Abstract
We have developed a low dose Mindfulness Based Intervention (MBI-ld) that reduces the time committed to meetings and formal mindfulness practice, while conducting the sessions during the workday. This reduced the barriers commonly mentioned for non-participation in mindfulness programs. In a controlled randomized trial we studied university faculty and staff (n=186) who were found to have an elevated CRP level, >3.0 mg/ml, and who either had, or were at risk for cardiovascular disease. This study was designed to evaluate if MBI-ld could produce a greater decrease in CRP, IL-6 and cortisol than an active control group receiving a lifestyle education program when measured at the end of the 2 month interventions. We found that MBI-ld significantly enhanced mindfulness by 2-months and it was maintained for up to a year when compared to the education control. No significant changes were noted between interventions in cortisol, IL-6 levels or self-reported measures of perceived stress, depression and sleep quality at 2-months. Although not statistically significant (p=.08), the CRP level at 2-months was one mg/ml lower in the MBI-ld group than in the education control group, a change which may have clinical significance (Ridker et al., 2000, Wassel et al., 2010). A larger MBI-ld effect on CRP (as compared to control) occurred among participants who had a baseline BMI<30 (−2.67 mg/ml) than for those with BMI>30 (−0.18mg/ml). We conclude that MBI-ld should be more fully investigated as a low-cost self-directed complementary strategy for decreasing inflammation, and it seems most promising for non-obese subjects.
Keywords: mindfulness, CRP, IL-6, cortisol, intervention, randomized-trial, inflammation
Introduction
Current research suggests that chronic stress in our society is a contributing factor to the behaviors and physiology that have accelerated the increase in chronic disease states. Hence low-cost self-directed stress reduction programs could be of great assistance in managing this epidemic. One such candidate is mindfulness-based stress reduction (MBSR), which is a structured group program that utilizes mindfulness meditation to help manage a variety of adverse health issues (Ludwig and Kabat-Zinn, 2008).
Mindfulness is characterized by non-judgmental, moment-to-moment awareness of physical sensations, perceptions, affective states, thoughts and imagery. It involves sustained awareness of mental phenomena which arise during waking consciousness. As a form of receptive awareness, mindfulness may create an interval of time where one is able to view one’s mental landscape, including one’s behavioral options. One goal of mindfulness practice is to enable the individual to make conscious life choices, allowing for a greater appreciation of possible responses to life events. Mindfulness practice may create a resilience resource for enhancing health, and recovery from illness by exposing the self induced stress caused by the framing of internal and external events. Improvements have been noted in standardized mental health measures including quality of life scales, depression, anxiety, coping style, and other affective dimensions of disability following mindfulness training (Ludwig and Kabat-Zinn, 2008). For chronic disease, meditative practices that cultivate and enhance awareness (exposing thoughts as narratives of our thinking and not as reality) may modulate the experience of pain and/or improve the capacity to deal with pain (Morone et al., 2008, Zautra et al., 2008), enhance the management of type 2 diabetes (Hartmann et al., 2012) and improve psoriasis (Kabat-Zinn et al., 1998).
It has been suggested that mindfulness practice may engage several biological pathways, including immune and endocrine changes evidenced by an increase in antibody titers to influenza vaccine (Davidson et al., 2003), higher salivary IgA levels and lower salivary cortisol levels following an acute stressor (Tang et al., 2007). Furthermore, only 5 days of body-mind training improved regulation of the autonomic nervous system (heart rate variability and blood pressure) and it was associated with EEG activation in the frontal cortex (Tang et al., 2009).
Functional MRI imaging demonstrate that individual disposition toward mindfulness is associated with extensive prefrontal cortical activation and diminished bilateral amygdala activity (Creswell et al., 2007) indicating thoughtful response patterns rather than hyperemotional reaction to life events. Both effects are associated with more controlled regulation of inflammation via the hypothalamic-pituitary-adrenal axis, the autonomic nervous system and immune system (Cerqueira et al., 2008).
Research over the past two decades has established chronic inflammation as a pathophysiologic component of numerous disease processes including various cardiovascular disorders. Levels of the inflammatory peptide CRP, that are in the highest tertile of the normal range increase the risk two-fold for a myocardial infarction over the following three years (Ridker et al., 2000).
CRP not only predicts adverse cardiovascular events but it also appears to induce a variety of pro-inflammatory processes in the vascular endothelium (Paffen and DeMaat, 2006).Furthermore, in a longitudinal study of aging, higher CRP and IL-6 levels predicted decreased survival (Wassel et al., 2010). Psychological and behavioral factors have been shown to predict CRP levels in middle aged and older adults (Suarez, 2004), and waist circumference, latency to sleep, smoking, and perceived stress were independently associated with increased CRP levels (McDade et al., 2006).
A recent review of published clinical studies have pointed to the shortcomings of clinical MBSR investigations that we have attempted to address. These problems include small numbers of participants, lack of an active control group, the inclusion of only subjective endpoints, lack of details of participant characteristics that allow generalization of findings, insufficient details of treatment methods, inadequate documentation of protocol adherence by the participants, and infrequent use of biologic measures (Ludwig and Kabat-Zinn, 2008).
In our mindfulness intervention, we have adhered to core MBSR principles, the 8-week program duration, and inclusion of a retreat, but have reduced the time committed to meetings and formal practice, while conducting the sessions onsite during the workday (Klatt et al., 2009). This has reduced the barriers commonly mentioned for non-participation in MBSR programs. Similar modifications to weekly/daily mindfulness programs based on MBSR have emerged, for example shortened programs for oncology patients (Ott et al., 2006) and those who are at risk or have cardiovascular disease (Olivo et al., 2009). In our trial we studied university faculty and staff who were found to have an elevated CRP level, >3.0 mg/ml, and who either had or were at risk for cardiovascular disease. This study focused on working adults who could benefit from lifestyle intervention strategies. In comparing the mindfulness intervention to the lifestyle education program, we focused on three biologic measures of chronic stress and inflammation (CRP, IL-6 and cortisol).
Methods
PARTICIPANTS
Subjects were recruited from faculty and staff of The Ohio State University. Advertising promoted the trial as a life style intervention program and the types of interventions were not specified, with participants unaware of the intervention type until the first day of the actual intervention.
Exclusion criteria focused on conditions that enhance inflammation and included: a psychiatric disorder other than depression within the past year; pregnancy; experiencing a major life stress such as death in the immediate family in the past two months; alcohol intake in excess of 2 drinks per day (two 1.25 oz shots of liquor, two 12 oz containers of beer, or two 6 oz glasses of wine); smoking more than ½ pack of cigarettes per day; recreational drug use; vaccination during the past 2-months; a cold or other illness in the past month; a BMI of greater than 40; and conditions that could decrease inflammation such as exercising more than ½ hour per day and previous practice of mind-body relaxation techniques.
Inclusion criteria was a CRP level in the upper tertile of risk for cardiovascular disease, >3.0 mg/ml and less than 10 mg/ml (values over 10 suggest acute inflammation) in a screening value obtained at the OSU Clinical Research Center (CRC).
Medication use was permitted to increase the generalizability of results. Fifty six participants in the education and fifty four in the MBI-ld group were taking medications. The total number of medications used at baseline in the MBI-ld group (134) was similar to the number (126) in the education control group. The number of different drug classifications groups and medications known to influence inflammation were similar for both interventions. See Table 4. We asked about medications being started or discontinued before each visit. Two individuals in the education group and one in the MBI-ld group stopped an antidepressant during the 2-month intervention. In sensitivity analysis of the MBI-ld effect, we controlled for both medication use and diagnoses.
Table 4.
Participant Medication and Diagnoses
| Medication | Diagnosis | ||||
|---|---|---|---|---|---|
| Education | MBI-ld | Education | MBI-ld | ||
| n (%) | n (%) | n (%) | n (%) | ||
| Anti-depressant | 27 (29) | 19 (20) | Depression | 29 (32) | 28 (30) |
| Birth control pill/Estrogen | 12 (13) | 18 (19) | Hypertension | 18 (20) | 22 (23) |
| BetaBlocker | 17 (19) | 21 (23) | Hyperlipidemia | 15 (16) | 18 (19) |
| Diuretics | 11 (12) | 9 (10) | GERD | 11 (12) | 10 (11) |
| NSAIDS | 9 (10) | 14 (15) | Osteoarthritis | 7 (8) | 9 (10) |
| Proton pump Inhibitor | 11 (12) | 9 (10) | Diabetes | 6 (7) | 5 (5) |
| Statins | 12 (13) | 12 (13) | |||
STUDY PROTOCOL
Based on our inclusion and exclusion criteria we accrued 186 patients with a CRP level greater than 3 mg/ml following their initial screening visit. They were consented and received $350 for their participation in the study. One week later, at a second visit to the CRC prior to randomization, they returned their salivary cortisol samples which had been obtained 20 min after arising, noon, 5 pm and at bedtime over three days at 7 day intervals. Cortisol collection time was uniformly two weeks pre intervention and the two week period immediately after the intervention for all subjects. At this visit baseline blood pressure, pulse rate, BMI, and a blood sample for CRP and IL-6 were obtained between 8 and 11 am to control for diurnal variation.
Thereafter, subjects were randomly assigned, using permuted blocks of size of 6. Within each block the assignment to the MBI-ld intervention or an education control was randomly ordered and balanced (3 in each group). Assigned subjects began their cohort’s intervention within one week of completing pre-study measures. All members of the research team were blinded to group assignment, except the instructors of the intervention and active control group. We stratified subjects into 2 BMI categories (< or >32), and randomized within each to ensure balance on this important indicator of inflammation. The median BMI was close to 32, so we had 92 subjects in the BMI<32 and 94 in the BMI>32 strata.
Between the screening visit and the invitation to return for randomization, subjects were asked to fill out a daily diary and questionnaires online using StudyTRAX (ScienceTRAX, Macon, GA, 2006) as well as obtain the salivary samples for cortisol determinations. Subjects were randomized in 6 different cohorts in order to keep the group size under 18 in each intervention, either MBI-ld or education.
Following the intervention the baseline studies were performed at 2-months. This trial was designed as an 8 week intervention with baseline and post intervention measurements. We asked participants, however, if they would continue to practice their interventions and return to complete questionnaires and a blood draw at 6 and 12 months to better evaluate changes over time, especially sustainability of any effects.
INTERVENTIONS
Mindfulness
MBI-ld was designed as a stress reduction program to be delivered on-site that included reflective writing, sharing among participants, mindfulness instruction, yoga, and formal mindfulness meditation, similar to traditional MBSR. MBI-ld augmented the yoga stretches with gentle background music as compared to traditional MBSR.
In this program we have retained the core components true to typical MBSR, only reducing the time spent on each component. The traditional group meeting time in MBSR is 2.5–3 hours per week and approximately 45 minutes per day in formal mindfulness practice. In MBI-ld, meeting time was reduced to one onsite lunchtime hour per week and formal practice to 20 minutes/day via prerecorded CD’s. Didactic presentation of the impact of chronic stress on health followed that of traditional MBSR. Group discussion (limited to 10–15 min), concerned practical daily challenges to being mindful while working full time. The sessions were conducted during the workday. Weekly sessions were held for 8 weeks. A comparison between traditional MBSR and MBI-ld is included in table 1.
Table 1.
Comparison Between MBSR and MBI-ld
| Length of Intervention |
Intervention Location |
Group Meeting Time |
Format of Group Weekly Meeting |
Daily Homework |
|
|---|---|---|---|---|---|
| MBSR | 8 weeks | Typically a location not a work site | 2.5–3 hours/week, plus one full day “retreat” | Standard MBSR program, Yoga movement is often done from the floor. | 45 minutes of mindfulness meditation |
| MBI-ld | 8 weeks | Usually on site location (worksite for a worksite study) | 1 hour/week, plus one 2 hour “retreat” | Standard MBSR program, Yoga movement is done standing or seated. Music is in background | 20 minutes of mindfulness meditation, Music is in background |
All instruction was conducted with the participants in chairs, or standing behind the chair. Loose fitting professional clothing was recommended to allow for movement. The veteran mindfulness Instructor was the same for all cohorts, held a PhD in Education and in 2003 had attended the 9 day MBSR training for Health Professionals. She has used mindfulness in her personal meditation practice and university classes since 1995. Attendance at weekly meetings was recorded and participants made entries onto TeleForm diaries each day to track informal and formal practice. These diary entries were collected each week.
Education Control Group
Our active control was a lifestyle education group, which provided an information-based approach enabling individuals to make health decisions based on scientific health information. The didactic lectures were based on concepts presented in the text “The Culprit and the Cure: Why lifestyle is the culprit behind America’s poor health and how transforming that lifestyle can be the cure” by Steven G. Aldana, PhD (2005). This was an accessible text that summarized the scientific research behind the health information presented by the popular media, bridging the gap between these two sources of health information. Homework for this group was 30 minutes of text reading/day to control for practice time of the MBI-ld group. The Instructor held a PhD in Exercise Physiology and worked with all cohorts.
Eight weekly 1 hour education sessions were also presented to the control subjects and homework reading was assigned that took the same time as the mindfulness exercises in the MBI-ld group (Table 2). The weekly reading homework was evidenced by quiz scores on weekly reading assigned. The amount of interaction time with the leaders of both interventions was identical.
Table 2.
Intervention Comparison
| Week | MBI-ld | Education Control |
|---|---|---|
| 1 | Willingness towards daily practice | Let science be your guide; Health in America |
| 2 | Cultivating mindful sleep | Food and your health |
| 3 | Supported by the breath | Bad fats and health; A good nutrition line up |
| 4 | Mindful eating | Exercise; What exercise can do for you |
| 5 | Movement through balance | Stress and your body; Importance of exercise |
| 6 | Centering through sensation | Being physically active for life |
| 7 | Clarity and release | Weight loss as a healthy lifestyle side effect |
| 8 | Strength of the mountain | Putting it all together |
The duration of each weekly meeting was 60 minutes with the exception of week 4, which was 120 minutes. The daily practice was 20 minutes.
During week four in each group a “retreat” style meeting occurred in which the participants further developed their understanding of the weekly themes, allowing for a deeper/longer meditation practice in the MBI-ld group.
ASSAYS
CRP
High sensitivity-CRP was analyzed using chemilluminescence methodology with the Immulite 1000 (Diagnostic Products Corporation, Los Angeles, CA). Sensitivity for this assay is 0.01 mg/dl. The intra-assay coefficient of variation was 3.8% and inter-assay coefficient of variation was 7.4%.
Interleukin 6
IL-6 was measured using a electrochemiluminescence method with ultra-sensitive kits purchased from Meso Scale Discovery (Gaithersburg, MD). Plates were read using the Meso Scale Discovery Sector Imager 2400. Sensitivity is 0.3 pg/ml. The intra-assay coefficient of variation for IL-6 is 2.8% and the inter-assay coefficient of variation is 12.5%.
Salivary Cortisol
Determinations are made using the Cortisol Coat-A-Count RIA (Diagnostic Products Corporation, Los Angeles, CA). Intra-assay variation is 4.3% and inter-assay variation is 5.2%. Sensitivity was adequate for this population at 0.025 ug/dl.
Leptin
Determinations were made using the Leptin RIA kit (Millipore Corporation, St. Charles, MO). Sensitivity is 0.5 ng/ml. Intra-assay coefficient of variation is 4.2% and inter-assay coefficient of variation is 4.5%.
QUESTIONNAIRES
Perceived Stress Scale (PSS)
Perceived stress has been associated with vulnerability to illness and injury. The Perceived Stress Scale, developed by Cohen et. al. (1988) is a 10 item scale and the most widely used psychological instrument for measuring the perception of stress. It is a measure of the degree to which situations in life are appraised as stressful. Items are designed to evaluate how overloaded, unpredictable and uncontrollable one finds his or her life. It also queries current levels of experienced stress.
Sleep
Sleep disturbance is both symptomatic of ill health and also is a vulnerability factor. The Pittsburgh Sleep Quality Index (PSQI) is a self-rated instrument that assesses sleep quality and sleep dysfunction over a one-month interval (Buysse, et al., 1998). It has good diagnostic sensitivity and specificity (a score of 6 or above yields a diagnostic sensitivity of 89.6% and a specificity of 86.5%) in distinguishing good and poor sleep. The scale yields a total score as well as 7 sub-scales which include subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction.
Depressive Symptoms
Depressive symptoms were assessed using the Center for Epidemiological Studies Depression (CES-D) 20-item scale (Radloff, 1977). The CES-D has been widely used to measure depressive symptomatology and has excellent psychometric characteristics. The 20 symptom-related items of the CES-D ask about how often one experienced depressive cognitions, affect, and behaviors during the past one week e.g., feeling depressed and lonely, disturbed appetite and sleep. Scores range from 0=none of the time or rarely to 3=most or all of the time. Scores of 16 or above reflect clinically significant levels of depressive symptoms.
Mindfulness
The Toronto Mindfulness Scale (TMS) is a 13 item measure that characterizes mindfulness as a state of curious, decentered awareness of one’s experience that is distinct from anxiously preoccupied and ruminative states of self-focused attention. The TMS scores increase with increasing mindfulness meditation experience and mindfulness interventions (Lau et al., 2006).
PRIMARY AND SECONDARY OUTCOMES
This study was designed to determine if MBI-ld could produce a greater decrease in biologic measures of chronic stress and inflammation (CRP, IL-6 and cortisol) than a standard lifestyle education program. We measured these primary outcomes at baseline prior to randomization and then again immediately after the 8 week program.
For cortisol, before randomization and post 8 week intervention participants were asked to collect saliva for cortisol measurements on 3 days (days 2, 8 and 14 of a 2-week period) at 20 minutes post rising, noon, 5 pm, and bedtime. We used the average of three cortisol measurements (noon, dinner, and bedtime) across the 3 days as our primary cortisol outcome. The slope of decline of cortisol from early morning to bedtime can be an indicator of risk and survival from cardiovascular disease (Kumari et al., 2011). In a sensitivity analysis, we used the difference between the level obtained at 20 minutes after rising and the average of the levels at dinner and bedtime, and averaged these across the 3 days.
Secondary outcomes included measures of depression, perceived stress, and sleep quality. These were also measured at baseline and immediately after the completion of the intervention. Finally we included a measure of self-reported mindfulness to establish the direct effect of the intervention.
SUSTAINABILITY OF OUTCOMES
At six months and 12 months we asked subjects to return for selected measurements to determine the sustainability of any effects seen immediately after the intervention.
STATISTICAL METHODS
We planned a global hypothesis testing strategy for the three primary endpoints at 2-months. It strongly controls type I error at alpha=.05 across all three outcomes while achieving the highest power for consistent differences between groups for the multiple measures (Lehmacher et al., 1991, Reitmeir and Wassmer, 1996). The global testing strategy involved testing an equally weighted average of estimated differences between the groups across the 3 measures after maximum-likelihood standardization of the variance of measures to 1.0 (Lin et all., 2000, Roy, 2003). The planned global test was double sided at alpha=.05. To obtain the global test, we used SAS’s Proc Mixed’s (2011) multivariate capabilities.
A multivariate longitudinal model with: overall group effects, group × measure interactions, baseline as a dependent variable, and BMI dichotomy (corresponding to stratification used in randomization) provided the measure-specific estimates of the difference between the two randomized groups at 2-months (Liu et al., 2009). Using a longitudinal model with baseline as a dependent variable as compared to using baseline as a covariate has certain advantages in reducing missing data bias (Liu et al., 2009). Consistent with the intention to treat principle, this longitudinal model allowed us to include in the hypothesis testing all 186 participants who were randomized.
To strongly control type I error, a closed hypothesis testing strategy was planned to test each of the three individual measures separately (Reitmeir and Wassmer, 1996). With the ninety-three subjects randomized to each of the two groups, we had power of over 80% for the global test under the assumption of consistent effect sizes of 0.34 standard deviations for each of the three measures. This power conservatively assumed an average correlation of 0.5 across the three measures and 10% missing data at follow-up. We considered this a preliminary trial, because the power for the individual tests of the three outcomes was sufficient at 80% only for a substantial effect size of 0.5 standard deviations, which is larger than we expected. The missing at random (MAR) assumption was used to adjust for potential missing data bias (Little, 1995, Schafer, 1997). Sensitivity/exploratory analyses were used to verify main findings, and to identify biases or sub-group interaction effects.
Results
PRIMARY
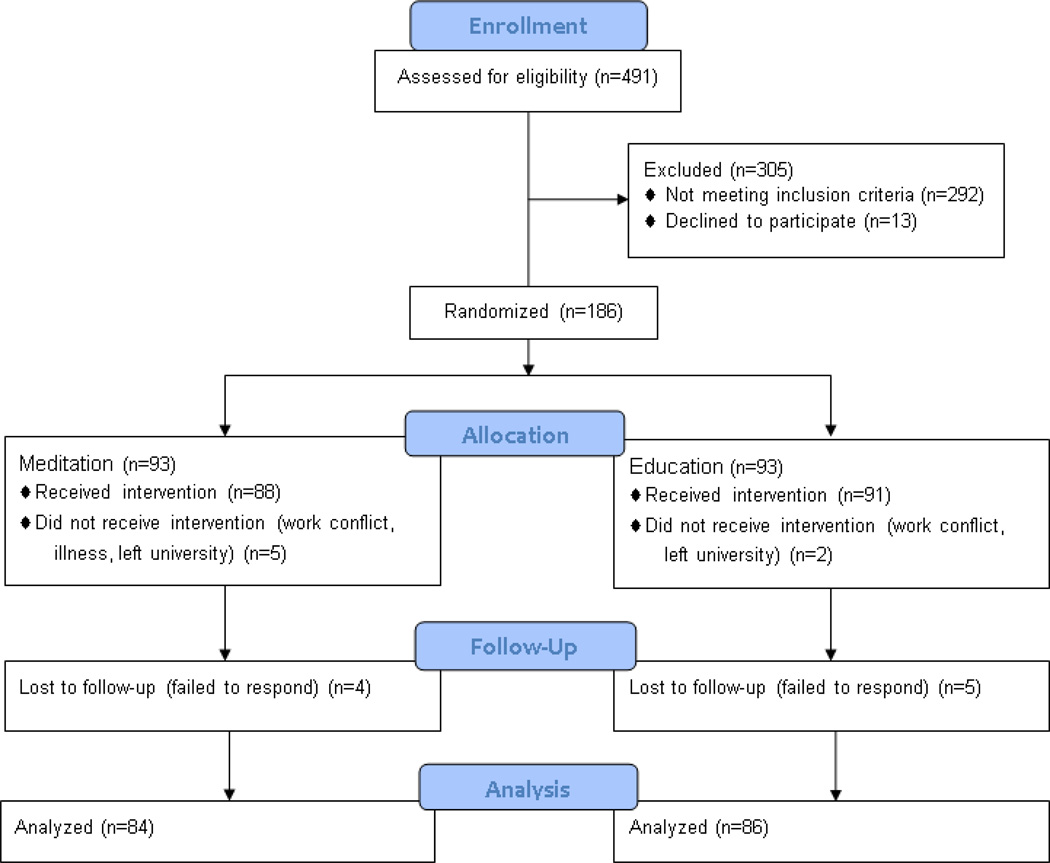
Figure 1 provides a description of the number of subjects that met inclusion/exclusion criteria, consented, and were randomized. The mean CRP at screening was 6.00 with a standard deviation of 2.3. The mean CRP at baseline (approximately 3 weeks post screen) dropped to 5.5, presumably because of regression to the mean. The correlation between screen and baseline CRP levels was 0.49.
Figure 1.
Recruitment and Retention Table
Of those who met criteria (199) almost all were randomized to the two arms (total trial n=186). Only 13 individuals dropped out (7%) because of an inability to make the time commitment required for the study. Three subjects were missing at least one of the baseline biomarkers (1 missing CRP and IL-6, and 2 missing cortisols). For the post intervention (2-months) measures we had more missing data. A total of 16 subjects (8.6%) did not return for blood samples and so were missing both IL-6 and CRP. In addition, one subject’s 8-week CRP was eliminated because it was extremely high relative to others and to his/her screen (probable infection), and the same for another’s IL-6 value. Identification of these outliers was done while blinded to group membership, and before any longitudinal models were fitted. Both happened to be in the MBI-ld group. Nine subjects had IL-6 and CRP measurements, but did not provide saliva samples for post intervention cortisol measurement.
Table 3 provides a comparison of the groups at baseline, prior to randomization. Note that they were similar on all variables. The groups were also comparable in regard to medication class and prior diagnoses (Table 4).
Table 3.
Comparison of Randomized Groups at Baseline
| Variables | Education (n=93) Mean (SE) (n) |
MBI-ld (n=93) Mean (SE) (n) |
95% CI for the difference of Education − MBI-ld |
|---|---|---|---|
| Age | 49 (0.8) (93) | 51 (0.8) (92) | −4.0, 0.4 |
| Female % | 87% (3%) (93) | 88% (3%) (91) | −10%, 9% |
| BMI | 32.4 (0.5) (93) | 32.8 (0.5) (93) | −1.9, 1.1 |
| CRP | 5.3 (0.4) (93) | 5.6 (0.4) (92) | −1.5, 0.9 |
| IL-6 | 1.7 (0.3) (93) | 1.9 (0.3) (92) | −1.0, 0.6 |
| Cortisol (mean of noon, 5pm, bed) | 0.15 (.03) (92) | 0.10 (.01) (92) | −0.11, 0.01 |
| PSS | 19.8 (0.3) (91) | 19.7 (0.3) (93) | −1.1, 0.7 |
| CES-D | 16.3 (0.5) (91) | 16.7 (0.5) (93) | −1.1, 1.9 |
| TSM | 1.4 (0.06) (89) | 1.4 (0.06) (86) | −0.2, 0.2 |
| PSQI | 8.4 (0.3) (91) | 8.7 (0.3) (92) | −0.6, 1.2 |
| Blood Pressure Systolic/Diastolic | 124/76 (1) (92) | 123/76 (1) (93) | −4.0, 2 |
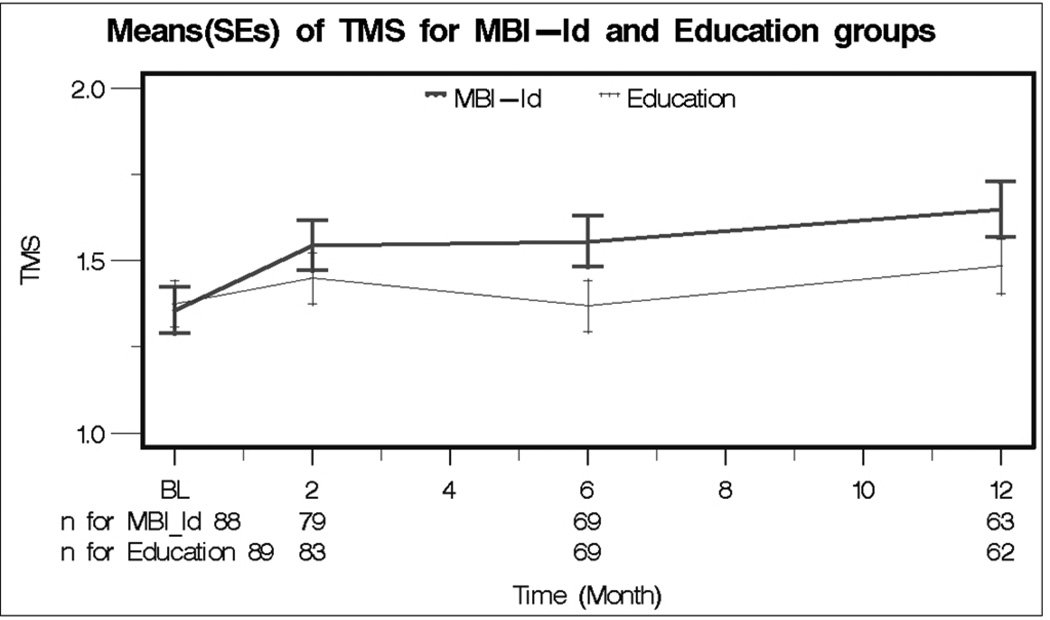
The mindfulness intervention was effective as the MBI-ld group demonstrated greater self-reported mindfulness than the education group at 2-months. This difference was sustained at 6 and 12 months (p=0.03) (Figure 2).
Figure 2.
Means (SEs) of Toronto Mindfulness Scale (TMS) for Meditation and Education groups
Table 5 provides estimates of the difference between the MBI-ld and the education control on the three primary outcomes post intervention (2-months). Since lower values are better for all three measures, a negative sign for these difference estimates is in the direction of superiority for the MBI-ld mindfulness group. The results of our formal global/closed hypothesis testing strategy proved to be non-significant. The global test p-value was 0.27, which makes the trial inconclusive according to our hypothesis testing strategy.
Table 5.
Effect of MBI-ld vs. Education Control at Two Months on CRP, IL-6, and Cortisol
| Biomarkers | Post Mean for MBI-ld Groupa |
Post Mean for Education Groupa |
MBI-ld − Education (Effect Estimates) |
Standard Errors |
Effect Size in SD Units |
p-Valueb |
|---|---|---|---|---|---|---|
| CRP | 4.70 | 5.67 | −0.97 | 0.56 | −0.23 | 0.08 |
| IL-6 | 1.91 | 1.76 | 0.15 | 0.16 | 0.05 | 0.36 |
| Cortisol (mean of noon, 5pm, bed) |
0.11 | 0.12 | −0.01 | 0.02 | −0.07 | 0.61 |
Estimates of 2-month means based on the multivariate longitudinal modeling.
These are double sided p-values uncorrected for multiplicity. The global test of the average effect size across the 3 biomarkers was the first stage of planned testing in a closed testing procedure that strongly controlled Type I error to alpha=0.05. Its p-value was 0.27, which means that no further planned testing was allowed. The p-values reported here are exploratory for decisions about future trials.
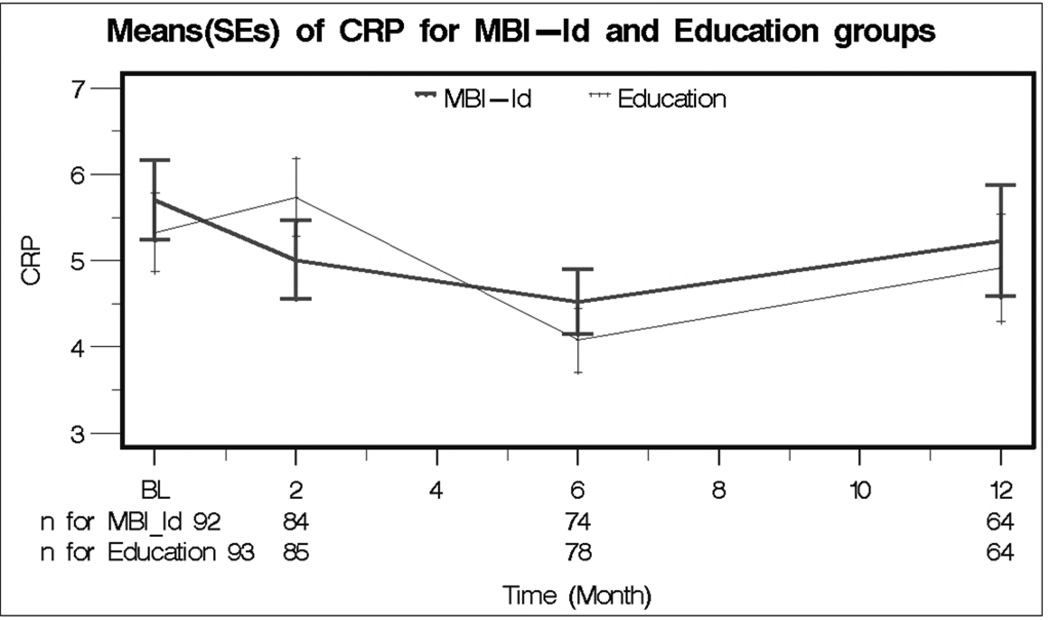
For CRP the difference in effectiveness of the MBI-ld and control interventions was in favor of the MBI-ld group by −0.97 (se=.56), i.e. the MBI-ld intervention decreased CRP almost 1 point more than the control intervention at 2-months. This difference corresponds to an effect size of −0.23 (se=.16) standard deviations. The exploratory p-value reported in Table 5 is 0.08. Figure 3 provides the plot for CRP measures at baseline and 2-months and included in it are the results for 6 and 12 months. In further exploratory analysis, the CRP measurements showed significant improvement at 6 months for both groups combined (baseline to 6-months change = −1.13, p=0.0001).
Figure 3.
Means (SEs) of CRP for Meditation and Education groups
In contrast the difference in effectiveness for IL-6 was small and in the wrong direction (0.15, se=0.16), with an effect size of 0.05 standard deviations (se=0.06) and an exploratory p-value of 0.36. Also, the difference for cortisol was small (−0.01, se=0.02), with an effect size of −0.07 standard deviations (se=0.16), and an exploratory p-value of 0.61. We also explored whether the effect was more pronounced for the decline (slope) in cortisol from rising to the dinner and evening. The intervention’s effect estimate for this decline was even smaller than for the mean cortisol. There was also no differences in the cortisol obtained at rising (p=.9).
To further understand the results, we estimated the correlations between baseline and 2-month measures. Table 6 shows that IL-6 is highly stable over 2-months with a correlation of 0.92. This stability suggests possible difficulty in changing IL-6 with behavioral changes. In contrast the CRP showed a correlation of 0.5, which suggests the potential for changing over time. It is well known that cortisol changes in response to stress. Its stability was the lowest with a correlation of 0.39, and it correlated near zero with the other two markers. The correlation between baseline IL-6 and CRP was 0.25, an association that had been previously reported (Castell et al., 1990).
Table 6.
Correlation between Biomarkers at Baseline and Two Months
| Biomarkers Correlation (p-value) |
CRP 2-month |
IL-6 Baseline |
IL-6 2-month |
Cortisol Baseline |
Cortisol 2-month |
|---|---|---|---|---|---|
| CRP Baseline |
0.50 (0.0001) |
0.25 (0.001) |
0.21 (0.007) |
−0.09 (0.2) |
−0.03 (0.7) |
| CRP 2-month |
0.22 (0.004) |
0.30 (0.0001) |
−0.11 (0.17) |
−0.01 (0.9) |
|
| IL-6 Baseline |
0.92 (0.0001) |
−0.03 (0.7) |
−0.06 (0.4) |
||
| IL-6 2-month |
−0.04 (0.6) |
0.02 (0.8) |
|||
| Cortisol Baseline |
0.39 (0.0001) |
SECONDARY
With measures of depression (CES-D), stress (Perceived Stress Scale), sleep quality (PSQI), no significant differences were found at 2-months. The global test across all five produced a p-value of 0.91. The PSS measure, however, asked the questions in reference to the past week rather than the past month as is the standard format, which permitted an evaluation of the intervention at completion. For the PSQI, the comparison between MBI-ld and education control were in favor of MBI-ld, but the p-value was not significant at 0.25. For CES-D and PSS p-values were 0.60 and 0.17, respectively. The two groups differed in BMI by only −0.3 at 2-months.
Leptin, which can increase CRP levels (Shamsuzzaman et al. 2004, Ble et al., 2005), did not differ between the groups at 2-months (mean concentrations were 38.7 and 38.2 ng/ml (p=0.8) respectively for MBl-ld and education). Also we found no relationship between change from baseline for leptin and change in CRP (r=-0.06, p=.4).
SENSITIVITY AND EXPLORATORY ANALYSIS
BMI
We explored whether the difference in effectiveness of the two interventions depended on BMI (BMI × intervention group interaction). A large BMI interaction effect was observed for CRP (p=0.04). For BMI<30 (n=59) the MBI-ld effect on CRP was a larger decrease of −2.67 (SE=1.0, p=.009) as compared to control, while for BMI>30 (n=127) the effect was just −0.18 (SE=.67, p=0.79). We further broke those with BMI>30 into two groups (between 30 and 35 vs. above 35). For those between 30 and 35, the effect estimate was still in favor of MBld but smaller, with a decrease of −1.1 (se=.96), while for those above 35, the effect estimated suggested MB-ld increased CRP by .67 (SE=0.94). For IL-6 and cortisol the differences between the BMI groups were much smaller and not significant.
Change as a function of Practice
In further analysis, we plotted the relationship between changes in the three biomarkers as a function of degree of participation in the interventions. We found no significant relationship between a decrease in CRP (baseline to 2-months) and the amount of time spent in intervention activities during the 2-month intervention period. The same was true for IL-6 and cortisol. The correlation between activity minutes per day and decline in CRP was −0.14 (after compression of outliers for minutes, and −0.10 without compression). This was in the expected direction, but not significant (p=0.19). We found in the MBI-ld group that 2/3 of the participants averaged between 10–20 minutes per day. The average overall was 15 minutes per day, which is close to our suggested practice time of around 20 minutes per day including weekly attendance. The remaining third were split almost evenly between less than 10 minutes and more than 20 minutes. A few participants recorded much higher minutes than others, .e.g. 60 minutes per day. When we used an objectively recorded measure of attendance at the weekly sessions, we also found no relationship with change, in either group. In further exploration, we also found no significant relationship between CRP change and minutes per day in the subgroup of participants with BMI<30.
Additional Exploration
In addition we checked whether change in perceived stress (PSS) or change in depression symptoms (CES-D) were associated with changes in the three primary outcomes (CRP, IL-6, cortisol). Near zero relationships were found for all six comparisons. Based on our BMI results for CRP, we also explored the relationship between CRP change and PSS change for those with BMI<30, and found a correlation in the expected direction of 0.4 (p=0.08). Also, we checked on our distribution assumptions by plotting residuals from the longitudinal model, and found no significant departure from normality for the three primary outcomes. Finally, plots of changes from baseline to 2-months for these outcomes appeared symmetric and bell-shaped.
For the three primary outcomes, we also checked whether any differences between the two groups in medication use or diagnosis could have affected our results. By including in our longitudinal model the medication use and diagnosis variables listed in Table 4, we found almost no change in the effects of the MBI-ld intervention. For example for CRP, the MBI-ld effect was estimated as −1.0 when we included these additional variables (recall that it was −0.97 in Table 5). We also checked whether depression diagnosis or use of anti-depressants modified the effects of the intervention. Again no significant interaction with either depression or anti-depressant use was found.
We also explored whether higher scores on the CESD depression measure at baseline modified the MBI-ld effect. Again we found no significant interaction for the three primary outcomes. In addition the relationship between change in CESD and change in the three primary outcomes was the same for subjects who were above or below 16 (often used as a cut point for the diagnosis of clinical depression) on the baseline CESD.
Finally, the intervention was administered at six different times (cohorts). We found no significant differences in the intervention effect across cohorts.
Discussion
In this randomized controlled trial the traditional MBSR program was reduced in scope so that it could be performed at lunchtime in the workplace. The participant group was representative of the greater Columbus area. We did not select for individuals who would be more inclined to participate in a meditative practice. Individuals were told that they would receive a lifestyle intervention but mindfulness meditation was not mentioned until after they were randomized. Therefore, we cannot generalize our findings to populations often included in other studies that were recruited for a mindfulness study as they may have had an affinity toward mindfulness.
The education control group met as frequently as the MBI-ld group and they were given homework and encouraged to begin implementing lifestyle changes during this 8 week period. At the weekly sessions many participants indicated that they were making changes and one individual began training for a marathon. Our active control group was structurally equivalent to our mindfulness intervention. It controlled for non-specific factors, and met all recommended criteria for control groups appropriate for studies on mindfulness-based interventions, including equivalent education (PhD) for the MBI-ld and the control group instructors (MacCoon et al., 2012).
MBI-ld significantly enhanced mindfulness by 2-months and it was maintained for up to a year when compared to the education control. One of the major questions about mindfulness programs is whether there effects could be sustained beyond the two month period of regular meetings. We used the Toronto Mindfulness Scale (TMS) as a self-report measure for mindfulness. Although the TMS doesn’t capture all the dimensions of mindfulness (its focus is on awareness and curiosity), it supports the contention that the mindfulness intervention was effective and sustainable.
The trial was designed to test whether MBI-ld was superior to an education control in lowering cortisol, IL-6 and CRP immediately at the end of the interventions. We did not confirm this hypothesis. MBSR in smaller observational studies has been reported by some but not all investigators to lower cortisol levels when the intervention is compared to a wait list control group (Carlson et al., 2007, Witek-Janusek et al., 2008, Matousek et al., 2010). Using an extensive pre and post MBI-ld salivary cortisol sampling protocol we saw no decrease in cortisol levels. Likewise we did not see any MBI-ld changes in IL-6 levels. The correlation between pre and two month post IL-6 levels combining both groups was 0.92 which suggests that IL-6 is a highly stable inflammatory marker.
Although not statistically significant (p=.08), at 2-months post MBI-ld intervention the CRP level was one mg/ml lower in the MBI-ld group than in the education control group. Both interventions produced similar decreases in CRP at 6 months. This decrease in CRP was not associated with a decrease in IL-6. Although IL-6 is an important regulator of liver production of CRP its production by the liver is dependent on more than IL-6. Other physiologic influences on CRP include IL-1, IL-17, and TGF-beta (Taylor et al., 1990, Eklund 2009).
Additionally, these decreases in CRP occurred in both groups without any significant weight loss. In regard to the active education control intervention, a low carbohydrate diet can decrease CRP in individuals with elevated CRP (> 3 mg/ml) without any associated weight loss (Seshadri et al., 2004).
The close relationship between CRP and adiposity has been well established (Visser et al., 1999), and we found that BMI predicted the magnitude of MBI-ld lowering of the CRP level. In participants with a BMI<30 (overweight but not obese) MBI-ld produced a decrease in CRP levels of −2.67 mg/ml whereas in those with a BMI>30 the decrease at 2-months was only −0.18 mg/ml. This finding suggests that the inflammation associated with obesity (Schenk et al., 2008) is more resistant to the anti-inflammatory processes initiated by mindfulness.
While MBI-ld lowered CRP at 2-months post intervention, by 6 months a similar decline in CRP levels were noted in the education group, which may reflect the time needed for nutrition and exercise changes to be initiated.
A decrease of CRP of 1 mg/ml as seen in this study could be of clinical significance in certain individuals as values of CRP above 3 mg/ml are associated with a twofold increase in risk of a myocardial infarction in the following three years (Ridker et al., 2000). In addition, in a trial of elderly people with hyperlipidemia in whom a statin decreased the CRP below 5 mg/l, there was almost a 50% reduction of major cardiovascular events (Glynn et al., 2010).
Some studies have suggested that the efficacy of mindfulness intervention does not correlate with the length of time spent on the didactic practice and that shorter or less frequent training sessions are effective (Carmody and Baer, 2009). We had subjects keep records of their formal and informal meditative practice for up to a year. We were not able to confirm that the amount of time spent in formal and/or informal practice correlated with the decrease in their CRP levels. The lack of a significant relationship between CRP change and minutes per day could be due to subjectivity in perceptions about what counts as mindful activity. This dissociation between self-reported practice time and biological outcomes with mindfulness practices has also been previously reported (Pace et al., 2010).
One mechanism for lowering CRP levels in this study might be a decrease in leptin levels. Leptin has numerous biologic effects in addition to suppressing appetite (Margetic et al., 2002). Leptin has been associated with CRP levels in normal individuals (Shamsuzzaman et al. 2004, Ble et al., 2005) and it stimulates C-reactive protein concentrations in vascular endothelial cells (Pasceri et al., 2000). In this study however, leptin levels did not change in either group over the 12 months of study.
A potential mechanism for the lowering of CRP by MBI-ld, but not evaluated in this study, is an increase in vagal parasympathetic tone (Tang et al., 2009, Ditto et al., 2006) which has been shown to have anti-inflammatory influences (Pavlov et al., 2003).
We did not see any significant changes in self-report measures for depressive symptoms, perceived stress, or sleep quality. Most but not all MBSR investigations have found improvements in these areas when the intervention is compared to a wait list control group (Carlson et al., 2007, Witek-Janusek et al., 2008, Winbush et al., 2007, Roth and Robbins, 2004, Britton et al., 2010).
MBI-ld was intense enough that a self-report mindfulness measure was significantly improved and this improvement was maintained for a year. It is possible, however, that the more intense traditional MBI program might have improved depression, sleep and perceived stress when compared to the active lifestyle education group. Conversely, MBI-ld may have achieved significant decreases in these variables had a control wait list group been employed.
Additionally, the burden of obesity (2/3 of participants above BMI of 30) and its associated complications in the participants may have produced resistance to experiencing an improvement in perceived stress, sleep, depressive symptoms and the primary biologic variables. In fact if we had focused only on participants with BMI<30, we would have likely concluded that MB-ld is effective in reducing CRP. A limitation of our study was omission of a wait list control group as the impact of the MBI-ld may have achieved significance in comparison, indicating the potential impact of such a workplace intervention.
Our education intervention did control for time and attention and provided the opportunity for subjects to change behavior immediately during the 8-week intervention period. So our study answered the question of whether intense education about stress and suggested lifestyle changes was inferior to this meditation practice intervention.
In summary, we have performed a randomized trial with a compressed MBSR intervention in which instruction and practice occurred in the workplace. This reduced the barriers commonly mentioned for non-participation in MBSR programs. Adherence to the program was greater than 90% for 8 weeks (evidenced by weekly attendance/practice sheets) even though the subjects were unaware that mindfulness meditation was one of the lifestyle interventions being offered. Additionally, mindfulness was achieved and sustained for at least one year.
We observed that CRP decreased in the MBI-ld group at the end of the intervention although not significantly, with a large decrease occurring in those with a BMI<30. It is possible that a more intense intervention would have produced more significant effects. We conclude that MBI-ld should be more fully investigated as a low-cost self-directed complementary strategy for reducing inflammation.
Research highlight.
A randomized mindfulness-based intervention performed in the workplace decreased CRP levels in overweight/obese participants.
Acknowledgements
The project described was supported by Award Number R21AT003670 from the National Center For Complementary & Alternative Medicine and by the National Center for Research Resources, Grant UL1RR025755 which is now at the National Center for Advancing Translational Sciences, Grant UL1TR000090.
The authors would like to thank the nursing staff at The Ohio State University Clinical Research Center, and Kemba Days Yancey for study coordination.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement:
All authors declare that there are no conflicts of interest.
Contributor Information
William B. Malarkey, The Ohio State University.
David Jarjoura, The Ohio State University.
Maryanna Klatt, The Ohio State University.
References
- Aldana S. The Culprit and the Cure: Why Lifestyle Is the Culprit Behind America's Poor Health. Mapleton, Utah: Maple Mountain Press; 2005. [Google Scholar]
- Ble A, Windham BG, Bandinelli S, Taub DD, Volpato S, Bartali B, Tracy RP, Guralnik JM, Ferrucci L. Relation of plasma leptin to C-reactive protein in older adults (from the Invecchiare nel Chianti study) Am. J. Cardiol. 2005;96:991–995. doi: 10.1016/j.amjcard.2005.05.058. [DOI] [PubMed] [Google Scholar]
- Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosom. Med. 2010;72:539–548. doi: 10.1097/PSY.0b013e3181dc1bad. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behav. Immun. 2007;21:1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J. Clin. Psychol. 2009;65:627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- Castell JV, Gómez-Lechón MJ, David M, Fabra R, Trullenque R, Heinrich PC. Acute-phase response of human hepatocytes: Regulation of acute-phase protein synthesis by interleukin-6. Hepatology. 1990;12:1179–1186. doi: 10.1002/hep.1840120517. [DOI] [PubMed] [Google Scholar]
- Cerqueira JJ, Almeida OF, Sousa N. The stressed prefrontal cortex. Left? Right! Brain. Behav. Immun. 2008;22:630–638. doi: 10.1016/j.bbi.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Newbury Park: Sage Publications; 1988. pp. 31–67. [Google Scholar]
- Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosom. Med. 2007;69:560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, Sheridan JF. Alterations in brain and immune function produced by mindfulness meditation. Psychosom. Med. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Ditto B, Eclache M, Goldman N. Short-term autonomic and cardiovascular effects of mindfulness body scan meditation. Ann. Behav. Med. 2006;32:227–234. doi: 10.1207/s15324796abm3203_9. [DOI] [PubMed] [Google Scholar]
- Eklund CM. Proinflammatory cytokines in CRP baseline regulation. Adv. Clin. Chem. 2009;48:111–136. doi: 10.1016/s0065-2423(09)48005-3. [DOI] [PubMed] [Google Scholar]
- Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann. Intern. Med. 2010;152:488–496. doi: 10.1059/0003-4819-152-8-201004200-00005. W174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann M, Kopf S, Kircher C, Faude-Lang V, Djuric Z, Augstein F, Friederich HC, Kieser M, Bierhaus A, Humpert PM, Herzog W, Nawroth PP. Sustained Effects of a Mindfulness-Based Stress-Reduction Intervention in Type 2 Diabetic Patients: Design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-Study) Diabetes Care. 2012;35:945–947. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropley TG, Hosmer D, Bernhard JD. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosom. Med. 1998;60:625–632. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- Klatt MD, Buckworth J, Malarkey WB. Effects of low-dose mindfulness-based stress reduction (MBSR-ld) on working adults. Health Educ. Behav. 2009;36:601–614. doi: 10.1177/1090198108317627. [DOI] [PubMed] [Google Scholar]
- Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. J. Clin. Endocrinol. Metab. 2011;96:1478–1485. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, Carlson L, Shapiro S, Carmody J, Abbey S, Devins G. The Toronto Mindfulness Scale: development and validation. J. Clin. Psychol. 2006;62:1445–1467. doi: 10.1002/jclp.20326. [DOI] [PubMed] [Google Scholar]
- Lehmacher W, Wassmer G, Reitmeir P. Procedures for two-sample comparisons with multiple endpoints controlling the experiment-wise error rate. Biometrics. 1991;47:511–512. [PubMed] [Google Scholar]
- Little R. Modeling the dropout mechanism in repeated measures studies. J. Am. Stat. Assoc. 1995;90:1112–1121. [Google Scholar]
- Lin X, Ryan L, Sammel M, Zhang D, Padungtod C, Xu X. A scaled linear mixed model for multiple outcomes. Biometrics. 2000;56:593–601. doi: 10.1111/j.0006-341x.2000.00593.x. [DOI] [PubMed] [Google Scholar]
- Liu GF, Lu K, Mogg R, Mallick M, Mehrotra DV. Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Stat. Med. 2009;28:2509–2530. doi: 10.1002/sim.3639. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300:1350–1352. doi: 10.1001/jama.300.11.1350. [DOI] [PubMed] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, Bonus KA, Stoney CM, Salomons TV, Davidson RJ, Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav. Res. Ther. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margetic S, Gazzola C, Pegg GG, Hill RA. Leptin: a review of its peripheral actions and interactions. Int. J. Obes. Relat. Metab. Disord. 2002;26:1407–1433. doi: 10.1038/sj.ijo.0802142. [DOI] [PubMed] [Google Scholar]
- Matousek RH, Dobkin PL, Pruessner J. Cortisol as a marker for improvement in mindfulness-based stress reduction. Complement. Ther. Clin. Pract. 2010;16:13–19. doi: 10.1016/j.ctcp.2009.06.004. [DOI] [PubMed] [Google Scholar]
- McDade TW, Hawkley LC, Cacioppo JT. Psychosocial and behavioral predictors of inflammation in middle-aged and older adults: the Chicago health, aging, and social relations study. Psychosom. Med. 2006;68:376–381. doi: 10.1097/01.psy.0000221371.43607.64. [DOI] [PubMed] [Google Scholar]
- Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134:310–319. doi: 10.1016/j.pain.2007.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivo EL, Dodson-Lavelle B, Wren A, Fang Y, Oz MC. Feasibility and effectiveness of a brief meditation-based stress management intervention for patients diagnosed with or at risk for coronary heart disease: a pilot study. Psychol. Health. Med. 2009;14:513–523. doi: 10.1080/13548500902890087. [DOI] [PubMed] [Google Scholar]
- Ott MJ, Norris RL, Bauer-Wu SM. Mindfulness meditation for oncology patients: a discussion and critical review. Integr. Cancer. Ther. 2006;5:98–108. doi: 10.1177/1534735406288083. [DOI] [PubMed] [Google Scholar]
- Pace TW, Negi LT, Sivilli TI, Issa MJ, Cole SP, Adame DD, Raison CL. Innate immune, neuroendocrine and behavioral responses to psychosocial stress do not predict subsequent compassion meditation practice time. Psychoneuroendocrinology. 2010;35:310–315. doi: 10.1016/j.psyneuen.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paffen E, DeMaat MP. C-reactive protein in atherosclerosis: A causal factor? Cardiovasc. Res. 2006;71:30–39. doi: 10.1016/j.cardiores.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect on C-reactive protein on human endothelial cells. Circulation. 2000;102:2165–2168. doi: 10.1161/01.cir.102.18.2165. [DOI] [PubMed] [Google Scholar]
- Pavlov VA, Wang H, Czura CJ, Friedman SG, Tracey KJ. The cholinergic anti-inflammatory pathway: a missing link in neuroimmunomodulation. Mol. Med. 2003;9:125–134. [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Reitmeir P, Wassmer G. One-sided multiple endpoint testing in two-sample comparisons. Communication in Statistics-Simula. 1996;25:99–117. [Google Scholar]
- Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Eng.l. J. Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- Roth B, Robbins Mindfulness-based stress reduction and health-related quality of life: findings from a bilingual inner-city patient population. Psychosom. Med. 2004;66:113–123. doi: 10.1097/01.psy.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]
- Roy J. Scaled marginal models for multiple continuous outcomes. Biostatistics. 2003;4:371–383. doi: 10.1093/biostatistics/4.3.371. [DOI] [PubMed] [Google Scholar]
- SAS Proc Mixed, Version 9.0. Cary, North Carolina: SAS Institute; 2009. [Google Scholar]
- Schafer J. Analysis of incomplete multivariate data. Chapman Hall, London: 1997. [Google Scholar]
- Schenk S, Saberi M, Olefsky JM. Insulin sensitivity: modulation by nutrients and inflammation. J. Clin. Invest. 2008;118:2992–3002. doi: 10.1172/JCI34260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seshadri P, Iqbal N, Stern L, Williams M, Chicano KL, Daily DA, McGrory J, Gracely EJ, Rader DJ, Samaha FF. A randomized study comparing the effects of a low-carbohydrate diet and a conventional diet on lipoprotein subfractions and C-reactive protein levels in patients with severe obesity. Am. J. Med. 2004;117:398–405. doi: 10.1016/j.amjmed.2004.04.009. [DOI] [PubMed] [Google Scholar]
- Shamsuzzaman AS, Winnicki M, Wolk R, Svatikova A, Phillips BG, Davison DE, Berger PB, Somers VK. Independent association between plasma leptin and C-reactive protein in healthy humans. Circulation. 2004;109:2181–2185. doi: 10.1161/01.CIR.0000127960.28627.75. [DOI] [PubMed] [Google Scholar]
- Suarez ED. C-reactive protein is associated with psychological risk factors of cardiovascular disease in apparently healthy adults. Psychosom. Med. 2004;66:684–691. doi: 10.1097/01.psy.0000138281.73634.67. [DOI] [PubMed] [Google Scholar]
- Tang YY, Ma Y, Fan Y, Feng H, Wang J, Feng S, Lu Q, Hu B, Lin Y, Li J, Zhang Y, Wang Y, Zhou L, Fan M. Central and autonomic nervous system interaction is altered by short-term meditation. Proc. Natl. Acad. Sci. USA. 2009;106:8865–8870. doi: 10.1073/pnas.0904031106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, Yu Q, Sui D, Rothbart MK, Fan M, Posner MI. Short-term meditation training improves attention and self-regulation. Proc. Natl. Acad. Sci. USA. 2007;104:17152–17156. doi: 10.1073/pnas.0707678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AW, Ku NO, Mortensen RF. Regulation of cytokine-induced human C-reactive protein production by transforming growth factor-beta. J. Immunol. 1990;145:2507–2513. [PubMed] [Google Scholar]
- Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282:2131–2135. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- Wassel CL, Barrett-Connor E, Laughlin GA. Association of circulating C-reactive protein and interleukin-6 with longevity into the 80s and 90s: The Rancho Bernardo Study. J. Clin. Endocrinol. Metab. 2010;95:4748–4755. doi: 10.1210/jc.2010-0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: a systematic review. Explore (NY) 2007;3:585–591. doi: 10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo-Arvizu R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav. Immun. 2008;22:969–981. doi: 10.1016/j.bbi.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassario P, Tennen H, Finan P, Kratz A, Parrish B, Irwin MR. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J. Consult. Clin. Psychol. 2008;76:408–421. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]