Abstract
Stafne bone cavity (SBC) was mostly described as a small oval radiolucency in the posterior mandibular region. To the best of our knowledge, the literature does not contain any report of the use of cone beam CT (CBCT) sialography for the diagnosis of this entity. The aim of this paper is to present a large, irregular and expanded atypical SBC, which made diagnosis difficult. A CBCT sialography was performed to get a definite diagnosis of this rare entity.
Keywords: Stafne bone cavity, cone beam computed tomography, sialography
Case report
A 40-year-old male patient was referred to the Department of Prosthetic Dentistry for a dental implant. The panoramic radiography exhibited a well-defined radiolucent area with a corticated smooth but irregular margin at the level of the second to third molar on the left mandible (Figure 1). The radiolucency was rhomboidal in shape and approximately 3 × 1.8 cm in size, and overlapped the inferior alveolar canal. The second left mandibular molar was missing. The third left mandibular molar tooth was asymptomatic and the periodontal ligament space and lamina dura were intact. The patient had no history of trauma of the jaw. A clinical examination revealed no facial asymmetry and no lymphadenopathy. The most likely diagnosis was a non-odontogenic cyst.
Figure 1.
Panoramic radiograph showing well-defined corticated rhomboidal radiolucency in the left mandible. The adjacent third molar was intact and the inferior alveolar canal was overlapped by the lesion
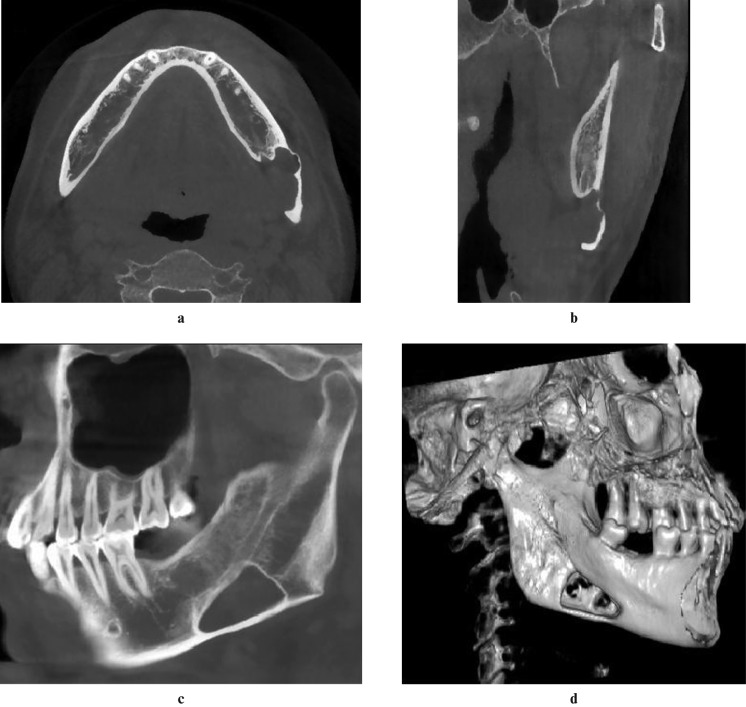
Aware of the unusual features, a next generation Newtom 3G cone beam CT (CBCT) unit (Newtom VG, Quantitative Radiology Srl, Verona, Italy) with a 15 × 15 cm flat panel detector was used to get more information on the cavity for a definitive diagnosis. A 0.3 mm voxel CBCT scan of the submandibular region was performed. The CBCT scans showed a well-defined lingual defect in the posterior aspect of the left mandible. The buccal cortex was expanded and possibly perforated. The cavity was partially filled by soft tissue that seemed to be continuous with the submandibular gland (Figure 2). Stafne bone cavity (SBC) was strongly suspected.
Figure 2.
Axial (a), coronal (b) and sagittal (c) sections of cone beam CT (CBCT) showing a large bone cavity with an irregular border. The inner tissue seemed to be continuous with the submandibular gland. The buccal cortex was expanded and perforated in three-dimensional volume rendering processing (d)
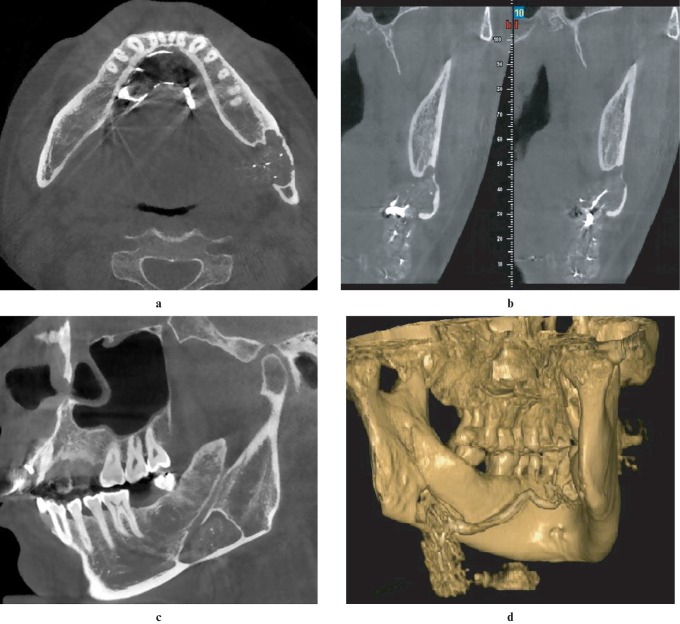
Because of the unusual shape and extent, it was necessary to use sialography to confirm the diagnosis. However, it was difficult to get a definitive image interpretation of the relationship between the submandibular gland and the cavity in a conventional sialogram (Figure 3). Another CBCT scan was performed immediately after the conventional sialography. Three-dimensional (3D) image processing was done simultaneouly. With the tomographic or volumetric nature of CBCT, two-dimensional (2D) CBCT sialograms combined with 3D CBCT sialograms offered significant improvement in demonstration of the duct system over a conventional sialogram. The cavity was mostly occupied by the contrast-filled submandibular gland tissue. Irregular bordered areas of a lower density, similar to fat tissue, were also clearly demonstrated in the CBCT sialography (Figure 4).
Figure 3.
Conventional sialogram showing that some branch ducts arising superiorly from the hilum of the submandibular gland seemed to distribute in the cavity area
Figure 4.
The cavity area was mostly occupied by contrast-filled submandibular gland tissue, and soft tissue of low attenuation was also clearly demonstrated between the cavity wall and gland (a–c). The three-dimensional processing of the cone beam CT (CBCT) sialography shows the spatial relationship of submandibular gland and the bone cavity (d)
Based on the CBCT sialography findings, a diagnosis of SBC was confirmed. The patient was informed about the lesion and a follow-up course was suggested.
Discussion
SBC is an uncommon lesion, originally described as a distinct entity by Stafne in 1942.1 The quoted incidence is 0.1–6.06% in different reports.2,3 SBC mostly involves patients aged 40–60 years, with a male predominance. It usually presents as a well-circumscribed corticated, oval or elliptical radiolucency, which is located below the inferior dental canal and above the lower border of the mandible in the angle or molar region. Interestingly, this lesion has also been reported in the lingual cortex of the anterior mandible, and the rarest variants have even been located on the lingual/buccal aspect of the mandibular ramus.3-8
Until now, the aetiology of SBC has been unclear. Stafne hypothesized that the defect was congenital and the lingual cavity was occupied by cartilaginous tissue due to defects in osteogenesis.1 The most widely accepted concept is pressure of the surrounding tissue to the mandible. Generally, the submandibular gland is responsible for the posterior lingual variant of the lesion while the sublingual gland causes the anterior lingual variant.4,5 The parotid gland is described in association with the ascending ramus variant.6 Rare case reports have also been published regarding muscular, lymphatic or vascular tissues related with the cavity.7,8 In a previous case series, no submandibular gland tissue was observed in any of the cases and blood vessels were seen in the SBCs in most of the cases (10/12) on contrast-enhanced CT and MRI. The authors thought that the main cause of SBC was not aberration of the submandibular gland but vascular compression erosion due to an acquired vascular lesion.9 In the present case, the submandibular gland was clearly distributed in the SBC. Our findings supported the idea that the submandibular gland may be the major risk factor in the formation of this entity. Further studies are necessary to better understand the role of the submandibular gland and other tissue of low attenuation in the SBCs.
SBC is generally found incidentally on routine radiographic examinations. CT is a complementary diagnostic procedure for SBC, and other cystic lesions could be distinguished with this method.10 Shimizu et al performed a CT analysis of the inner content of the cavity and found that SBCs contained mainly fatty tissue and other soft tissues on soft-tissue images. The different radiolucencies of the cavity might occur as a result of a different location of the submandibular gland.11 It's known that CT is more specific to bone lesions of the jaws and much less so to soft-tissue. With the advantage of superior soft-tissue characterization and discrimination, MRI was chosen to be a primary diagnostic technique in cases where SBC is suspected.12 Although MRI was suggested for definitive diagnosis of SBC and reported to identify the content of the cavity without radiation exposure, it also has some disadvantages, including cost, discomfort to patients and possible image distortion.12,13
CBCT is being widely used in recent years with high-resolution and low-dose radiation in dentomaxillofacial radiology. Several authors have recently described CBCT procedure as a non-invasive, easy method for diagnosis of SBC.14 It can also be used as an alternative method during the follow-up period. In general, lingual bone depression is the distinctive aspect of SBC and CBCT might be used for the differential diagnosis of suspicious radiolucent lesions of the mandible. Unfortunately, in the present case, the large, irregular lesion with buccal expansion made differential diagnosis difficult. To get a definitive diagnosis, the size and outline of SBC was investigated in relation to the surrounding structures. Sialography is a traditional diagnostic technique to determine the origin from the salivary gland,15 but it is limited by its planar imaging nature. 2D and 3D CBCT sialograms have succeeded in confirming the diagnosis of SBC. To the best of our knowledge, this is the first report of CBCT sialography for diagnosis of SBC. We have highlighted that the sialographic technique can be improved by the combination of sialography with CBCT, especially with 3D formatting.
It is known that SBCs are asymptomatic and non-progressive, thus the surgical treatment of the defect is controversial. The literature featured a case of ossifying fibroma presenting as SBC.16 Some studies showed that SBCs were not developmental lesions and continued to grow gradually and become larger over a long period of observation.17 In addition, superimposed pathology, such as pleomorphic adenoma, can develop in the entrapped salivary gland.18 Although the management of SBC should be conservative, a long-term radiographic follow-up is required.
In conclusion, a combination of CBCT with sialography was found to be a novel and promising approach for investigating SBC. CBCT sialography provided detailed information about the content of the cavity and allowed a definitive diagnosis for atypical SBC.
Reference
- 1.Stafne E. Bone cavities situated near the angle of the mandible. J Am Dent Assoc 1942;29:1969–1972 [Google Scholar]
- 2.Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal mandibular bone depressiones: A review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol 2002;31:281–290 [DOI] [PubMed] [Google Scholar]
- 3.Katz J, Chaushu G, Rotstein I. Stafne's bone cavity in the anterior mandible: a possible diagnostic challenge. J Endod 2001;27:304–307 [DOI] [PubMed] [Google Scholar]
- 4.Tsui SH, Chan FF. Lingual mandibular bone defect: case report and review of the literature. Aust Dent J 1994;39:368–371 [DOI] [PubMed] [Google Scholar]
- 5.de Courten A, Kuffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:460–464 [DOI] [PubMed] [Google Scholar]
- 6.Campos P, Panella J, Crusoé-Rebello I, Azevedo R, Pena N, Cunha T. Mandibular ramus-related Stafne's bone cavity. Dentomaxillofac Radiol 2004;33:63–66 [DOI] [PubMed] [Google Scholar]
- 7.Ariji E, Fujiwara N, Tabata O, Nakayama E, Kanda S, Shiratsuchi Y, et al. Stafne's bone cavity: Classification based on outline and content determined by computer tomography. Oral Surg Oral Med Oral Pathol 1993;76:375–380 [DOI] [PubMed] [Google Scholar]
- 8.Shields ED. Technical note: Stafne static mandibular bone defect—further expression on the buccal aspect of the ramus. Am J Phys Anthropol 2000;111:425–427 [DOI] [PubMed] [Google Scholar]
- 9.Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofac Radiol 2003;32:2–7 [DOI] [PubMed] [Google Scholar]
- 10.Quesada-Gomez C, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Stafne bone cavity: a retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal 2006;11:277–280 [PubMed] [Google Scholar]
- 11.Shimizu M, Osa N, Okamura K, Yoshiura K. CT analysis of the Stafne's bone defects of the mandible. Dentomaxillofac Radiol 2006;35:95–102 [DOI] [PubMed] [Google Scholar]
- 12.Segev Y, Puterman M, Bodner L. Stafne bone cavity—Magnetic resonance imaging. Med Oral Patol Oral Cir Bucal 2006;11:345–373 [PubMed] [Google Scholar]
- 13.Branstetter BF, Weissman JL, Kaplan SB. Imaging of a Stafne bone cavity: what MR adds and why a new name is needed. Am J Neuroradiol 1999;20:587–589 [PMC free article] [PubMed] [Google Scholar]
- 14.Slasky BS, Bar-Ziv J. Lingual mandibular bony defects: CT in the buccolingual plane. J Comput Assist Tomogr 1996;20:439–434 [DOI] [PubMed] [Google Scholar]
- 15.Oikarinen VJ, Wolf J, Julku M. A stereosialographic study of developmental mandibular bone defects (Stafne's idiopathic bone cavities). Int J Oral Surg 1975;4:51–54 [DOI] [PubMed] [Google Scholar]
- 16.Parvizi F, Rout PG. An ossifying fibroma presenting as Stafne's idiopathic bone cavity. Dentomaxillofac Radiol 1997;26:361–363 [DOI] [PubMed] [Google Scholar]
- 17.Hansson LG. Development of a lingual mandibular bone cavity in an 11-year-old boy. Oral Surg Oral Med Oral Pathol 1980;49:376–378 [DOI] [PubMed] [Google Scholar]
- 18.Simpson W. A Stafne's mandibular defect containing a pleomorphic adenoma: Report of a case. J Oral Surg Anesth Hosp Dent Serv 1965;23:553–556 [PubMed] [Google Scholar]