Abstract
Objectives
The radiological evaluation of the temporomandibular joint (TMJ) consists of demonstrating the morphological features of the disc and the condyle in closed and open mouth positions using MRI. We aimed to determine elasticity of the disc by measuring the amount of elongation during mouth opening.
Methods
The study population included 49 patients. Coronal T1 and multiplane oblique T2 weighted gradient recalled echo sequences were acquired in open and closed mouth positions. Biconcave TMJ disc lengths were measured on sagittal oblique images in both positions. Elongation ratio (ER) was calculated for each patient. According to the findings, TMJs are classified into subgroups: normal (N), dislocated with reduction (DWR), pure DWR (p-DWR), DWR with additional findings (DWR-a) and dislocated without reduction (DWOR). Statistical analysis was performed using the χ2 test and receiver operating characteristic analysis.
Results
Out of 98 discs, 22 of them were evaluated as N, 60 as DWR (28 p-DWR, 32 DWR-a) and 16 as DWOR. There was no significant difference among the disc lengths in three subgroups at the closed mouth position (P = 0.15), whereas there was significant difference in the open mouth position (P = 0.0001). There was significant difference among subgroups as far as ER is concerned (P < 0.05).
Conclusions
ER is a strong indicator of elasticity. Compared with the N group, elasticity of the disc was not significantly different in the p-DWR group but the disc elasticity was very degraded in DWR-a and in DWOR. A negative conversion or one smaller than 1.4 mm means a compromised disc, although sometimes it will possess normal anatomical configurations or signal characteristics.
Keywords: temporomandibular joint, magnetic resonance imaging, elongation
Introduction
The temporomandibular joint (TMJ) is a diarthrodial type of joint, located directly on either side of the head where the mandibular fossa of temporal bone and the mandibular condyle articulate.1
A biconcave fibrocartilaginous articular disc (Figure 1) divides the TMJ into two distinct compartments, superior and inferior. The inferior compartment allows rotation of the condylar head around an instantaneous axis,2 corresponding to the first 20 mm of the mouth opening process. After the mouth is open to this extent, the mouth can no longer open without the superior compartment of the TMJ becoming active. At this point, if the mouth continues to open, not only does the condylar head rotates within the lower compartment of the TMJ, but the entire apparatus (condylar head and articular disc) translates.2 This translation actually amounts to a rotation around another axis. The fibrocartilagenous articular disc in the human TMJ is assumed to behave as a shock absorber and distributor of the joint loads.3,4 However, the exact contribution of this disc to the mechanics of the TMJ is still poorly understood.2,4,5
Figure 1.
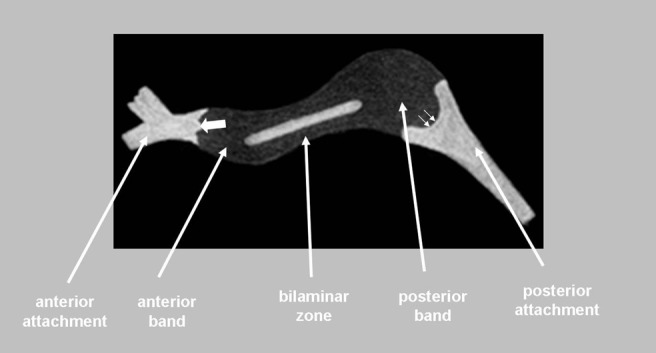
Schematic demonstration of the temporomandibular disc in sagittal projection. The main segments of the disc are shown. Posterior attachment is generally designated as bilaminar zone. Measurements were always performed on the midsagittal images where the disc had its maximum length, anteriorly from the junction of anterior band-anterior attachment (large white arrow), posteriorly from the junction of posterior band-posterior attachment (small arrows)
Internal derangement and associated complications are the most common pathological entities affecting the jaw. As a general term, internal derangement describes a structural abnormality within an articulation. The internal derangement of the TMJ is a specific term defined as an abnormal positional and functional relationship between the disc and the articulating surfaces. In the TMJ, deterioration of the disc elasticity might play a role in the development of the TMJ derangement.6,7 In a few studies the mechanical behaviour of the disc was evaluated with in vitro technique.6,7 Biomechanical tissue behaviour of the human temporomandibular joint disc was tested indirectly with in vitro simulations by experimental studies. The resistance against deformation and the energy dissipation capabilities of discs were measured during dynamic loading conditions.2,6,7 It was found that the biomechanical factors such as stress and strain are considered as initial factors for morphological changes that may cause initiation of internal derangement.8,9
In this study, we attempted to evaluate the disc elasticity in vivo, albeit indirectly, using a new technique that enables calculation of the elongation ratio (ER), which, to the best of our knowledge from the literature review, has not been performed previously.
Materials and methods
A total of 98 TMJs of 49 patients (32 male, 17 female, mean age: 36 ± 6.2 years) were examined by TMJ-MRI with a 1.5 T system (8 channel radiofrequency head coil, Siemens Vision Plus, Erlangen, Germany). After coronal T1 weighted (T1W) (gradient echo-gradient recalled echo (GRE)) and axial-coronal T2 weighted (T2W) GRE acquisitions, sagittal oblique images (Figure 2) were repeated with open and closed mouth positions with T2W GRE sequence. The study was approved by the local ethics committee and oral consent was obtained from each patient prior to the MRI examination. For each subject, the closed mouth position is when the mouth is closed neutrally with no motion. The acquisition time for sagittal oblique GRE images was 2.14 min for each joint. To obtain the open mouth position, a cylindrical shaped object 3.5 cm in diameter and coated with cotton was given to each patient to bite gently. In order to standardize the technique, patients who could not co-operate with the open mouth position (n = 7) and subjects with motion artefacts (n = 4) were not included in the study.
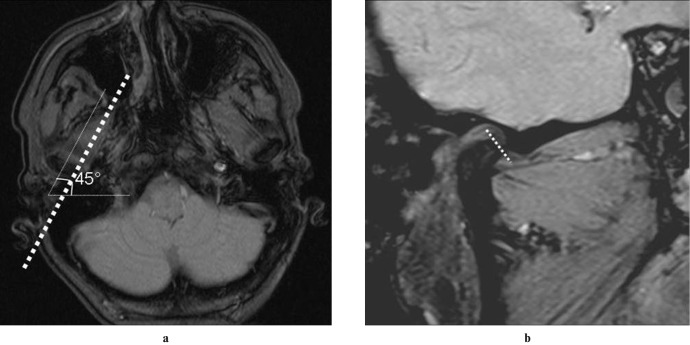
Figure 2.
The sagittal oblique images (performed in this study for the first time) which are acquired in addition to the routine protocol are shown. The angle is determined on the axial scout images (a), the disc length measurement is demonstrated at the sagittal oblique T2 weighted gradient recalled echo image (b)
The gradient pulse sequences and parameters were as follows: for T2W images, field of view (FOV) 160, slice thickness 3 mm, time of repetition (TR) 345 ms, time of echo (TE) 11 ms, flip angle (FA) 30°, matrix 256 × 1256, acquisition mode two-dimentional (2D); for T1W images, FOV 160, slice thickness 3 mm, TR 400 ms, TE 20 ms, FA 90° matrix 256 × 256, acquisition mode 2D. In this study, the scanning plan was not taken vertically to the long axis of the condyle, which is the classic method. The sagittal oblique sequence was instead at a 45° angle with the plane parallel to the lateral pterygoid muscle trace. This scanning plan was preferred because we believe it provides the best anatomy and demonstration of the longest axis of the disc.
According to the clinical findings and data obtained from MRI examinations, TMJs are classified into three main groups: “normal (N)”, “disc dislocation with reduction (DWR)” and “disc dislocation without reduction (DWOR)” as summarized in Table 1. The DWR group is generally accepted as a variation in the literature. In our study this group also has been divided in to two subgroups; pure-DWR (p-DWR), which has no additional symptoms or derangements, and DWR-additional (DWR-a), which has at least one additional sign of derangement (such as osteoarthritis, disc degeneration and effusion) or clinical symptoms.
Table 1. Table showing the disc lengths in millimetres in the open and closed mouth positions, elongation ratio values and the subgroup of each patient.
| Disc length |
Disc length |
||||||||
| CASE | Open mouth | Closed mouth | ER value | Pathology | CASE | Open mouth | Closed mouth | ER value | Pathology |
| 1R | 16.1 | 10.5 | 5.60 | N | 25L | 9.5 | 6.9 | 2.6 | DWR-a |
| 1L | 16.8 | 11.2 | 5.6 | N | 26R | 11.7 | 8.3 | 3.4 | N |
| 2R | 16.2 | 14.2 | 2 | p-DWR | 26L | 6.7 | 6.7 | 0 | DWR-a |
| 2L | 17.2 | 13.1 | 4.1 | p-DWR | 27R | 10.8 | 14.9 | −4.1 | N |
| 3R | 14.4 | 8.7 | 5.7 | p-DWR | 27L | 8.7 | 9.4 | −0.7 | DWOR |
| 3L | 14.5 | 9.7 | 4.8 | p-DWR | 28R | 10.9 | 10.4 | 0.5 | p-DWR |
| 4R | 13.2 | 9 | 4.2 | DWOR | 28L | 11.1 | 9.1 | 2 | N |
| 4L | 13.6 | 9.4 | 4.2 | DWOR | 29R | 12.7 | 11.6 | 1.1 | p-DWR |
| 5R | 7.2 | 8.5 | −1 | DWR-a | 29L | 15.8 | 10.9 | 4.9 | p-DWR |
| 5L | 10.6 | 11.7 | −1.1 | DWR-a | 30R | 11.3 | 8.8 | 2.5 | DWOR |
| 6R | 14.8 | 12.3 | 2.5 | N | 30L | 14.4 | 8.4 | 6 | p-DWR |
| 6L | 13.6 | 13.6 | 0 | DWOR | 31R | 16.3 | 11.3 | 5 | p-DWR |
| 7R | 12.6 | 9.3 | 3.3 | DWOR | 31L | 15.3 | 11.2 | 4.1 | p-DWR |
| 7L | 6.8 | 8.2 | −1.4 | DWR-a | 32R | 16.3 | 11.3 | 5 | p-DWR |
| 8R | 16.3 | 13.8 | 2.5 | p-DWR | 32L | 10.4 | 11.7 | −0.3 | DWOR |
| 8L | 12.2 | 11.8 | 0.4 | DWOR | 33R | 10.4 | 11.7 | −1.3 | N |
| 9R | 12.2 | 10.8 | 1.4 | DWOR | 33L | 7.4 | 8.6 | −1.2 | DWR-a |
| 9L | 12.5 | 9.7 | 2.8 | p-DWR | 34R | 9.2 | 10.4 | −1.2 | DWOR |
| 10R | 12.5 | 12.7 | −0.2 | p-DWR | 34L | 9.8 | 11.8 | −2 | DWOR |
| 10L | 7.8 | 6.7 | 1.1 | DWOR | 35R | 12.9 | 11.4 | 3.5 | DWR-a |
| 11R | 9.3 | 9.2 | 0.1 | DWOR | 35L | 13.8 | 12.6 | 1.2 | DWOR |
| 11L | 10.7 | 8.5 | 2.2 | DWOR | 36R | 7.4 | 9.4 | −2 | DWR-a |
| 12R | 14.7 | 8.7 | 6 | DWOR | 36L | 7.2 | 7.9 | −0.7 | DWR-a |
| 12L | 13.4 | 11.2 | 2.2 | DWOR | 37R | 13.8 | 9.8 | 4 | DWOR |
| 13R | 11.6 | 8.6 | 3 | p-DWR | 37L | 11.5 | 10.1 | 1.4 | DWOR |
| 13L | 9.6 | 8.4 | 1.2 | DWR-a | 38R | 14.8 | 12.8 | 2 | N |
| 14R | 9.7 | 12.3 | −2.6 | DWR-a | 38L | 13.2 | 11.4 | 1.8 | N |
| 14L | 10.7 | 11.2 | −0.5 | DWOR | 39R | 16.1 | 9.7 | 6.4 | p-DWR |
| 15R | 5.8 | 6.2 | −0.4 | DWOR | 39L | 15.9 | 10.8 | 5.1 | p-DWR |
| 15L | 9.8 | 8.4 | 1.4 | N | 40R | 12 | 8.3 | 3.7 | p-DWR |
| 16R | 8.9 | 8.6 | 0.3 | DWOR | 40L | 12.1 | 8.5 | 3.6 | p-DWR |
| 16L | 8.1 | 8.6 | −0.5 | DWOR | 41R | 11.9 | 8.8 | 3.1 | DWOR |
| 17R | 12.1 | 10.5 | 1.6 | DWOR | 41L | 12.2 | 8.9 | 3.3 | DWOR |
| 17L | 10.9 | 7.3 | 3.6 | DWOR | 42R | 14.9 | 12.2 | 2.7 | N |
| 18R | 10.9 | 9.8 | 1.1 | N | 42L | 14.8 | 12.1 | 2.7 | p-DWR |
| 18L | 6.9 | 7.7 | −0.8 | DWR-a | 43R | 15.4 | 12.4 | 3.2 | p-DWR |
| 19R | 14.2 | 10.5 | 3.7 | N | 43L | 15.5 | 12.3 | 3.2 | p-DWR |
| 19L | 14.4 | 10.9 | 3.5 | N | 44R | 7.7 | 7.9 | −0.2 | DWR-a |
| 20R | 15.3 | 12.2 | 3.1 | 11 | 44L | 11.4 | 10.2 | 1.2 | N |
| 20L | 12.6 | 11.4 | 1.2 | p-DWR | 45R | 12.8 | 9.8 | 3 | p-DWR |
| 21R | 13.9 | 10.7 | 3.2 | N | 45L | 14.8 | 14.2 | 2.6 | DWOR |
| 21L | 14.4 | 11.2 | 3.2 | N | 46R | 14.8 | 11.6 | 3.2 | p-DWR |
| 22R | 10.90 | 11.30 | −0.4 | p-DWR | 46L | 8.4 | 9.1 | −0.7 | DWR-a |
| 22L | 10.90 | 11.30 | −0.4 | p-DWR | 47R | 10.8 | 10.7 | 0.1 | DWOR |
| 23R | 14.2 | 11.7 | 2.5 | N | 47L | 13.8 | 12.5 | 1.3 | N |
| 23L | 12.9 | 10.7 | 2.2 | N | 48R | 10.2 | 10.4 | −0.2 | DWR-a |
| 24R | 10.6 | 9.7 | 0.9 | p-DWR | 48L | 8.5 | 10.2 | −1.7 | DWR-a |
| 24L | 12.3 | 10.1 | 2.2 | N | 49R | 11.9 | 8.1 | 3.8 | N |
| 25R | 12.9 | 10.1 | 2.8 | p-DWR | 49L | 12.3 | 9.4 | 2.4 | DWOR |
ER, elongation ratio; N, normal; DWR, disc dislocation with reduction; DWOR, disc dislocation without reduction; p-DWR, pure-DWR; DWR-a, DWR-additional
In all cases, TMJ disc length was measured at its longitudinal axis on the sagittal images which were acquired in both open and closed mouth positions bilaterally. While measuring the disc length, the longest anteroposterior dimension of the longest axis was chosen (Figure 1). For every disc, three measurements were performed in closed and open mouth positions and the mean values were obtained. Measurements were performed after electronic zooming of the image from the standard points. For each TMJ disc, the ER was calculated by subtracting the length of the longitudinal plane of the disc in closed mouth position from the corresponding value in open mouth position images. The major reasons for using the ER in this study were to minimize the effects of the structural length discrepancies of the discs and to quantify the elasticity.
The possible effects of demographic characters and gender on the pathology were evaluated respectively using the independent samples t-test and χ2 test.
Clinical findings have been used as the standard reference for comparison to determine the accuracy of the interpretations of MR images. Statistical analysis was conducted using MedCalc (MedCalc Software, Mariakerke, Belgium). The arithmetic mean and standard deviation (SD) is used for the analysis of the data. For the determination of cut off and compatibility points, ROC curves were drawn.
Intra-individual comparisons were performed regarding the disc lengths in closed and open mouth positions, and ER values obtained using an independent samples t-test. Pathological disc changes (dislocation, deformation) were tested in terms of right and left side differences at the intra-individual level (two-way analysis of variance (ANOVA) test).
The differences between groups were compared using the χ2 test according to the cut-off points. The results of the ROC curve were evaluated within 50% confidence interval and other results within 95%; the significance of P < 0.05 was accepted as meaningful.
Results
There is no significant difference among the mean ages between two gender groups (independent samples t-test) and the frequency of disc pathologies among two genders (χ2 test, P > 0.05).
There is a statistically significant difference in the disc lengths among the all groups in the open mouth position (P = 0.0001), although no significant difference was noted in the closed mouth position (P = 0.15). The mean disc lengths measured at open mouth position were 13.54 mm ± 1.6 mm (N); 12.37 mm ± 2.44 mm (DWR); 9.49 mm ± 2.73 mm (DWOR); at closed mouth position they were 10.41 mm ± 1.56 mm (N); 10 mm ± 1.94 mm (DWR); 9.71 mm ± 1.7 mm (DWOR).
The mean ERs, calculated for each TMJ disc separately, were 2.25 (N), 3.15 (p-DWR), 1.56 (DWR-a), and −0.39 (DWOR) (Table 2). The mean ER values of N and p-DWR were not statistically different, and the ROC curves for these two groups were also not significant (P > 0.05). The values of DWR-a and DWOR groups were significantly different from the N group (P < 0.05, Figure 3).
Table 2. Elongation ratio values of all the joints among all patients.
| N | Mean | SD | |
| N | 22 | 2.25 | 2.06 |
| p-DWR | 28 | 3.15 | 1.91 |
| DWR-a | 32 | 1.56 | 1.88 |
| DWOR | 16 | −0.39 | 1.61 |
| Total | 98 | 1.85 | 2.20 |
N, normal; DWR, disc dislocation with reduction; DWOR, disc dislocation without reduction; p-DWR, pure-DWR; DWR-a, DWR-additional; SD, standard deviation
Figure 3.
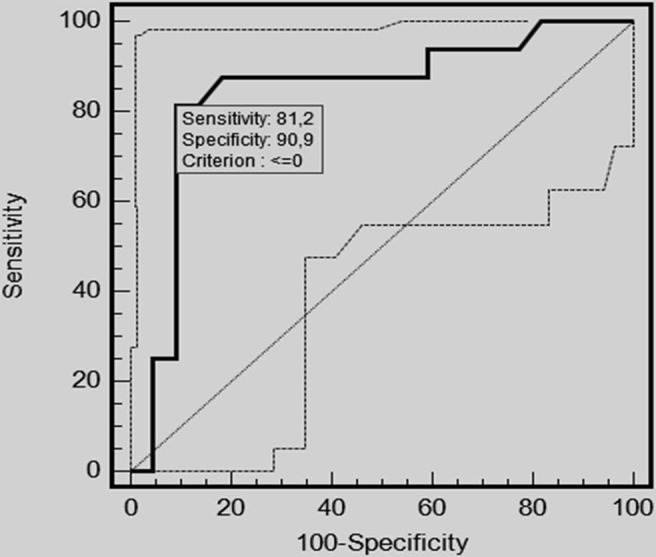
Receiver operating characteristic curve chart showing the relationship between the normal (N) group and disc dislocation without reduction (DWOR) group. Using the elongation ratio <0 value in DWOR patients, abnormal elasticity can be discerned with 81.2% sensitivity and 90.9% specificity
There were 32 joints with DWR-a (including 3 asymptomatic patients with osteoarthritis) and their ERs were significantly decreased (for all DWR-a: 1.56 mm, and for 3 osteoarthritis DWR-a: 0.66 mm) despite no deformation in discs and mild clinical symptoms. Except for the three asymptomatic patients with osteoarthritis, for the other six patients who have osteoarthritis and are symptomatic, the mean ER value was determined as 0.02 mm, which was significantly decreased (P = 0.0001).
There was no statistically significant difference of disc length and ER values in the open and closed mouth positions between the right and left sides within the same pathological group (N, p-DWR, DWR-a, DWR) (P > 0.05). Although there were significant differences between the mean values of different groups, there was no significant difference where the right and left sides are concerned. In general, all the values were higher in the N and p-DWR groups than in the DWR-a and DWR groups. Measuring the elongation value larger than or equal to 1.4 mm (cut-off value) during mouth opening resulted in normal disc elasticity in N and a still elastic disc in p-DWR (with 87.2% sensitivity and 88.2% specifity). Negative conversion or the ER values smaller than 1.4 mm shows a degenerated-compromised and/or a very desiccated disc which is almost consistent with DWOR. The degree of deformation in the disc and severity of the symptoms (pain, limitation of movement, restlessness, sensitivity) had increased as the ER value declined.
Discussion
Pathological conditions of the TMJ often present with pain, joint sounds, tenderness, stiffness, creaking, locking of the joints and functional abnormalities. In degeneration, which was regarded as the most common abnormality, chronic exposure to repetitive stress injuries lead to structural abnormalities such as osteoarthritis.10,11 With the advent of imaging modalities of the TMJ, internal derangement and associated complications have increasingly been regarded to be responsible for the vast majority of TMJ complaints.11 Generally, pathological conditions of the TMJ are not symmetrical, and repetitive microtrauma probably results in asymmetrical joint and disc problems.9 We believe that one of the most important points is detection of disc degeneration, since it is the first component of the joint to be effected. In cases where the degeneration in the disc is detected and treated early, development of possible irreversible changes (such as condylar flattening or osteophytes) may be avoided.9 It is well known that dislocation of the disc is an obvious indicator of joint damage. In addition to this, in the literature a number of indirect findings on MRI, which include thickening of an attachment of the lateral pterygoid muscle, rupture of retrodiscal layers and joint effusion, have been used as early indicatiors of disc and TMJ damage.9
A thorough understanding of joint anatomy and normal function is a prerequisite for understanding the basic mechanism of the joint dynamics. The mandibular head, fossa and articular eminence form the TMJ osseous contours.10,11 A layer of hyaline cartilage covers the articulating cortical bone.10,11 The interposed fibrocartilaginous disc has a bow-tie-shaped biconcave morphology. The anterior and posterior ridges of the disc are termed as anterior and posterior bands. The smaller anterior band attaches to the articular eminence, condylar head and joint capsule (Figure 1). The posterior band blends with highly vascularized, loose connective tissue residing in the retrodiscal space in the mandibular fossa and attaching to the condyle and temporal bone. Medially and laterally, the disc is firmly attached to the capsule and the condylar neck.11
When the jaw is opened, the disc slides into a position between the mandibular head and articular eminence. The loose tissue of the bilaminar zone allows a remarkable range of motion to the disc. The attachments of the disc prevent luxation during opening. Such a complex movement of the jaw is controlled by the forces produced by masticatory muscles.1,2,10 We evaluated the dynamic imaging in oblique sagittal configuration of the disc and aimed to measure the elasticity of the disc, which in turn could be an indirect but easy sign of disturbance in the joint dynamics.
Based on histological and immunohistochemical studies, the TMJ disc is composed mainly of compact type-I collagen fibres, water and proteoglycan, a few cells and elastic fibres.4,12 It was found that collagen microtrauma and loss of the gel layer on the disc surface caused by mechanical tensile and compressive forces plays a crucial role in the progression of the breakdown of the expansion pressure system in the TMJ disc. The latter correlated with deformation of the collagen–proteoglycan network configuration of the disc.4,12-16 This suggests that disc degeneration or failure is involved in the pathological mechanism of TMJ disorders.17-21 In the literature, all the biochemical studies on this topic have been carried out with in vitro techniques.6-9 The results of some of these studies are in concordance with our results. In our study (in vivo), we were able to denote the indirect data indicating impaired elasticity of the degenerated disc in symptomatic cases, non-invasively and in vivo. However, at this point we should indicate that only a limited number of joints with displaced discs produce symptoms, and progression to severe, sometimes debilitating, degenerative arthritis is noted in only a subset of these patients. With this method it may be possible to identify and predict the disc displacements that have a potential to progress and end up with disc damage.22
Physical examination findings in TMJ disorders are highly non-specific.23,24 On the other hand, 82% of patients presenting with pain have displaced discs when examined with MRI.25,26 Although MRI allows excellent depiction of TMJ anatomy and functional abnormalities, especially during imaging of the closed and open jaw positions, its specificity is also limited owing to the high prevalence of disc displacement as a variant. We believe that, in order to find out if displacement with reduction has clinical importance on a patient basis, deterioration of the disc elasticity and a decrease in the ER value can be used as criteria. As a matter of fact, in our study there were significant differences in the ER values among the asymptomatic group (p-DWR) vs symptomatic patients with DWR-a. This was also valid for cases with or without osteoarthritis. In asymptomatic patients with osteoarthritis which was detected only radiologically (ER = 0.66 mm) and in symptomatic osteoarthritic patients (ER = 0.02 mm), the discs' ERs were significantly shorter than in the N group (healthy subjects), which supports our theory (P < 0.05). In our study, absence of a significant difference between the right and left sides that may have a potential effect on the ER values detected by intra-individual statistical studies have increased the reliability of our results.
From the clinical point of view, it is very important to determine whether the disc is affected or not from the ongoing pathological processes in the TMJ. This will help to differentiate the real pathological cases from DWR groups which may represent the variant asymptomatic groups. In addition to these, determination of the severity of the disc rigidity may help to orientate the therapy. In this study, the disc ER value has been measured in a simple way, using parasagittal images without the need for complicated formulas or algorithms. We believe that this sequence can be added to the routine TMJ MRI protocol and hence possible contribution of disc pathology to the TMJ abnormality can be detected. The results of the current study suggest that disc rigidity can be detected as a decreased ER value before overt changes occur in its morphology and signal intensity. Compromised structural integrity of the disc may initiate or may be a sign of the process of osteoarthritis.27,28 With the technique presented in our study, in addition to routine TMJ-MRI results, determination of the disc abnormality will allow the clinician to apply therapeutic strategies that are optimally suited to the underlying abnormality. Just recently, early repair of injuries to the disc, its attachments and the articular capsule that regularly accompany high-grade fractures of the articular process of the mandible has become an issue.29
The most important limitation of our study is that the measurements, although performed 3 times, were done by a single observer (DY, a radiologist with 4 years experience). One possible advantage of a single observer is the lack of interobserver variance. During measurements, the discs were centralized and zoomed on the monitor. As shown in Figure 2, the measurements were performed electronically from standard points, which have minimized the measurement errors. The ER values of some of the patients were higher, with larger and longer disc structures. However, these subjects were also included in the study, assuming that these variations also exist in the normal population.
As a result of this study, we believe that disc ER is a strong indicator of elasticity, and when using the decreased ER value as the only criterion without any other criteria, abnormal discs can be detected. When compared with N group, elasticity of the disc is found to be increased (but not statistically different) in p-DWR group, whereas it is very decreased (even negatively opposed) in the DWR-a and/or DWOR group. Measuring an elongation value ≥ 1.4 mm (cut-off value) during mouth opening shows normal disc elasticity in N and a still elastic disc in p-DWR group (with 87.2% sensitivity and 88.2% specifity). Negative conversion or the ER values smaller than 1.4 mm points out a degenerated-compromised and/or very desiccated disc almost consistent with DWOR. The degree of deformation in the disc and severity of the symptoms (pain, limitation of movement, restlessness, sensitivity) increased as the ER value declined.
In conclusion, the average ER value of the N group, with no joint-related complaints and normal physical examination findings, and the p-DWR group did not differ significantly, where as in the DWR-a and DWOR groups, the ER value was significantly reduced with concordance of increased frequency of symptoms and osteoarthritic changes. With these findings, ER as an indicator of disc elasticity has the capability to provide additional information to previous grading systems; however, its use as a diagnostic criterion has to be validated with further research including larger group of patients.
References
- 1.Rayne J, Phil D. Functional anatomy of the temporomandibular joint. Br J Oral Maxillofac Surg 1987;25:92–99 [DOI] [PubMed] [Google Scholar]
- 2.Nickel J, Spilker R, Iwasaki L, Gonzalez Y, McCall WD, Ohrbach R, et al. Static and dynamic mechanics of the temporomandibular joint: plowing forces, joint load and tissue stress. Orthod Craniofac Res 2009;12:159–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scapino RP, Canham PB, Finlay HM, Mills DK. The behaviour of collagen fibres in stress relaxation and stress distribution in the jaw-joint disc of rabbits. Arch Oral Biol 1996;41:1039–1052 [DOI] [PubMed] [Google Scholar]
- 4.Kuboki T, Shinoda M, Orsini MG, Yamashita A. Viscoelastic properties of the pig temporomandibular joint articular soft tissues of the condyle and disc. J Dent Res 1997;76:1760–1769 [DOI] [PubMed] [Google Scholar]
- 5.Sadowsky C, Polson AM. Temporomandibular disorders and functional occlusion after orthodontic treatment: results of two long term studies. Am J Orthod 1984;86:386–390 [DOI] [PubMed] [Google Scholar]
- 6.Lumpkins SB, McFetridge PS. Regional variations in the viscoelastic compressive properties of the temporomandibular joint disc and implications toward tissue engineering. J Biomed Mater Res A 2009;90:784–791 [DOI] [PubMed] [Google Scholar]
- 7.Lai WF, Bowley J, Burch JG. Evaluation of shear stress of the human temporomandibular joint disc. J Orofac Pain 1998;12:153–159 [PubMed] [Google Scholar]
- 8.Mao JJ, Rahemtulla F, Scott PG. Proteoglycan expression in the rat temporomandibular joint in response to unilateral bite raise. J Dent Res 1998;77:1520–1528 [DOI] [PubMed] [Google Scholar]
- 9.Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, et al. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics 2006;26:765–781 [DOI] [PubMed] [Google Scholar]
- 10.Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology 1990;177:67–71 [DOI] [PubMed] [Google Scholar]
- 11.Kaplan PA, Tu HK, Williams SM, Lydlatt DD. The normal temporomandibular joint: MR and arthrographic correlation. Radiology 1987;165:177–178 [DOI] [PubMed] [Google Scholar]
- 12.Kang H, Bao G, Dong Y, Yi X, Chen MS. Tensile mechanics of mandibular condylar cartilage. J Chin Dent Res 2002;5:58–61 [PubMed] [Google Scholar]
- 14.Detamore MS, Athanathiou KA. Structure and function of the temporomandibular joint disc: implications for tissue engineering. J Oral Maxillofac Surg 2003;61:494–506 [DOI] [PubMed] [Google Scholar]
- 14.Detamore MS, Athanathiou KA. Tensile properties of the porcine temporomandibular joint disc. J Biomech Eng 2003;125:558–565 [DOI] [PubMed] [Google Scholar]
- 15.Gu Z, Zhang Z, Sun K. Transmission electron microscopic and light microscopic study of condylar and joint disk in TMJ disturbance syndrome. Chung Kuo Kou Qiang Ke Xue Za Zhi 1991;26:18–20 61 [PubMed] [Google Scholar]
- 16.Hasson TL. Current concepts about the temporomandibular joint. J Prosthet Dent 1986;55:370–374 [DOI] [PubMed] [Google Scholar]
- 17.Mow VC, Kuei SC, Lai WM, Armstrong CG. Biphasic creep and stress relaxation of articular cartilage in compression: theory and experiments. J Biomech Eng 1980;102:73–84 [DOI] [PubMed] [Google Scholar]
- 18.Nickel JC, Mclachlan KR. In vitro measurement of the stress-distribution properties of the pig temporomandibular joint disc. Arch Oral Biol 1994;39:439–446 [DOI] [PubMed] [Google Scholar]
- 19.Shengyi T, Yinghua X, Mongshi C, Yongnian L. Biomechanical properties and collagen orientation of the TMJ discs in dogs. Part II. Tensile mechanical properties of the disc. J Craniomandib Disord 1991;5:107–112 [PubMed] [Google Scholar]
- 20.Tanaka E, Del Pozo R, Sugiyama M, Tanne K. Biomechanical response of retrodiscal tissue in the temporomandibular joint under compression. J Oral Maxillofac Surg 2002;60:546–551 [DOI] [PubMed] [Google Scholar]
- 21.Tanne K, Tanaka E, Sakuda M. Stress distributions in the TMJ during clenching in patients with vertical discrepancies of the craniofacial complex. J Orofac Pain 1995;9:153–160 [PubMed] [Google Scholar]
- 22.Larheim TA, Westesson PL, Sano T. Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology 2001;218:428–443 [DOI] [PubMed] [Google Scholar]
- 23.Nebbe B, Major PW. Prevalence of TMJ disc displacement in a pre-orthodontic adolescent sample. Angle Orthod 2000;70:454–463 [DOI] [PubMed] [Google Scholar]
- 24.Kircos LT, Ortendahl DA, Mark AS, Arakawa M. Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers. J Oral Maxillofac Surg 1987;45:852–854 [DOI] [PubMed] [Google Scholar]
- 25.Helms CA, Kaplan P. Diagnostic imaging of the temporomandibular joint: recommendations for use of the various techniques. AJR Am J Roentgenol 1990;154:319–322 [DOI] [PubMed] [Google Scholar]
- 26.Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop 1996;109:249–262 [DOI] [PubMed] [Google Scholar]
- 27.Vogl TJ, Abolmaali N. MRI of the temporomandibular joint: technique, results, indications. Rofo Fortschr Geb Roentgenstr Neuen Bildgeb Verfahr 2001;173:969–979 [DOI] [PubMed] [Google Scholar]
- 28.Bradrick JP, Eckhauser ML, Indresano AT. Early response of canine temporomandibular joint tissues to arthroscopically guided neodymium: YAG laser wounds. J Oral Maxillofac Surg 1992;50:835–842 [DOI] [PubMed] [Google Scholar]
- 29.Gu Z, Shibata T, Cao Z, Feng J, Hu J. Chondrocyte apoptosis in temporomandibular joints with disc displacement. J Oral Maxillofac Surg 2002;60:1026–1031 [DOI] [PubMed] [Google Scholar]