Abstract
Aims
The purpose of the current study was to evaluate feasibility and efficacy of two promising approaches to indicated prevention of disordered gambling in a college population.
Design
Randomized controlled trial with assignment to a Personalized Feedback Intervention (PFI), Cognitive-Behavioral Intervention (CBI), or Assessment-Only Control (AOC). PFI was individually delivered in a single session and included feedback regarding gambling behavior, norms, consequences, and risk-reduction tips, delivered in a motivational interviewing style. CBI was delivered in small groups over 4-6 sessions and included functional analysis, brief cognitive correction, as well as identification of and alternatives for responding to gambling triggers.
Setting
College campus.
Participants
At-risk or probable pathological gamblers (N = 147; 65.3% male; group assignment: PFI, n = 52; CBI, n = 44; AOC, n = 51).
Measurements
Self-reported gambling quantity, frequency, consequences, psychopathology, normative perceptions, and beliefs.
Findings
Relative to control, results at 6-month follow-up indicated reductions in both interventions for gambling consequences (PFI d = .48; CBI d = .39) and DSM-IV criteria (PFI d=.60; CBI d=.48), reductions in frequency for PFI (d = .48). CBI was associated with reduced illusions of control, whereas PFI was associated with reduced perceptions of gambling frequency norms. Reductions in perceived gambling frequency norms mediated effects of PFI on gambling frequency.
Conclusions
A single-session Personalized Feedback Intervention and a multi-session Cognitive-Behavioral Intervention may be helpful in reducing disordered gambling in US college students.
Keywords: gambling, college students, brief interventions, cognitive behavioral, prevention
Introduction
Disordered gambling refers to a pattern of gambling resulting in subclinical or clinical levels of harm, typically corresponding to meeting partial or full DSM-IV diagnostic criteria for pathological gambling [1;2]. Gambling-related harms experienced by college students include increased suicidal behaviors [3;4], legal involvement [5;6], occupational/educational disruptions, financial difficulties, and strained interpersonal relationships [7]. As rates among college students (17%; [8]) are triple that of the U.S. adult population (5.5%; [9;10]), disordered gambling represents a significant public health concern [9;11].
Cognitive-behavioral models presume gambling is maintained through variable interval reinforcement combined with distorted cognitions, such as perceived ability to influence chance outcomes (illusions of control; [12-14]). Greater illusions of control are associated with increased gambling frequency [15], larger wagers [16], and other factors that may prolong gambling engagement [17;18]. Cognitive behavioral therapy (CBT), which targets maladaptive behavioral associations and challenges cognitive distortions, has been efficacious in reducing negative gambling outcomes among adults [19;20] and helping to maintain recovery [21;22]. CBT has also been efficacious in reducing gambling frequency, cognitive distortions, and gambling severity among non-treatment-seeking adults [19;23], suggesting CBT is a viable indicated prevention approach.
Social psychological theories emphasizing normative perceptions and personal attitudes as predictors of behavioral intentions [24;25] have also been used to explain disordered gambling [26-28]. Among college students, the greater one’s perception of the frequency of others’ gambling (descriptive norms), the greater the individual’s gambling and related problems [26-28]. Correcting normative misperceptions of college student drinking has resulted in reduced drinking consistent with the revised norm [29-31]. Consistent with these models, motivational interviewing (MI; [32;33]), an approach that highlights discrepancies between behavior and attitudes/perceptions while enhancing motivation and self-efficacy for behavior change, has also been advanced as a treatment for pathological gambling among adults [34].
Both CBT [35;36] and MI integrated with skills training and personalized feedback are efficacious in reducing college student substance use [37-40]. MI and CBT have also been successfully integrated for indicated prevention of disordered gambling. For example, Hodgins and colleagues [41] compared a telephone MI session with CBT self-help (MI+CBT) to self-help alone and assessment/referral only and found MI+CBT was more efficacious than self-help alone, and was particularly useful for those experiencing less severe gambling problems consistent with indicated prevention.
Research evaluating gambling interventions for college populations is limited [42;43]. Takushi and colleagues [42] randomized 28 college gamblers to a 45-minute integrated MI-CBT session with personalized feedback on personal gambling behavior, college gambling norms, and gambling beliefs (Personalized Feedback Intervention; PFI) or assessment only. Although group differences were not evident at follow-up due to small sample size, PFI showed promise for indicated gambling prevention. More recently, Petry and colleagues [43] found motivational enhancement with personalized feedback (MET) reduced gambling expenditure and severity among college students. However, a more intensive intervention combining MET and CBT reduced severity of gambling psychopathology but not other indices of gambling behavior (i.e., frequency and expenditure). Thus, more research is needed to elucidate the efficacy and mediators of these approaches among college students.
The current study evaluated an enhanced version of Takushi and colleagues’ [42] PFI among college students screened as disordered gamblers, compared to a multi-session group cognitive-behavioral intervention (CBI) adapted from Petry’s individual CBT protocol [44] and incorporating elements of cognitive correction [22;23].1 Both interventions reviewed high-risk gambling situations and provided risk-reduction strategies, but each contained distinct components consistent with their theoretical frameworks, including a unique focus on MI and perceived norms for gambling in the PFI condition, and a greater focus on gambling-related cognitive distortions in the CBI condition. We hypothesized both interventions would lead to greater reductions in gambling frequency, expenditures, and consequences than assessment-only control (AOC) at 6-month follow-up, but would be efficacious for different reasons. Specifically, PFI efficacy was expected to be mediated by changes in perceived gambling norms, whereas CBI efficacy was expected to be mediated by changes in gambling-related cognitions.
Methods
Screening participants and procedures
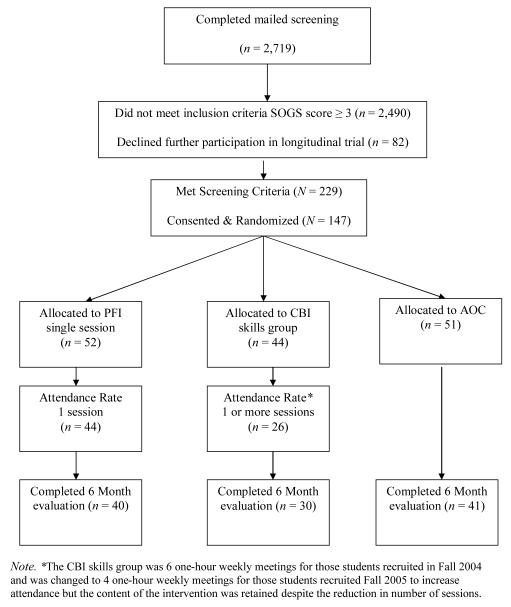
A random sample of 6,457 sophomores/juniors at a large U.S. university was invited to complete a mailed screening survey for $10-$15.2 Of these, 42.1 % completed screening, 9.1% met gambling inclusion criteria, of which 64.2% were successfully recruited (see Figure 1). Participants were 19-25 years old (M = 21.23, SD = 1.37), reporting race as 59.9% Caucasian, 27.9% Asian/Asian American, 6.8% multi-racial, 2.7% Native Hawaiian/Pacific Islander, 0.7% Native American, and 2.0% other or unknown. Across racial categories, 2.7% identified as Hispanic. The study sample included more men (65.3%) than the screening sample (41.9%), χ2(1, N = 2,172) = 30.69, p < .001, but did not otherwise differ demographically. Eligible participants who enrolled did not differ from those not enrolled on any demographic or gambling indicator at screening. At baseline, participants met on average 2.25 DSM-IV pathological gambling criteria in the past 6 months, with 10.2% meeting 5 or more criteria.
Figure 1.
Flow of participants through study protocol
Screening measures
The 20-item South Oaks Gambling Screen (SOGS; [45]) measures gambling involvement and problem severity based on DSM-III-R pathological gambling criteria [46] and was used to identify eligible participants. A score ≥3 (range: 0-20) denotes disordered gambling [47]. The SOGS was modified to assess internet gambling frequency and expand gambling frequency response options from a 3-point to a 5-point scale with anchors of 0 times, 1-10 times, More than 10 times, Less than weekly, Weekly or More than weekly, but less than daily, and Daily, allowing for greater precision for use in the PFI. This modified frequency scale has been shown to highly correlate with other measures of gambling frequency [7]. None of the modified items affected scoring.
The Gambling Quantity and Perceived Norms scale (GQPN; [7]) includes a 6-item expenditure subscale assessing amount of money won/lost through gambling on a 10-point scale from $0 to more than $2,000 over time periods from the past month to past year. Additional items assess gambling frequency (on a 10-point scale from never to every day in the past year), disposable income (on an 11-point scale from less than $50 to more than $500 per month), and perceptions of gambling frequency and expenditure for the typical college student (perceived norms). Gambling expenditure was calculated as the expenditure subscale mean residualized on disposable income. Actual campus-based descriptive norms used in the PFI were generated from screening sample data.
Baseline participants and procedures
One month after screening, eligible participants completed baseline (receiving $20), then were randomized to the individual PFI (n = 52), the group CBI (n = 44), or AOC (n = 51). Participants who completed follow-up 6 months post-baseline received $25. All procedures were reviewed and approved by the local Institutional Review Board.
Baseline and follow-up measures
Gambling frequency, expenditure, and perceived norms were assessed via the GQPN [7].
Gambling problems (or negative consequences) were assessed using the 20-item Gambling Problems Index (GPI, [7]). Participants indicated how often, from never to more than 10 times in the past 6 months, they experienced consequences while, or as a result of, gambling.
DSM-IV [1] criteria for pathological gambling were assessed using the 17-item National Opinion Research Center DSM-IV Screen (NODS; [48;49]). Some criteria have multiple items, but possible scores range from 0-10 DSM-IV criteria endorsed in the past 6 months.
Illusions of control were assessed via a 6-item subscale from the Beliefs About Control Scale (BACS; [15]), on a 5-point scale ranging from strongly disagree to strongly agree. Indicated prevention programs
Therapist training and intervention integrity
Five therapist pairs and seven individual therapists conducted CBI and PFI; no therapists provided both interventions. Most were clinical psychology graduate students and all had a minimum of Bachelor’s-level training. CBI therapists participated in a 2-day workshop led by Dr. Nancy Petry, reviewing CBT for gambling, including role-plays with feedback. Specific training on each module of the CBI manual was provided by the first and sixth authors. PFI therapists were trained by the first and seventh authors in MI and specific PFI components. Sessions were taped, and all therapists received weekly supervision to avoid drift. Over 60% of randomly-selected PFI sessions were coded using the Motivational Interviewing and Treatment Integrity system [50;51]. Therapists received a mean MI Spirit score of 5.3 (SD = 0.96) out of 7, which denotes foundational MI skills [51;52]. Although no equivalent coding system existed for CBI, therapists received ongoing feedback based on review of session tapes, and session content was administered in accordance with checklists.
PFI intervention
Sessions were 60-90 minutes and used MI to facilitate discussion of feedback from participants’ survey responses. Sessions began with open-ended questions about contextual factors associated with participants’ gambling, then review of each feedback section: gambling pattern; perceived gambling norms; positive expectancies and negative consequences of gambling; beliefs about control over gambling; and situational self-efficacy to avoid gambling. Participants were encouraged to consider the feedback in light of their personal goals. All participants received a copy of their feedback, a list of skills for limiting gambling, and a resource/referral list.
CBI
Initial participants (n = 21) were scheduled for 6 weekly one-hour sessions. In an effort to increase attendance, subsequent participants (n = 23) were scheduled to attend 4 sessions containing the same content, with some topics combined into a single session. Sessions covered functional analysis and gambling triggers; challenging cognitive distortions, with emphasis on illusions of control; coping with triggers; assertiveness; and relapse prevention [44]. Participants received a pamphlet covering each week’s topic (which was reviewed with the participant if a session was missed), as well as homework sheets and gambling diaries. Active participation was encouraged through open-ended questions and role-plays. Consistent with the original Petry intervention [44], CBI participants were asked to refrain from gambling for the duration of the group to provide an opportunity to practice and develop skills applicable to gambling and other behavior change situations.
Data Analytic Strategy
Hierarchical multiple regression [53], with two dummy-coded variables representing PFI and CBI with AOC as the reference, was used to compare each intervention to control. Follow-up outcome was regressed on baseline outcome at step 1 to control for baseline behavior. PFI and CBI dummy-coded variables were added at step 2. The F change test at step 2 represents an omnibus test of overall differences in outcome change across all three groups. B weights for the dummy-coded variables are directly interpretable as the mean difference between the PFI and control groups and between the CBI and control groups, respectively [53]. This strategy was selected as different mediators were predicted for PFI (perceived norms) and CBI (illusions of control). While both mediators are cognitive constructs they were clearly independent, being weakly related at baseline, r(147) = .16, p = .053, and uncorrelated at follow-up, r(111) = .10, p = .296. Effect size is provided as Cohen’s d, using the formula d = 2t/√df [54], with small, medium, and large effects equal to 0.2, 0.5, and 0.8, respectively [55].
Mediation analyses
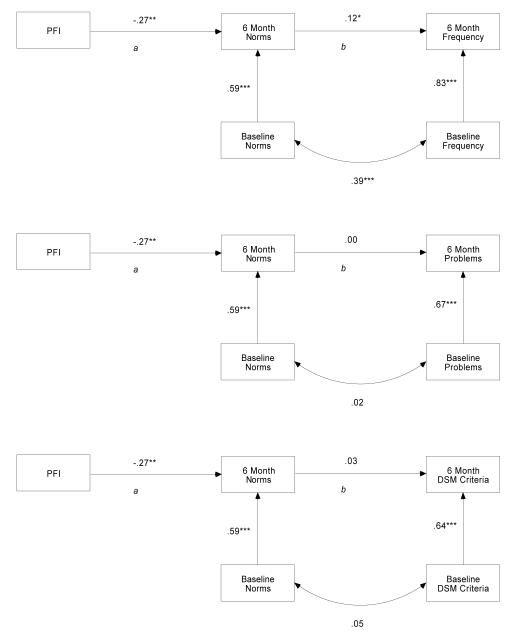
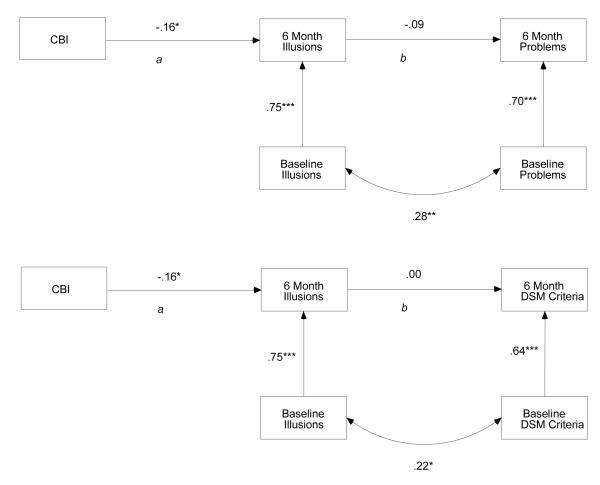
Perceived norms and illusions of control were tested as putative mediators of the PFI effect on frequency, gambling problems and DSM-IV criteria, and the CBI effect on gambling problems and DSM-IV criteria, respectively, in the context of path analysis [56], using the ab products method [57;58]. The Goodman formula [59] was used to estimate standard error for indirect effects. Follow-up mediators and outcomes were examined controlling for baseline values. Figure 2 and 3 represent mediation models with standardized parameter estimates using full information maximum likelihood [60]. Both dummy-coded intervention variables were included in all mediation models, so the paths from intervention to mediator represent the association between that intervention and the mediator relative to the control group. For the sake of parsimony, the non-relevant dummy-coded intervention variable is excluded from the figures.
Figure 2.
Perceived norms as mediator of PFI efficacy
Figure 3.
Illusions of control as mediator of CBI efficacy
Results
Attrition, Missing Data and Intervention Attendance
Follow-up attrition did not vary as a function of experimental condition, demographics, intervention attendance, or gambling indices. Group means on outcomes at baseline and follow-up are presented in Table 1. More participants completed PFI (88.46%) compared to attending ≥1 session of CBI (59.09%), χ2(1, N = 96) = 7.86, p = .005; 41% of CBI participants attended at least half the sessions offered.3 Primary analyses utilized an intent-to-treat approach [61], such that whether participants attended all, part, or none of their assigned intervention they were retained in follow-up assessments and analyses. Individuals were included in primary analyses if they completed the baseline and follow-up assessments (n = 111); those lost-to-follow-up were excluded (n = 36). Subsequent sensitivity analyses used last observation carried forward (LOCF) to assess effects of attrition and examined within-group changes in outcomes as a function of session attendance to assess the effects of intervention non-compliance on outcomes.4
Table 1.
Means and Standard Deviations of Outcome Measures at Baseline and 6 Month Follow-up.
| Baseline |
6 Month Follow-up |
|||||
|---|---|---|---|---|---|---|
| Outcome measures (SD) | PFI | CBI | AOC | PFI | CBI | AOC |
| Gambling Frequency | 3.86 (1.98) | 3.51 (1.83) | 3.71 (2.06) | 3.38 (2.16) | 3.29 (1.63) | 3.93 (2.17) |
| Gambling Expenditure | 0.20 (1.04) | −0.15 (0.57) | −0.08 (0.73) | 0.09 (1.05) | −0.19 (0.65) | 0.05 (0.73) |
| Gambling Problems | 5.71 (7.35) | 3.64 (4.20) | 5.55 (8.31) | 2.58 (5.95) | 2.00 (3.03) | 5.40 (6.92) |
| DSM-IV Criteria | 2.52 (1.75) | 1.93 (1.19) | 2.24 (1.90) | 1.73 (1.04) | 1.53 (1.14) | 2.26 (1.50) |
| Perceived Norms (Frequency) | 3.65 (1.29) | 3.89 (1.31) | 3.50 (1.53) | 2.90 (1.34) | 4.17 (1.29) | 3.50 (1.52) |
| Illusions of Control | 13.67 (3.92) | 13.34 (3.86) | 13.20 (3.96) | 12.60 (3.69) | 11.87 (3.89) | 13.20 (4.03) |
Note. PFI = Personalize Feedback Intervention; CBI = Cognitive Behavioral Intervention; AOC = Assessment-Only Control. Gambling frequency, gambling expenditure, and perceived norms were measured by the GQPN; gambling problems were measured by the GPI; DSM-IV criteria were measured by the NODS; illusions of control were measured by the BACS. No group differences between intervention conditions were evident at baseline for any outcome.
Sex and race.5
Neither sex nor race explained unique variance in follow-up outcomes after controlling for baseline. Results did not change when controlling for sex or race. Thus, aggregated results are reported.
Gambling Outcomes
Frequency
Controlling for baseline frequency, the omnibus difference across the three groups with respect to follow-up frequency approached significance, F(2, 104) = 2.94, p = .057, d = .34. Tests of parameter coefficients revealed PFI was associated with reduced frequency relative to control, d = .48, whereas CBI was not, d = .23. Regression results for baseline measures and intervention effects on all outcomes are summarized in Table 2.
Table 2.
Regression Results Evaluating Gambling Outcomes as a Function of Intervention Group.
| Criterion at Follow-up | Predictor | B | SE B | β | p |
|---|---|---|---|---|---|
| Gambling Frequency | Gambling Frequency (baseline) | 0.88 | 0.05 | 0.85 | <0.001 |
| PFI | −0.57 | 0.24 | −0.14 | 0.017 | |
| CBI | −0.30 | 0.26 | −0.06 | 0.250 | |
|
| |||||
| Gambling Expenditure | Gambling Expenditure (baseline) | 0.88 | 0.05 | 0.86 | <0.001 |
| PFI | −0.09 | 0.10 | −0.05 | 0.362 | |
| CBI | −0.12 | 0.10 | −0.06 | 0.247 | |
|
| |||||
| DSM-IV Criteria | DSM-IV Criteria (baseline) | 1.15 | 0.20 | 0.65 | <0.001 |
| PFI | −0.65 | 0..21 | −0.25 | 0.003 | |
| CBI | −0.56 | 0.23 | −0.20 | 0.016 | |
|
| |||||
| Gambling Problems | Gambling Problems (baseline) | 0.57 | 0.07 | 0.62 | <0.001 |
| PFI | −2.47 | 0.99 | −0.20 | 0.015 | |
| CBI | −2.18 | 1.08 | −0.17 | 0.046 | |
|
| |||||
| Perceived Norms | Perceived Norms (baseline) | 0.63 | 0.08 | 0.60 | <0.001 |
| PFI | −0.85 | 0.25 | −0.28 | 0.001 | |
| CBI | 0.40 | 0.27 | 0.12 | 0.135 | |
|
| |||||
| Illusions of Control | Illusions of Control (baseline) | 0.74 | 0.06 | 0.75 | <0.001 |
| PFI | −0.71 | 0.57 | −0.09 | 0.211 | |
| CBI | −1.36 | 0.61 | −0.16 | 0.029 | |
Note. p < .05.
p < .001
Expenditure
There was no omnibus difference across groups for expenditure, F(2, 107) = .77, p = .466, d = .18, and neither PFI, d = .18, nor CBI, d = .23, were associated with reductions in expenditure relative to control.
Problems
An omnibus effect for gambling problems emerged, F(2, 106) = 3.56, p = .032, d = .37. Tests of parameter coefficients revealed both PFI, d = .48, and CBI, d = .39, were associated with reductions in gambling problems relative to control.
DSM criteria
An overall omnibus group effect likewise emerged for DSM criteria, F(2, 105) = 5.39, p = .006, d = .45. Relative to control, both PFI, d = .60, and CBI, d = .48, endorsed fewer criteria at follow-up.
Perceived norms
Overall group differences were found for perceived norms, F(2, 105) = 12.40, p < .001, d = .69. PFI had greater reductions in perceived norms than AOC, d = .68.
Illusions of control
No overall group difference emerged for illusions of control, F(2, 107) = 2.48, p = .089, d = .30. Relative to AOC, CBI was associated with reduced illusions of control, d = .43.
Norms as mediator of PFI efficacy
An indirect effect of PFI through perceived norms emerged on gambling frequency, Z = 2.01, p = .044 (Figure 2 top). However, the indirect effects of PFI on gambling problems through norms, Z = .02, p = .984, (Figure 2 middle), and DSM criteria were not significant, Z = .37, p = .711, (Figure 2 bottom). Changes in norms did account for reduced gambling frequency as a function of PFI participation. The absence of mediation effects on problems and DSM criteria were largely due to lack of association between these outcomes and perceived gambling frequency norms.
Illusions of control as mediator of CBI efficacy
There were no indirect effects of illusions of control between CBI and problems, Z = 1.17, p = .242 (Figure 3 top), or between CBI and DSM criteria, Z = 0.02, p = .984 (Figure 3 bottom).
Discussion
This RCT of a single-session individual PFI and a 4-6 session group CBI to reduce gambling frequency, expenditures, and consequences in a college sample supported hypothesized intervention effects and provided preliminary evidence for the mediating influence of descriptive norms on the efficacy of the PFI for gambling frequency. However, contrary to hypotheses, changes in illusions of control did not mediate efficacy of CBI on gambling outcomes.
Consistent with hypotheses, PFI was associated with decreased gambling frequency relative to control. Additionally, consistent with research indicating small changes in behavior are associated with larger reductions in harmful effects of the behavior [39], both PFI and CBI were associated with reduced gambling consequences and DSM criteria. The absence of effects on gambling expenditure may reflect a lack of sensitivity in the selected measure. Although the GQPN has been validated, it is not designed to capture changes in event-level betting behavior. Further, in comparison to adult treatment-seeking samples [62;63], many of the gambling consequences reported by this non-treatment-seeking sample were related less to expenditure and more to frequency and time spent gambling. Thus, consequences may be reduced by changing the topography of gambling episodes, rather than expenditure. While prior research by Petry and colleagues [43] did not show effects of brief MI on gambling frequency among college students, it did show effects on gambling expenditure. This may reflect differences in inclusion criteria for the two studies. Petry and colleagues utilized a relatively high minimum expenditure criterion of $100 on at least 4 occasions in the past 2 months; thus, individuals in the current study may have had less opportunity to reduce their gambling expenditure.
With respect to theoretical mechanisms of efficacy, PFI participants reduced perceived norms and CBI participants reduced illusions of control. Moreover, changes in perceived norms mediated the relationship between PFI and gambling frequency. Consistent with past research [30], this suggests individuals modify their behavior to be more consistent with the corrected norm. Changes in perceived norms did not mediate negative consequences or DSM symptoms among PFI participants. This may have been due in part to the focus of the normative feedback, which did not specifically address norms for DSM symptoms or gambling consequences. Illusions of control did not mediate any gambling outcomes for CBI participants. It’s possible other aspects of CBI were responsible for intervention effects, such as enhancing coping skills and generating alternative behaviors. Results should be interpreted with caution as the mediator and outcome were assessed at the same time point, thus do not present a full mediation model.
Certain limitations should be considered. All data were self-report, though research indicates self-reported gambling is accurate compared to collateral reports when psychometrically-sound assessments are utilized [64;65]. With regard to generalizability, the screening survey response rate was 42.1%, and just 65.3% of those eligible participated. However, there were no demographic or gambling differences among eligible participants who did and did not participate. Moreover, individuals recruited through more intensive efforts do not differ from individuals who respond to initial invitations [66;67]. Thus, higher response rates may not be necessary for accurate parameter estimates. Attrition bias was also a concern, as only 75% of participants completed follow-up. Yet, there were no baseline differences between those who did and did not complete follow-up. Results were similar when LOCF was used to supplement complete-case analyses, with the exception that effect of CBI on gambling problems and illusions of control dropped below significance. The addition of participants who experience no change into analyses, which is the operational function of LOCF, necessarily reduces effect sizes. Effect sizes for PFI were large enough to sustain these reductions without losing statistical significance in the LOCF analyses but CBI effects were not.
CBI was efficacious in reducing gambling consequences, but low attendance suggests a multi-session group may be too great a commitment for young adults not necessarily motivated to change. Reduction of CBI to 4 sessions did not increase attendance, suggesting even briefer interventions may be necessary. Although change in intervention length may be considered a limitation, intervention content was held constant. Effects of CBI on gambling frequency were stronger among those who attended more sessions. However, effects for gambling consequences and DSM symptoms were obtained even with low intervention completion rates. No formal system for coding CBI therapist adherence was available, which also poses a limitation, though all therapists received close supervision. CBI participants were asked to refrain from gambling during the intervention period, whereas PFI participants were not. Though this may represent a limitation, it is consistent with the theoretical approaches on which these interventions are based. Finally, the interventions were delivered in different formats: individual and group. Although effects of intervention content cannot be disentangled from intervention implementation style, the current study was not intended to address this question. Rather, this study sought to test each intervention as a distinct product, and test key hypothesized mechanisms of each intervention.
Despite limitations, our study adds to the literature demonstrating efficacy of indicated prevention approaches for college student gambling. Consistent with public-health recommendations for indicated prevention [9], screening and outreach were used to identify individuals experiencing gambling-related problems but not yet expressing concern about their gambling or seeking treatment. Early identification through screening and brief intervention are hoped to prevent development of more severe problems that would necessitate more intensive treatment, which may include elements of PFI and CBI but is typically longer and includes more in-depth focus on skills training. While results support both interventions, PFI may be more feasible for students and was associated with effects on both gambling frequency and problems, with slightly larger effects than CBI. CBI may be more useful for individuals who voluntarily seek services [19;68] or as a program integrated into naturalistic college settings. Research is needed to evaluate efficacy of these interventions in naturalistic contexts, with young adults not in college, and assessing longer-term maintenance of effects.
Supplementary Material
Acknowledgments
Funding for this study was provided by the National Institute on Mental Health (NIMH; R21MH067026, Indicated Prevention with At-Risk Gamblers; PI: Larimer). Writing of this paper was also supported by the Group Health Foundation and a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; T32 AA007455, Psychology Training in Alcohol Research; PI: Larimer).
All funding sources for this study are listed in the acknowledgments.
Footnotes
Given the preventive focus of intervention in this non-treatment-seeking sample, as well as the time and resource demands inherent in implementing a multi-session individual CBI intervention, a group format for CBI was believed to be more feasible and more consistent with the majority of prevention efforts on college campuses (Larimer & Cronce, 2007).
Participant incentives for screening were increased from $10 to $15 during the course of the study in an attempt to increase response rates.
Independent samples t-tests revealed no baseline group differences between data provided by participants randomized to the 4- and 6-session formats of the CBI with respect to gender, race, and the gambling outcomes of interest (frequency, quantity, problems, perceived norms, and illusions of control; all ps > .14). Likewise, independent samples t-tests revealed no differences on the gambling outcomes of interest at follow-up controlling for baseline values (all ps > .10). As the specific content of the intervention was held constant across the two formats, and no group differences were evident at baseline or follow-up, data from participants randomized to the CBI condition were collapsed for all analyses.
Additional analyses examined gambling outcomes using LOCF and thus not excluding participants who were lost to follow-up. We followed the same approach reported for the primary analyses but imputed values for 6-month variables for the 38 participants who did not complete the follow-up assessment. Missing values were replaced with baseline values. Results of these analyses were consistent with the primary results with two exceptions. CBI was no longer associated with reduced gambling problems, t (143) = −1.56, p = .121 and the effect of CBI on illusions dropped below conventional criteria for statistical significance, t(145) = −1.84, p = .068. Conclusions remained unchanged for gambling expenditure, gambling norms, and DSM criteria.
Similarly, within-group differences in outcomes based on intervention attendance were examined controlling for baseline. For PFI, follow-up outcomes did not differ as a function of attendance with the exception of gambling norms. Attendees reported lower follow-up norms compared with non-attendees, t(37) = −2.32, p = .026. For CBI, attending any sessions was associated with reduced gambling frequency, t(25) = −2.94, p = .007. Attending a greater proportion of CBI sessions was likewise associated with reduced gambling frequency, t(25) = −2.65, p = .014.
Relative to women, men reported higher levels of gambling frequency, t(141) = 5.22, p < .001, d = .88, and gambling expenditure, t(145) = 4.71, p < .001, d = .78, at baseline. However, men reported lower perceived norms for gambling, t(145) = −2.40, p = .018, d = .40. Men and women did not differ with respect to gambling problems, t(145) = 1.62, p = .107, d = .27, or illusions of control, t(145) = 1.24, p = .217, d = .21. Given that Caucasian and Asian/Asian American (A/AA) participants were the two largest subgroups (accounting for 87.4% of the baseline sample) and A/AA have been identified as a risk group for disordered gambling relative to other ethnic groups, A/AA participants were compared to all others. At baseline, A/AA gambled less frequently, t(141) = −2.17, p = .032, d = .37, despite reporting more problems, t(145) = 1.96, p = .052, d = .33, higher perceived norms for gambling, t (145) = 2.40, p = .018, d = .40, and more illusions of control, t(145) = 3.60, p < .001, d = .60.
Declaration of Interest: All authors declare that they have no conflicts of interest.
Clinical Trials Registration: This Phase II trial was registered with ClinicalTrials.gov, identifier # NCT00078273.
References
- (1).American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text revision. [Google Scholar]
- (2).Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A meta-analysis. President and Fellows of Harvard College; Boston: 1997. [Google Scholar]
- (3).Frank ML, Lester D, Wexler A. Suicidal behavior among members of Gamblers Anonymous. Journal of Gambling Studies. 1991;7:249–254. doi: 10.1007/BF01019876. [DOI] [PubMed] [Google Scholar]
- (4).Maccallum F, Blaszczynski A. Pathological gambling and suicidality: An analysis of severity and lethality. Suicide & Life-Threatening Behavior. 2003;33:88–99. doi: 10.1521/suli.33.1.88.22781. [DOI] [PubMed] [Google Scholar]
- (5).Bland RC, Newman SC, Orn H, Stebelsky G. Epidemiology of pathological gambling in Edmonton. Canadian Journal of Psychiatry. 1993;38:108–112. doi: 10.1177/070674379303800207. [DOI] [PubMed] [Google Scholar]
- (6).Rosenthal RJ, Lorenz VC. The pathological gambler as criminal offender: Comments on evaluation and treatment. Psychiatric Clinics of North America. 1992;15:647–660. [PubMed] [Google Scholar]
- (7).Neighbors C, Lostutter TW, Larimer ME, Takushi RY. Measuring gambling outcomes among college students. Journal of Gambling Studies. 2002;18:339–360. doi: 10.1023/a:1021013132430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Shaffer HJ, Hall MN. Updating and refining prevalence estimates of disordered gambling behaviour in United States and Canada. Canadian Journal of Public Health. 2001;92:169–172. doi: 10.1007/BF03404298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Korn DA, Shaffer HJ. Gambling and the health of the public: Adopting a public health perspective. Journal of Gambling Studies. 1999;15:289–365. doi: 10.1023/a:1023005115932. [DOI] [PubMed] [Google Scholar]
- (10).Shaffer HJ, Hall MN, Vander Bilt J. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health. 1999;89:1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Cunningham-Williams RM, Cottler LB, Compton WM, III, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders-results from the St. Louis Epidemiologic Catchment Area Study. American Journal of Public Health. 1998;88:1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Baboushkin HR, Hardoon KK, Derevensky JL, Gupta R. Underlying cognitions in gambling behavior among university students. Journal of Applied Social Psychology. 2001;31:1409–1430. [Google Scholar]
- (13).Derevensky JL, Gupta R, Cioppa GD. A developmental perspective of gambling behavior in children and adolescents. Journal of Gambling Studies. 1996;12:49–66. doi: 10.1007/BF01533189. [DOI] [PubMed] [Google Scholar]
- (14).Toneatto T, Blitz-Miller T, Calderwood K, Dragonetti R, Tsanos A. Cognitive distortions in heaving gambling. Journal of Gambling Studies. 1997;13:253–266. doi: 10.1023/a:1024983300428. [DOI] [PubMed] [Google Scholar]
- (15).Moore SM, Ohtsuka K. Beliefs about control over gambling among young people, and their relation to problem gambling. Psychology of Addictive Behaviors. 1999;13:339–347. [Google Scholar]
- (16).Davis D, Sundahl I, Lesbo M. Illusory personal control as a determinant of bet size and type in casino craps games. Journal of Applied Social Psychology. 2000;30:1224–1242. [Google Scholar]
- (17).Goodie AS. The role of perceived control and overconfidence in pathological gambling. Journal of Gambling Studies. 2005;21:481–502. doi: 10.1007/s10899-005-5559-1. [DOI] [PubMed] [Google Scholar]
- (18).Wohl MJA, Enzle ME. The deployment of personal luck: Sympathetic magic and illusory control in games of pure chance. Personality and Social Psychology Bulletin. 2002;28:1388–1397. [Google Scholar]
- (19).Petry NM, Ammerman Y, Bohl J, et al. Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology. 2006;74:555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- (20).Petry NM. Cognitive-behavioral therapy. Pathological gambling: Etiology, comorbidity, and treatment. American Psychological Association; Washington, DC: 2005. pp. 229–256. [Google Scholar]
- (21).Ladouceur R, Sylvain C, Boutin C, et al. Cognitive treatment of pathological gambling. Journal of Nervous and Mental Disease. 2001;189:766–773. doi: 10.1097/00005053-200111000-00007. [DOI] [PubMed] [Google Scholar]
- (22).Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, Leblond J. Group therapy for pathological gamblers: A cognitive approach. Behaviour Research and Therapy. 2003;41:587–596. doi: 10.1016/s0005-7967(02)00036-0. [DOI] [PubMed] [Google Scholar]
- (23).Dorion JP, Nicki RM. Prevention of pathological gambling: A randomized controlled trial. Cognitive Behaviour Therapy. 2007;36:74–84. doi: 10.1080/16506070601092966. [DOI] [PubMed] [Google Scholar]
- (24).Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- (25).Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Addison-Wesley; Reading, MA: 1975. [Google Scholar]
- (26).Larimer ME, Neighbors C. Normative misperception and the impact of descriptive and injunctive norms on college student gambling. Psychology of Addictive Behaviors. 2003;17:235–243. doi: 10.1037/0893-164X.17.3.235. [DOI] [PubMed] [Google Scholar]
- (27).Moore SM, Ohtsuka K. The prediction of gambling behavior and problem gambling from attitudes and perceived descriptive norms. Social Behavior and Personality. 1999;27:455–466. [Google Scholar]
- (28).Sheeran P, Orbell S. Augmenting the theory of planned behavior: Roles for anticipated regret and descriptive norms. Journal of Applied Social Psychology. 1999;29:2107–2142. [Google Scholar]
- (29).Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68:728–733. [PubMed] [Google Scholar]
- (30).Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- (31).Neighbors C, Lewis MA, Bergstrom RL, Larimer ME. Being controlled by normative influences: Self-determination as a moderator of a normative feedback alcohol intervention. Health Psychology. 2006;25:571–579. doi: 10.1037/0278-6133.25.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. Guilford Press; New York: 1991. [Google Scholar]
- (33).Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed Guilford Press; New York: 2002. [Google Scholar]
- (34).Petry NM, Armentano C. Prevalence, assessment, and treatment of pathological gambling: A review. Psychiatric Services. 1999;50:1021–1027. doi: 10.1176/ps.50.8.1021. [DOI] [PubMed] [Google Scholar]
- (35).Baer JS, Marlatt GA, Kivlahan DR, Fromme K, Larimer ME, Williams E. An experimental test of three methods of alcohol risk reduction with young adults. Journal of Consulting and Clinical Psychology. 1992;60:974–979. doi: 10.1037//0022-006x.60.6.974. [DOI] [PubMed] [Google Scholar]
- (36).Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, Williams E. Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology. 1990;58:805–810. doi: 10.1037//0022-006x.58.6.805. [DOI] [PubMed] [Google Scholar]
- (37).Baer JS, Kivlahan DR, Blume AW, McKnight P, Marlatt GA. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 2001;91:1310–1316. doi: 10.2105/ajph.91.8.1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Larimer ME, Turner AP, Anderson BK, et al. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62:370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- (39).Marlatt GA, Baer JS, Kivlahan DR, et al. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- (40).Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- (41).Hodgins DC, Currie SR, el Guebaly N. Motivational enhancement and self-help treatments for problem gambling. Journal of Consulting and Clinical Psychology. 2001;69:50–57. doi: 10.1037//0022-006x.69.1.50. [DOI] [PubMed] [Google Scholar]
- (42).Takushi RY, Neighbors C, Larimer ME, Lostutter TW, Cronce JM, Marlatt GA. Indicated prevention of problem gambling among college students. Journal of Gambling Studies. 2004;20:83–93. doi: 10.1023/B:JOGS.0000016705.58903.8f. [DOI] [PubMed] [Google Scholar]
- (43).Petry NM, Weinstock J, Morasco BJ, Ledgerwood DM. Brief motivational interventions for college student problem gamblers. Addiction. 2009;104:1569–1578. doi: 10.1111/j.1360-0443.2009.02652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Petry NM. Gamblers anonymous and cognitive-behavioral therapies for pathological gamblers. Journal of Gambling Studies. 2005;21:27–33. doi: 10.1007/s10899-004-1919-5. [DOI] [PubMed] [Google Scholar]
- (45).Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- (46).American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1987. revised. [Google Scholar]
- (47).Volberg RA, Steadman HJ. Refining prevalence estimates of pathological gambling. American Journal of Psychiatry. 1988;145:502–505. doi: 10.1176/ajp.145.4.502. [DOI] [PubMed] [Google Scholar]
- (48).Wickwire EM, Jr, Burke RS, Brown SA, Parker JD, May RK. Psychometric evaluation of the National Opinion Research Center DSM-IV Screen for Gambling Problems (NODS) American Journal on Addictions. 2008;17:392–395. doi: 10.1080/10550490802268934. [DOI] [PubMed] [Google Scholar]
- (49).Gerstein D, Murphy S, Toce M, et al. Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission. National Opinion Research Center; Chicago: 1999. [Google Scholar]
- (50).Moyers TB, Martin T, Manuel JK, Miller WR. The motivational interviewing treatment integrity (MITI) code. (Version 2.0) 2003 http://casaa.unm.edu/download/miti.pdf.
- (51).Moyers TB, Martin TM, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- (52).Moyers TB, Miller WR, Hendrickson SML. How does motivational interviewing work? Therapist interpersonal skill as a predictor of client behavior within motivational interviewing sessions. Journal of Consulting and Clinical Psychology. 2005;73:590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- (53).Cohen J, Cohen P, West S, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed Lawrence Erlbaum Associates; Hillsdale, NJ: 2003. [Google Scholar]
- (54).Rosenthal R, Rosnow RL. Essentials of behavioral research: Methods and data analysis. 2nd ed McGraw-Hill; New York: 1991. [Google Scholar]
- (55).Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- (56).Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- (57).MacKinnon DP, Dwyer JH. Estimating mediating effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- (58).MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (59).Goodman LA. On the exact variance of products. Journal of the American Statistical Association. 1960;55:708–713. [Google Scholar]
- (60).Arbuckle JL, Wothke W. Amos 4.0 Users’ Guide. Smallwaters Corporation; Chicago: 1999. [Google Scholar]
- (61).Hollis S, Campbell F. What is meant by intention-to-treat analysis? Survey of published randomized controlled trials. British Medical Journal. 1999;319:670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (62).Hodgins DC, el Guebaly N. Natural and treatment-assisted recovery from gambling problems: A comparison of resolved and active gamblers. Addiction. 2000;95:777–789. doi: 10.1046/j.1360-0443.2000.95577713.x. [DOI] [PubMed] [Google Scholar]
- (63).Pulford J, Bellringer M, Abbott M, Clarke D, Hodgins D, Williams J. Reasons for seeking help for a gambling problem: The experience of gamblers who sought specialist assistance and the perceptions of those who have not. Journal of Gambling Studies. 2009;25:19–32. doi: 10.1007/s10899-008-9112-x. [DOI] [PubMed] [Google Scholar]
- (64).Hodgins DC, Makarchuk K. Trusting problem gamblers: Reliability and validity of self-reported gambling behavior. Psychology of Addictive Behaviors. 2003;17:244–248. doi: 10.1037/0893-164X.17.3.244. [DOI] [PubMed] [Google Scholar]
- (65).Taber JI, McCormick RA, Russo AM, Adkins BJ, Ramirez LF. Follow up of pathological gamblers after treatment. American Journal of Psychiatry. 1987;144:757–761. doi: 10.1176/ajp.144.6.757. [DOI] [PubMed] [Google Scholar]
- (66).Kypri K, Stephenson S, Langley J. Assessment of nonresponse bias in an internet survey of alcohol use. Alcoholism: Clinical and Experimental Research. 2004;28:630–634. doi: 10.1097/01.alc.0000121654.99277.26. [DOI] [PubMed] [Google Scholar]
- (67).Tournageau R. Survey research and societal change. Annual Review of Psychology. 2004;55:775–801. doi: 10.1146/annurev.psych.55.090902.142040. [DOI] [PubMed] [Google Scholar]
- (68).Petry NM. Stages of change in treatment-seeking pathological gamblers. Journal of Consulting and Clinical Psychology. 2005;73:312–322. doi: 10.1037/0022-006X.73.2.312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.