial compared with lateral meniscal repair was observed.
Appendix
Tables summarizing the characteristics of the included studies are available with the online version of this article as a data supplement at jbjs.org.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Tables summarizing the characteristics of the included studies
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011 Jun 1;93(11):994-1000 [DOI] [PubMed] [Google Scholar]
- 2.Garrett WE, Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ, Harrast J, Derosa GP. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: part-II, certification examination case mix. J Bone Joint Surg Am. 2006 Mar;88(3):660-7 [DOI] [PubMed] [Google Scholar]
- 3.Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986 Jul-Aug;14(4):270-5 [DOI] [PubMed] [Google Scholar]
- 4.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009 Oct;22(4):347-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17(4):214-8 [DOI] [PubMed] [Google Scholar]
- 6.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008 Sep;90(9):1922-31 [DOI] [PubMed] [Google Scholar]
- 7.Lee SJ, Aadalen KJ, Malaviya P, Lorenz EP, Hayden JK, Farr J, Kang RW, Cole BJ. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006 Aug;34(8):1334-44 Epub 2006 Apr 24 [DOI] [PubMed] [Google Scholar]
- 8.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948 Nov;30B(4):664-70 [PubMed] [Google Scholar]
- 9.Lozano J, Ma CB, Cannon WD. All-inside meniscus repair: a systematic review. Clin Orthop Relat Res. 2007 Feb;455:134-41 [DOI] [PubMed] [Google Scholar]
- 10.Lee GP, Diduch DR. Deteriorating outcomes after meniscal repair using the Meniscus Arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure rate with long-term follow-up. Am J Sports Med. 2005 Aug;33(8):1138-41 Epub 2005 Jul 6 [DOI] [PubMed] [Google Scholar]
- 11.Sommerlath K, Hamberg P. Healed meniscal tears in unstable knees. A long-term followup of seven years. Am J Sports Med. 1989 Mar-Apr;17(2):161-3 [DOI] [PubMed] [Google Scholar]
- 12.Sommerlath KG. Results of meniscal repair and partial meniscectomy in stable knees. Int Orthop. 1991;15(4):347-50 [DOI] [PubMed] [Google Scholar]
- 13.DeHaven KE, Lohrer WA, Lovelock JE. Long-term results of open meniscal repair. Am J Sports Med. 1995 Sep-Oct;23(5):524-30 [DOI] [PubMed] [Google Scholar]
- 14.Eggli S, Wegmüller H, Kosina J, Huckell C, Jakob RP. Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. Am J Sports Med. 1995 Nov-Dec;23(6):715-20 [DOI] [PubMed] [Google Scholar]
- 15.Rockborn P, Gillquist J. Results of open meniscus repair. Long-term follow-up study with a matched uninjured control group. J Bone Joint Surg Br. 2000 May;82(4):494-8 [DOI] [PubMed] [Google Scholar]
- 16.Majewski M, Stoll R, Widmer H, Müller W, Friederich NF. Midterm and long-term results after arthroscopic suture repair of isolated, longitudinal, vertical meniscal tears in stable knees. Am J Sports Med. 2006 Jul;34(7):1072-6 Epub 2006 Feb 1 [DOI] [PubMed] [Google Scholar]
- 17.Siebold R, Dehler C, Boes L, Ellermann A. Arthroscopic all-inside repair using the Meniscus Arrow: long-term clinical follow-up of 113 patients. Arthroscopy. 2007 Apr;23(4):394-9 [DOI] [PubMed] [Google Scholar]
- 18.Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete: results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009 Jun;37(6):1131-4 Epub 2009 Mar 11 [DOI] [PubMed] [Google Scholar]
- 19.Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011 May;39(5):1008-17 Epub 2011 Jan 29 [DOI] [PubMed] [Google Scholar]
- 20.Johnson MJ, Lucas GL, Dusek JK, Henning CE. Isolated arthroscopic meniscal repair: a long-term outcome study (more than 10 years). Am J Sports Med. 1999 Jan-Feb;27(1):44-9 [DOI] [PubMed] [Google Scholar]
- 21.Muellner T, Egkher A, Nikolic A, Funovics M, Metz V. Open meniscal repair: clinical and magnetic resonance imaging findings after twelve years. Am J Sports Med. 1999 Jan-Feb;27(1):16-20 [DOI] [PubMed] [Google Scholar]
- 22.Steenbrugge F, Verdonk R, Hürel C, Verstraete K. Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surg Sports Traumatol Arthrosc. 2004 Jan;12(1):43-9 Epub 2003 Sep 26 [DOI] [PubMed] [Google Scholar]
- 23.Higgins J, Green S, Cochrane handbook for systematic reviews of interventions. West Sussex: John Wiley & Sons Ltd; 2008 [Google Scholar]
- 24.Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011 Apr;39(4):735-42 Epub 2011 Jan 10 [DOI] [PubMed] [Google Scholar]
- 25.Warren RF. Meniscectomy and repair in the anterior cruciate ligament-deficient patient. Clin Orthop Relat Res. 1990 Mar;(252):55-63 [PubMed] [Google Scholar]
- 26.Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy. 1997 Aug;13(4):433-7 [DOI] [PubMed] [Google Scholar]
- 27.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991 Nov-Dec;19(6):632-7; discussion 637-8 [DOI] [PubMed] [Google Scholar]
- 28.Scott GA, Jolly BL, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone Joint Surg Am. 1986 Jul;68(6):847-61 [PubMed] [Google Scholar]
- 29.Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs. Factors that effect healing. Am J Sports Med. 1994 Nov-Dec;22(6):797-802 [DOI] [PubMed] [Google Scholar]
- 30.Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992 Mar-Apr;20(2):176-81 [DOI] [PubMed] [Google Scholar]
- 31.Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005 Feb;21(2):167-75 [DOI] [PubMed] [Google Scholar]
- 32.Belzer JP, Cannon WD., Jr Meniscus tears: treatment in the stable and unstable knee. J Am Acad Orthop Surg. 1993 Oct;1(1):41-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest
Tables summarizing the characteristics of the included studies


