Abstract
Bifid mandibular condyles (BMCs) are rare anomalies. The overwhelming majority of prior reports described their predominantly unilateral occurrence diagnosed by panoramic radiography. We present an even rarer case of bilateral BMC initially identified by panoramic radiography and confirmed with colour-enhanced three-dimensional CT. These images substantiate the theory that the secondary condyles arise from the neck of the mandible (Lopez-Lopez et al. Bifid condyle: review of the literature of the last 10 years and report of two cases. Cianio 2010; 28: 136–140).
Keywords: bifid mandibular condyle
Introduction
The existence of bifid mandibular condyles (BMCs) was first identified in 1941.1 From then until 2008, there were 79 reported cases; however, in the past 2 years alone, there have been an additional 69 reported cases.2-7 This marked increase in documenting BMC is probably owing to clinicians becoming more aware of its existence, as evidenced by 2 different research groups retrospectively reviewing 60 000 panoramic radiographs, and by clinicians' use of more sophisticated imaging studies, such as CT, cone beam CT and MRI.8,9 A review of the 148 patient case reports reveals that BMC occurs more often unilaterally than bilaterally in a ratio of approximately 4.4:1 and does not show predictable preference for age or gender. BMC is usually discovered incidentally on imaging studies; however, its aetiology and a precise description remain unsettled.
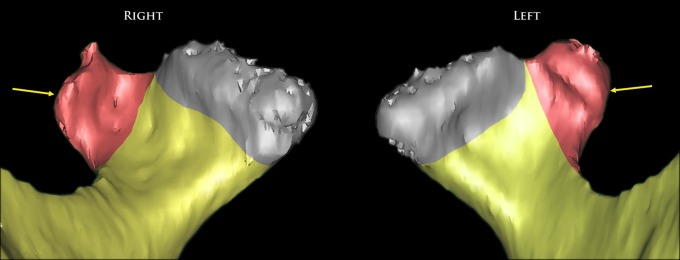
We report a case of bilateral BMC in which both secondary condylar heads arise from their respective necks of the mandible. This appearance is consistent with the most contemporaneous description of the entity, as provided by Lopez-Lopez et al,10 and we are the first research group to substantiate their thesis using three-dimensional (3D) CT colour-enhanced images which specifically delineate the exact anatomical landmarks that must be assessed in order to arrive at this diagnosis.
Case report
A 64-year-old Caucasian male presented to the oral and maxillofacial surgery clinic of the Los Angeles Veteren's Affairs Medical Center, Los Angeles, CA with a chief complaint of intermittent pain on a scale of eight out of ten in his right temporomandibular joint (TMJ). The patient's symptoms, as well as the bilateral condylar osseous irregularities seen on the panoramic radiograph (Figure 1), prompted the surgeon to obtain CT to better visualize the bony morphology and MRI to evaluate the disc/meniscus.
Figure 1.
A panoramic radiograph demonstrating a bilateral bifid mandibular condyle (arrows)
A detailed medical history revealed that over the past 5 years the patient had begun to notice episodic pain in his right TMJ when opening his mouth widely, but that the pain was not associated with mastication. The patient denied bruxism, parafunctional habits, a history of radiation therapy to the head and neck and a familial history of craniofacial abnormalities. The patient's medical history was, however, significant for osteoarthritis of the knees and hips for which he had been prescribed tramadol hydrochloride 50 mg by his primary care clinician. The clinical laboratory data was unremarkable.
Maxillofacial clinical examination
The extraoral examination was unremarkable with no obvious facial asymmetries or scars. Examination of the TMJ using a stethoscope revealed mild crepitus on the right side but no crepitus on the left. The muscles of mastication were not tender to palpation. Maximum incisal opening was 50 mm with a 10 mm left excursive movement and a 4 mm right excursive movement. Mandibular deviation was not noted upon either opening or closing. Intraoral examination revealed coincident midlines and a Class I canine relationship and the patient was partially edentulous. The dentition did not display fremitus or any unusual wear facets.
Radiographic interpretation
The panoramic radiograph demonstrated bilateral radiopaque masses apparently appended to the right and left condylar head and necks (Figure 1). CT (axial and coronal projections) of the mandible demonstrated bilateral, aberrant bony masses in the shape of secondary condylar heads (Figures 2 and 3). These smaller, non-articulating secondary heads were spatially oriented anterolaterally and, although apparently contiguous with the larger normally positioned condylar heads, a constriction between the two was noted. The MRI (Figure 4) demonstrated that the TMJ discs on each side were positioned between the glenoid fossa and larger, medial condylar heads. There was no evidence of disc subluxation. Using the CT images, a 3D reconstruction was rendered and provided a much clearer depiction of the discrepancy in size between the normal and secondary condylar heads. These images also more clearly delineated the spatial orientation of the condylar heads to each other as well as the fact that they were not contiguous with one another (Figure 5). Most importantly, the 3D reconstructed images were critical in determining that the secondary, lateral condylar heads were, in fact, emerging from the mandibular necks (Figure 6) as described by Lopez-Lopez et al.10
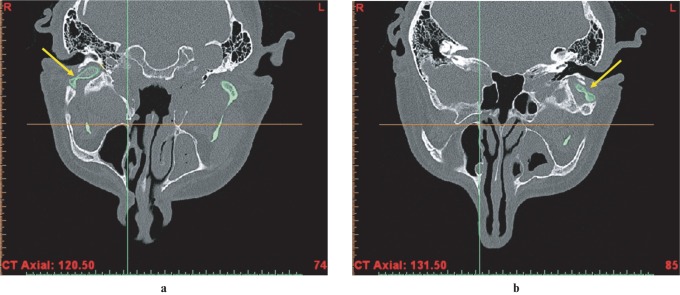
Figure 2.
A CT axial projection showing what appears to be contiguous condylar heads with a constricted region between them: (a) right condyle; (b) left condyle
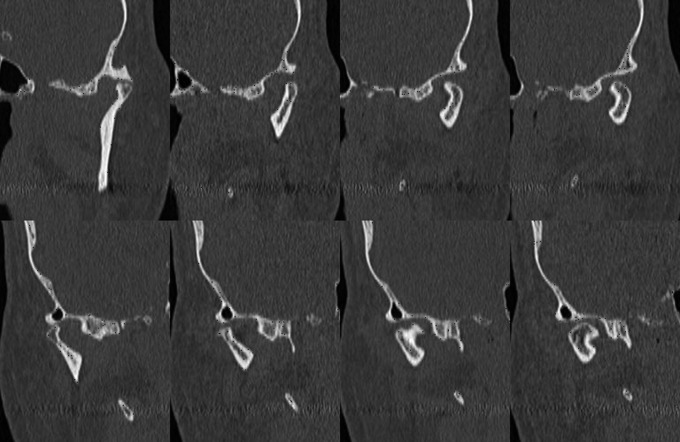
Figure 3.
A CT coronal projection: (top row) left condyle; (bottom row) right condyle. When viewing the images from left to right, their orientation moves from anterior to posterior. Note that there is not a single projection that was able to capture both condylar heads simultaneously
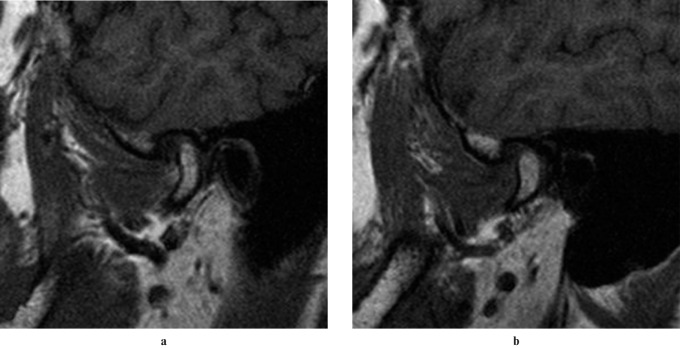
Figure 4.
A MRI demonstrating that the temporomandibular joint (TMJ) discs associated with the right and left functioning condylar heads are normal in the closed position: (a) left TMJ; (b) right TMJ
Figure 5.
A three-dimensional aerial view of the mandible constructed from a CT scan. Note that, on this view, it cannot be discerned if the condylar heads on the patient's left side are separate nor can it be concluded that the second (auxiliary) condylar heads arise from the mandibular neck. It is, however, obvious from this rendering that on each side the lateral heads are smaller than the articulating, medial (normal) condylar heads
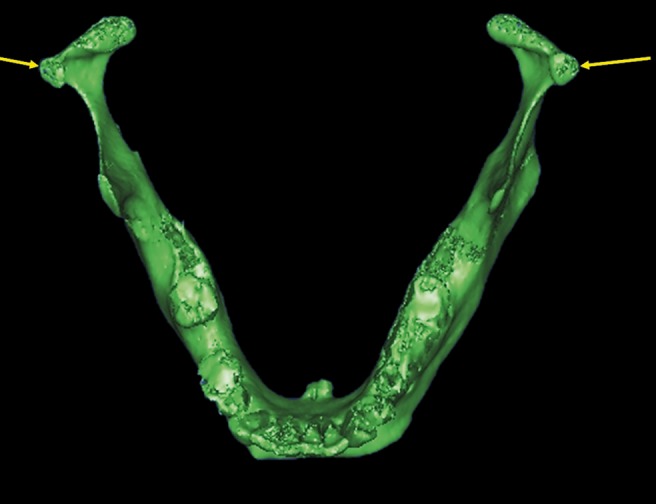
Figure 6.
A set of three-dimensional (3D) coronal (anterior) views reconstructed from a CT scan demonstrate that the auxiliary condyles emerge from the mandibular neck (note: the articulating surfaces of the condylar heads on CT axial and coronal images from which the 3D reconstruction was built showed smooth, rounded contours. The jagged articular surfaces of condyles are artefacts and arise from their electronic separation from glenoid fossa when extrapolating the mandible from the 3D skull image). Auxiliary condyles are indicated with arrows. The normal articulating condyles are located towards the centre of the figure
Discussion
This case report of bilateral BMC is consistent with the most contemporaneous description of the entity as reported by Lopez-Lopez et al,10 in which the secondary condylar heads arise from the respective necks of the mandible. However, with the recent upsurge in reporting of BMC, a wide variety of other presentations have been noted and so the exact definition of BMC remains controversial. In 1941, Hrdlicka described the anomaly as a “mandibular condyle spilt or [divided] into two parts by a sulcus or groove of variable depth”.1 Decades later in 1998, Stefanou et al11 described BMC as the splitting of the condylar head which can range from a shallow groove to the formation of two distinct condyles with but a single separate neck irrespective of whether the heads are oriented mediolaterally or anteroposteriorly. In 2008, Dennison et al12 suggested that “true” BMC must be orientated anteroposteriorly and that those presenting in the mediolateral position be excluded from the grouping and termed “condylar notching”. 2 years later in 2010, Lopez-Lopez et al10 declared that irrespective of the spatial orientation of the normal and secondary condylar heads, both have to emerge from the condylar neck in order to be considered “true” BMC.
Irrespective of how one defines bifidity, the anomaly exists and a differential diagnosis must be developed if the patient becomes symptomatic. It is plausible to speculate that BMCs are in fact osteomas. Osteomas, slow-growing benign tumour masses of mature compact or cancellous bone arising from a bony surface with a polypoid form and circumscribed sclerotic borders, often appear on imaging studies very much like BMC.13 The definitive diagnosis of an osteoma, however, requires a histological specimen whereas the diagnosis of BMC is made solely by imaging studies.
If the diagnosis of BMC requires that the condylar heads be positioned in an anteroposterior orientation, as proposed by Dennison et al,12 then our case would fall short in qualifying. However, we believe that Dennison et al's postulate does not take into account the fact that mandibular condyles are oriented in an oblique fashion, thus necessitating that TMJ studies be reformatted in an oblique, coronal (parallel to the horizontal long axis of the mandibular condyle) orientation.14-16 We question their definition because they only provide a two-dimensional description. This was demonstrated in our non-oblique coronal CT (Figure 3); both condylar heads were unable to be viewed in a single projection. Therefore, in order to arrive at the correct diagnosis and to fully assess whether the condylar heads emerge from the mandibular neck, we propose the use of 3D CT reconstructed images, if clinically indicated, to accurately diagnose BMC.
Conclusion
We have presented a case of bilateral BMC and substantiated diagnosis using 3D reconstruction models which demonstrated that each of the secondary condyles emerged from the respective condylar necks. Because the diagnosis of BMC is rendered purely from imaging studies, there need to be more precise criteria relating the specific appearance to the type of imaging system with the recognition that, if clinically indicated, 3D reconstruction of CT provides the most accurate depiction of the entity.
Acknowledgment
The authors gratefully acknowledge the technical and artistic assistance of Jon Nicolini, BS, in the preparation of the colour-enhanced 3D CT images.
References
- 1.Hrdlicka A. Lower jaw: double condyles. Am J Phys Anthropol 1941;28:75–89 [Google Scholar]
- 2.Sala-Perez S, Vazquez-Delgado E, Rodriguez-Baeza A, Gay-Escoda C. Bifid mandibular condyle: a disorder in its own right? J Am Dent Assoc 2010;141:1076–1085 [DOI] [PubMed] [Google Scholar]
- 3.Faisal M, Ali I, Pal US, Bannerjee K. Bifid mandibular condyle: report of two cases of varied etiology. Natl J Maxillofac Surg 2010;1:78–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunduz K, Avsever H, Karacayli U. Bilateral bifid condylar process. Int J Morphol 2010;28:941–944 [Google Scholar]
- 5.Balaji S. Bifid mandibular condyle with temporomandibular joint ankylosis—a pooled data analysis. Dent Traumatol 2010;26:332–337 [DOI] [PubMed] [Google Scholar]
- 6.Khonsari R, Corre P, Bouguila J, Lumineau JP, Heuze Y. Bifid mandibular condyle: position of the supernumerary condyle. Rev Stomatol Chir Maxillofac 2010;111:221–224 [DOI] [PubMed] [Google Scholar]
- 7.Fuentes FR, Flores FH, Silva MH, Flores LT. Bifid condylar process. Cases report. Int J Morphol 2009;27:539–541 [Google Scholar]
- 8.Miloglu O, Yalcin E, Buyukkurt M, Yilmaz A, Harorli A. The frequency of bifid mandibular condyle in a Turkish patient population. Dentomaxillofac Radiol 2010;39:42–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menezes A, de Moraes Ramos FM, de Vasconcelos-Filho JO, Kurita LM, de Almeida SM, Haiter-Neto F. The prevalence of bifid condyle detected in a Brazilian population. Dentomaxillofac Radiol 2008;37:220–223 [DOI] [PubMed] [Google Scholar]
- 10.Lopez-Lopez J, Ayuso-Montero R, Jane-Salas E, Rosello-Llabres X. Bifid condyle: review of the literature of the last 10 years and report of two cases. Cranio 2010;28:136–140 [DOI] [PubMed] [Google Scholar]
- 11.Stefanou E, Fanourakis IG, Vlastos K, Katerelou J. Bilateral bifid mandibular condyles. Report of four cases. Dentomaxillofac Radiol 1998;27:186–188 [DOI] [PubMed] [Google Scholar]
- 12.Dennison J, Mahoney P, Herbison P, Dias G. The false and the true bifid condyles. Homo 2008;59:149–159 [DOI] [PubMed] [Google Scholar]
- 13.Warner BF, Luna MA, Newland JR. Temporomandibular joint neoplasms and pseudotumors. Adv Anat Pathol 2000;7:365–381 [DOI] [PubMed] [Google Scholar]
- 14.Honey OB, Scarfe WC, Hilgers MJ, Klueber K, Silveira AM, Haskell BS, et al. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop 2007;132:429–438 [DOI] [PubMed] [Google Scholar]
- 15.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004;33:196–201 [DOI] [PubMed] [Google Scholar]
- 16.Mafee MF, Valvassori GE, Becker M. Imaging of the head and neck (2nd edn). Stuttgart: Georg Thieme Verlag, 2005 [Google Scholar]